Abstract
The virulence of the pathogenic Yersinia species depends on a plasmid-encoded type III secretion system that transfers six Yop effector proteins into host cells. One of these proteins, YopJ, has been shown to disrupt host cell signaling pathways involved in proinflammatory cytokine production and to induce macrophage apoptosis in vitro. YopJ-dependent apoptosis in mesenteric lymph nodes has also been demonstrated in a mouse model of Yersinia pseudotuberculosis infection. These results suggest that YopJ attenuates the host innate and adaptive immune response during infection, but the role of YopJ during bubonic plague has not been completely established. We evaluated the role of Yersinia pestis YopJ in a rat model of bubonic plague following intradermal infection with a fully virulent Y. pestis strain and an isogenic yopJ mutant. Deletion of yopJ resulted in a twofold decrease in the number of apoptotic immune cells in the bubo and a threefold increase in serum tumor necrosis factor alpha levels but did not result in decreased virulence, systemic spread, or colonization levels in the spleen and blood. Our results indicate that YopJ is not essential for bubonic plague pathogenesis, even after peripheral inoculation of low doses of Y. pestis. Instead, the effects of YopJ appear to overlap and augment the immunomodulatory effects of other Y. pestis virulence factors.
The genus Yersinia includes three species that are pathogenic for humans and animals. Yersinia enterocolitica and Yersinia pseudotuberculosis cause food-borne and waterborne enteric disease, and Yersinia pestis causes plague, which is usually transmitted by flea bites. All three species harbor very similar ∼70-kb virulence plasmids that encode a type III secretion system (TTSS), which functions to transport virulence proteins called Yops (Yersinia outer proteins) into eukaryotic cells (6). The six translocated Yop effector proteins (YopH, YopM, YopT, YopE, YpkA/YopO, and YopJ) interfere with mammalian cell signaling pathways, which inhibits phagocytosis, modulates cytokine production, and induces apoptosis (4, 16, 29). Current models of Yersinia pathogenesis postulate that the cumulative effect of the Yops and other proteins secreted by the TTSS attenuate the innate and adaptive immune responses (2, 5, 16, 29).
The plasmid-encoded TTSS is required for virulence of all three pathogenic Yersinia species (28), and biochemical functions of each of the effector Yops have been determined (for reviews see references 4, 16, and 29). However, the individual roles of the Yops during different stages of infection have not been completely established. For full virulence in mice, all three Yersinia pathogens require both YopH and YopE, and Y. pestis and Y. enterocolitica require YopM (the role of YopM has not been determined yet for Y. pseudotuberculosis); however, loss of YopT has no effect on Y. enterocolitica virulence (this has not been tested yet for the other two species) (10, 11, 26, 27). Conflicting results have been reported for the effects of YpkA/YopO and YopJ on virulence. For example, loss of YopJ (called YopP in Y. enterocolitica) had no effect on Y. pseudotuberculosis infectivity in one study (9) but resulted in a 64-fold increase in the 50% lethal dose (LD50) in another study (14). A Y. enterocolitica YopJ mutant was less infective after oral or intravenous challenge (27). In Y. pestis, insertional inactivation of yopJ increased the LD50 only 1.2- to 1.5-fold in a septicemic plague model that included direct intravenous injection of an attenuated strain (25, 26).
YopJ has several biochemical functions that are predicted to impair the normal mammalian immune response to infection. YopJ is a deubiquinating cysteine protease that blocks activation of members of the mitogen-activated protein kinase family, including MKK and IKKβ, thereby altering normal cytokine production and host cell survival pathways (1, 12, 17, 19, 22, 23, 33). These biochemical activities inhibit production of the proinflammatory cytokines tumor necrosis factor alpha (TNF-α) and interleukin 8 and induce macrophage apoptosis in vitro (13, 15, 23, 32). To determine whether these immunomodulatory activities occur in vivo and their role in the pathogenesis of plague, we deleted yopJ from the fully virulent Y. pestis 195/P strain and assessed the virulence of the resulting mutant after intradermal (ID) inoculation in a rat model of bubonic plague.
MATERIALS AND METHODS
Construction of a Y. pestis yopJ mutant.
