Abstract
Mycobacterium tuberculosis causes a lymphatic vasculitis in the lungs of guinea pigs infected by a low-dose aerosol. This observation suggests that in addition to being a direct conduit from the lungs to the regional lymph nodes, pulmonary lymphatics are themselves sites of infection and could be the site of latent infection.
The pathogenesis of Mycobacterium tuberculosis infection in the guinea pig following aerosol exposure includes early extrapulmonary spread to draining pulmonary and mediastinal lymph nodes (10, 17). The Ghon primary complex in infected humans is a clinical entity that represents the initial site of pulmonary inflammation in combination with concurrent involvement of the draining lymph nodes. In a proportion of patients, tuberculosis reactivation is thought to originate from these primary lesions, which may have remained quiescent for years. The combination of host factors and pathogen adaptations that favor the development of latent infections in humans is poorly understood but can be aided by animal models, such as the guinea pig model, that closely reflect the naturally occurring human disease.
Guinea pigs experimentally infected with M. tuberculosis by aerosol have patterns of infection and extrapulmonary spread similar to those seen in humans (18, 19). The guinea pig is highly susceptible to infection with laboratory strains as well as human clinical isolates (2, 15). While the pattern and degree of extrapulmonary dissemination may vary according to the virulence of isolates or the level of protection conferred by vaccination, the pulmonary lymph nodes are consistently affected. In this study, we extend our previous observations in an attempt to further elucidate the role of pulmonary lymphatics in the dissemination of M. tuberculosis (3, 10).
Female outbred Hartley guinea pigs of 3 months to 1 year of age were purchased from Charles River Laboratories (North Wilmington, MA). M. tuberculosis H37Rv was grown from low-passage seed lots in Proskauer-Beck liquid medium containing 0.05% Tween 80 to early mid-log phase. Animals were exposed to M. tuberculosis in a Madison chamber aerosol generation device calibrated to deliver approximately 20 bacilli per animal from frozen stocks diluted in double-distilled sterile water.
The right caudal lung lobes from guinea pigs (n = 4 for each time point) were collected at the time of necropsy, on days 5, 15, 20, 30, and 60 following aerosol exposure to M. tuberculosis. Tissue sections were processed routinely for histological evaluation following 4% paraformaldehyde fixation. Briefly, 4- to 6-μm-thick paraffin sections were stained with hematoxylin and eosin (H&E) and examined using light microscopy. Photomicrographic data were obtained for individual animals representative of the challenge model.
Among the time intervals examined in this study, 15 days was the earliest time that M. tuberculosis-associated inflammatory lesions were seen. Inflammatory cell infiltrates were occasionally seen in the alveoli surrounding small bronchioles (1 to 2 mm) within the pulmonary parenchyma, but most lesions were seen within the perivascular and peribronchial connective tissue (Fig. 1). Early changes consisted of scattered accumulations of cells within the stroma (Fig. 1A) or within the walls of lymphatics (Fig. 1B and C) that became organized as the lesions progressed. By 20 days, lesions had expanded in size and showed the first evidence of intralesional necrosis (Fig. 2A) associated with granulocyte infiltrates. Inflammatory cell infiltrates within the walls of lymphatics became organized and began to fill lymphatic vessel lumens (Fig. 2A to C). Infiltrates were evident within perivascular and peribronchial lymphatics and formed parallel nodular lesions that associated with the walls of airways, arteries, arterioles, and veins and had begun to extend into the surrounding alveoli (Fig. 3 and 4). Organized inflammatory cell infiltrates partially occluded lymphatic lumens, resulting in mild segmental dilation by protein-rich fluid (Fig. 3B). Occasionally, lymphatic lumens were markedly dilated and contained circulating inflammatory cells similar to those seen within organized lung lesions (Fig. 3C).
