Abstract
We compared posaconazole M27-A2 and M38-A MICs to Etest and YeastOne MICs for 92 zygomycetes, 126 Aspergillus isolates, 110 Candida isolates, and Cryptococcus neoformans. Reference MICs were also correlated with inhibition zone diameters in millimeters (modified M44-A disk and Neo-Sensitabs tablet methods). Etest MICs were obtained on solidified (1.5% agar) RPMI 1640 (2% dextrose), and zone diameters were obtained on supplemented (2% glucose and 0.5 μg/ml methylene blue [for all isolates]) and nonsupplemented Mueller-Hinton (MH; molds only) agar. MICs and zone diameters were obtained between 16 and 72 h. The overall agreement (% MIC pairs within a three-dilution range) between reference posaconazole and YeastOne MICs was 98 to 100% at 16 to 24 h for zygomycetes and yeasts and 99% at 24 to 48 h for Aspergillus. The overall agreement was lower between reference posaconazole and Etest MICs (94 to 97%) and by both methods with amphotericin B for all species (95 to 99.3%). For yeasts, the correlation coefficient was similar between reference posaconazole MICs and either disk (R, 0.810) or tablet (R, 0.769) zone diameter at 24 h and was superior on MH agar for molds at 16 to 48 h (R, 0.804 and 0.799 for disk and tablet, respectively). For amphotericin B, the best correlation between reference MICs and zone diameters was observed at 16 to 48 h for molds on MH agar (R, 0.736 to 0.812 and 0.765 to 0.749 for disk and tablet, respectively) and at 48 h for yeasts (R, 0.681 and 0.503 for disk and tablet, respectively). These data suggest the potential value of these alternative broth dilution and agar diffusion methods for testing posaconazole and amphotericin B in the clinical laboratory against the species evaluated.
Aspergillus fumigatus and Candida albicans are responsible for the majority (85 to 90%) of the different clinical manifestations of fungal infections. More recently, the zygomycetes, other Aspergillus spp., and Candida spp. have emerged as important fungal pathogens, especially in the severely immunocompromised host (19, 29). Posaconazole, a new triazole undergoing clinical trials, has demonstrated more in vitro activity than itraconazole and voriconazole against the zygomycetes and other molds (7-9, 27) as well as activity against most Candida spp. and Cryptococcus neoformans (24, 25). Posaconazole's potential use as a salvage therapy for zygomycosis has also been recently demonstrated (15); as of now, amphotericin B is the therapeutic choice for zygomycosis. Although the Clinical and Laboratory Standards Institute (CLSI; formerly NCCLS) Subcommittee on Antifungal Susceptibility Tests has developed reproducible procedures for the antifungal susceptibility testing of yeasts and molds by broth microdilution (documents M27-A2 and M38-A) and yeasts by disk (document M44-A for fluconazole and voriconazole) methods (2-4), reference guidelines are not available for mold disk testing.
The clinical laboratory needs easy, reliable, and non-time-consuming alternative methods for determining MICs of antifungal agents. The broth microdilution YeastOne Colorimetric Antifungal plate (TREK Diagnostics Systems, Cleveland, OH) and Etest (AB BIODISK, Solna, Sweden) have been cleared by the FDA for testing Candida spp. with fluconazole, itraconazole, and flucytosine. Both commercial methods have been favorably evaluated for MIC determination of voriconazole, amphotericin B, and itraconazole against Aspergillus spp. and other molds (1, 10, 20, 21, 26). More recently, Etest and disk methodology have been applied as alternative methods for testing posaconazole against yeasts (23) and molds (14, 17). The Neo-Sensitabs (A/S Rosco Diagnostica, Taastrup, Denmark) method utilizes a 9-mm tablet for antimicrobial susceptibility evaluation; it has been favorably investigated for testing yeasts with fluconazole (28).
The purpose of this study was to compare several agar diffusion (modified M44-A disk and Neo-Sensitabs tablet [inhibition zone diameters, in millimeters] and Etest [MICs]) and broth YeastOne (MICs) procedures to reference methods (M27-A2 and M38-A) for susceptibility testing of 10 species of zygomycetes, 5 species of Aspergillus, 8 species of Candida, and C. neoformans. The evaluation included the following determinations. (i) Determination of reference posaconazole MICs by CLSI broth microdilution M38-A and M27-A2 methods (yeasts and molds). (ii) Determination of posaconazole MICs by commercial broth microdilution colorimetric YeastOne plate and by agar diffusion Etest methods (yeasts and molds). (iii) Determination of posaconazole inhibition zone diameters (in millimeters) by modified reference M44-A disk diffusion and by commercial Neo-Sensitabs tablet agar diffusion methods (yeasts and molds). (iv) Determination of the correlation coefficient between inhibition zone diameters (in millimeters) and reference MICs for both yeasts and molds. Similar testing was performed with amphotericin B, but yeast isolates were not tested by YeastOne or Etest methods, because these methods have been extensively evaluated for this purpose.
MATERIALS AND METHODS
The investigational triazole posaconazole (Schering-Plough Research Institute, Kenilworth, N.J.) and amphotericin B (Bristol-Myers Squibb Pharmaceuticals Research Institute, Wallingford, Conn.) were provided by the manufacturers as standard powders for the preparation of CLSI microdilution trays. Drug dilutions were prepared at 100× the final concentration in polyethylene glycol (posaconazole) and dimethyl sulfoxide (amphotericin B) and then diluted in the standard RPMI 1640 medium to yield the final twofold drug concentrations of 16 to 0.03 μg/ml for CLSI methods (2, 3).
Isolates.
