Abstract
A 33-primer multiplex PCR-based reverse line blot (mPCR/RLB) assay was developed to identify Streptococcus agalactiae serotypes and surface protein antigen genes simultaneously. It was evaluated by using 551 clinical isolates. The mPCR/RLB assay was more sensitive than conventional serotyping, especially for protein antigen typing, but otherwise the results correlated well.
Recently, we developed separate multiplex PCR-based reverse line blot-hybridization (mPCR/RLB) assays to identify molecular serotypes (MS) (2) and protein antigen gene profiles (PGPs) (9) of Streptococcus agalactiae (group B streptococcus [GBS]). The aim of this study was to develop an assay that would identify MS and PGPs simultaneously and could potentially replace the use of antisera for typing. To evaluate the new combined assay, we compared the results with those of conventional serotyping for 27 well-characterized reference strains and 551 consecutive GBS isolates referred for serotyping to the Streptococcus Reference Laboratory, Institute of Environmental Science and Research (ESR), Porirua, New Zealand, some of which have been studied previously (3, 4).
Conventional serotyping (CS) was performed as described before (8). Rabbit antisera were raised at ESR, using standard methodology (WHO International Reference Centre for Streptococcus Typing, Prague, Czech Republic) and GBS serotype strains obtained from the New Zealand Reference Culture Collection Medical Section. Antisera were not raised against serotypes VI to VIII because they were very rare in New Zealand at the time. Antisera were checked for specificity against type-specific antigens for all strains.
mPCR/RLB primers and probes from our previous studies (2, 9) were combined together in the same mPCR/RLB assay for this study. The 17 targets were one GBS species-specific target (cfb), nine MS-specific targets (serotypes Ia to VIII) (2, 9), and seven PGP-specific targets (genes encoding Bca/Cα, Rib, Alp1 [Alp1/Alp5/Epsilon], Alp2, Alp3, Alp4, and the immunoglobulin A binding protein Bac/Cβ) (9). In all, there were 33 primers (alp2 and alp3 share the same forward primer) and 34 probes (two for each target). mPCR/RLB was performed as previously described (2, 9), except that for mPCR, the 33 primers were combined in the same tube with 0.2 μl (1 unit) rather than 0.1 μl (0.5 unit) QIAGEN Hotstar Taq polymerase (5 units/μl); for RLB, 17 probe pairs (see above) were used on the same membrane.
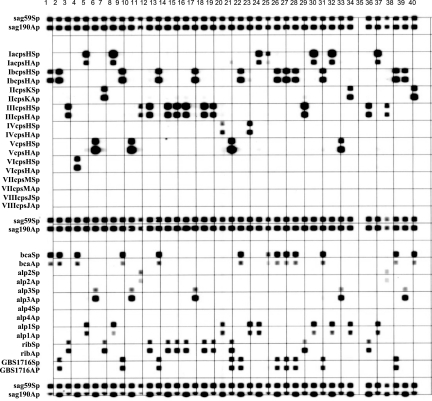
The MS and PGPs of all 27 reference strains (Table 1), as identified by the 33-primer mPCR/RLB assay, were identical to those obtained previously by PCR and sequencing (3, 4), separate MS 20-primer mPCR/RLB (2) and PGP 13-primer mPCR/RLB (9) assays, and CS for those that were serotypeable (25 reference strains) and for which protein type results were available (9 reference strains). The CS results and mPCR/RLB results for 551 clinical isolates are shown in Table 2. mPCR/RLB results for 40 isolates from 1997 to 1998 are shown in Fig. 1.
TABLE 1.