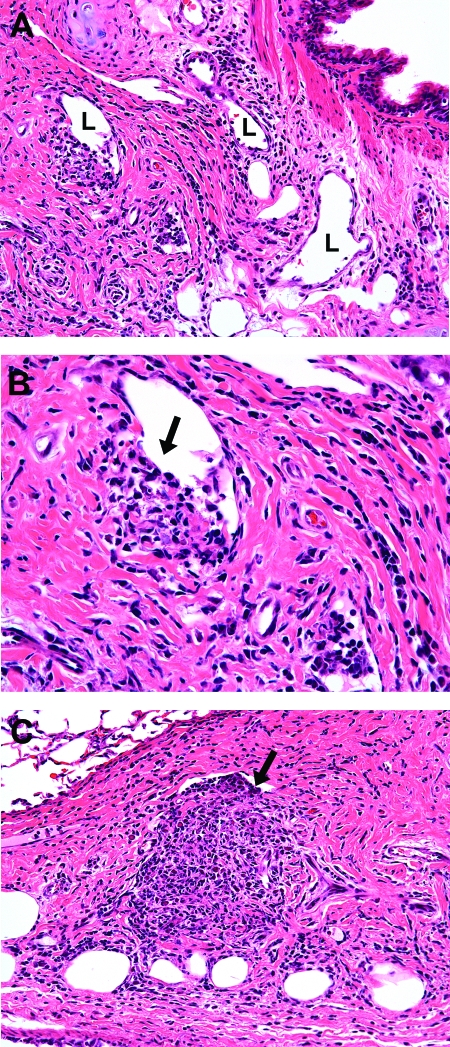
FIG. 1.
Photomicrographs of lungs of guinea pigs at 15 days postinfection with the H37Rv strain of M. tuberculosis. (A) Mixed inflammatory cells, including lymphocytes, macrophages, and granulocytes (heterophils and eosinophils), are present in the peribronchial connective tissue, which also contains variably sized lymphatic (L) vessels (magnification, ×200). (B) Small aggregates of inflammatory cells are present in the immediate perilymphatic connective tissue (arrow) and communicate with the lumen, which is partially devoid of endothelium (magnification, ×400). (C) A similar but larger accumulation of mixed inflammatory cells is present in the perilymphatic connective tissue that extends into the lymphatic lumen (arrow) (magnification, ×400). Tissues were stained with H&E.
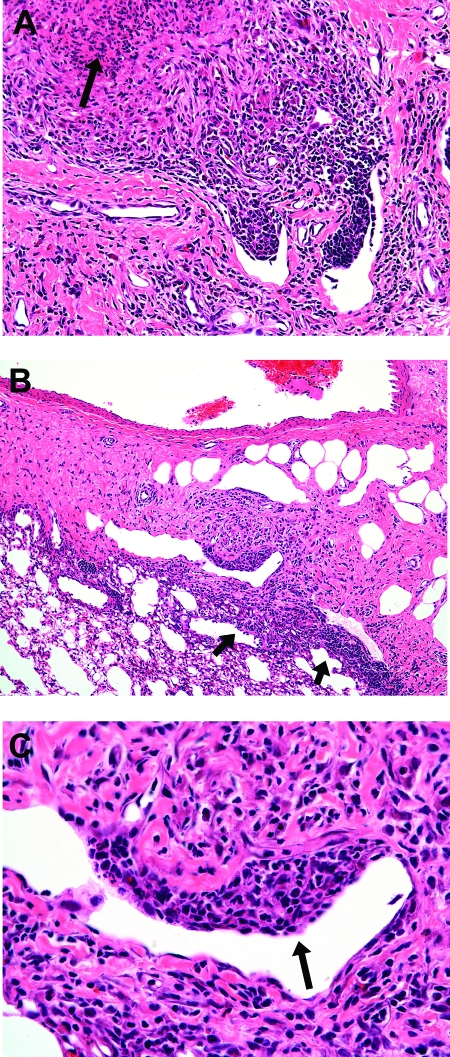
FIG. 2.