A total of 328 isolates were evaluated and included 11 Absidia corymbifera strains, 1 Actinomucor elegans strain, 11 Cunninghamella bertholletiae strains, 24 Mucor spp. strains, 2 Rhizomucor pusillus strains, 36 Rhizopus arrhizus strains, 4 R. microsporus var. microsporus strains, 3 Syncephalastrum spp. strains, 60 A. fumigatus strains, 18 A. flavus strains, 14 A. nidulans strains, 16 A. niger strains, 18 A. terreus strains, 25 C. albicans strains, 10 strains each of C. dubliniensis, C. glabrata, C. guilliermondii, C. lusitaniae, C. krusei, C. parapsilosis, C. tropicalis, and 15 Cryptococcus neoformans strains. The isolates were recovered from clinical specimens at the VCU Medical Center, Richmond, Va., University of Iowa College of Medicine, Iowa City, and University of Texas Health Sciences Center, San Antonio. Selected yeast and mold isolates with high and low MICs for both antifungal agents were included. The CLSI quality control (QC) isolates C. krusei ATCC 6258 and Paecilomyces variotii ATCC MYA-3630 were tested each time a set of isolates was evaluated. Posaconazole and amphotericin B MICs by both CLSI and commercial methods were within the established MIC limits (5, 11).
Inoculum preparation.
Stock inoculum suspensions for yeasts were prepared as described in the M27-A2 document from 24-h (Candida spp.) and 48-h (C. neoformans) cultures on Sabouraud dextrose agar (Remel, Lenexa, KS) (2). Stock inoculum suspensions for Aspergillus spp. and the zygomycetes were prepared from 7-day cultures grown on potato dextrose agar (Remel) and adjusted spectrophotometrically to optical densities that ranged from 0.09 to 0.17 (65 to 82% transmittance) (3).
(i) CLSI broth microdilution reference methods (M27-A2 and M38-A).
On the day of the test, each microdilution well containing 100 μl of the twofold drug concentrations was inoculated with 100 μl of the diluted twofold inoculum suspension (the final volume in each well was 200 μl); the twofold test inoculum sizes ranged from 1.2 × 103 to 3.8 × 103 CFU/ml (yeasts) to 0.9 × 104 to 3.8 × 104 CFU/ml (molds) as demonstrated by colony counts (2, 3). Growth (drug free) and sterility controls were included for each isolate tested. Microdilution trays were incubated in ambient air at 35°C and examined for MIC determination at 24 (zygomycetes), 48 (Candida spp. and Aspergillus spp.), and 72 h (C. neoformans). By visual examination, reference MICs were defined as the lowest concentrations that showed either 50% (only for yeasts with posaconazole) or 100% (yeasts and molds) growth inhibition compared to the control well (growth control) (2, 3). QC isolates were tested in the same manner.
(ii) Disk diffusion methodology.
The CLSI M44-A disk diffusion method describes guidelines for yeast testing with fluconazole and voriconazole; we followed these guidelines, with certain modifications (4). Briefly, the entire surface of Mueller-Hinton agar supplemented with 2% dextrose and 0.5 μg/ml methylene blue (MGM; Hardy Diagnostics, Santa Maria, Calif.) and nonsupplemented Mueller-Hinton (MH; Hardy Diagnostics) agar plates (150-mm plates) were inoculated simultaneously in three directions by using a nontoxic cotton swab dipped in the undiluted mold stock inoculum suspensions; stock yeast inoculum suspensions were inoculated only on MGM agar. The inoculated agar was allowed to dry for 15 to 30 min, and the disks (posaconazole, 5 μg [Becton Dickson and Company, Sparks, Md.]; amphotericin B, 10 μg [Abtek Biologicals Ltd., Liverpool, United Kingdom]) were applied to the inoculated agar with a pair of forceps. The plates were incubated in ambient air at 35°C. QC isolates were tested in the same manner.
(iii) Neo-Sensitabs tablet method.
The Neo-Sensitabs tablet method was performed according to the manufacturer's instructions and M44-A guidelines. Briefly, both MGM (molds and yeasts) and MH (only molds) agars (Hardy Diagnostics) were inoculated as described above for the disk methodology; 9-mm posaconazole (5 μg) and amphotericin B (10 μg) tablets, provided by Rosco Laboratory (A/S Rosco), were applied to the inoculated agar with a pair of forceps. The plates were incubated in ambient air at 35°C. QC isolates were tested in the same manner.
Inhibition zone diameter determination.
Zone diameters for both disk and tablet diffusion assays were measured to the nearest whole millimeter at the point in which there was a prominent reduction of growth (80%) after 16 (zygomycetes), 24, 48 (all isolates), and 72 h (C. neoformans). Mold filaments bending over the inhibition zones were ignored.
(iv) YeastOne colorimetric plate.
Posaconazole YeastOne MICs were obtained for all isolates. Because this panel has been extensively evaluated for testing amphotericin B versus yeasts, amphotericin B YeastOne colorimetric MICs were only obtained for the 92 zygomycete and 126 Aspergillus isolates. On the day of the test, the dried YeastOne plates were rehydrated with the working suspension (approximately 103 [yeasts] and 104 [molds] CFU/ml) by dispensing 100 μl into each well. YeastOne plates were sealed and incubated in ambient air at 35°C for 24 to 72 h. By means of a view box, YeastOne colorimetric MICs corresponded to the lowest concentration of the antifungal agent that remained blue or unchanged (indicating no growth; amphotericin B) or to the first dilution that either changed to slightly purple (which is equivalent to the CLSI standard of 50% or more growth inhibition) or remained unchanged (posaconazole). QC isolates were tested in the same manner.
(v) Etest.
Amphotericin B Etest MICs also were not obtained for yeast isolates. The undiluted stock inoculum suspension (Aspergillus and zygomycetes) was used to inoculate the surface of an RPMI 1640 agar plate (1.5% agar and 2% dextrose; Remel) for the determination of Etest MICs. The whole surface of the agar was inoculated with 400 μl of the inoculum suspension (150-mm plates), and the inoculum was spread in three directions by using a nontoxic cotton swab (14). The inoculated agar was allowed to dry for 15 to 30 min, and Etest strips were applied to the agar with a pair of forceps. The plates were incubated in ambient air at 35°C. As described by the manufacturer, Etest MICs were defined as the lowest drug concentration where the border of the inhibition ellipse intercepted the MIC scale on the strip at 16 h (zygomycetes) as well as 24 to 48 h (zygomycetes and Aspergillus spp.); filaments bending over the ellipse were ignored. QC isolates were tested in the same manner.
