Abstract
Women at obstetric high risk more often experience negative feelings related to childbirth than women with normal outcomes. For these high-risk women, an individual birth plan does not appear to improve the overall experience of childbirth; rather, it seems to intensify the negative feelings in several aspects. The increased vulnerability in women at high risk warrants special attention to the possibility that types of care routinely offered to all women may negatively influence the experiences of high-risk women.
Keywords: birth plan, childbirth experience, high-risk pregnancy, high-risk childbirth
Introduction
The childbirth experience is a complex event and an important life experience for women, with long-term impacts throughout life (Halldórsdóttir, 1996; Marut & Mercher, 1979; Simkin, 1991, 1992). The experience influences the future well-being of the woman, her child, and their relationship, as well as the woman's relationship with her partner (Brudal, 1985; Green, Coupland, & Kitzinger, 1990; Lagerkrantz, 1974; Morris-Thompson, 1992; Oakley, 1993). If they are in an obstetrical-risk situation, women can be fragile and vulnerable during the childbearing period (McCain & Deatrick, 1994; Mercher, 1990; Stainton, McNeil, & Harvey, 1992).
In modern Western society's antenatal care, special attention is paid to women with actual complications and to women with certain risk factors in pregnancy. For example, women with insulin-dependent diabetes mellitus may represent women with risk factors. In a hermeneutic phenomenological study, 14 diabetic women were interviewed three times during pregnancy (at gestational weeks 11–15, 22–27, and 32–39) (Berg & Honkasalo, 2000). The women expressed moral commitment to provide the growing child with the best conditions for a healthy start in life. The demands they experienced were divided into two main categories. The first, called objectification, included loss of control with an awareness of having an unwell, “risky” body. The women expressed dependency on blood glucose controls and assessments by midwives and doctors, as well as on support from their partners and significant others. The second category, exaggerated responsibility, had three expressions: constant worry for the child, constant pressure to create the best conditions for the child, and constant self-blame due to a feeling of failure to optimise the conditions for the child.
In a previously reported phenomenological interview study with 10 women (Berg & Dahlberg, 1998), the researchers described the essential derived meaning of an obstetrically complicated childbirth as confirmation, including its negative sense, disconfirmation. Confirmation included perceptions of trust and having a dialogue with the health care providers, keeping a sense of control over the situation, and feeling like a “good mother.” These experiences made women feel accepted as birthing subjects and as mothers-to-be, even if obstetric interventions including high technology were performed. On the other hand, disconfirmation included perceptions of not being seen and respected, having no dialogue, experiencing discouragement, losing a sense of control (with feelings of unreality), and becoming a depersonified object. It could also include feelings of guilt for giving the baby a traumatic birth, as well as a lack of confidence in one's own capacity for giving birth.
Since the 1980s, birth plans in a variety of formats (Whitford & Hillan, 1998) have been introduced as tools to help women gain a better experience of childbirth, mainly by allowing a higher degree of control (Kitzinger, 1983, 1988, 1992). A sense of control is associated with a positive experience of childbirth (Simkin, 1991, 1992), even in a complicated childbirth (Berg & Dahlberg, 1998). Women who do not feel in control of themselves or their environment are less satisfied and less likely to feel fulfilled, and they have low postnatal emotional well-being (Green et al., 1990). In some places in Sweden, birth plans have been introduced, mostly focusing on women's expressed specific needs and desires, such as pain-relief methods or other specific procedures. Studies that evaluate the effects of a birth plan are limited.
For the present study, a main question was whether or not the negative feelings of high-risk women—as described in the two qualitative studies of women at high risk (i.e., with risk factors or complications during pregnancy and childbirth) (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000)—were more common than in women with normal outcomes during both pregnancy and childbirth. A second question was whether or not an individual birth plan can positively influence the childbirth experiences of women at high risk.
Methods
Setting
Maternity care in Sweden is organized in two segments:
antenatal care, which is part of the community health care system and offers assistance to all women during pregnancy and 12 weeks postpartum, and
high-risk antenatal care and delivery care at the hospital level.
If the woman is healthy and has a normal pregnancy, midwives in the community provide all antenatal care, including childbirth education. Also, in the delivery ward, midwives staff the unit and are responsible for the care of women with normal conditions. When complications or risk factors occur, the obstetricians take charge. The midwives remain involved, but they lose some of their autonomy, provide care under supervision, and assist the obstetricians in obstetric interventions and specialised investigations. Many midwives are specialised in different fields (e.g., in ultrasound and diabetes care) and are given delegated responsibility. The midwife in antenatal care writes a summary of the pregnancy in the antenatal file at the end of the pregnancy. The summary serves as a report to the midwife at the delivery ward and sometimes includes the mother's specific needs and desires about the childbirth. A letter from the mother can also be added. Since the 1970s, the father or another significant relative is present at almost every childbirth to support the woman.
In many Swedish hospitals, delivery care has been differentiated during recent years: basic care for women with normal pregnancy and childbirth, and a second level for women with complications (Socialstyrelsen, 1996, 2001; World Health Organization, 1996). The Göteborg area in Sweden, where this study was conducted, has 18 antenatal care units (ACUs) and one clinic for women who are at high obstetric risk (i.e., have risk factors or obstetric complications). The participants in this study were chosen from seven ACUs: five public, one private, and the one for women at high risk. Three ACUs are located in suburbs, two in the city center, and one in a mixed area. The clinic for women at high risk is situated at the Sahlgrenska University (SU) Hospital. In Göteborg, there is one large unit for maternity delivery care: the SU Hospital. It consists of three delivery wards located in two different parts of Göteborg. This study was performed at SU/Östra, which has two delivery wards: one for women with normal pregnancies and one “special delivery ward” for women at high obstetric risk.
Ethical Considerations
Ethical approval and permission to undertake the study were obtained from the Research Ethics Committee, Göteborg University. Permission for access to the units to undertake the study was obtained from the physicians in charge at the hospital and antenatal care units.
Study Sample, Procedure, and Measures
In a synthesis of five qualitative studies of women's experiences during pregnancy and childbirth (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000; Berg, Lundgren, Hermansson, & Wahlberg, 1996; Lundgren & Dahlberg, 1998; Lundgren & Wahlberg, 1999), five categories were found to be essential. They also constituted the basis for the construction of two questionnaires and a birth plan. These five categories were:
relationship with midwife, physician, and partner/other relative;
fear of childbirth;
pain during childbirth;
sense of control; and
concerns for the child.
