Abstract
Alveolar macrophages (AM) are very important for pulmonary innate immune responses against invading inhaled pathogens because they directly kill the organisms and initiate a cascade of innate and adaptive immune responses. Although several factors contribute to inhalational anthrax, we hypothesized that unimpeded infection of Bacillus anthracis is directly linked to disabling the innate immune functions contributed by AM. Here, we investigated the effects of lethal toxin (LT), one of the binary complex virulence factors produced by B. anthracis, on freshly isolated nonhuman primate AM. Exposure of AM to doses of LT that killed susceptible macrophages had no effect on the viability of AM, despite complete MEK1 cleavage. Intoxicated AM remained fully capable of B. anthracis spore phagocytosis. However, pretreatment of AM with LT resulted in a significant decrease in the clearance of both the Sterne strain and the fully virulent Ames strain of B. anthracis, which may have been a result of impaired AM secretion of proinflammatory cytokines. Our data imply that cytolysis does not correlate with MEK1 cleavage, and this is the first report of LT-mediated impairment of nonhuman primate AM bactericidal activity against B. anthracis.
Due to their overwhelming presence in the lung, alveolar macrophages (AM) are the principal immune effector cells in the airways. AM and other cells in the lung, such as dendritic cells (DC), detect microbes through a family of receptors called pattern recognition receptors, which detect pathogen-associated molecular pattern components of microbes. AM are avidly phagocytic cells that are capable of directly killing engulfed microbes when pathogen-associated molecular patterns are detected (2). AM play a key role in maintaining anti-inflammatory conditions within the lung during steady state, helping to prevent chronic inflammatory responses to harmless inhaled antigens. However, during microbial invasion, it is primarily the responsibility of AM to initiate innate immune responses in the lung by releasing immunomodulatory products, such as prostaglandins, leukotrienes, chemokines, and cytokines. The secreted products act in concert to recruit and activate other leukocytes from the blood to the site of infection. Activated AM transmigrate to draining lymph nodes, where they present antigens and secrete cytokines to facilitate activation of the adaptive immune system (14).
The innate protective functions provided by AM appear to be manipulated by the dangerous pathogen Bacillus anthracis during inhalational anthrax, the most lethal form of the disease. A previous report suggested that inhaled spores are avidly phagocytosed by AM (25), and recently DC were implicated in anthrax pathogenesis (3). Phagocytosis of spores did not stimulate significant inflammation in the lung until at least 5 h postinfection (16). It has also been proposed that during this time spores are transported inside AM (16, 23) or DC (3) to the mediastinal and peribronchial lymph nodes. En route to the lymph nodes, the spores germinate into vegetative bacteria (10, 23), which are capable of secreting anthrax lethal toxin (LT) and edema toxin. In the lymph nodes, bacteria quickly escape from macrophages and are released into the lymphatics (8, 16). From there bacilli are disseminated into the circulatory system and throughout the host (15).
Lethal toxin, a combination of protective antigen and lethal factor secreted by B. anthracis, disrupts the mitogen-activated protein kinase (MAPK) signaling pathway of innate immune cells, such as AM and DC, and impairs intracellular signaling required to initiate adaptive immune function (1). To date, no direct causal relationship between disruption of MAPK signaling and LT-mediated cell death has been determined, and the importance of such a relationship for pathogenesis is unclear. Extensive studies of mouse macrophage cell lines demonstrated that LT induces cell death, suggesting that macrophages may be the primary target of LT activity. This hypothesis was supported by a study which showed that mice depleted of macrophages survived lethal doses of LT (11). In contrast, mouse strains whose macrophages were resistant to LT-induced cell death exhibited a higher mortality rate after B. anthracis infection than strains with susceptible macrophages (27). Furthermore, human peripheral blood mononuclear cells are resistant to LT-mediated cytotoxicity, suggesting that cell death may not be a primary function of LT in humans (22). A recent study indicated that the cytotoxic effect of LT on three different human monocytic cell lines was dependent on the differentiation state of the cells (13).
The notion that LT modulates innate and adaptive immunity is gaining momentum, but the exact mechanism of action is not known. To further elucidate the effect of LT on immune cells, we examined the link between toxin exposure and antibacterial responses of nonhuman primate AM.
MATERIALS AND METHODS
Culture and infection of alveolar macrophages.