Reproducibility methodology.
MICs and inhibition zone diameters were obtained on three different days for selected isolates (low and high reference MICs) for approximately 10% of the study isolates (32 yeast, Aspergillus spp., and zygomycete isolates) by each method.
Data analysis.
Both on-scale and off-scale MICs were included in the data analysis, and Etest MICs were elevated to the next twofold dilution concentration, which matched the drug dilution schema of the CLSI methods (2, 3). MIC ranges were obtained for each species and test by each method. Geometric mean MICs and MICs for 90% of the isolates tested also were determined for species represented by at least 10 isolates. MICs of the reference methods (at the recommended incubation times of 24 h for zygomycetes; 48 h for Aspergillus spp. and Candida spp.; and 72 h for C. neoformans [M27-A2 and M38-A documents]) were compared to those of Etest and YeastOne (first and second readings) methods, and differences between MICs of no more than two dilutions (e.g., 0.25, 0.5, and 1.0 μg/ml) were used to obtain the percentages of agreement; the same criterion was used to obtain MIC reproducibility data (obtained on three different days for selected isolates) (2, 3). For the correlation between reference MICs and inhibition zone diameters (in millimeters) around disks and tablets, a linear regression analysis using the least-square method (Pearson's correlation coefficient; MS Excel software) was performed by plotting zone diameters against their respective MIC endpoints. The reproducibility of zone diameters obtained in different days with selected study isolates was evaluated by calculating the percentage of replicate zone diameters that were within two standard deviations of the mean.
RESULTS AND DISCUSSION
We report the first evaluation of the suitability of testing posaconazole by Etest and YeastOne methods for the zygomycetes and of testing Candida spp. and C. neoformans by disk and Neo-Sensitabs tablet agar diffusion assays. A prior evaluation for testing posaconazole against molds by disk diffusion has been reported for three Mucor spp. and seven Rhizopus spp. isolates (17), while 92 isolates were included in our study. We also report the first evaluation of disk and tablet diffusion methods for testing amphotericin B. It is important to investigate the suitability of these simpler and commercially available assays (YeastOne, Etest, and Neo-Sensitabs) and the disk method, because CLSI broth microdilution methods are more cumbersome and time-consuming for use in the clinical laboratory.
The reproducibility of posaconazole and amphotericin B Etest and YeastOne MICs was excellent; a total of 95 to 98% of triplicate results were within a three-dilution range for the 32 selected isolates (from the total 328 isolates). Posaconazole and amphotericin B MICs for both QC isolates, C. krusei ATCC 6258 and P. variotii ATCC MYA-3630 (tested 12 times), were within the expected MIC ranges (5, 11). The reproducibility of posaconazole and amphotericin B zone diameters obtained by both disk and Neo-Sensitabs tablet assays was similar on both MGM and MH agars (89 to 98% within two standard deviations), with the highest percentages of agreement at 16 to 24 h for the zygomycetes and yeasts and at 48 to 72 h for Aspergillus spp. and C. neoformans. The reproducibility of these non-reference methods was similar to those obtained in CLSI studies that were conducted for the development of reference methods (2-6).
The agreement between either Etest or YeastOne and reference M38-A MICs for the 92 zygomycete isolates is listed in Table 1; only the percentage of agreement at the optimal incubation times identified for each species is listed. The highest agreement (100%) between posaconazole YeastOne and reference MICs was consistently observed at 16 (R. arrhizus) to 24 h for all species evaluated, while the agreement was poor at 48 h (0 to 100%; results not shown in Table 1). For amphotericin B, the agreement was higher at 48 h than at 24 h (96 to 100% versus 70 to 83%, respectively) for Absidia corymbifera, Mucor spp., and R. arrhizus. Similar results were obtained by Etest, with the exception that for R. arrhizus the best agreement was at 24 h with amphotericin B. The overall agreement between commercial and reference methods was slightly lower for Etest (95.7 to 96.5%) than for YeastOne (99.3 to 100%). The in vitro susceptibility data by the three methods were compatible with those previously reported for most of the species, where posaconazole demonstrated similar in vitro activity to that of amphotericin B (Table 1) as well as better activity than other triazoles (7-9, 27). The exceptions were our amphotericin B MICs, which were higher than those reported elsewhere for five isolates of C. bertholletiae (reference MIC range, 2 to 8 versus 0.12 to 2 μg/ml) (27); 11 isolate were tested in the present study.
TABLE 1.