An in-frame yopJ mutant of Y. pestis 195/P was constructed by allelic exchange mutagenesis. A 2-kb region encompassing the entire 867-bp yopJ coding sequence and upstream and downstream flanking regions was PCR amplified using primers YopJ1 (5′-caggaggtatcggagtttac-3′) and YopJ2 (5′-gatcagcgatgagatgtctg-3′) and cloned in pCRII-Topo (Invitrogen, Carlsbad, CA). Inverse PCR of the resulting plasmid with primers YopJ3 (5′-cagggaattaacagcggtat-3′) and YopJ4 (5′-ggaattatcagtttcggtac-3′) and religation yielded pCRII-Topo containing the yopJ sequence with an 803-bp internal deletion. The ΔyopJ allele was then subcloned into the suicide vector pCVD442 (7), which was transformed into Escherichia coli S17-1λpir. The yopJ deletion was introduced into the Y. pestis 195/P strain by conjugation and allelic exchange (7). The 803-bp internal deletion of yopJ in the Y. pestis ΔyopJ strain was verified by PCR and by Western blotting with a mouse anti-YopJ monoclonal antibody (data not shown).
Infection of rats and virulence testing.
Wild-type Y. pestis 195/P and the isogenic ΔyopJ mutant were cultured overnight in brain heart infusion broth at 21°C, quantified by Petroff-Hausser direct counting, and diluted in phosphate-buffered saline (PBS) (pH 7.4). The numbers of Y. pestis CFU in the dilutions were checked by plating samples on Yersinia selective agar (Difco).
Groups of 10 8-week-old female Brown Norway rats (Charles River Laboratories, Wilmington, MA) were inoculated intradermally with 50 μl of PBS containing ∼1, 10, 100, or 1,000 CFU in the left upper anterior thigh. When signs of terminal plague sepsis appeared (roughcast fur, watery eyes, tachypnea, hunched posture, reluctance to move, and limping of the hind leg adjacent to the bubo [24]), rats were euthanized, and the inguinal lymph node (ILN) proximal to the injection site, spleen, and heart blood were aseptically collected. Spleens were weighed and bisected; one half of each spleen was then formalin fixed, and the other half was triturated in PBS. Triturated spleen tissue and 50 μl of whole blood were diluted in PBS and plated on Yersinia selective agar to count CFU. The remaining whole blood was allowed to coagulate to obtain serum. All experiments were performed at biosafety level 3 and were approved by the NIH NIAID Rocky Mountain Laboratories biosafety and animal care and use committees in accordance with National Institutes of Health guidelines.
Histology and immunohistochemistry.
Formalin-fixed spleen and ILN samples were embedded in paraffin, sectioned, and stained with hematoxylin and eosin. Apoptotic cells in additional ILN sections were detected by immunohistochemical staining using anti-caspase-3 polyclonal antibody CP229B (BioCare Medical, Concord, CA) (24). Caspase-positive cells in 20 random nonoverlapping microscopic fields (magnification, ×1,000) were counted for ILN sections from seven rats infected with wild-type Y. pestis, eight rats infected with ΔyopJ Y. pestis, and four uninfected negative control rats.
Serum TNF-α assay.
The TNF-α concentration in each serum sample collected at the terminal stage of disease was determined by enzyme-linked immunosorbent assays using a rat BD OptEIA set (BD Biosciences, San Diego, CA) (24).
Statistical analysis.
The LD50 was calculated by using the Reed-Muench equation, and differences in percentages of survival were evaluated by the log rank test. Correlations between infectious dose, time to terminal disease, bacterial loads in the spleen and blood, serum TNF-α level, and the number of ILN caspase-3-positive cells were calculated by using linear regression and the Pearson correlation. Differences between the mean numbers of ILN caspase-3-positive cells and serum TNF-α levels of rats infected with the two Y. pestis strains were evaluated by a two-tailed t test; a P value of <0.05 was considered statistically significant.
RESULTS AND DISCUSSION
Y. pestis yopJ mutant is fully virulent in a rat model of bubonic plague.
In the Brown Norway rat, intradermal injection of Y. pestis leads to bubonic plague (24). Within 72 h, the bacteria disseminate from the ID injection site through afferent lymphatic vessels to the regional draining lymph nodes. Y. pestis multiplies rapidly in a lymph node and produces severe lymphadenitis, which is characterized by extensive necrosis, hemorrhage, fibrin deposition, and large masses of densely packed extracellular bacteria throughout the node, associated with an edematous, hemorrhagic periadenitis (24). The enlarged infected lymph node is referred to as a bubo, and the same histopathology is seen in human bubonic plague (3). Systemic spread from the bubo leads to septicemic plague, which is characterized by high-density bacteremia and colonization of the spleen, liver, and other tissues.