Nonhuman primate alveolar macrophages from cynomolgus macaques (Macaca fascicularis) were obtained as described previously (6). AM were washed twice in phosphate-buffered saline (PBS) supplemented with 1 mM EDTA and 20 μg/ml of gentamicin. The cells were cultured in Dulbecco modified Eagle medium supplemented with 7.5% fetal bovine serum, 1% minimum essential medium, nonessential amino acids, and 1% glutamine (referred to below as cDMEM). AM were purified by adherence to cell culture plates or glass coverslips and were cultured in cDMEM supplemented with 100 IU of penicillin and 100 μg/ml of streptomycin. The purity of AM was determined by May-Grünwald-Giemsa staining of air-dried cytospin smears. Lavaged cells were 97 to 100% macrophages, and trypan blue exclusion indicated that more than 80% of the AM were viable. Before use in experiments, AM cultures were washed four times to remove antibiotics and any dead cells. AM cultured in cDMEM were treated with recombinant LT or spores at a multiplicity of infection (MOI) of 1 to 5, unless indicated otherwise. For all infections of AM, cell culture plates were centrifuged for 5 min at 500 × g to synchronize infection.
B. anthracis spores.
Culturing, spore preparation, and engineering of green fluorescent protein (GFP)-labeled Sterne spores and nonfluorescent Ames spores were performed as described previously (12, 24). Briefly, to generate GFP-labeled Sterne spores, plasmid pAFp8gfp was used in transfections of B. anthracis bacilli to produce bacilli that constitutively expressed GFP. Plasmid pAFp8gfp contains a kanamycin resistance gene and a synthetic B. anthracis promoter sequence ligated upstream of gfp. The extrachromosomal plasmid replicated during proliferation and segregated with progeny cells. During sporulation, GFP was incorporated inside spores (as determined by immunoelectron microscopy [not shown]), which resulted in GFP-labeled spores. Spores were purified by centrifugation through Renografin (Renocal-76; Bracco Diagnostics, Princeton, N.J.). The purified spores were washed three times with cold sterile water and stored at 4°C. Endotoxin-free reagents were used for spore preparation. Spore preparations were incubated at 65°C for 30 min to kill any vegetative cells and to activate the spores before infection of AM. Spores were resuspended in cDMEM immediately before infection.
Electron microscopy.
For transmission electron microscopy (TEM), AM infected with Ames or Sterne spores for 30 min were fixed at 25°C with 2.5% glutaraldehyde for 1 h. The samples were treated with 1% osmium tetroxide in modified Millonig's buffer (0.1 M PBS, 0.5% dextrose; pH 7.3) (17), stained en bloc with 0.5% uranyl acetate in ethanol, dehydrated in graded ethanol and propylene oxide, and embedded in Poly/Bed 812 resin (Polysciences, Inc., Warrington, PA). Ultrathin sections were placed on 200-mesh nickel grids and stained with 5% uranyl acetate and 0.2% lead citrate.
Fluorescence microscopy.
For detection of early endosomal antigen-1 (EEA1) on phagosome membranes, AM were purified by adherence to microscope coverslips. AM were infected with GFP-labeled Sterne spores at an MOI of 10, centrifuged at 500 × g for 5 min at 4°C, washed with cDMEM, and incubated for 15 min at 37°C. Samples were then fixed with 4% paraformaldehyde in PBS for 30 min, washed with PBS, and permeabilized with cold methanol for 10 s. After incubation for 5 min in blocking buffer that contained 2% donkey serum (Sigma), samples were stained with rabbit anti-EEA1 (Affinity BioReagents, Golden, CO), followed by Alexa 594-conjugated goat anti-rabbit antibody and 4′,6′-diamidino-2-phenylindole (DAPI) (Molecular Probes, Eugene, OR). EEA1 immunofluorescence and intraphagosomal GFP-labeled bacteria were detected either by wide-field epifluorescence microscopy or by confocal microscopy.
To count ingested GFP-labeled Sterne spores, B. anthracis cells located inside AM were distinguished from noninternalized B. anthracis cells after 30 min of infection. Nonpermeablized cells were incubated with a mixture of monoclonal antibodies specific for B. anthracis spore exosporium and for bacillus polysaccharide (kindly provided by T. Abshire and J. Ezzell, USAMRIID) to label all extracellular B. anthracis cells, and this was followed by incubation with a secondary antibody conjugated to Alexa 594 fluorophore. Approximately 200 AM per sample were examined to enumerate internalized spores. Images were collected using a Bio-Rad 2000MP confocal microscope (Bio-Rad, Hercules, CA). The numbers of internal and external spores were determined, and the results were expressed as percentages of the total number of spores counted.