Percent agreement at optimal incubation times of either posaconazole or amphotericin B Etest and YeastOne MICs with reference MICs and susceptibility data obtained by the three methods for 92 zygomycete isolatesa
| Species (no. of isolates tested) | Agent | % Agreement of reference with E/Yb | MICs (μg/ml) by:
|
|||||
|---|---|---|---|---|---|---|---|---|
| Etest
|
M38-A
|
YeastOne
|
||||||
| Range | G/MIC90 | Range | G/MIC90 | Range | G/MIC90 | |||
| Absidia corymbifera (11) | P | 100c/100c | 0.12-1.0 | 0.4/0.25 | 0.25-1.0 | 0.56/1.0 | 0.25-1.0 | 0.56/0.5 |
| A | 100d/100d | 0.5-2 | 1.4/1.0 | 0.25-1.0 | 0.84/1.0 | 0.25-0.5 | 0.67/0.5 | |
| Cunninghamella bertholletiae (11) | P | 100c/100c | 0.25-1.0 | 0.48/1.0 | 0.25-1.0 | 0.61/1.0 | 0.06-1.0 | 0.53/1.0 |
| A | 100c/100c | 2->8 | 4.72/8 | 2-8 | 3.45/8 | 2-4 | 2.18/2 | |
| Mucor spp. (18) | P | 83c/100c | 0.06->8 | 2.42/8 | 0.06-4 | 0.78/1.0 | 0.12-8 | 0.93/1.0 |
| A | 83d/100d | 0.25->8 | 3.2/1.0 | 0.25-4 | 0.79/1.0 | 0.25-4 | 0.96/2 | |
| M. circinelloides (3) | P | 100c/100c | 0.5-1.0 | ND | 1.0-2 | ND | 0.5-1.0 | ND |
| A | 100c/100c | 0.25-1.0 | ND | 0.5-1.0 | ND | 0.5-1.0 | ND | |
| M. ramosissimus (3) | P | 100c/100c | 0.5-1.0 | ND | 1.0-2 | ND | 0.5-1.0 | ND |
| A | 100c/100c | 1.0 | ND | 0.25-1.0 | ND | 0.5 | ND | |
| Rhizopus arrhizus (36) | P | 91c/100c | 0.25->8 | 3.9/4 | 0.25-4 | 1.4/2 | 0.25-8 | 1.68/2 |
| A | 91c/96d | 0.06-2 | 0.7/2 | 0.25-4 | 1.14/2 | 0.5-8 | 1.28/2 | |
| R. microsporus var. microsporus (4) | P | 100c/100c | 0.5-2 | ND | 0.5-1.0 | ND | 0.25-1.0 | ND |
| A | 100c/100c | 1.0-4 | ND | 1.0-2 | ND | 2 | ND | |
| Syncephalastrum spp. (3) | P | 100c/100c | 0.5-1.0 | ND | 0.12-1.0 | ND | 0.06-0.5 | ND |
| A | 100d/100c | 0.12-0.25 | ND | 0.25-0.5 | ND | 0.12-0.5 | ND | |
| Others (3)e | P | 100c/100c | 0.12 | ND | 0.12-0.5 | ND | 0.03-0.25 | ND |
| A | 100d/100c | 0.25-2 | ND | 0.25-1.0 | ND | 0.12-0.25 | ND | |
| All zygomycetes (92) | P | 95.7c/100c | 0.06->8 | 2.29/8 | 0.06-4 | 0.91/2 | 0.03-8 | 1.05/2 |
| A | 96.5/99.3 | 0.06->8 | 2.2/4 | 0.25-8 | 1.26/2 | 0.12-8 | 1.2/2 | |
NCCLS M38-A broth microdilution method; G, geometric mean MIC; MIC90, MICs for 90% of the isolates tested.
Percentage of agreement between MICs by reference and Etest (E) and between reference and YeastOne (Y); P, posaconazole; A, amphotericin B.
Highest percentage of agreement was obtained at 16 to 24 h (commercial methods) and 24 h (reference method).
Highest percentage of agreement was obtained at 48 h (commercial method).
Includes 1 Actinomucor elegans and 2 Rhizomucor pusillus isolates.
Table 2 presents the suitability of either YeastOne or Etest for testing five species of Aspergillus with posaconazole and amphotericin B; again, only the percentage of agreement at the optimal incubation times identified for each species is listed. The agreement between the posaconazole reference and YeastOne MICs was good to excellent; the best agreement was at 48 h (98 to 100% versus 80 to 100% at 24 h); agreement was also excellent at 24 h for A. flavus and A. terreus (100%). An 85 to 98% agreement has been demonstrated between reference and YeastOne voriconazole MICs for Aspergillus spp. at 48 h (1, 16). Amphotericin B YeastOne MICs were also more in agreement with reference results at 48 h, but the differences were smaller (90 to 100% versus 88 to 100% at 24 h), which indicates that results could be obtained when sufficient growth allows it. Previous reports have reported comparable data (93 to 100%) (20, 21), but only one of these two studies evaluated the 24-h incubation time (21). Between reference and posaconazole Etest endpoints, agreement was also superior at 48 h (90 to 100% versus 80 to 100% at 24 h), with the exception of A. flavus and A. nidulans. In contrast, for amphotericin B Etest MICs, the agreement was consistently superior at 24 h (92 to 100%) (Table 2). Similar percentages of agreement (87 to 100%) have been previously obtained between reference and either amphotericin B, posaconazole, or voriconazole Etest MICs at the same incubation times (10, 14, 20, 21).
TABLE 2.