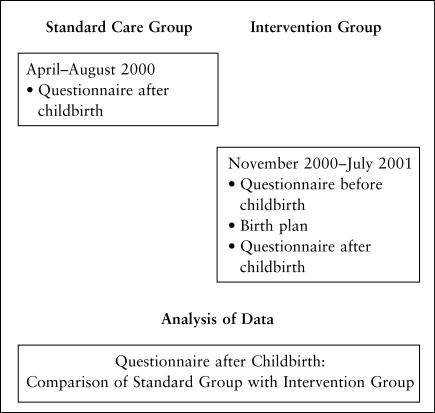
Between April and August 2000, women (n = 271) who had received standard care during pregnancy at the seven ACUs and gave birth at SU/Östra, the normal delivery ward, and the special delivery ward were consecutively recruited to the study as a control group for comparison with a subsequent intervention group.
Between November 2000 and July 2001, pregnant women from the same seven ACUs were recruited consecutively for the intervention described below. All women who intended to give birth at the regional hospital, SU/Östra, were invited to participate. Exceptions in both the control and intervention groups included women who planned an elective cesarean birth and women who did not speak or write Swedish well.
When the numbers of primiparae and multiparae recruited from each ACU had reached the numbers in the previously studied standard care group, the recruitment of the intervention group was stopped to ensure comparability with the standard care group. Of the eligible women, 41 were never included because the midwife did not have time, and 45 women did not want to participate in the study. Lost to follow-up were 49 women who were transferred to another hospital for delivery and two women with stillbirths. In total, 271 women participated in the study's two groups (intervention and standard) and all delivered at the same hospital.
Research Instruments
The intervention consisted of a questionnaire at the end of pregnancy (after 33 gestational weeks), followed by an individual birth plan written together by the ACU midwife and the woman. The childbirth experience was evaluated in a questionnaire within one week after childbirth. In contrast, the group of women who received standard care were only asked to answer the postpartum questionnaire at one week postpartum, which thus was the instrument for evaluation of the intervention. See Figure for an illustration of the study design.
Study Design
The researchers personally administered the questionnaire to the mothers at the postpartum ward unit. The statements in the questionnaires measured degree of satisfaction on a 6-grade scale from totally disagree to totally agree. For each statement, the woman scored the degree of agreement from 1–6. Examples of statements were as follows:
“The midwife listened and paid attention to my needs and desires.”
“I had confidence in my own capacity.”
“During childbirth, I was constantly afraid that complications would affect the child.”
The birth plan had six categories: the five previously mentioned categories and an additional one labelled other needs and desires. With this open-ended set of categories as a basis, the midwife and woman together identified the woman's needs and desires, as expressed in her own words (see Tables 1 and 2). The woman then brought the birth plan to the delivery ward where the midwives had been instructed to use it as guide for care. The questionnaires were not previously statistically validated.
Table 1.
Example of an Individual Birth Plan from a Woman with a Normal Pregnancy
| Name |
| Civil Registration Number |
| Estimated Date of Delivery |
| Relationship with Midwife, Physician, Partner/Other Relative |
| I would like my husband to be present during the childbirth. Not too many people in the delivery room. I would like support from the midwife. |
| Fear of Childbirth |
| I am afraid that something unexpected may happen and that a state of emergency may occur that might influence my capacity to manage, mentally and emotionally. I am also afraid that a perineal rupture may occur. |
| Pain during Childbirth |
| I have a fear of pain during the second stage. I also fear that something will happen to the child. I am afraid that I will not be able to cope with the pain. However, I want the childbirth to be as natural as possible. To achieve this, I need great support. |
| Sense of Control |
| I would like to be informed about what is happening. I certainly don't want to be disregarded. |
| Concerns for the Child |
| I want it to be calm and peaceful, and that the child should have as soft and pleasant a birth as possible—for example, softened light, an avoidance of scalp electrode. |
| Other Needs and Desires |
Table 2.
Example of an Individual Birth Plan from a Woman with a Complicated Pregnancy
| Name |
| Civil Registration Number |
| Estimated Date of Delivery |
| Relationship with Midwife, Physician, Partner/Other Relative |
| Relies upon the husband being able to assist; wants hints on what he can assist with. He looks forward to it being a “normal” delivery. |
| Fear of Childbirth |
| Is not particularly nervous, but is a little bit worried that complications may arise. Relies on her own ability. |
| Pain during Childbirth |
| Did not experience much pain in connection with a cesarean in 1998. |
| Sense of Control |
| Would like a certain degree of control, but relies on the staff. Wants monitoring in the form of cardiotocography. Wants to be informed about what is happening. |
| Concerns for the Child |
| Is worried that complications will occur during delivery. |
| Other Needs and Desires |
| Wants concrete advice. |
In the present analysis, 23 of the 61 statements in the postpartum questionnaire were chosen based on the essential findings in the two previous qualitative studies of women at high risk (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000). The statements addressed four areas: relationship, control, demands and worry, and the overall estimation of the childbirth experience (see Table 3).
Table 3.
Evaluation of Childbirth Experience—Postpartum Questionnaire
| Category | Questions/Statements |
|---|---|
| Relationship | (7 statements) |
| Midwives 1 & 2*, Physician | •Listening (3x1 statements) |
| •Paying attention to needs and desires; trust (3x1 statements) | |
| Husband/Partner | (1 statement) |
| •Support | |
| Control | (9 statements): |
| •Sense of control during labor | |
| •Sense of control during second stage | |
| •Sense of control, on the whole | |
| •No need of control, if the staff had control | |
| •Check-ups basis for security | |
| •Participation in decision/objectification | |
| •Difficulty in interpreting body signals during labor | |
| •Difficulty in interpreting body signals during second stage | |
| •Difficulty in interpreting body signals, on the whole | |
| Demands and Worry | (6 statements): |
| •Confidence in own capacity | |
| •Severe demands | |
| •Feeling of failure | |
| •Hard birth for the child | |
| •Constant fear of complications affecting the child | |
| •Suffering pain for the child's sake | |
| The Overall Experience | (1 statement) |
| •The childbirth experience, on the whole |
If the woman was cared for by more than one midwife, she was asked to judge the first (Midwife 1) and one of the other midwives who assisted during the second stage of delivery (Midwife 2).