Results of CS, MS identification based on PCR and sequencing, and mPCR/RLB for 27 reference strains
| Strain | CSa | MS | PGPa |
|---|---|---|---|
| O90 (Rockefeller University)b | Ia | Ia | Alp1 |
| H36B (ATCC 12401; NCTC 8187)b | Ib | Ib | Bca and Bac |
| 18 RS 21 (NCTC 11079)b | II | II | Rib |
| M 781 (ATCC BAA-22)b | III | III | Rib |
| 3139b | IV | IV | Alp1 |
| CJB 111 (ATCC BAA-23)b | V | V | Alp3 |
| SS 1214b | VI | VI | Alp1 |
| 7271b | VII | VII | Alp3 |
| JM9 130013b | VIII | VIII | Alp3 |
| A909 (NCTC 11078)b | Ia | Ia | Bca and Bac |
| BM110b | III/R4/Rib | III | Rib |
| NZRM 908 (NCDC SS 615)c | Ia | Ia | Alp2 |
| NZRM 909 (NCDC SS 618)c | Ib | Ib | Bca and Bac |
| NZRM 910 (NCDC SS 700)c | Ia/c | Ia | Bca and Bac |
| NZRM 911 (NCDC SS 619)c | II | II | Rib |
| NZRM 912 (NCDC SS 620)c | III | III | Alp2 |
| NZRM 2832 (Prague 1/82; ATCC 49446)c | IV | IV | Alp1 |
| NZRM 2833 (Prague 10/84; ATCC 49447)c | V | V | Alp3 |
| NZRM 2834 (Prague 118754)c | VI | VI | Bca and Bac |
| NZRM 2217 (Prague 25/60; ATCC 49448)c,d | NT-R | II | Alp4 |
| O90 (ATCC 12400)e | Ia | Ia | Alp2 |
| A909 (NCTC 11078)e | Ia-AB | Ia | Bca and Bac |
| 335 (NCTC 12906)e | Ia-A | Ia | Alp1 |
| 70339 (NCTC 12907)e | Ia-BR4 | Ia | Bca, Bac, and Rib |
| 65604 (3)e | III-R4 | III | Rib |
| 15626/81 (3)e | IV-B | IV | Bca and Bac |
| Pattison (NCTC 9828)e | NT-R3R4 | II | Alp4 |
NT, nonserotypeable; Bca, Cα; Bac, Cß; Alp1, Alp1/Alp5/Epsilon.
Eleven GBS reference strains from Lawrence Paoletti and Catherine Lachenauer, Channing Laboratory, Boston, Mass.
Nine GBS reference strains from Diana Martin, Streptococcus Reference Laboratory, ESR, Wellington, New Zealand.
This isolate is the atypical reference strain Prague 25/60, which was nonserotypeable using capsular polysaccharide antisera but was assigned to molecular serotype II. It expresses a protein that is antigenically similar to R (and is used to generate R antiserum), encoded by the gene alp4.
Seven GBS reference strains from Johan Maeland, Department of Microbiology, School of Medicine, Norwegian University of Science and Technology, Trondheim, Norway.
TABLE 2.
Comparison of CS for capsular type with mPCR/RLB results for 551 GBS clinical isolates
| CS | No. of isolates | No. of isolates with MS by mPCR/RLB
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ia | Ib | II | III | IV | V | VI | VII | VIII | ||
| Ia | 122 | 122 | ||||||||
| Ib | 58 | 58 | ||||||||
| II | 43 | 43 | ||||||||
| III | 149 | 149 | ||||||||
| IV | 16 | 16 | ||||||||
| V | 94 | 94 | ||||||||
| NTa | 69 | 6 | 18 | 7 | 8 | 2 | 17 | 6 | 2 | 3 |
| Total | 551 | 128 | 76 | 50 | 157 | 18 | 111 | 6 | 2 | 3 |
NT, nontypeable (includes one isolate which was retyped as MS VII by CS).
FIG. 1.
Results of mPCR/RLB assay for 40 consecutive isolates. Sample 35 was buffer, which was used as a negative control. Probes sag59Sp and sag190Ap are group B streptococcus specific. Molecular serotype probes are named according to the corresponding serotype, the cps gene target (e.g., cpsH, cpsK, etc.), and whether the probe is sense (S) or antisense (A). Protein gene probes are named for the corresponding protein, except for GBS1716Ap and GBS1716Sp, which are the sense (S) and antisense (A) probes targeting the Cβ gene (bac) (3, 4).