Percent agreement at optimal incubation times of either posaconazole or amphotericin B by Etest and YeastOne MICs with reference MICs and susceptibility data for the three methods for 126 Aspergillus isolatesa
| Species (no. of isolates tested) | Agent | % Agreement of reference with E/Yb | MICs (μg/ml) by:
|
|||||
|---|---|---|---|---|---|---|---|---|
| Etest
|
M38-A
|
YeastOne
|
||||||
| Range | G/MIC90 | Range | G/MIC90 | Range | G/MIC90 | |||
| A. flavus (18) | P | 100c/100d | 0.01-0.12 | 0.02/0.06 | 0.03-0.12 | 0.04/0.06 | 0.01-0.12 | 0.05/0.06 |
| A | 92c/94d | 0.5->8 | 4.1/>8 | 0.25-4 | 0.96/2 | 1.0-4 | 1.0/2 | |
| A. fumigatus (60) | P | 984/98d | <0.01-1.0 | 0.04/0.25 | 0.03-0.5 | 0.04/0.12 | 0.01-1.0 | 0.04/0.12 |
| A | 97c/92d | 0.25-8 | 1.45/2 | 0.12-4 | 0.67/2 | 0.25-2 | 0.58/1.0 | |
| A. nidulans (14) | P | 100c/100d | <0.01-0.03 | 0.01/0.03 | <0.01/0.06 | 0.03/0.06 | 0.01-0.25 | 0.05/0.12 |
| A | 93c/100d | 0.25->8 | 1.5/2 | 0.25-2 | 1.04/2 | 0.12/1.0 | 0.87/1.0 | |
| A. niger (16) | P | 904/100d | 0.12-0.5 | 0.21/0.5 | 0.06-0.25 | 0.06/0.25 | 0.03-0.12 | 0.08/0.12 |
| A | 100c/100d | 0.5-1.0 | 0.75/1.0 | 0.12-1.0 | 0.3/0.5 | 0.25-0.5 | 0.25/0.5 | |
| A. terreus (18) | P | 1004/100d | 0.06-0.12 | 0.06/0.06 | 0.03-0.06 | 0.03/0.03 | 0.03-0.12 | 0.06/0.12 |
| A | 100c/90d | 0.25-8 | 2.85/4 | 0.25-4 | 1.8/4 | 0.25-4 | 1.6/4 | |
| All Aspergillus spp. (126) | P | 97/99d | <0.015-1.0 | 0.068/0.25 | <0.01-0.5 | 0.04/0.12 | 0.01-1.0 | 0.056/0.12 |
| A | 96c/95d | 0.25->8 | 2.13/2 | 0.12-4 | 0.96/2 | 0.12-4 | 0.86/2 | |
NCCLS M38-A broth microdilution method; G, geometric mean MIC; MIC90, MICs for 90% of the isolates tested.
Percentage of agreement between MICs by reference (obtained at the recommended time of 48 h) and Etest (E) and between reference and YeastOne (Y); P, posaconazole; A, amphotericin B.
Highest percentage of agreement was obtained at 24 h (commercial method).
Highest percentage of agreement was obtained at 48 h.
Table 3 depicts the results of our comparison between either posaconazole YeastOne or Etest MICs (24 and 48 h) with reference M27-A2 MICs for Candida spp. and C. neoformans; amphotericin B MICs were not determined for the yeasts by these methods. As expected and previously reported in a collaborative study (13, 22), the overall agreement between YeastOne and reference MICs was superior at 24 (98%) than at 48 h (82%) for Candida spp., with the exception of C. glabrata (90 and 100% at 24 and 48 h, respectively). The agreement was poor for C. neoformans (79%); although this type of comparison has not been previously reported for this species, YeastOne was also found to be unsuitable for testing C. neoformans compared to other antifungal agents (12). In contrast, between Etest and reference MICs the highest overall level of agreement was at 48 h (94 versus 83% at 24 h). However, percentages of agreement between the methods for each species indicate that Etest MICs of C. albicans, C. dubliniensis, C. glabrata, and C. krusei could be defined at 24 h (Table 3). In a previous study, the lowest percentages of agreement were for C. glabrata, C. parapsilosis, and C. krusei (88 to 93%), but posaconazole Etest MICs were only determined at 48 h (23). The lack of comparative data between posaconazole Etest and reference data for C. neoformans precluded comparison of results, but the performance of Etest for testing this species was good (93% agreement with reference MICs) in the present study.
TABLE 3.
Percent agreement of posaconazole Etest and YeastOne MICs with reference MICs and susceptibility data by the three methods for 110 yeast isolatesa
| Species (no. of isolates tested) | % Agreement of reference with E/Yb | Incubation time (h) | MICs in μg/ml by:
|
|||||
|---|---|---|---|---|---|---|---|---|
| Etest
|
M27-A2
|
YeastOne
|
||||||
| Range | G/MIC90 | Range | G/MIC90 | Range | G/MIC90 | |||
| C. albicans (25) | 92/92 | 24 | <0.01-≥8 | 0.07/4 | 0.03-2 | 0.15/1.0 | ||
| 92/28 | 48 | <0.01-≥8 | 0.1/4 | <0.01-≥8 | 0.15/0.5 | 0.03-≥8 | 0.22/≥8 | |
| C. dubliniensis (10) | 92/100 | 24 | <0.01-0.12 | 0.01/0.06 | 0.01-0.03 | 0.012/0.03 | ||
| 92/100 | 48 | 0.01-0.12 | 0.01/0.12 | 0.01-0.06 | 0.03/0.06 | 0.03-0.25 | 0.03/0.12 | |
| C. glabrata (10) | 100/90 | 24 | 1.0-≥8 | 2/≥8 | 0.5-≥8 | 1.85/≥8 | ||
| 90/100 | 48 | 1.0-≥8 | 2.5/≥8 | 0.5-≥8 | 1.0/≥8 | 1.0-≥8 | 3.2/≥8 | |
| C. guilliermondii (10) | 80/100 | 24 | <0.01-≥8 | 0.04/.25 | 0.06-4 | 0.3/0.5 | ||
| 100/90 | 48 | 0.06-≥8 | 0.15/.5 | 0.03-1.0 | 0.16/0.5 | 0.06-≥8 | 0.46/1.0 | |
| C. krusei (10) | 100/100 | 24 | 0.06-2 | 0.36/1.0 | 0.25-1.0 | 0.42/1.0 | ||
| 100/100 | 48 | 0.5-4 | 1.0/2 | 0.25-1.0 | 0.46/1.0 | 0.5-1.0 | 0.79/1.0 | |
| C. lusitaniae (10) | 70/100 | 24 | <0.01-0.03 | <0.01/0.01 | <0.01-0.12 | 0.02/0.12 | ||
| 90/90 | 48 | <0.01-0.06 | <0.01/0.03 | 0.01-0.06 | 0.03/0.06 | 0.03-0.5 | 0.05/0.25 | |
| C. parapsilosis (10) | 60/100 | 24 | <0.01-0.12 | 0.02/0.12 | 0.01-0.12 | 0.03/0.12 | ||
| 90/100 | 48 | <0.01-0.12 | 0.03/0.12 | 0.03-0.12 | 0.06/0.12 | 0.03-0.25 | 0.1/0.25 | |
| C. tropicalis (10) | 70/100 | 24 | <0.01-≥8 | 0.02/0.25 | 0.12-≥8 | 0.17/0.5 | ||
| 100/50 | 48 | <0.01-≥8 | 0.07/1.0 | <0.01-≥8 | 0.06/1.0 | 0.12-≥8 | 0.37/≥8 | |
| Cryptococcus neoformans (15) | NDc/ND | 48 | ND | ND | ND | ND | ||
| 93/79 | 72 | <0.01-1.0 | 0.11/0.5 | 0.12-0.5 | 0.19/0.5 | <0.01-1.0 | 0.08/0.5 | |
| All isolates (110) | 83/98 | 24 | <0.01-≥8 | 0.36/≥8 | <0.01-≥8 | 0.42/2 | ||
| 94/82 | 48 | <0.01-≥8 | 0.5/≥8 | <0.01-≥8 | 0.13/1.0 | 0.01-≥8 | 0.73/≥8 | |
M27-A2 broth microdilution method; G, geometric mean MIC; MIC90, MICs for 90% of the isolates tested.