Photomicrographs of lungs of guinea pigs at 20 days postinfection with the H37Rv strain of M. tuberculosis. (A) Mixed inflammatory cells, including lymphocytes, macrophages, and granulocytes (heterophils and eosinophils), are present in the perilymphatic connective tissue, with early intralesional necrosis (arrow) and granulocyte infiltration (magnification, ×200). (B) Mixed inflammation extends from the periarterial and perilymphatic connective tissue and into the surrounding (arrows) pulmonary parenchyma (magnification, ×100). (C) Higher magnification of the field shown in panel B, demonstrating lymphangitis where the mixed inflammation infiltrates the wall (arrow) of a lymphatic vessel (magnification, ×400). Tissues were stained with H&E.
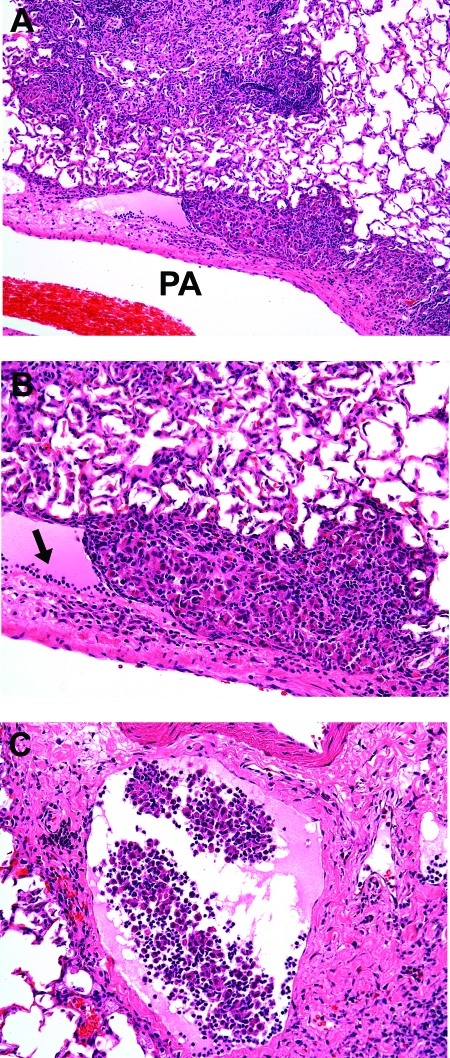
FIG. 3.
Photomicrographs of lungs of guinea pigs at 30 days postinfection with the H37Rv strain of M. tuberculosis. (A) Longitudinal section through a branch of a pulmonary artery (PA), showing parallel, nodular infiltrates of mixed inflammatory cells within the lumen of a periarterial lymphatic (lymphangitis), which is shown at a higher magnification in panel B (magnification, ×100). (B) Inflammatory cells occlude the lumen of a periarterial lymphatic that is distended with protein-rich acidophilic fluid and marginating (arrow) lymphocytes (magnification, ×400). (C) Markedly dilated periarterial lymphatic that contains circulating mixed inflammatory cells with no evidence of lymphangitis (magnification, ×200). Tissues were stained with H&E.
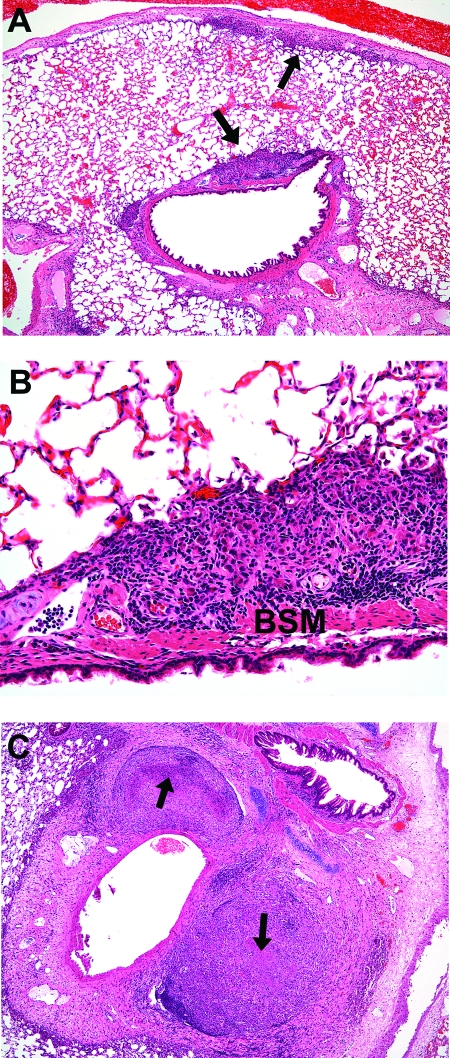
FIG. 4.