For the analysis, women in the stanard and intervention groups were divided into four subgroups with respect to risk factors and complications during pregnancy and delivery:
Normal Pregnancy and Normal Childbirth (NPNC),
Complicated Pregnancy and Normal Childbirth (CPNC),
Normal Pregnancy and Complicated Childbirth (NPCC), and
Complicated Pregnancy and Complicated Childbirth (CPCC).
Complicated pregnancy was defined as displaying either the presence of risk factors for obstetric complications or complications manifested during pregnancy. A risk factor could, for example, be a chronic disease that might influence pregnancy outcome and the level of super-vision or interventions during pregnancy (e.g., diabetes mellitus, hypertension, or bad obstetric history). Complications during pregnancy could, for example, be gestational diabetes, gestational hypertension, pre-eclampsia, or growth retardation of the fetus. Complicated childbirth included forceps/vacuum extraction, emergency cesarean birth, blood loss > 1000 ml, manual removal of placenta, perineal tear degree III–IV, duplex, neonatal asphyxia (apgar score < 7 at five minutes), or vaginal breech delivery.
Each complicated subgroup (CPNC, NPCC, CPCC) was compared with the normals (NPNC). This comparative analysis was carried out 1) in the standard group, 2) in the intervention group, and 3) between subgroups in the standard and intervention groups.
Data were analyzed using SPSS (Statistical Package for Social Sciences) version 10.0. The cross-tabulation program was used for the statistical calculations of differences (Person chi-square), and a p-value of less than 0.05 was considered significant. Significance test (Chi-square) was done for each of the three comparisons, one by one, and was calculated on the whole distribution 1–6. The extreme answers (i.e., 1 + 2 [disagree] and 5 + 6 [agree]) are presented below.
Results
Comparative Analysis between Subgroups
The respondent rate was 91.4% in the group receiving standard care (N = 271) and 98% in the intervention group (N = 271), which was given a questionnaire and formulated a birth plan in late pregnancy. Main characteristics of the participants in the two groups were similar (see Table 4). All first-time mothers in both groups had participated in the prenatal education classes offered at the antenatal care unit. Almost all women had their partner or another relative present as their companion at birth. The results are presented together in a summarized form under the headings below. An overview of the ratings in each subgroup of women is presented in Tables 5a, 5b, 6a, 6b, 7a, and 7b.
Table 4.
Characteristics of Study Participants
| Characteristics | Standard Group | Intervention Group |
|---|---|---|
| Subgroups | N (%) | N (%) |
| NPNC | 126 (46.5) | 134 (49.5) |
| CPNC | 60 (22.1) | 57 (21.0) |
| NPCC | 62 (22.9) | 61 (22.5) |
| CPCC | 23 (8.5) | 19 (7.0) |
| Maternal Age | Mean | Mean |
| NPNC | 29.92 | 29.67 |
| CPNC | 30.88 | 9.96 |
| NPCC | 36.23 | 31.33 |
| CPCC | 33.74 | 34.42 |
| Primiparous | N (%) | N (%) |
| NPNC | 61 (48.4) | 58 (43.3) |
| CPNC | 30 (50.0) | 26 (45.6) |
| NPCC | 33 (53.2) | 40 (65.6) |
| CPCC | 7 (30.4) | 7 (36.8) |
NP = Normal Pregnancy NC = Normal Childbirth CP = Complicated Pregnancy CC = Complicated Childbirth
Table 5a.
Standard Group—Experience of Relationship. Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1 + 2 and 5 + 6 for each question. P-value for each complicated group compared with the normal group. |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
||||||||
| Question | 1 + 2 |
5 + 6 |
1 + 2 |
5 + 6 |
P |
1 + 2 |
5 + 6 |
P |
1 + 2 |
5 + 6 |
P |
|
Midwife 1 | |||||||||||
| Listening, paying attention to needs and desires | 32.0 (4) | 92.8 (116) | 0.0 (0) | 90.3 (56) | ns | 0.0 (0) | 88.7 (55) | 0.031 | 4.5 (1) | 95.4 (21) | ns |
| Trust | 3.2 (4) | 92.8 (117) | 1.7 (1) | 95.0 (57) | ns | 1.6 (1) | 85.3 (53) | 0.025 | 0.0 (0) | 81.3 (18) | ns |
| Midwife 2 | |||||||||||
| Listening, paying attention to needs and desires | 0.0 (0) | 96.0 (49) | 5.8 (2) | 82.9 (29) | ns | 0.0 (0) | 90.0 (36) | ns | 6.3 (2) | 94.0 (14) | ns |
| Trust | 0.0 (0) | 92.2 (47) | 3.2 (2) | 88.5 (31) | ns | 5.0 (3) | 85.0 (34) | ns | 0.0 (0) | 97.5 (14) | ns |
| Physician | |||||||||||
| Listening, paying attention to needs and desires | 12.5 (3) | 66.7 (16) | 7.7 (2) | 73.0 (19) | ns | 6.2 (2) | 71.0 (22) | ns | 12.5 (1) | 62.5 (5) | ns |
| Trust | 16.6 (2) | 75.0 (18) | 11.5 (3) | 80.8 (21) | ns | 9.1 (3) | 78.8 (26) | ns | 25.0 (2) | 75.0 (6) | ns |
| Partner/Other Relative | |||||||||||
| Support | 0.8 (1) | 97.6 (119) | 0.0 (0) | 96.5 (55) | ns | 0.0 (0) | 98.4 (60) | ns | 0.0 (0) | 100.0 (23) | ns |
NP = Normal Pregnancy__NC = Normal Childbirth__CP = Complicated Pregnancy__CC = Complicated Childbirth
Table 5b.