Percentage of agreement between MICs by reference (obtained at the recommended times of 48 h for Candida and 72 h for C. neoformans) and Etest (E) and between reference and YeastOne (Y).
ND, not determined due to insufficient growth.
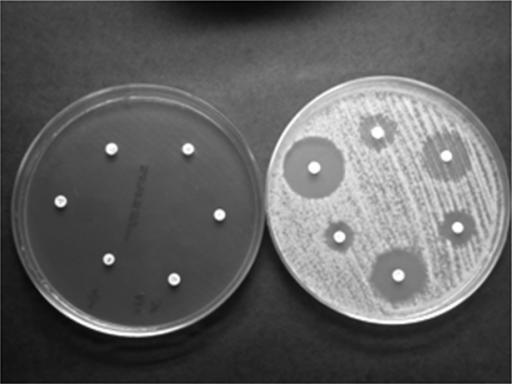
Table 4 lists the results of the correlation coefficient (linear regression analysis) between either reference posaconazole or amphotericin B MICs and corresponding inhibition zones in millimeters (disk and tablet) for molds and yeasts. The correlation was superior for Aspergillus spp. with posaconazole on MH than on MGM agar (e.g., R of 0.826 versus 0.616; posaconazole disk at 48 h). More importantly, MH agar supported better growth, especially of A. fumigatus (Fig. 1), which facilitated an easier reading of inhibition zone diameters. Our posaconazole disk evaluation on MGM agar produced R values similar to those obtained with the same agar for 78 molds, including 10 zygomycete isolates (R, 0.722 to 0.746) (17) and with voriconazole for Aspergillus spp. (R, 0.8) (26); these authors did not evaluate MH agar. The poor performance of MGM as a growth medium for molds is not apparent until larger numbers of isolates and species, such as A. fumigatus, Paecilomyces lilacinus, Alternaria spp., and Bipolaris spp. are tested (A. Espinel-Ingroff, B. A. Arthington-Skaggs, D. J. Diekema, D. Ellis, A. Fothergill, D. Gibbs, S. Messer, and M. Rinaldi, unpublished data). Since MH agar was not suitable for disk testing of yeasts, it was not previously evaluated for disk testing of molds; it is fortunate that nonsupplemented Mueller-Hinton (readily available in microbiology laboratories) appears to perform better than MGM. As expected for yeasts, the correlation between reference posaconazole MICs and zone inhibition diameters (disk and tablet) in millimeters was superior at 24 h (R, 0.810 and 0.769, disk and tablet, respectively) than at 48 h (0.685 and 0.717, disk and tablet, respectively); zones of inhibition for C. neoformans were more readily measured at 72 h. The CLSI has established inhibition zone diameters in millimeters for posaconazole versus four QC Candida spp., and our results for QC isolate C. krusei ATCC 6258 were within the expected range of 21 to 31 mm (6a). To our knowledge, no other reports are available of either disk or tablet testing with posaconazole for species of Candida and C. neoformans. However, our results were similar to those obtained with fluconazole and voriconazole (6). Because this is also the first evaluation of an amphotericin B disk or tablet for testing both molds and yeasts, comparison with previous results was precluded. However, the correlation with reference values was similar to those for posaconazole (Table 4). These results suggest that this simpler disk-tablet methodology could also be applied to either mold or yeast testing with these two agents in the clinical setting.
TABLE 4.
Correlation between posaconazole and amphotericin B inhibition zone diameters with reference M38-A or M27-A2 MICs for zygomycetes, Aspergillus spp., Candida spp., and C. neoformans
| Fungi testeda | Agent | Method | Incubation time (h) | Correlation coefficient (R) for:
|
|
|---|---|---|---|---|---|
| MGM | MH | ||||
| Molds | P | Disk | 24 | 0.779 | 0.804 |
| 48 | 0.616 | 0.826 | |||
| Tablet | 24 | 0.662 | 0.799 | ||
| 48 | 0.667 | 0.799 | |||
| Yeasts | P | Disk | 24 | 0.810 | NDb |
| 48 | 0.685 | ND | |||
| Tablet | 24 | 0.769 | ND | ||
| 48 | 0.717 | ND | |||
| Molds | A | Disk | 24 | 0.683 | 0.736 |
| 48 | 0.515 | 0.8118 | |||
| Tablet | 24 | 0.683 | 0.765 | ||
| 48 | 0.495 | 0.749 | |||
| Yeasts | A | Disk | 24 | 0.681 | ND |
| 48 | 0.681 | ND | |||
| Tablet | 24 | 0.478 | ND | ||
| 48 | 0.503 | ND | |||
Molds: zygomycetes (16- to 24-h results) and Aspergillus spp. (48-h results). Yeasts: Candida spp. and C. neoformans (results obtained at 24 and 72 h, respectively).