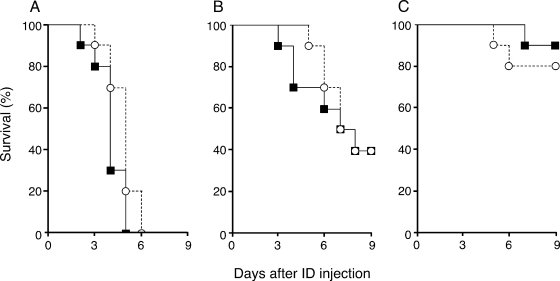
To evaluate the effect of YopJ on the different stages and kinetics of the progression of bubonic plague, which may also include an initial intracellular stage in dermal phagocytes (20), we infected rats with a fully virulent Y. pestis strain and with the isogenic ΔyopJ mutant. The LD50 of both strains following ID injection was <10 CFU (Fig. 1). The survival rate, the time to terminal disease, and the progression of the clinical signs of plague were also the same for rats infected with the wild-type strain and rats infected with the mutant. The median times to terminal disease for rats infected with 100 CFU of the wild type and rats infected with 100 CFU of ΔyopJ Y. pestis were 4 and 5 days, respectively, and the maximum survival time was 6 days (Fig. 1A). The survival curves for rats infected with 100 or 1,000 CFU of the strains did not differ significantly. At a lower ID inoculation dose (10 CFU), 60% of the rats infected with either the wild-type or ΔyopJ strain developed plague, and the median time to terminal disease was 7.5 days (Fig. 1B). For each of the four infectious doses, the differences in incidence and the time to terminal disease between rats infected with the yopJ mutant and rats infected with the wild-type parent strain were not significant (P > 0.05). These results showed that yopJ is dispensable during all stages of the development of bubonic and septicemic plague.
FIG. 1.
Incidence of terminal plague in Brown Norway rats following intradermal injection of 100 CFU (A), 10 CFU (B), or ∼1 CFU (C) of wild-type (solid squares) or ΔyopJ (open circles) Y. pestis. The calculated LD50 of both strains is <10 CFU.
In previous studies of the role of YopJ in Y. pestis pathogenesis the workers used attenuated strains lacking the Yersinia high-pathogenicity island that is required for virulence when peripheral routes of infection are used (25, 26). Direct intravenous injection of these strains indicated that YopJ is not required for the development of fatal septicemic plague in mice, but the results did not address the role of YopJ during earlier disease stages when the normal intradermal route of infection was used. Our results corroborate and extend the results obtained with the septicemic plague model and establish that YopJ is not required for virulence regardless of the dose or the route of infection.
Loss of YopJ does not affect systemic spread, colonization, or histopathology of bubonic plague.
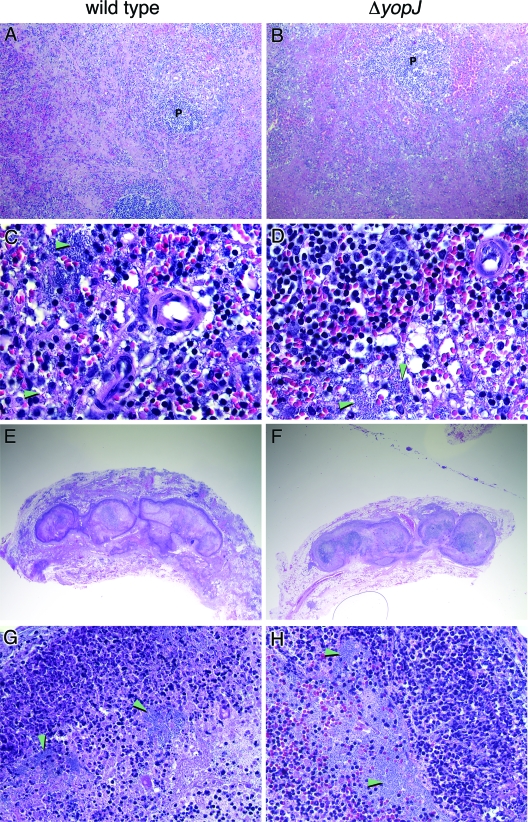
All rats that developed terminal plague with either the Y. pestis wild-type strain or the ΔyopJ strain had the same clinical signs, including a palpable enlarged inguinal bubo. After euthanasia, ILN and spleens were collected from all of these rats, and similar histopathologies were seen in both bubo and spleen tissue. The architecture of the ILN and spleen was markedly affected, and there were many large aggregates of extracellular bacteria and associated necrosis (Fig. 2). The bacterial loads in the spleen and blood were also similar (Fig. 3). Although the time to terminal disease was indirectly correlated with the initial ID injection dose (1, 10, or ≥100 CFU) (Fig. 1), the histopathologies of the bubo and the bacterial loads in the spleen and blood at the terminal stage of disease were equivalent for all rats, regardless of the strain or infectious dose (Fig. 2 and 3). The mean levels recovered were 108.2 CFU/g spleen for all wild-type infected rats and 107.8 CFU/g spleen for all ΔyopJ-infected rats. The mean bacteremia levels were 107.3 CFU/ml for rats infected with the wild-type strain and 106.2 for rats infected with the ΔyopJ mutant. The differences were not statistically significant (P = 0.37 and 0.09, respectively).