Intervention Group (Women with a Birth Plan)—Experience of Relationship.Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1 + 2 and 5 + 6 for each question. P-value for each complicated group compared with the normal group. |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
|||||||||
| Question | 1 + 2 | 5 + 6 | 1 + 2 | 5 + 6 | P | 1 + 2 | 5 + 6 | P | 1 + 2 | 5 + 6 | P | |
| Midwife 1 | ||||||||||||
| Listening, paying attention to needs and desires | 3.8 (5) | 86.4 (14) | 5.4 (3) | 78.5 (44) | ns | 3.3 (2) | 86.6 (51) | ns | 5.3 (1) | 79.0 (15) | ns | |
| Trust | 6.8 (5) | 84.1 (11) | 3.6 (2) | 85.4 (47) | ns | 6.6 (4) | 85.3 (52) | ns | 5.3 (1) | 68.4 (13) | ns | |
| Midwife 2 | ||||||||||||
| Listening, paying attention to needs and desires | 1.5 (1) | 87.8 (58) | 2.5 (1) | 72.5 (29) | 0.037 | 2.3 (1) | 95.5 (42) | ns | 0.0 (0) | 85.7 (12) | ns | |
| Trust | 3.0 (2) | 88.0 (59) | 7.6 (3) | 79.5 (31) | ns | 2.3 (1) | 95.5 (42) | ns | 0.0 (0) | 92.8 (13) | ns | |
| Physician | ||||||||||||
| Listening, paying attention to needs and desires | 5.3 (1) | 84.2 (16) | 8.0 (2) | 56.0 (19) | ns | 2.8 (1) | 61.1 (22) | ns | 0.0 (0) | 84.7 (6) | ns | |
| Trust | 5.0 (1) | 85.0 (17) | 3.8 (3) | 76.9 (20) | ns | 0.0 (0) | 75.7 (28) | ns | 0.0 (0) | 84.7 (6) | ns | |
| Partner/Other Relative | ||||||||||||
| Support | 0.8 (1) | 96.6 (131) | 5.9 (3) | 92.1 (47) | ns | 1.7 (1) | 98.3 (58) | ns | 0.0 (0) | 100.0 (19) | ns | |
NP = Normal Pregnancy NC = Normal Childbirth CP = Complicated Pregnancy CC = Complicated Childbirth
Table 6a.
Standard Group—Experience of Control. Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1+2 and 5+6 for each question. P-value for each complicated group compared with the normal group. |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
||||||||
| Question | 1+2 |
5+6 |
1+2 |
5+6 |
P |
1+2 |
5+6 |
P |
1+2 |
5+6 |
P |
| I had control during labor | 17.6 (22) | 48.8 (61) | 25.0 (14) | 32.1 (18) | ns | 22.5 (14) | 46.7 (29) | ns | 4.3 (19) | 69.6 (16) | 0.006 |
| I had control during second stage | 23.0 (29) | 43.7 (55) | 31.4 (16) | 47.1 (24) | ns | 28.6 (16) | 30.3 (17) | 0.023 | 13.0 (3) | 39.1 (9) | ns |
| On the whole, I had control | 31.2 (19) | 35.3 (43) | 30.9 (17) | 38.1 (21) | ns | 33.8 (11) | 27.1 (16) | ns | 27.3 (6) | 36.6 (8) | ns |
| No need of control if the staff had control | 72.2 (91) | 11.9 (15) | 69.6 (39) | 14.3 (8) | ns | 68.4 (37) | 12.3 (8) | 0.032 | 81.6 (18) | 13.6 (3) | ns |
| Check-ups basis for security | 31.2 (19) | 35.3 (43) | 30.9 (17) | 38.1 (21) | ns | 33.8 (11) | 27.1 (16) | ns | 27.3 (6) | 36.3 (8) | ns |
| No participation in decisions/objectification | 91.3 (115) | 3.3 (4) | 72.7 (40) | 3.6 (2) | 0.02 | 79.0 (49) | 6.4 (4) | ns | 100.0 (22) | 0.0 (0) | ns |
| Difficult to interpret body signals during labor | 63.5 (80) | 12.7 (16) | 54.6 (30) | 21.8 (12) | ns | 59.3 (35) | 15.3 (9) | ns | 78.7 (17) | 8.7 (2) | ns |
| Difficult to interpret body signals during second stage | 65.1 (82) | 15.8 (20) | 59.6 (31) | 21.1 (11) | ns | 65.0 (37) | 21.0 (12) | ns | 73.9 (17) | 8.6 (3) | ns |
| On the whole, difficult to interpret body signals | 68.0 (85) | 8.4 (11) | 55.4 (31) | 12.5 (7) | ns | 61.0 (36) | 11.9 (7) | ns | 82.6 (19) | 4.3 (1) | Ns |
NP = Normal Pregnancy__NC = Normal Childbirth__CP = Complicated Pregnancy__CC = Complicated Childbirth
Table 6b.
Intervention Group (Women with a Birth Plan)—Experience of Control. Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1+2 and 5+6 for each question. P-value for each complicated group compared with the normal group. |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
||||||||
| Question | 1+2 | 5+6 | 1+2 | 5+6 | P | 1+2 | 5+6 | P | 1+2 | 5+6 | P |
| I had control during labor | 14.2 (19) | 53.0 (71) | 21.0 (12) | 50.9 (39) | ns | 15.3 (9) | 47.4 (28) | ns | 21.1 (4) | 31.6 (6) | 0.006 |
| I had control during second stage | 18.1 (379) | 40.2 (53) | 27.8 (15) | 46.0 (25) | ns | 37.3 (19) | 31.4 (16) | ns | 33.4 (6) | 38.9 (7) | ns |
| On the whole, I had control | 12.9 (17) | 46.7 (62) | 21.1 (12) | 33.3 (19) | ns | 15.5 (9) | 37.9 (22) | ns | 21.1 (4) | 36.9 (7) | ns |
| No need of control if the staff had control | 67.7 (90) | 15.8 (21) | 65.0 (37) | 14.0 (8) | ns | 67.8 (40) | 13.6 (8) | ns | 63.1 (12) | 21.1 (4) | ns |
| Check-ups basis for security | 43.9 (58) | 23.5 (31) | 35.2 (19) | 46.3 (25) | 0.021 | 33.8 (20) | 38.9 (23) | ns | 26.4 (5) | 57.2 (10) | ns |
| No participation in decisions/objectification | 87.9 (116) | 3.8 (59) | 77.2 (44) | 8.8 (5) | 0.04 | 86.2 (50) | 6.8 (4) | ns | 89.5 (17) | 5.3 (1) | ns |
| Difficult to interpret body signals during labor | 71.6 (96) | 14.2 (19) | 57.1 (32) | 17.8 (10) | ns | 59.3 (35) | 15.3 (9) | ns | 84.2 (16) | 5.3 (1) | ns |
| Difficult to interpret body signals during second stage | 64.9 (87) | 12.7 (17) | 59.3 (32) | 24.1 (13) | ns | 59.6 (31) | 25.0 (13) | 0.006 | 68.4 (13) | 10.5 (2) | ns |
| On the whole, difficult to interpret body signals | 75.4 (101) | 5.9 (8) | 56.4 (319 | 18.1 (10) | 0.019 | 64.3 (36) | 10.7 (6) | ns | 84.2 (16) | 5.3 (1) | ns |
NP = Normal Pregnancy NC = Normal Childbirth CP = Complicated Pregnancy CC = Complicated Childbirth
Table 7a.
