Abstract
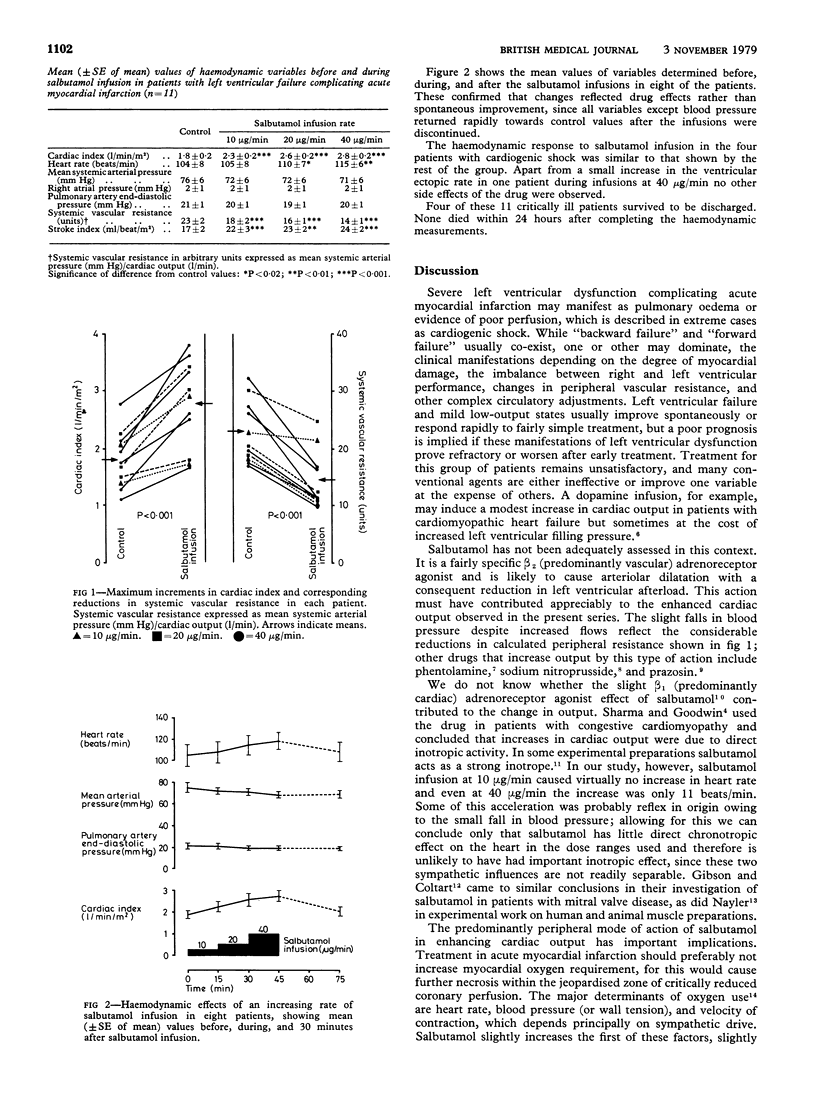
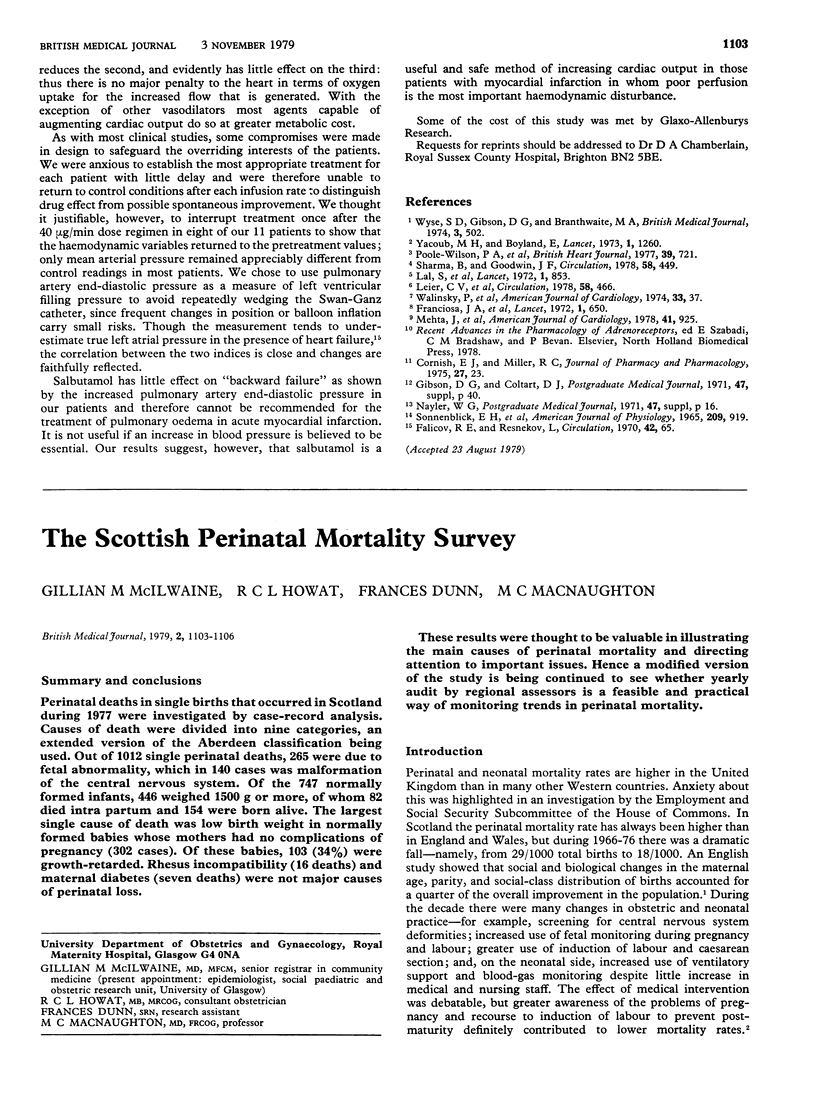
The haemodynamic effects of salbutamol infusions at rates of 10,20, and 40 micrograms/min were measured in 11 patients with acute myocardial infarction complicated by left ventricular failure. Four patients also had cardiogenic shock. Consistent increases were observed in cardiac outputs at all doses (up to 56% at 40 micrograms/min), while the mean systemic arterial pressure fell slightly (average 5 mm Hg), implying a reduction in peripheral vascular resistance. Changes in right atrial pressure and indirect left atrial pressure (measured as pulmonary artery end-diastolic pressure) were small and not significant. Analysis of data from individual patients showed that the greatest increment in cardiac output was reached at 10 micrograms/min in two cases, 20 microgram/min in three, and 40 micrograms/min in the remaining six. Heart rate at these doses increased by an average of only 10 beats/min. Salbutamol failed to reduce left ventricular filling pressure and cannot be recommended for the treatment of pulmonary oedema in acute myocardial infarction. The increase in cardiac output, however, was