Photomicrographs of lungs of guinea pigs at 30 days postinfection with the H37Rv strain of M. tuberculosis. (A) Mixed inflammatory cells infiltrate the periarterial (small arrow) and peribronchial (large arrow) connective tissue, which is shown at a higher magnification in panel B (magnification, ×40). (B) Peribronchial mixed inflammation within the peribronchial lymphatics deep to the bronchial smooth muscle (BSM). There is minimal extension of inflammation into the surrounding alveoli of the pulmonary parenchyma (magnification, ×200). (C) Multiple well-organized lesions in the periarterial connective tissue of an immature animal. Margins are often sharply demarcated from the more loosely organized connective tissue stroma than that in mature animals. Lesions have extensive, coalescing foci (arrows) of central necrosis (magnification, ×40). Tissues were stained with H&E.
Immature guinea pigs (3 months of age) were similarly aerosol infected and euthanized when acute inflammation was maximal, at 30 days postinfection, to determine what effect age might have on the development of pulmonary lymphangitis. The perivascular and peribronchial connective tissue stroma in immature animals is less dense and more expansive than that in adult animals (Fig. 4C). Similar but more advanced lesions developed in immature animals than those in adult animals by 30 days postinfection. Lymphangiocentric lesions increased in size and progressed to necrosis by 30 days, in contrast to the 30 to 60 days seen in adult animals. In addition, lesions were well delineated and closely followed the contours of pulmonary arteries, corresponding to the anatomic localization of lymphatics (Fig. 4C). Progression of the lymphatic lesions was evident by the resolution of acute inflammation, central necrosis, fibrosis, and dystrophic mineralization of necrotic debris (Fig. 5).
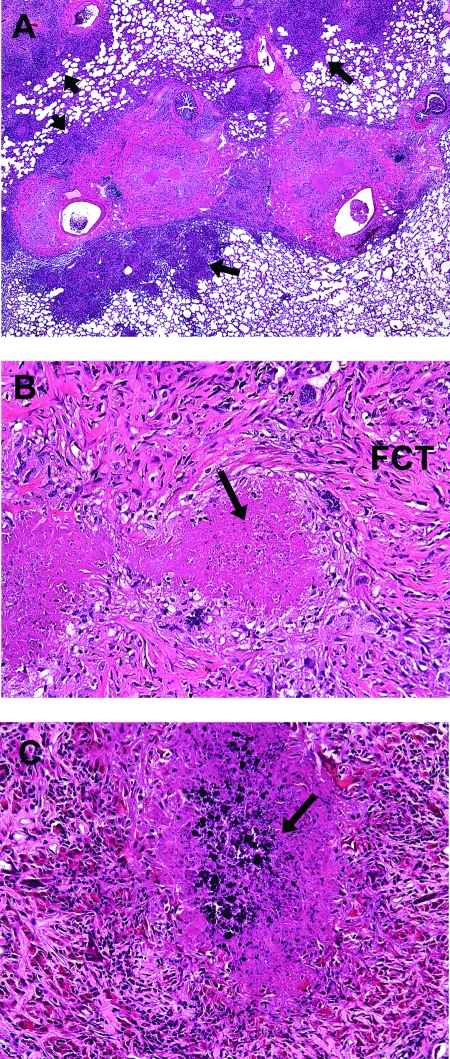
FIG. 5.