ND, not determined.
FIG. 1.
A. fumigatus on MGM and MH agar.
The evaluation of any new method requires the determination of categorical agreement between new and reference method results, as was demonstrated for fluconazole and more recently for voriconazole (6). Although this type of analysis was not possible for these two antifungal agents (breakpoints are not yet available), most isolates for which higher posaconazole MICs (0.5 to >8 μg/ml) for Aspergillus spp. and yeasts were determined were identified by narrower inhibition zones by both disk and tablet methods (0 to 20 mm versus 21 to 41 mm). For the zygomycetes, posaconazole MICs of >1 μg/ml corresponded to the lowest inhibition zone diameters (0 to 15 mm). The smaller amphotericin B inhibition zone diameters (0 to 14 mm versus 15 to 32 mm) were observed for MICs of ≥2 μg/ml, including zone values for the well-documented amphotericin B-resistant C. albicans (ATCC 200955), C. lusitaniae (ATCC 200950 and ATCC 200951), and C. tropicalis (ATCC 200956) (18). Both Etest and YeastOne methods also yielded higher MICs for these strains (Tables 1 to 3).
In conclusion, the optimal testing incubation times were as follows: (i) for posaconazole by YeastOne, 16 h for Rhizopus spp., 24 h for other zygomycetes and most Candida spp., and 48 h for Aspergillus spp. and C. glabrata; (ii) for posaconazole by Etest, 16 h for Rhizopus spp. and 24 h for other zygomycetes, A. flavus, A. nidulans, C. albicans, C. dubliniensis, C. glabrata, and C. krusei, and 48 h for other Candida spp. and Aspergillus spp.; (iii) for amphotericin B by YeastOne, 48 h for Absidia corymbifera, Mucor spp., R. arrhizus spp., and all Aspergillus spp., and 24 h for other zygomycetes; (iv) for amphotericin B by Etest, 48 h for Absidia corymbifera, Mucor spp., and Syncephalastrum spp., and 16 to 24 h for other zygomycetes and all Aspergillus spp. The incubation times were similar for disk-tablet testing with both antifungal agents. MICs were much higher and zone diameters substantially lower at longer incubation times, especially with posaconazole. Based on these results and those of previous studies, it appears that Etest, YeastOne, disk, and tablet assays could be alternative methods for use in the clinical laboratory to determine the susceptibility of yeast and mold species evaluated. Collaborative studies (in progress for disk testing with the molds) will better evaluate the suitability of these methods.
Acknowledgments
Schering-Plough and Rosco Diagnostica provided posaconazole Etest strips, YeastOne panels, and the prototype posaconazole tablet as well as amphotericin B tablets. The two types of Mueller-Hinton agars were donated by Hardy Scientific. Data analysis was conducted by Emilia Canton, Andrew Wang, and David Gibbs. Many thanks to Mercedes Ramirez and Ana Rodriguez for their technical help.
Footnotes
Published ahead of print on 30 August 2006.
REFERENCES
- 1.Castro, C., M. C. Serrano, B. Flores, A. Espinel-Ingroff, and E. Martin-Mazuelos. 2004. Comparison of the Sensititre YeastOne colorimetric antifungal panel with a modified NCCLS M38-A method to determine the activity of voriconazole against clinical isolates of Aspergillus spp. J. Clin. Microbiol. 42:4358-4360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clinical and Laboratory Standards Institute/National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution susceptibility testing of yeasts. Approved Standard, 2nd ed. Document M27-A2. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 3.Clinical and Laboratory Standards Institute/National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard. Document M38-A. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 4.Clinical and Laboratory Standards Institute/National Committee for Clinical Laboratory Standards. 2004. Method for antifungal disk diffusion susceptility testing of yeasts. Approved guideline. Document M44-A. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 5.Clinical and Laboratory Standards Institute. 2006. Quality control minimal inhibitory concentration (MIC) limits for broth microdilution and MIC interpretive breakpoints. Supplement M27-S2. Clinical and Laboratory Standards Institute, Wayne, Pa.
- 6.Clinical and Laboratory Standards Institute. 2006. Zone diameter interpretive standards and corresponding minimal inhibitory concentration (MIC) interpretive breakpoints. Supplement M44-S1. Clinical and Laboratory Standards Institute, Wayne, Pa.
- 6a.CLSI. 2005. Minutes of the CLSI Antifungal Subcommittee Meeting, 2005. CLSI, Wayne, Pa.