B. anthracis viability.
AM were purified by adherence to glass coverslips and infected in duplicate wells with Sterne or Ames spores at an MOI of 10 for various times before the supernatants were removed and 1% saponin was added to each well for 5 min. The supernatant and coverslip from each well were transferred to a 15-ml conical centrifuge tube. Each well was washed twice with sterile water, and the water was added to the tube containing the corresponding supernatant and coverslip. The wells were examined by microscopy to ensure that all AM were lysed. The contents of each tube were serially diluted into sterile water, and aliquots were plated onto solid LB agar plates and incubated at 37°C for 16 h. The CFU were counted, and the results are expressed as percent changes in CFU from the time of initial infection.
Macrophage viability.
Murine J774A.1 cells or AM were treated with anthrax LT at concentrations ranging from 0 to 10 μg/ml of protective antigen and from 0 to 10 μg/ml of lethal factor (List Biologicals Inc., Campbell, CA). After 4 h of incubation with LT, 125 μg of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (18) dye was added, and the cells were incubated for 2 h. The reaction was stopped by adding an equal volume of lysis buffer (20% dimethyl formamide, 20% sodium dodecyl sulfate, pH 4.7) to the culture medium. Plates were incubated overnight at 37°C, and the absorbance at 570 nm was determined with a multiwell plate reader.
Western blot analysis.
AM were not treated, were treated with lipopolysaccharide (LPS) (Escherichia coli O11:B4), or were exposed to different concentrations of LT. After 4 or 16 h of incubation with LT, cells were lysed in buffer (50 mM Tris-HCl [pH 7.4], 150 mM NaCl, 2 mM EDTA, 25 mM β-glycerophosphate, 1% Triton X-100, 10 mM NaF, 1 mM Na3VO4, protease inhibitor cocktail, phosphatase inhibitor cocktails I and II) and incubated on ice for 30 min. Cellular debris was removed by centrifugation. Total protein (30 μg protein/sample) was separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and then Western blotted with MEK1 N terminus and transferrin receptor antibodies (Upstate Biotechnology, Waltham, MA). Immunoreactive proteins were visualized by enhanced chemiluminescence (Pierce, Rockford, IL).
Cytokine analysis.
Culture supernatants collected from AM treated with either LPS or LT were analyzed by using a human inflammation cytometric bead array kit (BD Biosciences, San Jose, CA) according to the manufacturer's directions. All analyses were performed with a FACSCalibur (BD Biosciences).
RESULTS
Phagocytosis of B. anthracis spores by AM.
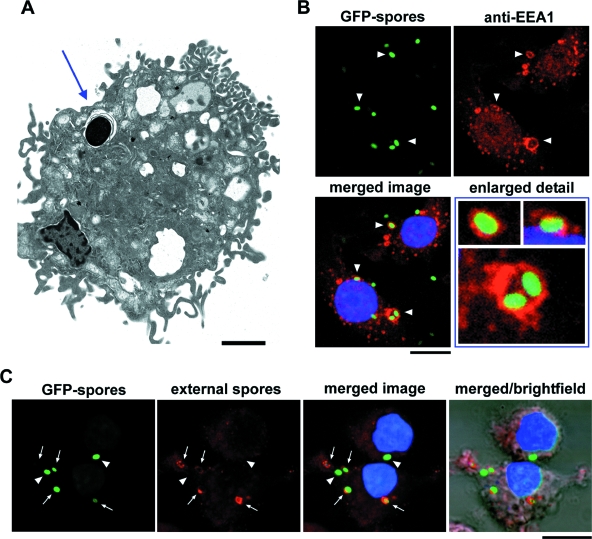
To examine whether AM were able to phagocytose spores via the normal endocytic pathway, the cells were infected with Ames or Sterne spores for 30 min to allow phagocytosis. The intracellular location of both Sterne (Fig. 1A) and Ames (data not shown) spores was determined by TEM, which revealed spores surrounded by a phagosomal membrane. Confocal microscopy showed that within 15 min of infection with GFP-labeled Sterne spores, EEA1, a protein recruited to early phagosomes after endosome fusion, was detected on phagosomes containing B. anthracis. This confirmed the endosomal localization of spores (Fig. 1B). Occasionally, more than one spore was detected within a single phagosome (Fig. 1B). Similar results were obtained with Ames spores (data not shown). Antibody labeling of B. anthracis exosporium and polysaccharide after mild fixation of samples provided an additional way to determine whether GFP-labeled Sterne (Fig. 1C) and Ames (data not shown) spores and bacilli were located inside or outside AM. While all spores and bacilli could be detected by expression of GFP, the antibodies did not cross the intact membranes of the cells, and thus only extracellular spores and bacilli fluoresced both green and red (Fig. 1C).