Photomicrographs of lungs of guinea pigs at 60 days postinfection with the H37Rv strain of M. tuberculosis. (A) Multiple lesions in the periarterial connective tissue coalesce within the connective tissue stroma and are continuous with inflammatory lesions that extend into the surrounding alveoli (arrows) of the pulmonary parenchyma (magnification, ×20). (B) Higher-magnification image of that shown in panel A, showing central necrosis (arrow) with resolving inflammation which is replaced by fibrous connective tissue (FCT) (magnification, ×200). (C) More advanced periarterial lesions show evidence of early mineralization (arrow) of the central necrosis (magnification, ×200). Tissues were stained with H&E.
Here we show that one of the earliest lesions in the lungs of guinea pigs infected with M. tuberculosis is inflammation of the pulmonary lymphatic vessels. Pulmonary lymphangitis developed between 5 and 15 days postinfection as foci of inflammation formed within the connective tissue stroma that supports main lymphatic vessels as well as in the alveoli of the subpleural and deep pulmonary parenchyma. Perilymphatic inflammation organized within the vessel walls and extended into lumens, forming linear segments of granulomatous inflammation that followed the contours of normal lymphatics in the peribronchial and perivascular stroma. Lymphangiocentric lesions progressed similarly to parenchymal lesions, resulting in central necrosis that coincided with the infiltration of granulocytes. Fibroblast infiltration with fibroplasia and dystrophic mineralization accompanied the resolution of acute inflammation in the chronic stages of infection.
Pulmonary lymphatics provide a direct route for the spread of M. tuberculosis from the initial site of infection in the lung to the draining lymph nodes, where the acquired immune response is initiated (4, 23). The findings in our current study suggest that the lymphatic vessels themselves develop progressive inflammation as part of the primary infection. The bacilli seed draining lymph nodes within the first days of infection, but evidence of a progressive infection of pulmonary lymph nodes in the guinea pig low-dose aerosol model does not become evident until the first 1 to 2 weeks postinfection (1, 3, 22). In humans, this combination of lung and lymph node lesions is referred to clinically as the Ghon primary complex. In susceptible hosts, such as children and immunocompromised individuals, both lung and lymph node lesions can progress rapidly, with the lymph nodes representing the first of multiple sites of extrapulmonary spread (2, 12, 14, 20). Disseminated tuberculosis is common in children, initially presenting as lymphadenopathy and progressing to potentially debilitating or life-threatening meningitis, osteomyelitis, or miliary tuberculosis (14, 20).
The recognition of pulmonary lymphatic involvement, as demonstrated in this study, is important in understanding the first phase of extrapulmonary dissemination. One of the advantages of the guinea pig model of tuberculosis is that the granulomatous lesions in the lung and elsewhere resemble those of humans and show a pattern of progression that correlates with lesion age (24). Primary lesions start as foci of acute mixed inflammation that progress to central necrosis, fibrosis, and mineralization in the more chronic stages of infection. Necrosis is an important feature that may facilitate M. tuberculosis dissemination and often corresponds to the infiltration of polymorphonuclear leukocytes (6, 10, 21, 24).
The lymphangiocentric lesions observed here had a pattern of progression that is similar to and characteristic of that of primary parenchymal lesions. The significance of this observation may be that early lung infection becomes established in a site that affords some degree of protection for both the host and the microbe, similar to other primary lung lesions (5). The development and maintenance of a fibrous capsule in the primary lesion are thought to be important features of the tuberculosis granuloma that is responsible for containing a localized infection (5). However, the major pulmonary lymphatic vessels are deeply embedded in the preexisting perivascular and peribronchial stroma, which is composed of dense fibrous connective tissue (8, 13). The development of lesions within preexisting connective tissue enables bacilli to become established rapidly within a privileged site protected from the peripheral circulation and, thus, host defenses.
Immature guinea pigs normally have loosely organized and less dense perivascular and peribronchial connective tissue stromata than those of mature animals. We compared lesions at 30 days postinfection from animals of 3 and 12 months of age to determine if this structural difference would influence lesion development. A difference in the rate and extent of lymphangiocentric lesion development was seen between immature and mature animals. The more rapid increase in size and progression of lesions within lymphatics in immature animals may be related to the less organized perivascular stroma allowing for uninhibited lesion expansion. This may explain, in part, the age-associated difference in disease severity and propensity for dissemination of M. tuberculosis (11).