Standard Group—Experience of Demands and Worry and Overall Satisfaction. Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1+2 and 5+6 for each question. P-value for each complicated group compared with the normal group. |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
||||||||
| Question | 1+2 |
5+6 |
1+2 |
5+6 |
P |
1+2 |
5+6 |
P |
1+2 |
5+6 |
P |
| Confidence in own capacity | 4.8 (7) | 61.4 (70) | 6.9 (4) | 50.0 (29) | ns | 16.6 (5) | 51.7 (31) | ns | 4.3 (1) | 82.6 (19) | ns |
| Too severe demands | 74.2 (64) | 8.0 (10) | 71.8 (23) | 15.8 (9) | ns | 46.6 (27) | 13.7 (8) | ns | 82.6 (15) | 4.3 (1) | ns |
| Feeling of failure | 90.4 (113) | 3.2 (4) | 84.2 (48) | 7.0 (4) | ns | 88.4 (53) | 0.0 (0) | ns | 94.7 (22) | 0.0 (0) | ns |
| My child had a difficult birth | 72.8 (91) | 10.4 (13) | 62.0 (36) | 15.9 (9) | ns | 50.0 (30) | 23.4 (14) | 0.017 | 66.7 (14) | 4.8 (1) | ns |
| Constant fear of complications affecting the child | 66.4 (83) | 12.8 (16) | 68.4 (39) | 14.0 (8) | ns | 45.8 (27) | 27.2 (16) | ns | 50.0 (11) | 13.6 (3) | ns |
| Suffer pain for the child's sake | 10.7 (13) | 60.8 (74) | 28.0 (16) | 40.3 (23) | 0.029 | 20.4 (12) | 59.1 (33) | ns | 8.7 (2) | 65.2 (15) | ns |
| Childbirth positive, on the whole | 13.6 (17) | 65.6 (82) | 17.2 (10) | 53.4 (31) | ns | 17.0 (10) | 51.8 (30) | ns | 4.3 (1) | 73.9 (17) | ns |
NP = Normal Pregnancy__NC = Normal Childbirth__CP = Complicated Pregnancy__CC = Complicated Childbirth
Table 7b.
Intervention Group (Women with a Birth Plan)—Experience of Demands and Worry and Overall Satisfaction. Comparison between Women with Normal Pregnancy and Childbirth and Women with Complications
| % (No.) of ratings 1+2 and 5+6 for each question. P-value for each complicated group compared with the normal group. |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NPNC |
CPNC |
NPCC |
CPCC |
||||||||
| Question | 1+2 | 5+6 | 1+2 | 5+6 | P | 1+2 | 5+6 | P | 1+2 | 5+6 | P |
| Confidence in own capacity | 7.5 (10) | 65.4 (97) | 16.1 (9) | 60.7 (34) | ns | 13.4 (8) | 50.0 (30) | ns | 10.6 (2) | 57.9 (11) | 0.031 |
| Too severe demands | 83.4 (111) | 4.5 (6) | 57.2 (32) | 14.3 (8) | 0.01 | 66.7 (40) | 11.7 (7) | ns | 73.7 (14) | 5.3 (1) | ns |
| Feeling of failure | 93.3 (125) | 0.0 (0) | 80.3 (45) | 10.8 (6) | 0.009 | 80.0 (48) | 5.0 (3) | 0.028 | 88.3 (12) | 0.0 (0) | ns |
| My child had a difficult birth | 45.2 (90) | 9.8 (13) | 52.6 (30) | 21.1 (12) | ns | 47.6 (29) | 31.2 (19) | 0.001 | 47.4 (9) | 15.8 (3) | ns |
| Constant fear of complications affecting the child | 62.7 (84) | 14.9 (20) | 35.7 (20) | 41.1 (23) | 0.001 | 56.7 (34) | 26.7 (16) | ns | 47.4 (9) | 36.8 (7) | ns |
| Suffer pain for the child's sake | 10.7 (20) | 60.6 (75) | 12.3 (7) | 71.2 (41) | ns | 20.4 (8) | 59.1 (32) | ns | 8.7 (3) | 65.2 (11) | ns |
| Childbirth positive, on the whole | 6.7 (9) | 66.5 (89) | 17.0 (10) | 56.2 (32) | 0.016 | 24.6 (15) | 54.1 (33) | 0.004 | 10.2 (2) | 63.2 (12) | ns |
NP = Normal Pregnancy NC = Normal Childbirth CP = Complicated Pregnancy CC = Complicated Childbirth
Relationship with Midwives, Physician, and Partner/Other
Support from partner/other relative scored very high (5 + 6: ≥ 92.1% or more) in all the subgroups with no significant differences. All groups generally had high ratings (≥ 68.4%) concerning trust in staff and feelings that staff were listening and paying attention to their needs and desires. However, the analysis revealed some statistical differences when comparing the normals (NPCC) with the other subgroups with complications, both in the standard group and the group with a birth plan. In the standard care group, women with normal pregnancy and complicated childbirth (NPCC) felt less of a degree of trust in the first midwife compared with the normals (5 + 6: 85.3% vs. 92.8%; p = 0.025). They also gave lower scores to the degree of listening and paying attention to their needs and desires (5 + 6: 88.7% vs. 92.8%; p = 0.031). In the intervention group, women with complicated pregnancy and normal childbirth (CPNC) had lower ratings for the second midwife concerning listening and considering their needs and desires than the normals (5 + 6:72.5% vs. 87.8%; p=0.037) (see Tables 5a and 5b).