FIG. 1.
Phagocytosis of B. anthracis spores by AM. (A) AM were infected with B. anthracis strain Sterne spores for 30 min and were analyzed by TEM. The position of a spore inside the AM is indicated by an arrow. Scale bar = 2 μm. (B) AM were infected with GFP-labeled B. anthracis Sterne spores for 15 min and analyzed by confocal fluorescence microscopy for EEA1 (red) recruitment to phagosomes that contained spores (arrowheads). DNA was stained with DAPI (blue). Scale bar = 10 μm. (C) AM were infected with GFP-labeled B. anthracis Sterne spores (green) for 30 min and were stained using a mixture of monoclonal antibodies specific for B. anthracis spore exosporium to label extracellular spores and for bacillus polysaccharide to label extracellular vegetative cells (red). Extracellular GFP-labeled spores and bacilli were available to the antibodies and were stained red (arrows), whereas intracellular GFP-labeled spores and bacilli were shielded from antibody staining and are green only (arrowheads). DNA was stained with DAPI (blue). Scale bar = 10 μm.
Viability of B. anthracis strains after phagocytosis.
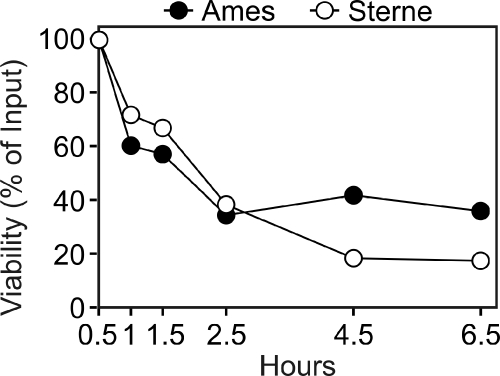
We next determined whether AM could kill B. anthracis. After infection of AM, bacterial viability was monitored at different time intervals. A continuous rapid decline in the viability of Ames and Sterne until 6.5 h postinfection was observed (Fig. 2). Within 6.5 h, more than 60 to 80% of Ames and Sterne spores were killed by AM. Although we found no statistically significant difference between killing of Ames spores by AM and killing of Sterne spores by AM, the AM tended to kill lower numbers of Ames spores than Sterne spores. It is noteworthy that during the 6.5-h incubation, AM were unable to kill all of the spores. This was not due to AM death during Ames and Sterne infections (data not shown).
FIG. 2.
Bactericidal activity of AM against B. anthracis spores. AM were infected with B. anthracis Ames and Sterne spores for different times, and the numbers of CFU were determined. The data are expressed as percent viability and are representative of the responses observed in AM from three nonhuman primates.
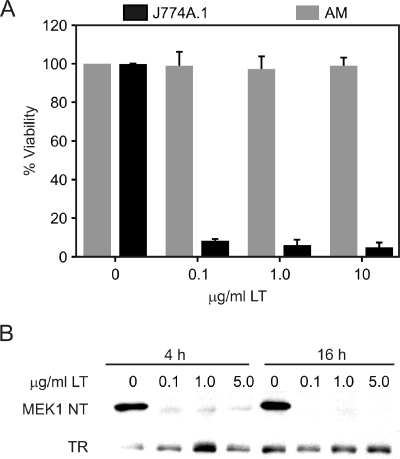
Effect of LT on AM viability and MEK1 cleavage.
Since anthrax LT can kill susceptible macrophages, we next examined the sensitivity of nonhuman primate AM to LT-mediated cell death. AM and J774A.1 macrophages were exposed to different concentrations of LT for 4 h, and cell viability was determined by the MTT assay. At the lowest concentration of LT (0.1 μg/ml), less than 10% of J774A.1 cells were viable, compared to the 98% survival of similarly treated AM (Fig. 3A). Increasing the concentration of LT to 10 μg/ml had little additional effect on the viability of AM, as revealed either by microscopy or by the MTT assay. These results demonstrated that LT is not cytolytic for AM compared to J774A.1 indicator macrophages. To determine if endogenous MEK1 is sensitive to LT-mediated cleavage, AM were incubated with different concentrations of LT. Western blot analysis revealed that MEK1 was cleaved both 4 and 16 h following LT treatment (Fig. 3B).