mPCR/RLB identified the MS of all 551 isolates, including 65 (12%) that were nonserotypeable by CS. MS III, Ia, V, Ib, and II accounted for 85% of isolates. In New Zealand, MS VI and VIII were first isolated in 1998 and MS VII was first isolated in 2001; 11 of 551 (1.9%) isolates (16% of those that were nonserotypeable by CS) belonged to these MS. There were 5 of 484 isolates for which the results of both CS and MS were available but discordant. These isolates were sent to Central Public Health Laboratory, Health Protection Authority, United Kingdom, for serotyping, with the following results: two (previously identified by CS as serotypes III and Ib) were nonserotypeable (mPCR/RLB identified them as MS Ia and V, respectively); one identified as serotype Ib by CS was retyped as serotype VI, which was concordant with the MS result; one previously identified by CS as serotype III was retyped as serotype V, which agreed with the MS result; and one previously identified by CS as serotype Ib and by mPCR/RLB as MS V was confirmed to be serotype Ib. The mPCR/RLB assay was repeated for this isolate, and the result also confirmed that it was MS Ib, suggesting that the wrong isolate was tested or the result was wrongly transcribed the first time. Thus, in all, there were 67 (12%) isolates that were nonserotypeable by CS. The final results are shown in Table 2.
The majority of isolates (401 [73%]) were nontypeable using antisera against the R and C antigens. R protein antigens were identified in 96 (17%) isolates, and C antigens were identified in 54 (10%) of 551 isolates. However, at least one protein antigen gene was identified by mPCR/RLB in 547 (99%) isolates (Table 3); bca was the most common and usually was present with another protein gene (most commonly bac), as previously reported (9). Apart from bac, protein genes were almost always mutually exclusive, except for the case of a single atypical isolate which had both bca and rib. Of the 96 isolates with R proteins, 1 had no detectable protein genes, 71 (73%) contained rib, 23 (24%) contained alp3, and 1 contained alp1. Apart from the first and last isolates, these results were consistent between CS and mPCR/RLB. Of the 54 isolates that were positive for the C protein, 34 (62%) contained alp1, 19 (35%) contained bac (of which 10 also had bca), and 1 contained alp2. Only the last result was inconsistent between CS and mPCR/RLB. As previously demonstrated, the identification of protein antigens using antisera is difficult, and cross-reactions are common (6). However, in general, isolates that express the R protein, as demonstrated using antisera, contain rib or alp3, and those that express the C protein contain alp1 or bac (Cα), with or without bca (Cβ) (5, 7, 9).
TABLE 3.
Relationships between MS and PGPs for 551 GBS clinical isolates
| MS | No. of isolates | No. of isolates with PGPa
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| bca only | bca and bac | alp1 | alp2 | alp3 | rib | rib and bac | Noneb | ||
| Ia | 127 | 7 | 3 | 112 | 4 | 1 | |||
| Ib | 77 | 3 | 70 | 4 | |||||
| II | 50 | 13 | 9 | 6 | 1 | 12 | 8 | 1 | |
| III | 158 | 1 | 14 | 5 | 137 | 1 | |||
| IV | 18 | 17 | 1 | ||||||
| V | 110 | 1 | 3 | 3 | 98 | 2 | 1 | 2 | |
| VI | 6 | 4 | 1 | 1 | |||||
| VII | 2 | 1 | 1 | ||||||
| VIII | 3 | 3 | |||||||
| Total | 551 | 28 | 87 | 140 | 19 | 124 | 148 | 1 | 4 |
No isolates contained alp4.
None of the seven PGPs were detected.
In this study, the relationships between MS and PGPs were generally the same as previously demonstrated, namely, MS Ia and IV strains carried alp1, MS Ib strains carried bca and bac, MS II strains carried various genes, MS III strains carried rib, and MS V and VIII strains carried alp3 (Table 3) (3). A minority of isolates had an atypical combination, suggesting the occurrence of gene recombination. The identification of these atypical isolates will be important for disease surveillance in relation to potential vaccine use.