Sense of Control
The ratings about aspects of sense of control varied greatly within all subgroups, but without major differences between the groups. The exceptions included women with complicated pregnancy and childbirth (CPCC) in the standard group. They agreed much more often to the statement of control during labor, significantly more often than the normals (5 + 6: 69.6% vs. 48.8%; p = 0.006). Women in the standard group with normal pregnancy and complicated childbirth (NPCC) scored lower on sense of control compared with the normals during the second stage (5 + 6: 28.6% vs. 43.7%, p = 0.023). A vast majority in all groups (63.1%–81.6%) had low ratings (1+2), indicating that they did not agree with the statement that there was no need of control if the staff had control. Only 12%–14% agreed totally that they could leave the control to the staff. No significant differences between the subgroups were found. The majority of women in all subgroups felt that some capacity to interpret body signals was maintained. In the intervention group, women with normal pregnancy and complicated childbirth (NPCC) felt difficulty in interpreting body signals during second stage to a higher degree than the normals (5 + 6: 25.0% vs. 12.7%; p = 0.006). Women with complicated pregnancy and normal childbirth (CPNC) in the intervention group also had greater difficulty in interpreting body signals on the whole, compared with the normals (5 + 6: 18.1% vs. 5.9%; p = 0.019).
A majority of women in all groups disagreed with the statement of no participation in decisions (objectification). However, women with complicated pregnancy and normal childbirth (CPNC) disagreed to a lesser degree, indicating a lesser feeling of participation (1 + 2: 72.7% vs. 91.3%; p = 0.020) compared with the normals in the standard group. A similar difference in CPNC was seen in the intervention group (1 + 2: 77.2% vs. 87.9%; p = 0.04). The dependency on check-ups as a basis for a feeling of security was scored similarly in the different groups, except in the group with complicated pregnancy and normal childbirth (CPNC) with a birth plan who needed the check-ups as a basis for security to a significantly greater extent (5+6: 46.3% vs. 23.5%; p=0.021) (see Tables 6a and 6b).
Feelings of Demands and Worries
All groups had high ratings concerning confidence in their own capacity (5+6: 50% or more). Too severe demands was rated quite low in all groups, but a significantly higher affirmation to this statement was seen in the group of women with a complicated pregnancy and normal childbirth (CPNC) with a birth plan when compared to the normals (5 + 6: 14.3% vs. 4.5%; p = 0.01). Feeling of failure was not common. Only a few women totally agreed among the subgroups with either complicated pregnancy or childbirth (CPNC and NPCC) belonging to the group with a birth plan. Nevertheless, the difference was significant compared with the normals. The highest ratings affirming that their child had experienced a difficult birth were seen in the subgroup of women with normal pregnancy but complicated childbirth (NPCC). This difference was even larger after use of the birth plan (SG: 5 + 6: 23.4% vs. 10.4%; p = 0.017. IG: 5 + 6: 31.2% vs. 9.8%; p = 0.001). Scores concerning fear of complications affecting the child were generally higher in the subgroups with complications compared with the normals; however, the only significant difference was when comparing the CPNC group with a birth plan with the normals (5 + 6: 41.1% vs. 14.9%; p = 0.001). The majority in all subgroups had a high degree of acceptance to suffer pain for the child's sake, except women with complicated pregnancy and normal childbirth in the standard group whose ratings were significantly lower than the normals (5 + 6: 40.3% vs. 60.6%; p = 0.029) (see Tables 7a and 7b).
The Total Experience
The majority of women (≥ 51.8%) expressed agreement with the statement that childbirth on the whole was positive. However, among women with a birth plan, significantly lower scores were seen in groups with either complicated pregnancy or complicated childbirth (CPNC and NPCC) (see Tables 7a and 7b).
Further Comparative Analysis of Subgroups
A comparison of women who received a birth plan versus women who received standard care was carried out, subgroup by subgroup. When comparing the two groups of women with normal pregnancy and childbirth (NPNC), the two groups of women with normal pregnancy and complicated childbirth (NPCC), and those with complicated pregnancy and childbirth (CPCC), no significant differences were found in any of the statements. In contrast, a difference was observed when comparing the two groups of women with complicated pregnancy and normal childbirth (CPNC). When the statement of constant fear of complications affecting the child was presented, women who were prepared with a questionnaire and an individual birth plan scored much higher than women without such an intervention (5 + 6: 41.1% vs. 14.0%; p = 0.007). They also more often expressed that they could suffer pain for the child's sake (5 + 6: 71.8% vs. 40.3%; p = 0.025).
Discussion
Some limitations in the study are obvious. The questionnaire was not previously validated statistically. However, the reviewed areas were derived from earlier qualitative studies. Further, randomization was not considered feasible, but the study controls were very close in time and similar in all respects to the women in the intervention group. Because the data collection in the control group was completed before the intervention, the later intervention would not have influenced these women and their midwives. Specifics such as demographics and pain-relief methods used during labor were not addressed on the assumption that the method of subject recruitment would result in comparable groups on these variables. Also, the specific effect of prolonged bed rest—an experience with potential impact on perceived control—was not studied because this treatment is very rare in Sweden. Finally, with the many statistical comparisons in the analysis, the risk of mass significance cannot be ignored. However, the evident pattern in the results accords well with the essential findings in the two qualitative studies (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000) of frequent negative feelings in women at high risk.
The intervention, with of the use of a questionnaire and birth plan, did not improve the childbirth experience in any subgroup. Rather, for both the intervention and standard groups, more negative feelings were expressed by women with complications either during pregnancy or childbirth. Thus, the results indicate that women at high risk are more vulnerable during pregnancy or childbirth compared to those with “normal” processes. As might be expected, they expressed more negative feelings. The surprising exception was the group of women with both complicated pregnancy and complicated childbirth who did not differ from the normals. The reason for this is not obvious. This subgroup was smaller in number, but the fact that this pattern occurred for both standard and intervention groups adds strength to the finding.
The negative effect of the birth plan is of special interest in the group with complicated pregnancy (CPNC) who nonetheless had a totally normal childbirth (i.e., no complications at all during childbirth). The overall satisfaction with childbirth was lower, they expressed higher dependency on check-ups and higher degree of objectification, and as a whole they found it more difficult to interpret body signals. Ten percent of them expressed feelings of failure, and a higher proportion of them felt severe demands compared with the normals. The most remarkable finding was that the birth-plan mothers' constant fear of complications affecting the child was three times as common as in the corresponding subgroup with standard care, as well as in all other subgroups. The majority of these women agreed to suffer pain for the child's sake. This may reflect a wish to do something to decrease the risks they perceived for the child by denying themselves pain relief and suffering for the child's sake (for similar thoughts on this topic in a more general nature, see Eriksson, 1994). Concern for the health of the child as a legitimate reason for anxiety and uncertainty has been reported both in women with high- and low-risk pregnancies (Clauson, 1996; Rubin, 1975; Stainton et al., 1992; White & Ritchie, 1984). This study's results indicate that women with high-risk pregnancies are, to a higher degree, filled with anxiety and that elements in the care may strengthen this feeling.