FIG. 3.
Anthrax lethal toxin does not kill AM but cleaves MEK1. (A) J774A.1 macrophages or AM were incubated with different concentrations of lethal toxin for 4 h, and viability was analyzed by using MTT. The data are expressed as percentages of the viability of untreated macrophages. (B) AM were treated as indicated above for panel A, and samples were analyzed by Western blotting using antibodies specific for the MEK1 N terminus (MEK1 NT) and transferrin (TR). The data represent responses observed for AM from three nonhuman primates.
AM cytokine responses after LT treatment.
Because LT treatment did not induce the death of AM despite cleavage of critical signaling proteins, we next investigated functional impairment of AM by LT. Treatment of AM with LT alone for 4 h resulted in a slight increase in secretion of interleukin-1β (IL-1β) compared to the secretion by untreated AM. There was essentially no effect on tumor necrosis factor alpha (TNF-α), IL-6, or IL-8 secretion (Fig. 4). As expected, addition of LPS to AM elicited production of TNF-α, IL-1β, IL-6, and IL-8, indicating that the AM were capable of producing these cytokines. Simultaneous treatment of AM with LT and LPS resulted in reduced levels of secreted TNF-α, IL-1β, IL-6, and IL-8 after 4 h compared to the levels for AM treated with LPS alone (Fig. 4). These results suggested that the consequence of MEK1 cleavage for AM was impaired induction of proinflammatory cytokine genes partially regulated by signaling in this pathway.
FIG. 4.
Lethal toxin affects cytokine secretion by nonhuman primate alveolar macrophages. AM were treated with 1 μg/ml LT, 100 ng/ml LPS, or both simultaneously for 4 h before culture supernatants were harvested and analyzed by using a cytometric bead array kit. The data represent AM responses for at least three nonhuman primates.
Effect of LT on AM bactericidal activity against B. anthracis.
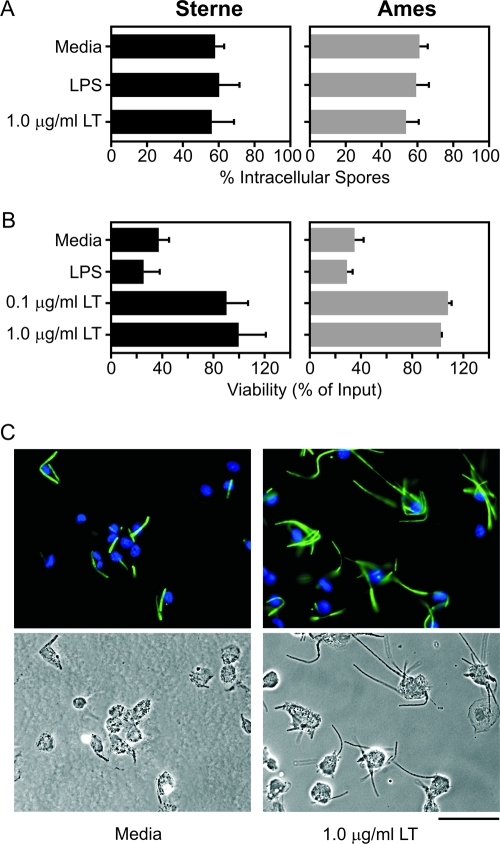
Since LT treatment impaired MAPK signaling and suppressed cytokine production, we next tried to determine whether LT-treated AM were phagocytic. The numbers of phagocytosed Sterne or Ames spores for AM that were treated for 16 h with LT or LPS were not significantly different from the numbers of phagocytosed Sterne or Ames spores for untreated AM (Fig. 5A). Therefore, AM phagocytosis was not impaired by LT despite MEK1 cleavage and cytokine suppression.
FIG. 5.