Our present studies corroborate observations first made by pathologists in the mid- to late 1800s, at a time before the etiologic agent of tuberculosis was identified. In a model referred to as artificial tuberculosis (7, 8, 9, 16), guinea pigs inoculated subcutaneously with exudate obtained from naturally occurring human cases of tuberculosis developed disseminated pulmonary and extrapulmonary lesions. Detailed microscopic observations revealed that early lesions developed in the perivascular and peribronchiolar connective tissue corresponding to pulmonary lymphatics. Enlargement of lymph nodes, with inflammatory lesions near the site of inoculation or those associated with the lung, was a consistent finding. These early observations have not been maintained in the current literature but warrant further investigation using modern concepts and methodologies.
Future studies are needed to elucidate how M. tuberculosis penetrates the lymphatic vessels of the lung and its potential interactions with the lymphatic endothelium. Pulmonary lymphatics that are occluded as a result of primary infection may be favorable sites for the establishment of latent tuberculosis, preventing the further influx of effecter or memory immune cells or preventing chemotherapeutic agents from reaching inhibitory concentrations.
Acknowledgments
This work was supported by National Institutes of Health grant AI-054697.
We thank Susan L. Kraft, Helle Bielefeldt-Ohmann, and Mary Ann DeGroote for valuable discussions and critical reviews of the manuscript.
Editor: J. L. Flynn
REFERENCES
- 1.Abadie, V., E. Badell, P. Douillard, D. Ensergueix, P. J. Leenen, M. Tanguy, L. Fiette, S. Saeland, B. Gicquel, and N. Winter. 2005. Neutrophils rapidly migrate via lymphatics after Mycobacterium bovis BCG intradermal vaccination and shuttle live bacilli to the draining lymph nodes. Blood 106:1843-1850. [DOI] [PubMed] [Google Scholar]
- 2.Balasubramanian, V., E. H. Wiegeshaus, and D. W. Smith. 1992. Growth characteristics of recent sputum isolates of Mycobacterium tuberculosis in guinea pigs infected by the respiratory route. Infect. Immun. 60:4762-4767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basaraba, R. J., D. D. Dailey, C. T. McFarland, C. A. Shanley, E. E. Smith, D. N. McMurray, and I. M. Orme. 2006. Lymphadenitis as a major element of disease in the guinea pig model of tuberculosis. Tuberculosis (Edinburgh) [Epub ahead of print.] [DOI] [PubMed]
- 4.Chackerian, A. A., J. M. Alt, T. V. Perera, C. C. Dascher, and S. M. Behar. 2002. Dissemination of Mycobacterium tuberculosis is influenced by host factors and precedes the initiation of T-cell immunity. Infect. Immun. 70:4501-4509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dheda, K., H. Booth, J. F. Huggett, M. A. Johnson, A. Zumla, and G. A. Rook. 2005. Lung remodeling in pulmonary tuberculosis. J. Infect. Dis. 192:1201-1209. [DOI] [PubMed] [Google Scholar]
- 6.Dobos, K. M., E. A. Spotts, F. D. Quinn, and C. H. King. 2000. Necrosis of lung epithelial cells during infection with Mycobacterium tuberculosis is preceded by cell permeation. Infect. Immun. 68:6300-6310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox, W. 1868. On the artificial production of tubercle in the lower animals. MacMillan and Co., London, United Kingdom.
- 8.Klein, E. E. 1875. The anatomy of the lymphatic system, vol. II. The lung. Smith, Elder, & Co., London, United Kingdom.