FIG. 2.
Identical histopathologies produced by wild-type and ΔyopJ Y. pestis. Hematoxylin-and-eosin-stained sections of spleens (A to D) and inguinal buboes (E to H) from rats infected with wild-type (left column) or ΔyopJ (right column) Y. pestis were examined. The arrowheads indicate large aggregates of extracellular bacteria. P, periarterial lymphatic sheath. Original magnifications, ×200 (A and B), ×600 (C and D), ×10 (E and F), and ×400 (G and H).
FIG. 3.
Colonization in the spleen (A) and blood (B) in rats inoculated intradermally with ∼1, 10, 100, or 1,000 CFU wild-type Y. pestis (solid circles) or ΔyopJ Y. pestis (open circles). Each symbol indicates the bacterial load in a single rat at the terminal stage of plague; the horizontal lines indicate the mean log CFU per gram of spleen or milliliter of blood.
Y. pestis YopJ contributes to apoptosis and suppresses TNF-α induction during bubonic plague.
Because YopJ appeared to have no effect on disease progression, virulence, histopathology, or systemic spread and tissue colonization, we sought evidence for two of its predicted functions, apoptosis of immune cells in the lymph node and suppression of the normal TNF-α response, during bubonic plague.
At the terminal stage of disease, the mean number of apoptotic cells in the bubo was two- to threefold higher in rats infected with wild-type Y. pestis than in rats infected with the ΔyopJ mutant (P < 0.0001) (Table 1). However, the number of apoptotic cells in ΔyopJ-infected rats was significantly higher than the background level (<1 caspase-positive cell/field) in the ILN of uninfected controls. Thus, the biochemical activities of YopJ augment apoptosis of lymph node cells during bubonic plague but are not solely responsible for it.
TABLE 1.
Effect of Y. pestis YopJ on apoptosis in the bubo
| Rat | Bacterial load ina:
|
No. of apoptotic cells/fielda | |
|---|---|---|---|
| Blood (log CFU/ml) | Spleen (log CFU/g) | ||
| Rats infected with Y. pestis wild type | |||
| 1 | 6.1 | 6.5 | 15.4 |
| 2 | NDb | ND | 15.4 |
| 3 | ND | 9.3 | 14.4 |
| 4 | 8.6 | 9.5 | 21.2 |
| 5 | 8.7 | 9.8 | 20.0 |
| 6 | 9.0 | 9.4 | 19.2 |
| 7 | 9.3 | 9.0 | 16.6 |
| Mean ± SD | 17.5 ± 2.6 | ||
| Rats infected with Y. pestis ΔyopJ | |||
| 1 | 5.0 | ND | 7.5 |
| 2 | ND | 7.1 | 5.4 |
| 3 | ND | 7.8 | 4.6 |
| 4 | ND | 8.3 | 8.6 |
| 5 | ND | 8.8 | 8.9 |
| 6 | 8.2 | 8.8 | 7.4 |
| 7 | ND | 9.1 | 5.9 |
| 8 | ND | 9.2 | 5.7 |
| Mean ± SD | 6.8 ± 1.6c | ||
Mean number of caspase-positive cells in 20 random microscopic fields.
ND, not determined.
Statistically significantly different from the value for rats infected with Y. pestis wild type (P < 0.0001).
The ΔyopJ mutant was also defective in the ability to suppress host TNF-α production during infection. The mean serum TNF-α level in rats with terminal plague caused by the ΔyopJ mutant was significantly higher (P = 0.02) than the level in rats infected with the wild type (Table 2). The TNF-α levels in the rats infected with the wild type are consistent with the results of a previous study (24), in which serum TNF-α was detected only in the late septic stage of disease. Again, although the presence of YopJ reduced the TNF-α level threefold, production of this cytokine was not completely suppressed, since all four uninfected control rats had <40 pg/ml of serum. Additionally, there was no correlation between the numbers of CFU in the spleen or blood and the TNF-α levels or numbers of caspase-3-positive cells in rats infected with either wild-type or ΔyopJ Y. pestis (P > 0.3).
TABLE 2.
Effect of Y. pestis YopJ on TNF-α induction during bubonic plague
| Rat | Bacterial load ina:
|
TNF-α concn (pg/ml serum) | |
|---|---|---|---|
| Blood (log CFU/ml) | Spleen (log CFU/g) | ||
| Rats infected with Y. pestis wild type | |||
| 1 | 4.4 | 5.0 | 292 |
| 2 | 5.0 | 5.5 | <40 |
| 3 | 5.4 | 4.9 | 1,105 |
| 4 | 6.1 | 7.1 | <40 |
| 5 | 7.3 | 8.2 | 317 |
| 6 | 9.3 | 9.1 | 128 |
| Mean ± SD | 320 ± 403 | ||
| Rats infected with Y. pestis ΔyopJ | |||
| 1 | 3.4 | 5.5 | 623 |
| 2 | 4.2 | ND | 411 |
| 3 | 5.0 | ND | 1,537 |
| 4 | 5.0 | 5.7 | 2,277 |
| 5 | 6.5 | 8.0 | 1,026 |
| 6 | 7.7 | 8.9 | 1,453 |
| 7 | 9.2 | 9.3 | 681 |
| Mean ± SD | 1,144 ± 655b | ||
ND, not determined.
Statistically significantly different from the value for rats infected with Y. pestis wild type (P = 0.02).
Our results indicate that although YopJ contributes to apoptosis and suppression of TNF-α during bubonic plague, it is not necessary for normal plague pathogenesis in rats. In contrast, loss of yopJ in enteropathogenic Yersinia has been correlated with reduced bacterial persistence and virulence in mouse infection models. For example, Monack et al. showed that the number of cells of a Y. pseudotuberculosis yopJ mutant in the spleen decreased 100-fold by 3 days after oral infection, and the LD50 of this mutant was 64-fold higher than that of the parental strain (14). Similarly, a Y. enterocolitica yopP mutant was slightly attenuated in an oral infection model because it was less able to colonize the small intestine and Peyer's patches and to cause systemic disease (27). On the other hand, Galyov et al. reported that YopJ had no effect on Y. pseudotuberculosis virulence or spleen colonization (9). These conflicting results could have been due to the different oral challenge doses given or to unrecognized genetic differences between the yopJ mutants or mouse strains used.
Y. pestis causes apoptosis of immune cells in an infected bubo (24). Our results indicate that the activity of YopJ does not entirely account for this. To date, YopJ is the only Yop effector known to induce apoptosis. However, lipopolysaccharide activation of Toll-like receptor 4-dependent pathways may be the primary stimulus for apoptosis, and YopJ may have a contributory role, inhibiting antiapoptotic pathways (21, 30, 31). Likewise, YopJ modulated but did not eliminate TNF-α induction in vivo, as predicted from in vitro studies with Y. pseudotuberculosis and Y. enterocolitica yopJ/P mutants (1, 17, 18, 21, 23). Nevertheless, neither the decreased apoptosis in the bubo nor the increased serum TNF-α level generated by the ΔyopJ mutant was sufficient to significantly delay systemic infection and the onset of fatal disease in rats (Fig. 1). Thus, YopJ appears to have a synergistic but nonessential role in Y. pestis pathogenesis. As is the case for the multiple TTSS effectors of Salmonella, however, any one of which is often dispensable for virulence in a given animal model (8), the Y. pestis Yops may constitute a multifactorial system whose combined effects ensure productive infection in a range of hosts.
Acknowledgments
We thank David Erickson, Viveka Vadyvaloo, and Leigh Knodler for reviews of the manuscript. We also acknowledge Richard Siegel, NIH NIAMS, for his gift of an anti-YopJ monoclonal antibody.
This work was supported by the Division of Intramural Research, NIAID, NIH, and by the Ellison Medical Foundation (New Scholars Award in Global Infectious Diseases to B.J.H.).
Editor: J. B. Bliska
REFERENCES
- 1.Boland, A., and G. R. Cornelis. 1998. Role of YopP in suppression of tumor necrosis factor alpha release by macrophages during Yersinia infection. Infect. Immun. 66:1878-1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brubaker, R. R. 2003. Interleukin-10 and inhibition of innate immunity to yersiniae: roles of Yops and LcrV (V antigen). Infect. Immun. 71:3673-3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butler, T. 1983. Plague and other Yersinia infections. Plenum Press, New York, N.Y.
- 4.Cornelis, G. R. 2000. Molecular and cell biology aspects of plague. Proc. Natl. Acad. Sci. USA 97:8778-8783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornelis, G. R. 2002. Yersinia type III secretion: send in the effectors. J. Cell Biol. 158:401-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornelis, G. R., A. Boland, A. P. Boyd, C. Geuijen, M. Iriarte, C. Neyt, M. P. Sory, and I. Stainier. 1998. The virulence plasmid of Yersinia, an antihost genome. Microbiol. Mol. Biol. Rev. 62:1315-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnenberg, M. S., and J. B. Kaper. 1991. Construction of an eae deletion mutant of enteropathogenic Escherichia coli by using a positive-selection suicide vector. Infect. Immun. 59:4310-4317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fierer, J., and D. G. Guiney. 2001. Diverse virulence traits underlying different clinical outcomes of Salmonella infection. J. Clin. Investig. 107:775-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galyov, E. E., S. Hakansson, and H. Wolf-Watz. 1994. Characterization of the operon encoding the YpkA Ser/Thr protein kinase and the YopJ protein of Yersinia pseudotuberculosis. J. Bacteriol. 176:4543-4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kerschen, E. J., D. A. Cohen, A. M. Kaplan, and S. C. Straley. 2004. The plague virulence protein YopM targets the innate immune response by causing a global depletion of NK cells. Infect. Immun. 72:4589-4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logsdon, L. K., and J. Mecsas. 2003. Requirement of the Yersinia pseudotuberculosis effectors YopH and YopE in colonization and persistence in intestinal and lymph tissues. Infect. Immun. 71:4595-4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meijer, L. K., K. Schesser, H. Wolf-Watz, P. Sassone-Corsi, and S. Pettersson. 2000. The bacterial protein YopJ abrogates multiple signal transduction pathways that converge on the transcription factor CREB. Cell. Microbiol. 2:231-238. [DOI] [PubMed] [Google Scholar]
- 13.Mills, S. D., A. Boland, M. P. Sory, P. van der Smissen, C. Kerbourch, B. B. Finlay, and G. R. Cornelis. 1997. Yersinia enterocolitica induces apoptosis in macrophages by a process requiring functional type III secretion and translocation mechanisms and involving YopP, presumably acting as an effector protein. Proc. Natl. Acad. Sci. USA 94:12638-12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monack, D. M., J. Mecsas, D. Bouley, and S. Falkow. 1998. Yersinia-induced apoptosis in vivo aids in the establishment of a systemic infection of mice. J. Exp. Med. 188:2127-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monack, D. M., J. Mecsas, N. Ghori, and S. Falkow. 1997. Yersinia signals macrophages to undergo apoptosis and YopJ is necessary for this cell death. Proc. Natl. Acad. Sci. USA 94:10385-10390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Navarro, L., N. M. Alto, and J. E. Dixon. 2005. Functions of the Yersinia effector proteins in inhibiting host immune responses. Curr. Opin. Microbiol. 8:21-27. [DOI] [PubMed] [Google Scholar]
- 17.Orth, K., Z. Xu, M. B. Mudgett, Z. Q. Bao, L. E. Palmer, J. B. Bliska, W. F. Mangel, B. Staskawicz, and J. E. Dixon. 2000. Disruption of signaling by Yersinia effector YopJ, a ubiquitin-like protein protease. Science 290:1594-1597. [DOI] [PubMed] [Google Scholar]
- 18.Palmer, L. E., S. Hobbie, J. E. Galan, and J. B. Bliska. 1998. YopJ of Yersinia pseudotuberculosis is required for the inhibition of macrophage TNF-alpha production and downregulation of the MAP kinases p38 and JNK. Mol. Microbiol. 27:953-965. [DOI] [PubMed] [Google Scholar]
- 19.Palmer, L. E., A. R. Pancetti, S. Greenberg, and J. B. Bliska. 1999. YopJ of Yersinia spp. is sufficient to cause downregulation of multiple mitogen-activated protein kinases in eukaryotic cells. Infect. Immun. 67:708-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pujol, C., and J. B. Bliska. 2005. Turning Yersinia pathogenesis outside in: subversion of macrophage function by intracellular yersiniae. Clin. Immunol. 114:216-226. [DOI] [PubMed] [Google Scholar]
- 21.Ruckdeschel, K., S. Harb, A. Roggenkamp, M. Hornef, R. Zumbihl, S. Kohler, J. Heesemann, and B. Rouot. 1998. Yersinia enterocolitica impairs activation of transcription factor NF-κB: involvement in the induction of programmed cell death and in the suppression of the macrophage tumor necrosis factor alpha production. J. Exp. Med. 187:1069-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruckdeschel, K., J. Machold, A. Roggenkamp, S. Schubert, J. Pierre, R. Zumbihl, J. P. Liautard, J. Heesemann, and B. Rouot. 1997. Yersinia enterocolitica promotes deactivation of macrophage mitogen-activated protein kinases extracellular signal-regulated kinase-1/2, p38, and c-Jun NH2-terminal kinase. Correlation with its inhibitory effect on tumor necrosis factor-alpha production. J. Biol. Chem. 272:15920-15927. [DOI] [PubMed] [Google Scholar]
- 23.Schesser, K., A. K. Spiik, J. M. Dukuzumuremyi, M. F. Neurath, S. Pettersson, and H. Wolf-Watz. 1998. The yopJ locus is required for Yersinia-mediated inhibition of NF-κB activation and cytokine expression: YopJ contains a eukaryotic SH2-like domain that is essential for its repressive activity. Mol. Microbiol. 28:1067-1079. [DOI] [PubMed] [Google Scholar]
- 24.Sebbane, F., D. Gardner, D. Long, B. B. Gowen, and B. J. Hinnebusch. 2005. Kinetics of disease progression and host response in a rat model of bubonic plague. Am. J. Pathol. 166:1427-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Straley, S. C., and W. S. Bowmer. 1986. Virulence genes regulated at the transcriptional level by Ca2+ in Yersinia pestis include structural genes for outer membrane proteins. Infect. Immun. 51:445-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Straley, S. C., and M. L. Cibull. 1989. Differential clearance and host-pathogen interactions of YopE− and YopK− YopL− Yersinia pestis in BALB/c mice. Infect. Immun. 57:1200-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trülzsch, K., T. Sporleder, E. I. Igwe, H. Russmann, and J. Heesemann. 2004. Contribution of the major secreted Yops of Yersinia enterocolitica O:8 to pathogenicity in the mouse infection model. Infect. Immun. 72:5227-5234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Une, T., and R. R. Brubaker. 1984. In vivo comparison of avirulent Vwa− and Pgm− or Pstr phenotypes of yersiniae. Infect. Immun. 43:895-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viboud, G. I., and J. B. Bliska. 2005. Yersinia outer proteins: role in modulation of host cell signaling responses and pathogenesis. Annu. Rev. Microbiol. 59:69-89. [DOI] [PubMed] [Google Scholar]
- 30.Zhang, Y., and J. B. Bliska. 2005. Role of macrophage apoptosis in the pathogenesis of Yersinia. Curr. Top. Microbiol. Immunol. 289:151-173. [DOI] [PubMed] [Google Scholar]
- 31.Zhang, Y., and J. B. Bliska. 2003. Role of Toll-like receptor signaling in the apoptotic response of macrophages to Yersinia infection. Infect. Immun. 71:1513-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang, Y., A. T. Ting, K. B. Marcu, and J. B. Bliska. 2005. Inhibition of MAPK and NF-κB pathways is necessary for rapid apoptosis in macrophages infected with Yersinia. J. Immunol. 174:7939-7949. [DOI] [PubMed] [Google Scholar]
- 33.Zhou, H., D. M. Monack, N. Kayagaki, I. Wertz, J. Yin, B. Wolf, and V. M. Dixit. 2005. Yersinia virulence factor YopJ acts as a deubiquitinase to inhibit NF-kappa B activation. J. Exp. Med. 202:1327-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]