Lethal toxin impairs bactericidal activity but not phagocytic activity of nonhuman primate alveolar macrophages. (A) AM were treated overnight with 100 ng/ml of LPS or with LT (1 μg/ml) and then infected with Ames or Sterne spores (MOI, 10). After 30 min samples were fixed, and ingested spores were distinguished from external spores by staining nonpermeablized samples with a mixture of antispore and antibacillus antibodies. Internalized spores were counted, and the data were expressed as the percentage of spores internalized based on the total input. (B) AM were treated overnight with either 0.1 μg/ml or 1 μg/ml of LT and then infected for 4.5 h with Ames or Sterne spores, and the numbers of viable CFU were determined. (C) AM were treated overnight with 1 μg/ml LT and then infected with GFP-labeled Sterne spores for 4.5 h before samples were fixed and examined by fluorescence and phase-contrast microscopy. The upper panels show green fluorescent bacilli and DAPI-stained nuclei of macrophages (blue). The data are representative of AM responses for three nonhuman primates. Scale bar = 50 μm.
Next, we examined whether pretreatment of AM with LT impaired their ability to kill B. anthracis. When AM were treated for 16 h with 0.1 or 1 μg/ml of LT and then infected with B. anthracis spores for 4.5 h, the bactericidal activity was substantially reduced, as indicated by enhanced bacterial survival (Fig. 5B). Microscopic examination of AM cultures (Fig. 5C) after 4.5 h of infection with Sterne revealed that the bacteria were able to replicate more efficiently in LT-treated AM cultures than in untreated AM cultures.
DISCUSSION
Alveolar macrophages are a component of sentinel immune cells that protect against infections after inhalation of microbial pathogens. These phagocytic cells can engulf microorganisms and/or other foreign particles and mediate an innate immune response through secretion of cytokines and chemokines. The fate of AM and their response to B. anthracis spores deposited in the lungs are fundamental aspects of the progression of inhalational anthrax. To characterize events in the lungs immediately after aerosol exposure, we examined the interactions between spores of B. anthracis and purified nonhuman primate alveolar macrophages. AM readily phagocytosed B. anthracis spores. The fully virulent Ames spores and the attenuated Sterne spores were both observed in phagosomes surrounded by EEA1 within a few minutes after infection. While the mechanism has not been established yet, mouse (21, 26) and guinea pig peritoneal macrophages (7) can kill B. anthracis. Mouse macrophages phagocytosed germinated Sterne strain 7702 spores and inhibited their growth (9). However, in contrast to nonhuman primate AM (data not shown), murine macrophages did not survive infection.
The MAPK pathway relays environmental signals to the transcriptional machinery in the nucleus. The signaling pathways involving MEK1, MEK2, and MEK3 play a crucial role in activation of macrophages and are directly involved in production of proinflammatory cytokines, such as TNF-α, IL-1β, and IL-6. In our study, nonhuman primate AM viability was not affected, but MEK1 cleavage was detected 4 to 16 h following the exposure of AM to LT (Fig. 3B). In addition, LT impaired the ability of LPS-treated AM to secrete cytokines, which was probably a consequence of MEK1 cleavage. There are conflicting data concerning the modulation of cytokines by LT. Sublethal doses of LT induced production of TNF-α and IL-1β (11) in mouse macrophages, but an absence of this effect has also been reported (4). Additionally, LT has been shown to inhibit the production of nitric oxide (NO) and TNF-α induced by LPS in murine macrophage lines and mouse peritoneal macrophages (20). Excessive amounts of nitric oxide, TNF-α, and IL-1β secreted by macrophages can lead to the development of shock. Mice depleted of macrophages were shown to be insensitive to LT-induced shock, a consequence of the inability of the remaining immune cells to secrete IL-1β (11). It was proposed previously that the impairment of macrophage and dendritic cell (3, 21) cytokine responses by LT may be a means by which B. anthracis inhibits the innate immune response, thereby enhancing its ability to establish an infection.
Despite MEK1 cleavage, impairment of cytokine secretion, and loss of bactericidal activity following LT treatment, AM were still capable of phagocytosis (Fig. 5). The inability of AM to completely eradicate B. anthracis after 6.5 h of infection with spores may have been due to accumulation of LT to critical intoxicating levels inside AM or in the tissue culture medium. Therefore, the primary function of LT in anthrax pathogenesis may be to facilitate bacterial survival and outgrowth from AM, but not AM death. A similar LT-induced loss of guinea pig AM bactericidal activity was described by Gimenez et al. (7), who attributed the effect to LT-inhibited group IIA secreted phospholipase A2. However, we did not detect group IIA secreted phospholipase A2 in the B. anthracis-infected AM culture media (data not shown). It is not known exactly how much LT is produced by B. anthracis during infection, and the amount may depend on the stage of infection. In our study, we were able to observe modulation of AM in the presence of submicrogram amounts of LT. The concentration of LT may be important in pathogenesis, and larger amounts of LT may be relevant during the septicemic stage of anthrax, at which time measurable amounts of LT have been found in the plasma of infected animals (5, 19).