Women with normal pregnancy and complicated childbirth (NPCC) with a birth plan also presented more negative feelings compared to the normal group with a birth plan. The overall satisfaction was lower. To a higher degree, they felt difficulty in interpreting the body signals during the second stage. A feeling of failure was more frequent and, to a higher degree, they stated that their child experienced a difficult birth. This difference would be expected since birth was complicated. However, the difference between NPCC and normals is more pronounced in the intervention group than in the standard care group.
A negative feeling is also expressed in the statement, “My child had a difficult birth.” Because this perception was scored higher by women with a normal pregnancy but a complicated childbirth (NPCC), irrespective of type of care, it seems to be a central feeling for all such women. Because many interventions occurred during these childbirths, the reasons for this expected response are varied.
Why are the differences between women with and without complications increased when a birth plan preceded by a questionnaire is introduced? It is possible that merely taking part in the research and being stimulated to think more than usual about the situation may have subconsciously aggravated and provoked intense feelings. Without any doubt, the results clearly indicate that stimulating women to think more about their situation and to formulate these thoughts in a written birth plan should not be used as a benign standard routine. A higher degree of involvement may confuse the women and increase the anxiety level (Green et al., 1990), at least among women with complications or risk factors, possibly due to their increased vulnerability. A birth plan is not just another piece of paper in the file (Too, 1996). It is important to regularly evaluate new routines in the care of childbearing women.
Feelings of demands and worries for the child are central among women at high risk (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000). Feelings of failure may make the pregnancy difficult (Berg & Honkasalo, 2000; Jones, 1986). In the standard care group, the complicated subgroups did not differ from the group with normal conditions. But in women who had formulated a birth plan, groups with complications indicated more negative feelings compared with their respective normals. This may be because, through the routines of care that include increased medical attention, women with risk factors or complications become more aware of possible risks and, therefore, become more vulnerable if they are stimulated to think more about the coming childbirth.
The results of this study, which demonstrate that the birth plan did not improve women's sense of control during childbirth, support earlier findings (Whitford & Hillan, 1998). Further, the results show that women at high risk have the same need for control as the normals. For the staff to have control was not enough to satisfy high-risk women; the women needed to be involved themselves. They also expressed the same level of perceived control as women with normal conditions. The feelings of objectification were denied in almost the same degree as among those with normal pregnancy and childbirth. Perhaps the reason was the high degree of good relationships with the staff. The nature of a caring relationship is suggested to have a direct impact on the degree of control women feel during childbirth (Coyle, Hauck, Percival, & Kristjanson, 2001), and midwifery care is shown to influence women's feelings of being in control (Gibbins & Thomson, 2001). Shared control, a strategy that is developed when a good collaboration exists with the health professionals (Berg & Dahlberg, 1998; Berg & Honkasalo, 2000; Corbin, 1987), seems to be the best model of care for women at high risk. One aspect of control is the degree of dependency on medical check-ups. On the whole, this need was confirmed in the present study among all groups of women. However, among the birth-plan women with a complicated pregnancy and normal childbirth, it was significantly higher.
One of the reasons for the introduction of birth plans during the 1980s was that a lack of communication was cited as the most common negative feeling among childbearing women (Cartwright, 1979; Kirke, 1980; Macintyre, 1982; McIntosh, 1988). In the study described here, it is remarkable that all women, regardless of whether their condition was normal or complicated, reported such a positive experience of their relationship with midwives and physicians. The importance of a good, caring relationship has been on the agenda among health professionals in Sweden to a higher degree during recent years and, thus, the birth plan may not have the same positive significance in an overall more positive environment of care. The results indicate that, despite difficult working conditions with minimized staff resources, health professionals still can manage to prioritize the caring relationship. This is important information because support from the midwife or other person is shown to be one of the most vital factors contributing to a positive childbirth (Berg & Dahlberg, 1998; Berg et al., 1996; Jones, 1986). Additionally, the presence of a partner providing important support is strongly confirmed in this study.
Implications for Further Study
This study's results would benefit from replication in a large enough sample to control for more details such as prolonged bed rest, frequency of special check-ups (e.g., ultrasound and blood glucose level), and birth experiences (e.g., companions, medications, and frequency of specific interventions). A similar study on the outcomes of childbirth education in general is warranted since little or no research is available to suggest what types of information is most useful to which categories of mothers. In general, childbirth education has been treated as a routine, beneficial intervention. Challenging the practice of birth plans as a routine intervention for all raises the same questions about childbirth education and, thus, should be studied.
Conclusion
Women with complications either during pregnancy or childbirth seem to have more negative feelings than women with “normal” conditions. A birth plan preceded by a questionnaire appears to intensify the negative feelings in these women with complications. The result underscores that women at high risk are more vulnerable. Further, it stresses that new routines of care, such as birth plans, need to be evaluated. Health professionals have to be aware that increased attention to women at high risk and activities, such as a birth plan, that increase their awareness of possible occurrences may increase women's negative feelings.
Acknowledgments
The authors express their gratitude to George Lappas for statistical guidance. The study was funded in part by the Department of Health Sciences, University of Skövde, and the Department of Women's and Children's Health, University Hospital, Uppsala, Sweden.
References
- Berg M, Dahlberg K. A phenomenological study of women's experience of complicated childbirth. Midwifery. 1998;14:23–39. doi: 10.1016/s0266-6138(98)90111-5. [DOI] [PubMed] [Google Scholar]
- Berg M, Honkasalo M.-L. Pregnancy and diabetes—A hermeneutic phenomenological study of women's experiences. Journal of Psychosomatic Obstetrics and Gynecology. 2000;21:39–48. doi: 10.3109/01674820009075607. [DOI] [PubMed] [Google Scholar]
- Berg M, Lundgren I, Hermansson E, Wahlberg V. Women's experience of the encounter with the midwife during childbirth. Midwifery. 1996;12:11–15. doi: 10.1016/s0266-6138(96)90033-9. [DOI] [PubMed] [Google Scholar]
- Brudal L. F. 1985. Födandets psykologi (The psychology of childbirth). Vällingby, Sweden: Natur och kultur. [Google Scholar]
- Cartwright A. 1979. The dignity of labour. Cambridge, MA: Travistock Publications. [Google Scholar]
- Clauson M. Uncertainty and stress in women hospitalised with high-risk pregnancy. Clinical Nursing Research. 1996;5:309–325. doi: 10.1177/105477389600500306. [DOI] [PubMed] [Google Scholar]
- Corbin J. M. Women's perceptions and management of a pregnancy complicated by chronic illness. Health Care Women Int. 1987;8:317–337. doi: 10.1080/07399338709515797. [DOI] [PubMed] [Google Scholar]
- Coyle K, Hauck Y, Percival P, Kristjanson L. Normality and collaboration: Mothers' perceptions of birth centre versus hospital care. Midwifery. 2001;17:182–193. doi: 10.1054/midw.2001.0256. [DOI] [PubMed] [Google Scholar]
- Eriksson K. 1994. Den lidande människan (The suffering human). Stockholm: Liber. [Google Scholar]
- Gibbins J, Thomson A. M. Women's expectations and experiences of childbirth. Midwifery. 2001;17:302–313. doi: 10.1054/midw.2001.0263. [DOI] [PubMed] [Google Scholar]
- Green J. M, Coupland V. A, Kitzinger J. V. Expectations, experiences, and psychological outcomes of childbirth: A prospective study of 825 women. Birth. 1990;17:15–24. doi: 10.1111/j.1523-536x.1990.tb00004.x. [DOI] [PubMed] [Google Scholar]
- Halldórsdóttir S. Caring and uncaring encounters in nursing and health care—Developing a theory. 1996. (Doctoral dissertation, Linköping University, 1996). Linköping University Medical Dissertations No. 493. [DOI] [PubMed]
- Jones M. B. The high-risk pregnancy. 1986. In S. H. Johnson (Ed.), Nursing assessment and strategies for the family at risk (2nd ed., pp. 11–128). Philadelphia: Lippincott.
- Kirke P. N. Mothers' views of obstetric care. British Journal of Obstetrics and Gynaecology. 1980;87:1029–1033. doi: 10.1111/j.1471-0528.1980.tb04468.x. [DOI] [PubMed] [Google Scholar]
- Kitzinger S. 1983. The new good birth guide. London: Harmondsworth. [Google Scholar]
- Kitzinger S. 1988. Freedom and choice in childbirth. London: Penguin. [Google Scholar]
- Kitzinger S. Sheila Kitzinger's letter from England: Birth plans. Birth. 1992;19:36–37. doi: 10.1111/j.1523-536x.1992.tb00373.x. [DOI] [PubMed] [Google Scholar]
- Lagerkrantz E. Psykologiska synpunkter på graviditet och förlossning (Psychological aspects on pregnancy and childbirth). Läkartidningen. 1974;71:2064–2066. [PubMed] [Google Scholar]
- Lundgren I, Dahlberg K. Women's experience of pain during childbirth. Midwifery. 1998;14:105–110. doi: 10.1016/s0266-6138(98)90007-9. [DOI] [PubMed] [Google Scholar]
- Lundgren I, Wahlberg V. The experience of pregnancy: A hermeneutical/phenomenological study. Journal of Perinatal Education. 1999;8(3):12–20. doi: 10.1624/105812499X87196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S. Communication between pregnant women and their medical and midwifery attendant. Midwives Chronicle. 1982;95:387–394. [PubMed] [Google Scholar]
- Marut J. S, Mercher R. T. Comparison of primiparas' perceptions of vaginal and caesarean birth. Nursing Research. 1979;28:260–266. [PubMed] [Google Scholar]
- McCain G. C, Deatrick J. A. The experience of high-risk pregnancy. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1994;23:421–427. doi: 10.1111/j.1552-6909.1994.tb01899.x. [DOI] [PubMed] [Google Scholar]
- McIntosh J. Women's views of communication during labour and delivery. 1988. Midwifery, 4, 166–170. [DOI] [PubMed]
- Mercher R. T. 1990. Parents at risk. New York: Springer Publication Company Inc. [Google Scholar]
- Morris-Thompson P. Consumers, continuity and control. Nursing Times. 1992;88:29–31. [PubMed] [Google Scholar]
- Oakley A. Social consequences of obstetric technology—The importance of measuring soft outcomes. Birth. 1993;10:99–108. doi: 10.1111/j.1523-536x.1983.tb01408.x. [DOI] [PubMed] [Google Scholar]
- Rubin R. Maternal tasks in pregnancy. Journal of Advanced Nursing. 1975;1:367–376. doi: 10.1111/j.1365-2648.1976.tb00921.x. [DOI] [PubMed] [Google Scholar]
- Simkin P. Just another day in a woman's life? Women's long-term perceptions of their first birth experience: Part I. Birth. 1991;18:203–210. doi: 10.1111/j.1523-536x.1991.tb00103.x. [DOI] [PubMed] [Google Scholar]
- Simkin P. Just another day in a woman's life? Part II: Nature and consistency of women's long-term memories of their first birth experience. Birth. 1992;19:64–81. doi: 10.1111/j.1523-536x.1992.tb00382.x. [DOI] [PubMed] [Google Scholar]
- Socialstyrelsen. 1996. Hälsovård före, under och efter graviditeten. (National Board of Health and Welfare: Health care before, during and after pregnancy). SoS-rapport 1996:7. Stockholm, Sweden: Author. [Google Scholar]
- Socialstyrelsen. 2001. Handläggning av normal förlossning. (National Board of Health and Welfare: Normal birth-state of the art). Stockholm, Sweden: Author. [Google Scholar]
- Stainton M. C, McNeil D, Harvey S. Maternal tasks of uncertain motherhood. Maternal-Child Nursing Journal. 1992;3:113–123. [PubMed] [Google Scholar]
- Too S.-K. Do birth plans empower women? A study of midwives' views. Nursing Standard. 1996;10:33–37. doi: 10.7748/ns1996.04.10.31.33.c6222. [DOI] [PubMed] [Google Scholar]
- White M, Ritchie J. Psychological stressors in antepartum hospitalisation. Maternal-Child Nursing Journal. 1984;13:47–56. [PubMed] [Google Scholar]
- Whitford H. M, Hillan E. M. Women's perceptions of birth plan. Midwifery. 1998;14:248–253. doi: 10.1016/s0266-6138(98)90097-3. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 1996. Care in normal birth: A practical guide (Report of the Technical Working Group). Geneva, Switzerland: Author. [PubMed] [Google Scholar]