Some probes reacted (usually very weakly) with amplicons from more than one serotype. For example, amplicons from most MS Ia and V isolates cross-hybridized weakly with VcpsHSp and IacpsHSp, as previously described (2). However, the combined results for VcpsHAp/VcpsHSp and IacpsHAp/IacpsHSp clearly distinguished between serotypes Ia and V (Fig. 1). Otherwise, the sensitivity and specificity of mPCR/RLB were considerably better than those of CS and similar to those of individual serotype-specific PCRs for confirmed GBS isolates.
The development of multivalent conjugate GBS vaccines containing the most important serotypes and, potentially, specific GBS protein antigens is under way. Epidemiological studies and surveillance of GBS serotype and PGP distributions for different diseases, age groups, and countries and over time are needed to support vaccine development. The relatively recent emergence of serotypes VI, VII, and VIII demonstrates the ongoing evolution of GBS. Our mPCR/RLB assay for detection of MS and PGPs will provide a convenient and inexpensive tool for ongoing surveillance. The mPCR/RLB assay is easy to perform and does not require the use of expensive commercial antisera (which are available only for some serotypes) or in-house antisera, which have variable specificity and quality and frequently cross-react. The amplification products of 43 isolates can be tested simultaneously in the mPCR/RLB assay, making the assay suitable for high-throughput epidemiological studies of GBS (2). Because PCR detects the presence of capsular genes, it can characterize isolates with low or absent capsular expression, which are nonserotypeable by CS. The mPCR/RLB assay has enabled, for the first time, the objective, simultaneous identification of GBS capsular types and protein antigens without the need for interpretation requiring an experienced operator. It also has the potential to be used directly for clinical specimens (1).
Acknowledgments
Fanrong Kong and Xianyu Zeng contributed equally to this work.
Several isolates for which the results were controversial were kindly tested with antisera against all serotypes by Androulla Efstratiou at the WHO Collaborating Centre for Diphtheria and Streptococcal Infections, Health Protection Agency Centre for Infections, Colindale, London, United Kingdom. We thank Ilya Henner for precious help with sequencing.
REFERENCES
- 1.Gold, B. 2003. Origin and utility of the reverse dot-blot. Expert Rev. Mol. Diagn. 3:143-152. [DOI] [PubMed] [Google Scholar]
- 2.Kong, F., L. Ma, and G. L. Gilbert. 2005. Simultaneous detection and serotype identification of Streptococcus agalactiae using multiplex PCR and reverse line blot hybridization. J. Med. Microbiol. 54:1133-1138. [DOI] [PubMed] [Google Scholar]
- 3.Kong, F., S. Gowan, D. Martin, G. James, and G. L. Gilbert. 2002. Molecular profiles of group B streptococcal surface protein antigen genes: relationship to molecular serotypes. J. Clin. Microbiol. 40:620-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kong, F., S. Gowan, D. Martin, G. James, and G. L. Gilbert. 2002. Serotype identification of group B streptococci by PCR and sequencing. J. Clin. Microbiol. 40:216-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lachenauer, C. S., R. Creti, J. L. Michel, and L. C. Madoff. 2000. Mosaicism in the alpha-like protein genes of group B streptococci. Proc. Natl. Acad. Sci. USA 97:9630-9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lachenauer, C. S., D. L. Kasper, J. Shimada, Y. Ichiman, H. Ohtsuka, M. Kaku, L. C. Paoletti, P. Ferrieri, and L. C. Madoff. 1999. Serotypes VI and VIII predominate among group B streptococci isolated from pregnant Japanese women. J. Infect. Dis. 179:1030-1033. [DOI] [PubMed] [Google Scholar]
- 7.Lindahl, G., M. Stalhammar-Carlemalm, and T. Areschoug. 2005. Surface proteins of Streptococcus agalactiae and related proteins in other bacterial pathogens. Clin. Microbiol. Rev. 18:102-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkinson, H. W., and M. D. Moody. 1969. Serological relationships of type I antigens of group B streptococci. J. Bacteriol. 97:629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao, Z., F. Kong, and G. L. Gilbert. 2006. Reverse line blot assay for direct identification of seven Streptococcus agalactiae major surface protein antigen genes. Clin. Vaccine Immunol. 13:145-149. [DOI] [PMC free article] [PubMed] [Google Scholar]