Taken together, these findings suggest that modulation of cytokine responses by LT is a means by which B. anthracis might survive the bactericidal activity of macrophages in the later stages of an infection. The inability of AM to completely eradicate bacteria suggests that intracellularly secreted lethal factor, edema factor, or other virulence factors help overcome the lethal consequences of ingestion by AM. The inhibitory effects of LT on the bactericidal activity of AM may be similar to the effects that LT has on other resident and circulating macrophages in later stages of infection. Our data suggest that following AM infection spores quickly reach endosomal compartments. Subsequent phagosome maturation may lead to killing of some of the organisms. However, in numerous experiments we have observed the presence of apparently dormant B. anthracis spores residing in phagosomes within macrophages of various origins. Such spores can be observed readily by confocal microscopy of RAW cells (24). The inherent ability of spores to withstand harsh conditions may help prevent their killing by AM. Delayed germination of B. anthracis spores, until transport to the lymph nodes, may facilitate their survival until a more favorable environment is encountered. Release from alveolar macrophages and subsequent germination within the lymph fluids might allow sufficient synthesis of LT and edema toxin, which may help overcome the bactericidal activity of circulating macrophages. This would further enhance survival, growth, and dissemination in an infected mammalian host. It would therefore be critical that antitoxin therapeutics be administered before LT disables the host innate immune response.
Acknowledgments
We thank Kathleen Kuehl for excellent help with electron micrograph studies and David Heath for critical reading of the manuscript.
This work was partially funded by DTRA-JSTO project B_X003_04_RD_B. This project was funded in whole or in part with funds from the National Cancer Institute, National Institutes of Health, under contract N01-CO-12400. This research was supported in part by the Developmental Therapeutics Program in the Division of Cancer Treatment and Diagnosis of the National Cancer Institute. K.C.B. is a recipient of National Research Council fellowships.
The contents of this paper do not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
Editor: V. J. DiRita
REFERENCES
- 1.Agrawal, A., J. Lingappa, S. H. Leppla, S. Agrawal, A. Jabbar, C. Quinn, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 424:329-334. [DOI] [PubMed] [Google Scholar]
- 2.Blander, J. M., and R. Medzhitov. 2004. Regulation of phagosome maturation by signals from Toll-like receptors. Science 304:1014-1018. [DOI] [PubMed] [Google Scholar]
- 3.Brittingham, K. C., G. Ruthel, R. G. Panchal, C. L. Fuller, W. J. Ribot, T. A. Hoover, H. A. Young, A. O. Anderson, and S. Bavari. 2005. Dendritic cells endocytose Bacillus anthracis spores: implications for anthrax pathogenesis. J. Immunol. 174:5545-5552. [DOI] [PubMed] [Google Scholar]
- 4.Erwin, J. L., L. M. DaSilva, S. Bavari, S. F. Little, A. M. Friedlander, and T. C. Chanh. 2001. Macrophage-derived cell lines do not express proinflammatory cytokines after exposure to Bacillus anthracis lethal toxin. Infect. Immun. 69:1175-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ezzell, J. W., Jr., and T. G. Abshire. 1992. Serum protease cleavage of Bacillus anthracis protective antigen. J. Gen. Microbiol. 138:543-549. [DOI] [PubMed] [Google Scholar]
- 6.Gibb, T. R., D. A. Norwood, Jr., N. Woollen, and E. A. Henchal. 2002. Viral replication and host gene expression in alveolar macrophages infected with ebola virus (Zaire strain). Clin. Diagn. Lab. Immunol. 9:19-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gimenez, A. P., Y. Z. Wu, M. Paya, C. Delclaux, L. Touqui, and P. L. Goossens. 2004. High bactericidal efficiency of type iia phospholipase A2 against Bacillus anthracis and inhibition of its secretion by the lethal toxin. J. Immunol. 173:521-530. [DOI] [PubMed] [Google Scholar]
- 8.Grinberg, L. M., F. A. Abramova, O. V. Yampolskaya, D. H. Walker, and J. H. Smith. 2001. Quantitative pathology of inhalational anthrax. I. Quantitative microscopic findings. Mod. Pathol. 14:482-495. [DOI] [PubMed] [Google Scholar]
- 9.Guidi-Rontani, C., M. Levy, H. Ohayon, and M. Mock. 2001. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 42:931-938. [DOI] [PubMed] [Google Scholar]
- 10.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 11.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivins, B. E., P. F. Fellows, and G. O. Nelson. 1994. Efficacy of a standard human anthrax vaccine against Bacillus anthracis spore challenge in guinea-pigs. Vaccine 12:872-874. [DOI] [PubMed] [Google Scholar]
- 13.Kassam, A., S. D. Der, and J. Mogridge. 2005. Differentiation of human monocytic cell lines confers susceptibility to Bacillus anthracis lethal toxin. Cell. Microbiol. 7:281-292. [DOI] [PubMed] [Google Scholar]
- 14.Kraal, G., E. Broug, J. F. V. Iwaarden, J. H. A. Persoons, and T. Thepen. 1997. The role of alveolar macrophages in pulmonary immune function, 1st ed. Marcel Dekker, Inc., New York, NY.