considerable, so that the drug may be important in the management of low-output states. This action is probably a result of peripheral arteriolar dilatation (itself a result of beta 2-adrenoreceptor stimulation) and is achieved with little alteration in the principal determinants of myocardial oxygen requirement.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Falicov R. E., Resnekov L. Relationship of the pulmonary artery end-diastolic pressure to the left ventricular end-diastolic and mean filling pressures in patients with and without left ventricular dysfunction. Circulation. 1970 Jul;42(1):65–73. doi: 10.1161/01.cir.42.1.65. [DOI] [PubMed] [Google Scholar]
- Franciosa J. A., Limas C. J., Guiha N. H., Rodriguera E., Cohn J. N. Improved left ventricular function during nitroprusside infusion in acute myocardial infarction. Lancet. 1972 Mar 25;1(7752):650–654. doi: 10.1016/s0140-6736(72)90460-6. [DOI] [PubMed] [Google Scholar]
- Lal S., Savidge R. S., Davies D. M., Ali M. M., Soni V. Intravenous salbutamol and cardiogenic shock. Lancet. 1972 Apr 15;1(7755):853–854. doi: 10.1016/s0140-6736(72)90846-x. [DOI] [PubMed] [Google Scholar]
- Leier C. V., Heban P. T., Huss P., