Abstract
Type III protein secretion systems, which are organelles with the capacity to deliver bacterial proteins into host cells, have been adapted to deliver heterologous antigens for vaccine development. A limitation of these antigen delivery systems is that some proteins are not amenable to secretion through this pathway. We show here that proteins from the simian and human immunodeficiency viruses that are not permissive for secretion through a Salmonella enterica serovar Typhimurium type III secretion system can be modified to travel this secretion pathway by introduction of discrete mutations. Proteins optimized for secretion were presented more efficiently via the major histocompatibility complex class I pathway and were able to induce a better immune response.
Avirulent strains of Salmonella enterica serovar Typhimurium are being considered as antigen delivery vectors for heterologous vaccine development (8, 19, 27, 40). The availability of several virulence-attenuating mutations and the ease with which Salmonella can be genetically manipulated, coupled with its intrinsic ability to stimulate the innate immune system, have made Salmonella a very promising platform for the construction of vaccines to protect against a variety of infectious diseases or even cancer. Thus, Salmonella vaccine strains endowed with the capacity to express heterologous antigens have been constructed and tested in a variety of animal models and human volunteers (3, 10, 19, 21, 33, 40, 45). A limitation in the use of Salmonella as a vaccine platform, however, has been its apparent inefficiency at stimulating major histocompatibility complex (MHC) class I-restricted CD8+ (cytotoxic) T-cell responses (18, 36, 47). This limitation is most likely due to some intrinsic properties of the intracellular lifestyle of Salmonella. During its intracellular stage, Salmonella remains within a membrane-bound compartment (13). Therefore, heterologous antigens expressed in Salmonella do not efficiently reach the cytosol and subsequently the proteosome, a prerequisite for efficient stimulation of CD8+ T-cell responses. Since efficient protection against some microorganisms (e.g., viral and certain parasitic and bacterial pathogens) requires this type of immune response, this limitation hampers the use of Salmonella as a “universal” vaccine platform.
We have used a Salmonella type III secretion system (TTSS) encoded in Salmonella pathogenicity island 1 (SPI-1) as an antigen delivery system to overcome this limitation (39). Type III protein secretion systems have the capacity to deliver into the host cell cytosol a battery of bacterial proteins that can modulate host cell functions to increase pathogen survival and replication (14). Proteins destined to travel in this secretion pathway possess discrete secretion signals that target them to the secretion machine and subsequently to host cells (7). When fused to heterologous proteins, these signals can mediate delivery into the cytosol of eukaryotic cells (42). We have adapted this system to construct avirulent S. enterica serovar Typhimurium strains expressing chimeric proteins consisting of the secretion and translocation signals of Salmonella type III secreted proteins (e.g., SopE or SptP) fused to different MHC class I epitopes from different pathogens (11, 39, 41). These strains were able to induce CD8+ T-cell responses directed to the heterologous proteins, which in some cases were able to confer protection in animal models of infection (11, 24, 39, 41).
Previous studies in which the TTSS was used as an antigen delivery vehicle were carried out with either discrete epitopes or small portions of the heterologous proteins fused to the type III secretion (TTS) signals (11, 24, 39, 41). However, efficient protection in most cases requires delivery of a larger repertoire of epitopes contained in larger polypeptides (8). Although size per se is not an impediment for type III secretion (proteins that are vastly different sizes can be secreted by this machine), it is clear that there are proteins or protein motifs that are not amenable to secretion through this pathway (1, 30). Since unfolding is a prerequisite for type III secretion, proteins with domains that have high intrinsic stability cannot be unfolded by the TTSS-associated ATPase and therefore cannot be secreted (1). Therefore, if such a domain was present within a polypeptide relevant for vaccine development, it would hamper its delivery via the type III secretion pathway. We have been using the S. enterica serovar Typhimurium SPI-1 TTSS to construct a vaccine against human immune deficiency virus (HIV) (11). Using the highly related simian immune deficiency virus (SIV) as a model, we have demonstrated that the S. enterica serovar Typhimurium SPI-1 TTSS can deliver a region of the viral Gag protein containing a MamuA-*01 epitope and prime mucosal antigen-specific CD8+ T-cell immune responses in inoculated rhesus macaques (11). However, construction of an effective HIV vaccine will require delivery of the entire Gag protein and presumably other viral proteins. In this paper, we describe construction of an S. enterica serovar Typhimurium vaccine strain that is capable of delivering via its SPI-1-TTSS the entire HIV and SIV Gag proteins, as well as a polypeptide made of sequences derived from the Rev, Tat, and Nef viral proteins. Construction of this strain required specific engineering of these viral proteins as the wild-type forms are not amenable to type III secretion. The strategy described in this study can be utilized to render any protein of interest permissive to type III secretion for vaccine construction.
MATERIALS AND METHODS
Bacterial strains and culture conditions.
The attenuated S. enterica serovar Typhimurium ΔphoP ΔphoQ (16) and Δasd (17) strains have been described previously and were grown in L broth containing 0.3 M sodium chloride at 37°C under conditions that stimulate expression of the SPI-1 TTSS (15). When required, ampicillin was added at a final concentration of 100 μg/ml. The growth characteristics of all strains used in these studies were indistinguishable.
Plasmid construction.
Plasmid constructs expressing fusions between the secretion and translocation signals of the SPI-1 TTSS effector protein SopE or SptP (28, 29) and different segments of the SIV or HIV-1 protein Gag, Rev, Tat, or Nef were constructed using standard recombinant DNA techniques in low-copy-number plasmid pWSK30 (46). The adenovirus epitope M45 (34) and the H-2b-restricted influenza virus nucleoprotein epitope NP366-374 (FluNP) (38) were included between the SopE and viral sequences to enable detection of the chimeric proteins and assaying of antigen presentation in murine reporter cells, respectively. In all cases, expression of the constructs was driven by the sopE promoter. Plasmids were introduced into the S. enterica serovar Typhimurium strains by electroporation.
Type III protein secretion assay.
Analysis of bacterial culture supernatant proteins was carried out by Western immunoblotting as previously described (25), using a monoclonal antibody that recognized the M45 epitope present in the different constructs.
Antigen presentation assay.
RMA cells (C57BL/6J mouse lymphoma) (9) were used as antigen-presenting cells (APCs) after infection with S. enterica serovar Typhimurium strains grown as described elsewhere (39). About 3 × 108 bacterial CFU was used to infect 107 APCs in 1 ml of Dulbecco's modified Eagle's medium at 37°C for 3 h. APCs subjected to the different procedures were washed, incubated for 1 h in Dulbecco's modified Eagle's medium containing gentamicin at a concentration of 100 μg/ml, and distributed in quadruplicate 100-μl cultures in 96-well plates containing 2 × 105 APCs each. Influenza NP-specific T-cell hybridoma 12.164 (2 × 105 cells) (9) was added to the treated RMA cell cultures. Culture medium was collected after incubation for 40 h at 37°C to determine the interleukin-2 (IL-2) concentration by a capture enzyme-linked immunosorbent assay (ELISA) (Pharmingen). Addition of the influenza NP peptide and addition of an irrelevant peptide from the lymphocytic choriomeningitis virus nucleoprotein (1 μM) served as positive and negative controls, respectively. All bacterial strains used in these studies invaded RMA cells at the same levels.
Animal immunization.
Groups of BALB/c female mice (eight mice per category) were fasted for 4 h before oral inoculation by stomach gavage of ∼108 ΔphoP ΔphoQ S. enterica serovar Typhimurium cells expressing wild-type or TTS-optimized HIV Gag fused to the secretion and translocation signals of SopE or carrying the vector control. Four weeks after the first inoculation, animals were boosted by administering intraperitoneally ∼104 Δasd S. enterica serovar Typhimurium cells carrying the same plasmids. The latter strain was used because it is severely attenuated and therefore can be administered intraperitoneally safely.
Measurement of Gag-specific CD8+ T-cell responses in vaccinated mice by tetramer staining and flow cytometric analysis.
Five days after boosting, immunized mice were sacrificed by CO2 intoxication, and the spleens were removed. Splenocytes were isolated by forcing the spleens through a metal strainer with a 1-mm2 mesh. Erythrocytes were lysed in buffer (pH 7.4) containing 0.15 M NH4Cl and 1 mM NaHCO3. Splenocytes were resuspended in phosphate-buffered saline containing 0.5% bovine serum albumin and 0.02% NaN3. Cells (∼5 × 106 cells) were placed in a V-bottom 96-well plate for staining with streptavidin-APC-conjugated tetramers (obtained from the National Institutes of Health MHC Tetramer Core Facility, Emory University Vaccine Center) directed to an MHC H-2Kd immunodominant Gag epitope (N-AMQMLKETI-C) (32) along with phycoerythrin-conjugated anti-CD62L and fluorescein isothiocyanate-conjugated anti-CD8a antibodies, using standard procedures. Stained cells were analyzed with a FACSCalibur flow cytometer (Becton-Dickinson, San Jose, Calif.), and the flow cyometric profile was analyzed using the FlowJo software (Tree Star, Inc., San Carlos, Calif.).
RESULTS AND DISCUSSION
Identification of regions of SIV and HIV Gag that interfere with type III secretion.
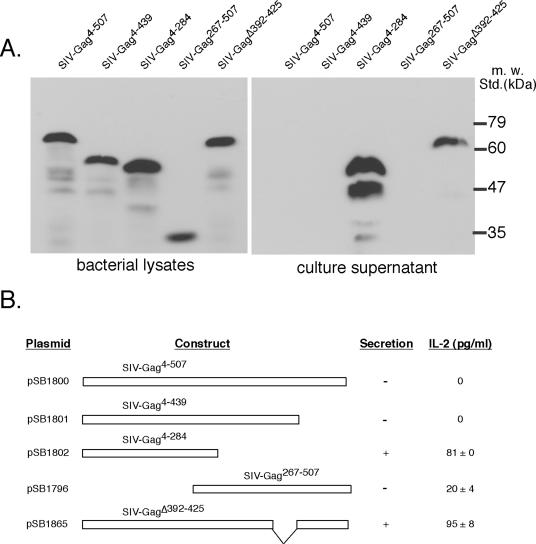
Protection against HIV is thought to require robust CD8+ T-cell responses to viral protein antigens (35, 37). SIV is the best model to study HIV pathogenesis and immunity because (i) it is highly related to HIV; (ii) SIV infections in primate animal models closely resembles HIV infections; and (iii) the parameters of protection are thought to be similar for the two diseases (20, 23). We have previously shown that a chimeric protein composed of the secretion and translocation signals of the type III secreted protein SopE fused to the first 284 amino acids of the SIV Gag protein (SopE1-104SIV-Gag4-284) was secreted efficiently via the SPI-1 TTSS and was able to prime CD8+ T-cell responses when it was delivered by a Salmonella vaccine strain in inoculated rhesus macaques (11). However, efficient protection most likely requires stimulation of responses against the entire SIV Gag protein, as well as other viral antigens. We therefore examined the ability of an S. enterica serovar Typhimurium vaccine strain to secrete a chimeric protein composed of full-length SIV Gag fused to the secretion and translocation signals of SopE (28) and a class I-restricted T-cell reporter epitope consisting of residues 366 through 374 from the influenza virus nucleoprotein (SopE1-104SIV-Gag4-507) (38). Although SopE1-104SIV-Gag4-507 was efficiently expressed by S. enterica serovar Typhimurium, the chimeric protein was not secreted into cultured supernatants of the vaccine strain (Fig. 1A). Consistent with the inability of this protein to be secreted by the SPI-1 TTSS, APCs infected with the S. enterica serovar Typhimurium strain expressing SopE1-104SIV-Gag4-507 did not present the FluNP366-374 reporter epitope of the chimeric protein to a class I antigen-presenting pathway, as demonstrated using a reporter T-cell hybridoma (Fig. 1B). The inability of SopE1-104 to drive the secretion and translocation of SIV-Gag4-507 suggested that some region(s) of this protein interferes with type III secretion. In an attempt to identify the region of SIV Gag responsible for its secretion incompetence, we constructed a series of deletions of the chimeric protein and tested them to determine whether they could be secreted via the SPI-1 TTSS. As previously shown (11), SopE1-104SIV-Gag4-284, which encompasses the amino-terminal half of SIV Gag, was efficiently secreted by the SPI-1 TTSS (Fig. 1A) and was delivered to the class I antigen-presenting pathway (Fig. 1B). These results indicated that the interfering region must be located within the carboxyl-terminal half of SIV Gag. Consistent with this hypothesis, a chimeric protein composed of SopE1-104SIV-Gag267-507 was poorly secreted (Fig. 1 A) and was inefficient at stimulating class I-restricted T-cell responses in vitro when it was expressed by an S. enterica serovar Typhimurium vaccine strain (Fig. 1B). Furthermore, SopE1-104SIV-Gag4-439 was poorly secreted and inefficiently delivered by S. enterica serovar Typhimurium to a class I antigen-presenting pathway of RMA-infected cells (Fig. 1A and B). These results indicate that the interfering region is located within a domain located between amino acids 284 and 439 of the SIV Gag protein. Previous studies have demonstrated that proteins or domains with high intrinsic stability cannot be properly unfolded by the TTSS-associated ATPase and hence cannot be efficiently secreted by the secretion machine (1). The carboxyl terminus of SIV Gag possesses two 18-residue zinc finger domains that are essential for viral packaging (2). We hypothesized that removal of these zinc finger domains may destabilize this protein and render it permissive for type III secretion. We therefore introduced a deletion within the SIV Gag protein that removed most of the two Zn fingers (SIV-GagΔ392-425). We then fused the SIV Gag mutant protein to the secretion and translocation signals of SopE and tested the chimeric protein (SopE1-104SIV-GagΔ392-425) for the ability to be secreted via the SPI-1 TTSS. Unlike SopE1-104SIV-Gag4-507, the deletion mutant SopE1-104SIV-GagΔ392-425 was efficiently secreted into the culture supernatant of an S. enterica serovar Typhimurium vaccine strain in an SPI-1 TTSS-dependent manner (Fig. 1A). In addition, the deletion mutant was efficiently delivered to a class I antigen-presenting pathway of antigen-presenting cells infected with an S. enterica serovar Typhimurium strain expressing SopE1-104SIV-GagΔ392-425 (Fig. 1B). Taken together, these results indicate that removal of its Zn finger domains renders SIV Gag permissive for type III secretion and delivery to the class I antigen-presenting pathway.
FIG. 1.
Optimization of SIV Gag for delivery through the S. enterica serovar Typhimurium type III secretion pathway. (A) Western blot analysis of bacterial lysates and culture supernatants of bacterial strains carrying plasmids that express the SopE-SIV Gag chimeras indicated. All cultures were standardized to the same optical density before processing, and a monoclonal antibody directed to the M45 epitope tag present in the constructs was used. m. w. Std., molecular mass standards. (B) Antigen presentation by RMA cells infected with S. enterica serovar Typhimurium expressing different SIV Gag constructs. RMA cells were infected with the strains indicated prior to exposure to 12.164 hybridoma cells, which produce IL-2 upon antigen presentation. The concentration of IL-2 secreted into the medium was determined by an ELISA. The data are means ± standard deviations of three independent experiments.
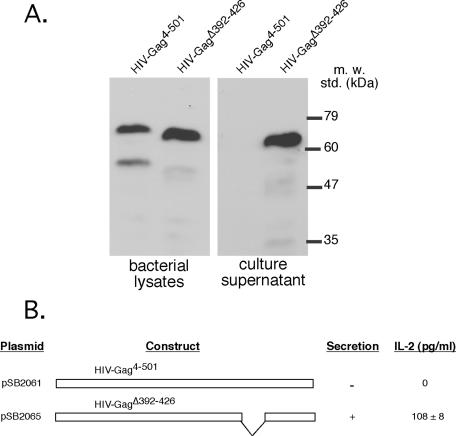
We then examined the ability of the S. enterica serovar Typhimurium SPI-1 TTSS to secrete HIV Gag when it was fused to the secretion and translocation signals of SopE. Consistent with the results obtained with SIV Gag, a chimeric protein consisting of the secretion and translocation signals of SopE fused to the FluNP366-374 reporter T-cell epitope and full-length HIV Gag (SopE1-104HIV-Gag4-501) was not secreted by the S. enterica serovar Typhimurium SPI-1 TTSS, although it was readily detected in bacterial lysates (Fig. 2A). In addition, an S. enterica serovar Typhimurium strain expressing SopE1-104HIV-Gag4-501 did not deliver the chimeric protein into a class I antigen-presenting pathway of infected APCs. These results indicated that similar to SIV Gag, a region of HIV Gag prevents delivery of the protein through the SPI-1 TTSS. We then investigated whether, similar to SIV Gag, removal of the Zn finger domains rendered HIV Gag permissive for type III secretion. We found that removal of residues 392 through 426, which contain the two Zn fingers, rendered HIV Gag permissive for SopE1-104-mediated secretion (Fig. 2A) and for delivery to the class I antigen-presenting pathway (Fig. 2B). Taken together, these results indicate that removal of discrete domains that may interfere with the TTSS can render a nonpermissive protein competent for engagement by the type III secretion machinery. Since class I-restricted epitopes tend to be linear and not influenced by the tertiary structure of the protein from which they are derived (31), removal of a small discrete region of Gag is not likely to affect its immunogenicity.
FIG. 2.
Optimization of HIV Gag for delivery through the S. enterica serovar Typhimurium type III secretion pathway. (A) Western blot analysis of bacterial lysates and culture supernatants of bacterial strains carrying plasmids that express the SopE-HIV Gag chimeras indicated. All cultures were standardized to the same optical density before processing, and a monoclonal antibody directed to the M45 epitope tag present in the constructs was used. m. w. std., molecular mass standards. (B) Antigen presentation by RMA cells infected with S. enterica serovar Typhimurium expressing different HIV Gag constructs. RMA cells were infected with the strains indicated prior to exposure to 12.164 hybridoma cells, which produce IL-2 upon antigen presentation. The concentration of IL-2 secreted into the medium was determined by an ELISA. The data are means ± standard deviations of three independent experiments.
Comparison of the abilities of the secretion and translocation signals of SopE and SptP to mediate delivery of heterologous proteins to a class I antigen-presenting pathway.
In previous studies, we have shown that the secretion and translocation signals of both SptP and SopE can mediate the delivery of heterologous peptides to the class I antigen-presenting pathway (11, 39). However, the relative efficiencies of delivery of these different signals have not been specifically compared. Since these proteins utilize different chaperones for targeting to the secretion machinery (12, 28), it is possible that the secretion domains may mediate heterologous secretion with different efficiencies. We therefore compared the abilities of the secretion and translocation signals of SopE and SptP to deliver different SIV Gag constructs to the class I antigen-presenting pathway. Delivery to this antigen-presenting pathway requires secretion from the bacterial cell, as well as translocation into and processing within antigen-presenting cells. Therefore, antigen presentation probes the ability of a given secretion and translocation signal to perform all the functions relevant for heterologous antigen delivery. To carry out the comparison, we used SIV Gag constructs that showed different efficiencies of secretion when they were fused to the secretion and translocation signals of SopE (Fig. 1). We fused the same Gag regions of these constructs to the SptP secretion and translocation signals and the FluNP366-374 reporter T-cell epitope and compared the abilities of the different chimeras to be delivered to a class I antigen-presenting pathway. We found that the secretion and translocation signals of SopE were consistently more efficient at delivering the different Gag constructs to the class I antigen-presenting pathway than were the signals derived from SptP (Table 1). In all cases, Gag constructs that were not secreted and delivered to the class I antigen-presenting pathway by the SopE signals were also not delivered to the class I pathway by the SptP signals. In conclusion, at least for these Gag constructs, the secretion signals derived from SopE are more effective at mediating delivery of heterologous proteins to a class I antigen-presenting pathway.
TABLE 1.
Comparison of eficiency of antigen delivery by SopE- or SptP-based vectors
| SIV Gag construct | IL-2 (pg/ml) for secretion signal from vectora
|
||
|---|---|---|---|
| None | SptP | SopE | |
| FluNP peptide control | 1,515 ± 176 | ||
| Gag4-507 | <10 | <10 | |
| Gag4-439 | <10 | <10 | |
| Gag4-284 | 82 ± 3 | 315 ± 13 | |
| Gag146-213 | 360 ± 31 | 480 ± 5 | |
| Vector (with FluNP epitode) | 324 ± 33 | 488 ± 35 | |
| Vector (with LCMV NP epitope)b | <10 | <10 | |
Values are the means±standard deviations for three independent determinations.
LCMV, lymphocytic choriomeningitis virus.
Comparison of the immunogenicities of optimized and wild-type Gag proteins when they are delivered by the S. enterica serovar Typhimurium SPI-1 TTSS in infected mice.
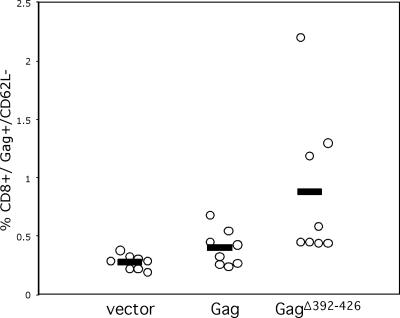
To investigate whether the optimization of heterologous protein secretion via the TTSS results in increased immunogenicity, we compared using a mouse model the immunogenicities of avirulent S. enterica serovar Typhimurium strains expressing wild-type and TTS-optimized HIV Gag fused to the secretion and translocation signals of SopE (SopE1-104HIV-Gag4-501 and SopE1-104HIV-GagΔ392-426, respectively). Mice were immunized orally with an avirulent ΔphoP ΔphoQ S. enterica serovar Typhimurium strain expressing SopE1-104HIV-Gag4-501 or SopE1-104HIV-GagΔ392-426 or carrying the vector control. Four weeks after oral immunization, animals were boosted with an intraperitoneal dose of avirulent Δasd S. enterica serovar Typhimurium strains expressing the same constructs. One week after the boost, animals were sacrificed, and the levels of HIV Gag-specific CD8+ T cells in the spleen were quantified by tetramer staining and flow cytometry. The mice immunized with S. enterica serovar Typhimurium expressing the optimized HIV Gag protein developed significantly larger numbers of Gag-specific CD8+ T cells than the mice immunized with the strains expressing the wild-type form of Gag or the empty vector control developed (Fig. 3). Consistent with the in vitro studies, these results demonstrate that the optimization of proteins for TTSS-mediated delivery results in improved immunogenicity in vivo.
FIG. 3.
Comparison of the immunogenicities of type III secretion-optimized and nonoptimized HIV Gag. Mice (eight mice per group) were immunized with avirulent strains of S. enterica serovar Typhimurium expressing wild-type HIV Gag (SopE1-104HIV-Gag4-501) (Gag) or type III secretion-optimized HIV Gag (SopE1-104HIV-GagΔ392-426) (GagΔ392-426) fused to the type III secretion and translocation signals of SopE or carrying the empty vector control (vector). Splenocytes from immunized animals were examined by flow cytometry to determine the levels of HIV Gag-specific CD8+ T cells. Open circles represent individual mice, and the values are the percentages of CD8 T cells that are tetramer specific for the Gag epitope. The horizontal bars indicate the means. The differences between the levels of Gag-specific CD8 T cells in animals immunized with the optimized Gag and the levels of Gag-specific CD8 T cells in animals immunized with the nonoptimized Gag and between the levels of Gag-specific CD8 T cells in animals immunized with the optimized Gag and the levels of Gag-specific CD8 T cells in animals immunized with the vector control were statistically significant (P = 0.038 and 0.0001, respectively).
Optimization of SIV and HIV Rev, Tat, and Nef for type III secretion.
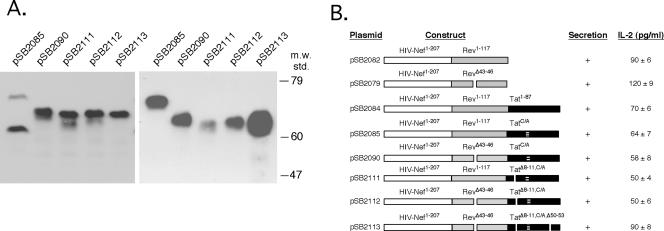
Optimal protection against a given pathogen is likely to require immunization with several antigens from the pathogen. Indeed, it is often the case that the best protection is obtained using attenuated live forms of the pathogen that the vaccine is intended to protect against (8, 22). This is likely due to the fact that efficient protection is likely to require the ability to induce complex immune responses directed to several antigens from the pathogen. For example, in the case of SIV infections, a model for HIV infections, it has been shown that attenuated forms of the virus confer probably the best protection against experimental challenge (26). However, due to safety concerns, the use of attenuated HIV as a vaccine is considered to be impractical. In an attempt to construct a vaccine able to induce an immune response to as many HIV (or model virus SIV) antigens as possible without safety concerns, we investigated delivery of the viral proteins Rev, Tat, and Nef via the S. enterica serovar Typhimurium SPI-1 TTSS. We fused each of the open reading frames of these proteins to the secretion and translocation signals of SopE (SopE1-104) and the FluNP366-374 reporter T-cell epitope and examined the type III secretion and MHC class I antigen presentation of the chimeric proteins. In all cases we used a mutant form of Nef (NefΔ239-240), which has been shown to lack the ability to down regulate the expression of MHC class I molecules (6). Although SIV Nef was secreted via the SPI-1 TTSS, Rev and Tat were not (data not shown). In close correlation with type III secretion, chimeric SopE1-104-SIV-Nef was efficiently delivered to a class I antigen presentation pathway in APCs infected with S. enterica serovar Typhimurium expressing this protein, while SIV Rev and SIV Tat were not (Fig. 4A).
FIG. 4.
Optimization of SIV Rev, Tat, and Nef for delivery through the S. enterica serovar Typhimurium type III secretion pathway. (A, B, and D) Antigen presentation by RMA cells infected with S. enterica serovar Typhimurium expressing different SIV Rev, Tat, and/or Nef constructs. RMA cells were infected with the strains indicated prior to exposure to 12.164 hybridoma cells, which produce IL-2 upon antigen presentation. The concentration of IL-2 secreted into the medium was determined by an ELISA. The data are means ± standard deviations of three independent experiments. (C) Western blot analysis of bacterial lysates and culture supernatants of bacterial strains carrying plasmids that express the SIV Rev-Tat-Nef constructs indicated. M.W. Std., molecular weight standards.
We then carried out a detail deletion analysis to identify the regions of SIV Rev and SIV Tat that interfere with type III secretion. Chimeric proteins containing different portions of the carboxyl terminus of Rev fused to the secretion and translocation signals of SopE (SopE1-104-SIV-Rev58-107 and SopE1-104-SIV-Rev78-107) were efficiently secreted via the SPI-1 TTSS (data not shown) and delivered to the class I antigen-presenting pathway (Fig. 4B). In contrast, the amino-terminal half of Rev was not secreted when it was fused to SopE1-104 (data not shown) or delivered to the class I antigen-presenting pathway (Fig. 4B). These results indicated that the region of Rev interfering with TTS is located within its amino terminus. Within this region of Rev there is a helix-turn-helix domain involved in RNA binding (5). We hypothesized that destabilization of this domain may render Rev more permissive for secretion. Indeed, removal of amino acids 39 to 46 of Rev, which encompass its RNA-binding domain, rendered this protein permissive for TTS (data not shown) and delivery into the class I antigen-presenting pathway (Fig. 4B).
Although delivery of different antigens by the S. enterica serovar Typhimurium TTSS could be achieved by administration of a mixture of bacteria expressing different chimeric proteins, it would be advantageous to minimize the number of strains used in a potential vaccine. Since Rev, Tat, and Nef are small polypeptides, we reasoned that they could be engineered so that they are delivered simultaneously as a single polypeptide fused to a type III secretion signal. We first constructed a plasmid expressing a chimeric protein consisting of the secretion and translocation signals of SopE (SopE-1-104) fused to the FluNP366-374 reporter T-cell epitope and to a polyprotein made of wild-type and TTS-optimized SIV Rev (SIV-RevΔ39-46), SIV Tat (SIV-Tat1-130), and SIV Nef (SIV-Nef1-264). The resulting chimera containing wild-type Rev was not secreted by the TTSS (Fig. 4C) or delivered into the class I antigen-presenting pathway (Fig. 4D). In contrast, the chimera containing the TTS-optimized Rev was secreted into culture supernatants (Fig. 4C) and delivered into the class I antigen-presenting pathway (Fig. 4D), although with reduced efficiency. Since SIV Nef is efficiently secreted by the SPI-1 TTSS (Fig. 1A), a series of deletions were introduced into SIV Tat to identify the regions that interfere with secretion of the chimeric protein. Two regions of Tat were targeted: a cysteine-rich region that coordinates the binding of two Zn atoms (amino acids 56 to 66) and a basic region proposed to bind RNA (amino acids 80 to 88) (4). Removal of one of these domains improved secretion and antigen presentation, and removal of both regions improved secretion and antigen presentation even further (Fig. 4C and D).
We then used the information gained through the TTSS optimization of SIV Rev, Tat, and Nef to construct a similar polyprotein containing the HIV homologs. It has been proposed previously that regions located immediately adjacent to the secretion and translocation signals of type III-secreted proteins may play an important role during the unfolding process prior to secretion (43, 44). We therefore placed HIV Nef immediately adjacent to the secretion and translocation signals of SopE since SIV Nef was found to be permissive for secretion. Indeed, placing HIV Nef immediately before the secretion-incompetent HIV protein Rev resulted in a chimeric protein that was competent for secretion and antigen presentation (Fig. 5A and B and data not shown). In an effort to further optimize the type III secretion of the HIV Nef-Rev polypeptide, we introduced deletions into the regions of HIV Rev that were shown to be deleterious for secretion in the SIV homolog. As shown in Fig. 5, introduction of the optimizing deletion into Rev did not significantly improve the secretion and antigen presentation of the HIV Nef-Rev chimera. Addition of Tat to the Nef-Rev polyprotein resulted in a chimeric protein that, unlike the SIV Rev-Tat-Nef polyprotein (Fig. 4C and D), was secreted and delivered to the class I antigen-presenting pathway (Fig. 5A and B). Disruption of the cysteine-rich region of Tat by changing five cysteines to either alanine or glycine (the original sequence, CKKCCFHCQVC, was changed to GKKGAFHAQVG) or by introducing a deletion did not significantly improve the secretion of the polyprotein (Fig. 5A and B). In summary, placing the TTS-competent protein Nef immediately adjacent to the secretion signal significantly improved the efficiency of delivery by the SPI-1 TTSS of the HIV Nef-Rev-Tat chimera. These results indicate that addition of a protein domain that easily unfolds may be a general strategy for optimizing delivery of heterologous proteins via the TTSS.
FIG. 5.
Optimization of HIV Rev, Tat, and Nef for delivery through the S. enterica serovar Typhimurium type III secretion pathway. (A) Western blot analysis of bacterial lysates and culture supernatants of bacterial strains carrying plasmids that express SopE-HIV Nef-Rev-Tat chimeras. All cultures were standardized to the same optical density before processing, and a monoclonal antibody directed to the M45 epitope tag present in the constructs was used. m.w. std., molecular weight standards. (B) Antigen presentation by RMA cells infected with S. enterica serovar Typhimurium expressing different SopE-HIV Nef-Rev-Tat constructs. RMA cells were infected with the strains indicated prior to exposure to 12.164 hybridoma cells, which produce IL-2 upon antigen presentation. The concentration of IL-2 secreted into the medium was determined by an ELISA. The data are means ± standard deviations of three independent experiments. C/A indicates the region of Tat in which the original amino acid sequence, CKKCCFHCQVC, was changed to GKKGAFHAQVG.
Concluding remarks.
In this study, we demonstrated the feasibility of an approach to render heterologous proteins that are nonpermisive for secretion via the S. enterica serovar Typhimurium SPI-1 TTSS amenable to transit through this pathway by introducing discrete small changes within interfering domains or by placing domains more prone to unfolding immediately adjacent to the secretion signal. We used this approach to optimize the secretion of several SIV and HIV proteins. Optimization of proteins for delivery through the type III secretion pathway should allow the use of this system for construction of vaccines against any microbial pathogen.
Acknowledgments
We thank Ron Desrosiers and Lou Alexander for providing SIV and HIV plasmids and Maria Lara-Tejero for help with the detection of antigen-specific CD8+ T cells and for critical reading of the manuscript.
This work was supported by Public Health Service grants AI46953 and U54 AI0157158 from the National Institutes of Health to J.E.G.
Editor: J. B. Bliska
REFERENCES
- 1.Akeda, Y., and J. E. Galan. 2005. Chaperone release and unfolding of substrates in type III secretion. Nature 437:911-915. [DOI] [PubMed] [Google Scholar]
- 2.Aldovini, A., and R. Young. 1990. Mutations of RNA and protein sequences involved in human immunodeficiency virus type 1 packaging result in production of noninfectious virus. J. Virol. 64:1920-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angelakopoulos, H., and E. L. Hohmann. 2000. Pilot study of phoP/phoQ-deleted Salmonella enterica serovar Typhimurium expressing Helicobacter pylori urease in adult volunteers. Infect. Immun. 68:2135-2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bayer, P., M. Kraft, A. Ejchart, M. Westendorp, R. Frank, and P. Rosch. 1995. Structural studies of HIV-1 Tat protein. Related articles, links. J. Mol. Biol. 247:529-535. [DOI] [PubMed] [Google Scholar]
- 5.Berger, J., C. Aepinus, M. Dobrovnik, B. Fleckenstein, J. Hauber, and E. Bohnlein. 1991. Mutational analysis of functional domains in the HIV-1 Rev trans-regulatory protein. Virology 183:630-635. [DOI] [PubMed] [Google Scholar]
- 6.Collins, K., B. Chen, S. Kalams, B. Walker, and D. Baltimore. 1998. HIV-1 Nef protein protects infected primary cells against killing by cytotoxic T lymphocytes. Nature 391:397-401. [DOI] [PubMed] [Google Scholar]
- 7.Cornelis, G. R., and F. Van Gijsegem. 2000. Assembly and function of type III secretory systems. Annu. Rev. Microbiol. 54:735-774. [DOI] [PubMed] [Google Scholar]
- 8.Curtiss, R. R. 2002. Bacterial infectious disease control by vaccine development. J. Clin. Investig. 110:1061-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deckhut, A. M., W. Allan, A. McMickle, M. Eichelberger, M. A. Blackman, P. C. Doherty, and D. L. Woodland. 1993. Prominent usage of V beta 8.3 T cells in the H-2Db-restricted response to an influenza A virus nucleoprotein epitope. J. Immunol. 151:2658-2666. [PubMed] [Google Scholar]
- 10.DiPetrillo, M. D., T. Tibbetts, H. Kleanthous, K. P. Killeen, and E. L. Hohmann. 1999. Safety and immunogenicity of phoP/phoQ-deleted Salmonella typhi expressing Helicobacter pylori urease in adult volunteers. Vaccine 18:449-459. [DOI] [PubMed] [Google Scholar]
- 11.Evans, D. T., L.-M. Chen, J. Gillis, K.-C. Lin, B. Harty, G. P. Mazzara, R. O. Donis, K. G. Mansfield, J. D. Lifson, R. C. Desrosiers, J. E. Galan, and R. P. Johnson. 2003. Mucosal priming of SIV-specific CTL responses in rhesus macaques by the Salmonella type III secretion antigen delivery system. J. Virol. 77:2400-2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fu, Y., and J. E. Galán. 1998. Identification of a specific chaperone for SptP, a substrate of the centisome 63 type III secretion system of Salmonella typhimurium. J. Bacteriol. 180:3393-3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galán, J. E. 2001. Salmonella interaction with host cells: type III secretion at work. Annu. Rev. Cell Dev. Biol. 17:53-86. [DOI] [PubMed] [Google Scholar]
- 14.Galán, J. E., and A. Collmer. 1999. Type III secretion machines: bacterial devices for protein delivery into host cells. Science 284:1322-1328. [DOI] [PubMed] [Google Scholar]
- 15.Galán, J. E., and R. Curtiss III. 1990. Expression of Salmonella typhimurium genes required for invasion is regulated by changes in DNA supercoiling. Infect. Immun. 58:1879-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galán, J. E., and R. C. Curtiss III. 1989. Virulence and vaccines potential of phoP mutants of S. typhimurium. Microb. Pathog. 6:433-443. [DOI] [PubMed] [Google Scholar]
- 17.Galán, J. E., K. Nakayama, and R. D. Curtiss. 1990. Cloning and characterization of the asd gene of Salmonella typhimurium: use in stable maintenance of recombinant plasmids in Salmonella vaccine strains. Gene 94:29-35. [DOI] [PubMed] [Google Scholar]
- 18.Gao, X. M., J. P. Tite, M. Lipscombe, J. S. Rowland, D. J. Ferguson, and A. J. McMichael. 1992. Recombinant Salmonella typhimurium strains that invade nonphagocytic cells are resistant to recognition by antigen-specific cytotoxic T lymphocytes. Infect. Immun. 60:3780-3789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garmory, H., K. Brown, and R. Titball. 2002. Salmonella vaccines for use in humans: present and future perspectives. FEMS Microbiol. Rev. 26:339-353. [DOI] [PubMed] [Google Scholar]
- 20.Geretti, A. 1999. Simian immunodeficiency virus as a model of human HIV disease. Rev. Med. Virol. 9:57-67. [DOI] [PubMed] [Google Scholar]
- 21.Gilbert, P., Y. Chiu, M. Allen, D. Lawrence, C. Chapdu, H. Israel, D. Holman, M. Keefer, M. Wolff, and S. Frey. 2003. Long-term safety analysis of preventive HIV-1 vaccines evaluated in AIDS vaccine evaluation group NIAID-sponsored phase I and II clinical trials. Vaccine 21:2933-2947. [DOI] [PubMed] [Google Scholar]
- 22.Hilleman, M. 2000. Vaccines in historic evolution and perspective: a narrative of vaccine discoveries. Vaccine 18:1436-1447. [DOI] [PubMed] [Google Scholar]
- 23.Hu, S. 2005. Non-human primate models for AIDS vaccine research. Curr. Drug Targets Infect. Disord. 5:193-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Igwe, E., G. Geginat, and H. Russmann. 2002. Concomitant cytosolic delivery of two immunodominant listerial antigens by Salmonella enterica serovar Typhimurium confers superior protection against murine listeriosis. Infect. Immun. 70:7114-7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaniga, K., S. C. Tucker, D. Trollinger, and J. E. Galán. 1995. Homologues of the Shigella IpaB and IpaC invasins are required for Salmonella typhimurium entry into cultured epithelial cells. J. Bacteriol. 177:3965-3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koff, W., P. Johnson, D. Watkins, D. Burton, J. Lifson, K. Hasenkrug, A. B. McDermott, A. Schultz, T. Zamb, R. Boyle, and R. Desrosiers. 2006. HIV vaccine design: insights from live attenuated SIV vaccines. Nat. Immunol. 7:19-23. [DOI] [PubMed] [Google Scholar]
- 27.Kotton, C., and E. Hohmann. 2004. Enteric pathogens as vaccine vectors for foreign antigen delivery. Infect. Immun. 72:5535-5547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee, S. H., and J. E. Galan. 2003. InvB is a type III secretion-associated chaperone for the Salmonella enterica effector protein SopE. J. Bacteriol. 185:7279-7284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee, S. H., and J. E. Galan. 2004. Salmonella type III secretion-associated chaperones confer secretion-pathway specificity. Mol. Microbiol. 51:483-495. [DOI] [PubMed] [Google Scholar]
- 30.Lee, V. T., and O. Schneewind. 2002. Yop fusions to tightly folded protein domains and their effects on Yersinia enterocolitica type III secretion. J. Bacteriol. 184:3740-3745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Livingstone, A., and C. Fathman. 1987. The structure of T-cell epitopes. Annu. Rev. Immunol. 5:477-501. [DOI] [PubMed] [Google Scholar]
- 32.Mata, M., P. J. Travers, Q. Liu, F. R. A. Frankel, and Y. Paterson. 1998. The MHC class I-restricted immune response to HIV-gag in BALB/c mice selects a single epitope that does not have a predictable MHC-binding motif and binds to Kd through interactions between a glutamine at P3 and pocket D. J. Immunol. 161:2985-2993. [PubMed] [Google Scholar]
- 33.Metzger, W., E. Mansouri, M. Kronawitter, S. Diescher, M. Soerensen, R. Hurwitz, D. Bumann, T. Aebischer, B. Von Specht, and T. Meyer. 2004. Impact of vector-priming on the immunogenicity of a live recombinant Salmonella enterica serovar Typhi Ty21a vaccine expressing urease A and B from Helicobacter pylori in human volunteers. Vaccine 22:2273-2277. [DOI] [PubMed] [Google Scholar]
- 34.Obert, S., R. J. O'Connor, S. Schmid, and P. Hearing. 1994. The adenovirus E4-6/7 protein transactivates the E2 promoter by inducing dimerization of a heteromeric E2F complex. Mol. Cell. Biol. 14:1333-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piazza, P., Z. Fan, and C. J. Rinaldo. 2002. CD8+ T-cell immunity to HIV infection. Clin. Lab. Med. 22:773-797. [DOI] [PubMed] [Google Scholar]
- 36.Ringrose, J. H., B. A. Yard, G. M. Verjans, and C. J. Boog. 1996. Immunization of HLA-B27 transgenic and nontransgenic mice with Salmonella typhimurium results predominantly in the generation of proliferative T cell responses. Clin. Rheumatol 15(Suppl. 1):79-85. [DOI] [PubMed] [Google Scholar]
- 37.Robinson, H., and R. Amara. 2005. T cell vaccines for microbial infections. Nat. Med. 11:S25-S32. [DOI] [PubMed] [Google Scholar]
- 38.Rotzschke, O., K. Falk, K. Deres, H. Schild, M. Norda, J. Metzger, G. Jung, and H. G. Rammensee. 1990. Isolation and analysis of naturally processed viral peptides as recognized by cytotoxic T cells. Nature 348:252-254. [DOI] [PubMed] [Google Scholar]
- 39.Russmann, H., H. Shams, F. Poblete, Y. Fu, J. E. Galán, and R. O. Donis. 1998. Delivery of epitopes by the Salmonella type III secretion system for vaccine development. Science 281:565-568. [DOI] [PubMed] [Google Scholar]
- 40.Schodel, F., and R. R. Curtiss. 1995. Salmonellae as oral vaccine carriers. Dev. Biol. Stand. 84:245-253. [PubMed] [Google Scholar]
- 41.Shams, H., F. Poblete, H. Russmann, J. E. Galán, and R. O. Donis. 2001. Induction of specific CD8+ memory T cells and long lasting protection following immunization with Salmonella typhimurium expressing a lymphocytic choriomeningitis MHC class I-restricted epitope. Vaccine 20:577-585. [DOI] [PubMed] [Google Scholar]
- 42.Sory, M.-P., A. Boland, I. Lambermount, and G. Cornelis. 1995. Identification of the YopE and YopH domains required for secretion and internalization into the cytosol of macrophages, using the cyaA gene fusion approach. Proc. Natl. Acad. Sci. USA 92:11998-12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stebbins, C. E., and J. E. Galan. 2003. Priming virulence factors for delivery into the host. Nat. Rev. Mol. Biol. 4:738-743. [DOI] [PubMed] [Google Scholar]
- 44.Stebbins, C. E., and J. E. Galán. 2000. Modulation of host signaling by a bacterial mimic: structure of the Salmonella effector SptP bound to Rac1. Mol. Cell. 6:1449-1460. [DOI] [PubMed] [Google Scholar]
- 45.Tacket, C., J. Galen, M. Sztein, G. Losonsky, T. Wyant, J. Nataro, S. Wasserman, R. Edelman, S. Chatfield, G. Dougan, and M. Levine. 2000. Safety and immune responses to attenuated Salmonella enterica serovar Typhi oral live vector vaccines expressing tetanus toxin fragment C. Clin. Immunol. 97:146-153. [DOI] [PubMed] [Google Scholar]
- 46.Wang, R. F., and S. R. Kushner. 1991. Construction of versatile low-copy-number vectors for cloning, sequencing and gene expression in Escherichia coli. Gene 100:195-199. [PubMed] [Google Scholar]
- 47.Yang, D. M., N. Fairweather, L. L. Button, W. R. McMaster, L. P. Kahl, and F. Y. Liew. 1990. Oral Salmonella typhimurium (AroA−) vaccine expressing a major leishmanial surface protein (gp63) preferentially induces T helper 1 cells and protective immunity against leishmaniasis. J. Immunol. 145:2281-2285. [PubMed] [Google Scholar]