- 9.Klein, E. E. 1874. Contributions to the normal and pathological anatomy of the lymphatic system of the lungs. Proc. R. Soc. London 22:133-145. [Google Scholar]
- 10.Kraft, S. L., D. Dailey, M. Kovach, K. L. Stasiak, J. Bennett, C. T. McFarland, D. N. McMurray, A. A. Izzo, I. M. Orme, and R. J. Basaraba. 2004. Magnetic resonance imaging of pulmonary lesions in guinea pigs infected with Mycobacterium tuberculosis. Infect. Immun. 72:5963-5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandalakas, A. M., and J. R. Starke. 2005. Current concepts of childhood tuberculosis. Semin. Pediatr. Infect. Dis. 16:93-104. [DOI] [PubMed] [Google Scholar]
- 12.Marais, B. J., R. P. Gie, H. S. Schaaf, A. C. Hesseling, C. C. Obihara, J. J. Starke, D. A. Enarson, P. R. Donald, and N. Beyers. 2004. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int. J. Tuberc. Lung Dis. 8:392-402. [PubMed] [Google Scholar]
- 13.Okada, Y. 1989. Lymphatic system of the human lung. Kinpodo Publishing, Kyoto, Japan.
- 14.Pineda, P. R., A. Leung, N. L. Muller, E. A. Allen, W. A. Black, and J. M. FitzGerald. 1993. Intrathoracic paediatric tuberculosis: a report of 202 cases. Tuber. Lung Dis. 74:261-266. [DOI] [PubMed] [Google Scholar]
- 15.Ratcliffe, H. L., and V. S. Palladino. 1953. Tuberculosis induced by droplet nuclei infection; initial homogeneous response of small mammals (rats, mice, guinea pigs, and hamsters) to human and to bovine bacilli, and the rate and pattern of tubercle development. J. Exp. Med. 97:61-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanderson, J. B. 1867. On the communicability of tubercle by innoculation, p. 11-151. In Tenth report of the Medical Officer of the Privy Council, vol. 6. George E. Eyre and William Spottiswoode, London, England. [Google Scholar]
- 17.Smith, D. W., D. N. McMurray, E. H. Wiegeshaus, A. A. Grover, and G. E. Harding. 1970. Host-parasite relationships in experimental airborne tuberculosis. IV. Early events in the course of infection in vaccinated and nonvaccinated guinea pigs. Am. Rev. Respir. Dis. 102:937-949. [DOI] [PubMed] [Google Scholar]
- 18.Smith, D. W., and G. E. Harding. 1977. Animal model of human disease. Pulmonary tuberculosis. Animal model: experimental airborne tuberculosis in the guinea pig. Am. J. Pathol. 89:273-276. [PMC free article] [PubMed] [Google Scholar]
- 19.Smith, D. W., and E. H. Wiegeshaus. 1989. What animal models can teach us about the pathogenesis of tuberculosis in humans. Rev. Infect. Dis. 11(Suppl. 2):S385-S393. [DOI] [PubMed] [Google Scholar]
- 20.Starke, J. R., and K. T. Taylor-Watts. 1989. Tuberculosis in the pediatric population of Houston, Texas. Pediatrics 84:28-35. [PubMed] [Google Scholar]
- 21.Taylor, J. L., O. C. Turner, R. J. Basaraba, J. T. Belisle, K. Huygen, and I. M. Orme. 2003. Pulmonary necrosis resulting from DNA vaccination against tuberculosis. Infect. Immun. 71:2192-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teitelbaum, R., W. Schubert, L. Gunther, Y. Kress, F. Macaluso, J. W. Pollard, D. N. McMurray, and B. R. Bloom. 1999. The M cell as a portal of entry to the lung for the bacterial pathogen Mycobacterium tuberculosis. Immunity 10:641-650. [DOI] [PubMed] [Google Scholar]
- 23.Tian, T., J. Woodworth, M. Skold, and S. M. Behar. 2005. In vivo depletion of CD11c+ cells delays the CD4+ T cell response to Mycobacterium tuberculosis and exacerbates the outcome of infection. J. Immunol. 175:3268-3272. [DOI] [PubMed] [Google Scholar]
- 24.Turner, O. C., R. J. Basaraba, and I. M. Orme. 2003. Immunopathogenesis of pulmonary granulomas in the guinea pig after infection with Mycobacterium tuberculosis. Infect. Immun. 71:864-871. [DOI] [PMC free article] [PubMed] [Google Scholar]