- 15.Lincon, R. E., D. R. Hodges, F. Klein, B. G. Mahlandt, W. I. Jones, B. W. Haines, M. A. Rhian, and J. S. Walker. 1965. Role of the lymphatics in the pathogenesis of anthrax. J. Infect. Dis. 115:481-494. [DOI] [PubMed] [Google Scholar]
- 16.Lyons, C. R., J. Lovchik, J. Hutt, M. F. Lipscomb, E. Wang, S. Heninger, L. Berliba, and K. Garrison. 2004. Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun. 72:4801-4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Millonig, G. 1961. Advantages of a phosphate buffer for OsO4 solutions in fixation. J. Appl. Phys. 32:1637. [Google Scholar]
- 18.Mosmann, T. 1983. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J. Immunol. Methods 65:55-63. [DOI] [PubMed] [Google Scholar]
- 19.Panchal, R. G., K. M. Halverson, W. Ribot, D. Lane, T. Kenny, T. G. Abshire, J. W. Ezzell, T. A. Hoover, B. Powell, S. Little, J. J. Kasianowicz, and S. Bavari. 2005. Purified Bacillus anthracis lethal toxin complex formed in vitro and during infection exhibits functional and biological activity. J. Biol. Chem. 280:10834-10839. [DOI] [PubMed] [Google Scholar]
- 20.Pellizzari, R., C. Guidi-Rontani, G. Vitale, M. Mock, and C. Montecucco. 1999. Anthrax lethal factor cleaves MKK3 in macrophages and inhibits the LPS/IFNgamma-induced release of NO and TNFalpha. FEBS Lett. 462:199-204. [DOI] [PubMed] [Google Scholar]
- 21.Pickering, A. K., M. Osorio, G. M. Lee, V. K. Grippe, M. Bray, and T. J. Merkel. 2004. Cytokine response to infection with Bacillus anthracis spores. Infect. Immun. 72:6382-6389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Popov, S. G., R. Villasmil, J. Bernardi, E. Grene, J. Cardwell, T. Popova, A. Wu, D. Alibek, C. Bailey, and K. Alibek. 2002. Effect of Bacillus anthracis lethal toxin on human peripheral blood mononuclear cells. FEBS Lett. 527:211-215. [DOI] [PubMed] [Google Scholar]
- 23.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 78:485-494. [Google Scholar]
- 24.Ruthel, G., W. J. Ribot, S. Bavari, and T. A. Hoover. 2004. Time-lapse confocal imaging of development of Bacillus anthracis in macrophages. J. Infect. Dis. 189:1313-1316. [DOI] [PubMed] [Google Scholar]
- 25.Shafa, F., B. J. Moberly, and P. Gerhardt. 1966. Cytological features of anthrax spores phagocytized in vitro by rabbit alveolar macrophages. J. Infect. Dis. 116:401-413. [DOI] [PubMed] [Google Scholar]
- 26.Welkos, S., A. Friedlander, S. Weeks, S. Little, and I. Mendelson. 2002. In-vitro characterisation of the phagocytosis and fate of anthrax spores in macrophages and the effects of anti-PA antibody. J. Med. Microbiol. 51:821-831. [DOI] [PubMed] [Google Scholar]
- 27.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51:795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]