- 7.Dannaoui, E., J. Meletiadis, J. W. Mouton, J. F. G. M. Meis, P. E. Verweij, and the Eurofong Network. 2003. In vitro susceptibilities of zygomycetes to conventional and new antifungals. J. Antimicrob. Chemother. 51:45-52. [DOI] [PubMed] [Google Scholar]
- 8.Diekema, D. J., S. A. Messer, R. J. Hollis, R. N. Jones, and M. A. Pfaller. 2003. Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J. Clin. Microbiol. 41:3623-3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Espinel-Ingroff, A. 1998. Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J. Clin. Microbiol. 36:2950-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinel-Ingroff, A. 2001. Comparison of the E-test with the NCCLS M38-P method for antifungal susceptibility testing of common and emerging pathogenic filamentous fungi. J. Clin. Microbiol. 39:1360-1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espinel-Ingroff, A., A. Fothergill, M. Ghannoum, E. Manavathu, L. Ostrosky-Zeichner, M. Pfaller, M. Rinaldi, W. Schell, and T. Walsh. 2005. Quality control and reference guidelines for CLSI broth microdilution susceptibility method (M38-A document) for amphotericin B, itraconazole, posaconazole, and voriconazole. J. Clin. Microbiol. 43:5243-5246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Espinel-Ingroff, A., M. Pfaller, S. A. Messer, C. C. Knapp, S. Killian, H. A. Norris, and M. A. Ghannoum. 1999. Multicenter comparison of the sensititre YestOne colorimetric antifungal panel with the National Committee for Clinical Laboratory Standards M27-A reference method for testing clinical isolates of common and emerging Candida spp., Cryptococcus spp., and other yeast and yeast-like organisms. J. Clin. Microbiol. 37:591-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Espinel-Ingroff, A., M. Pfaller, S. A. Messer, C. C. Knapp, N. Holliday, and S. B. Killian. 2004. Multicenter comparison of the Sensititre YeastOne colorimetric antifungal panel with the NCCLS M27-A2 reference method for testing new antifungal agents against clinical isolates of Candida spp. J. Clin. Microbiol. 42:718-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Espinel-Ingroff, A., and A. Rezusta. 2002. E-test method for testing susceptibilities of Aspergillus spp. to the new triazoles voriconazole and posaconazole and to established antifungal agents: comparison with NCCLS broth microdilution method. J. Clin. Microbiol. 40:2101-2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greenberg, R. N., K. Mullane, J.-A. H. van Burik, I. Raad, M. J. Abzug, G. Anstead, R. Herbrecht, A. Langston, K. A. Marr, G. Schiller, M. Schuster, J. R. Wingard, C. E. Gonzalez, S. G. Revankar, G. Corcoran, R. J. Kryscio, and R. Hare. 2006. Posaconazole as salvage therapy for zygomycosis. Antimicrob. Agents Chemother. 50:126-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linares, M. J., G. Charriel, F. Solis, F. Rodriguez, A. Ibarra, and M. Casal. 2005. Susceptibility of filamentous fungi to voriconazole tested by two microdilution methods. J. Clin. Microbiol. 43:250-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopez-Oviedo, E., A. I. Aller, C. Martin, C. Castro, M. Ramirez, J. M. Peman, E. Canton, C. Almeida, and E. Martin-Mazuelos. 2006. Evaluation of disk diffusion method for determining posaconazole susceptibility of filamentous fungi: comparison with CLSI broth microdilution method. Antimicrob. Agents Chemother. 50:1108-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lozano-Chiu, M., P. W. Nelson, M. Lancaster, M. A. Pfaller, and J. H. Rex. 1997. Lot-to-lot variability of antibiotic medium 3 used for testing susceptibility of Candida isolates to amphotericin B. J. Clin. Microbiol. 35:270-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marr, K. A., R. A. Carter, F. Crippa, A. Wald, and L. Corey. 2002. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin. Infect. Dis. 34:909-917. [DOI] [PubMed] [Google Scholar]
- 20.Martin-Mazuelos, E., J. Peman, A. Valverde, M. Chaves, M. C. Serrano, and E. Canton. 2003. Comparison of the Sensititre YeastOne colorimetric antifungal panel and Etest with the NCCLS M38-A method to determine the activity of amphotericin B and itraconazole against clinical isolates of Aspergillus spp. J. Antimicrob. Chemother. 52:365-370. [DOI] [PubMed] [Google Scholar]
- 21.Meletiadis, J., J. W. Mouton, J. F. G. M. Meis, B. A. Bouman, P. E. Verweij, and the EUROFUNG Network. 2002. Comparison of the Etest and the Sensititre colorimetric methods with the NCCLS proposed standard for antifungal susceptibility testing of Aspergillus species. J. Clin. Microbiol. 40:2876-2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pfaller, M. A., A. Espinel-Ingroff, and R. N. Jones. 2004. Clinical evaluation of the Sensititre YeastOne colorimetric antifungal plate for antifungal susceptibility testing of the new triazoles voriconazole, posaconazole, and ravuconazole. J. Clin. Microbiol. 42:4577-4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfaller, M. A., S. A. Messer, K. Mills, A. Bolmström, and R. N. Jones. 2001. Evaluation of Etest method for determining posaconazole MICs for 314 clinical isolates of Candida species. J. Clin. Microbiol. 39:3952-3954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pfaller, M. A., S. A. Messer, R. J. Hollis, and R. N. Jones. 2001. In vitro activities of posaconazole (Sch 56592) compared with those of itraconazole and fluconazole against 3,685 clinical isolates of Candida spp. and Cryptococcus neoformans. Antimicrob. Agents Chemother. 45:2862-2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pfaller, M. A., S. A. Messer, L. Boyken, C. Rice, S. Tendolkar, R. J. Hollis, G. V. Doern, and D. J. Diekema. 2005. Global trends in the antifungal susceptibility of Cryptococcus neoformans: 1990 to 2004. J. Clin. Microbiol. 43:2163-2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Serrano, M. C., M. Ramirez, D. Morilla, A. Valverde, M. Chavez, A. Espinel-Ingroff, R. Claro, A. Fernandez, C. Almeida, and E. Martin-Mazuelos. 2004. A comparative study of the disc diffusion method with the broth microdilution and Etest methods for voriconazole susceptibility testing of Aspergillus spp. J. Antimicrob. Chemother. 53:739-742. [DOI] [PubMed] [Google Scholar]
- 27.Sun, Q. N., A. W. Fothergill, D. I. McCarthy, M. G. Rinaldi, and J. R. Graybill. 2002. In vitro activities of posaconazole, itraconazole, voriconazole, amphotericin B, and fluconazole against 37 clinical isolates of zygomycetes. Antimicrob. Agents Chemother. 46:1581-1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vandenbossche, I., M. Vaneechoutte, M. Vandevenne, T. De Baere, and G. Verschraegen. 2002. Susceptibility testing of fluconazole by the NCCLS broth microdilution method, E-test, and disk diffusion for application in the routine laboratory. J. Clin. Microbiol. 40:918-921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walsh, T. J., and A. H. Groll. 1999. Emerging fungal pathogens: evolving challenges to immunocompromised patients for the twenty-first century. Transplant. Infect. Dis. 1:247-261. [DOI] [PubMed] [Google Scholar]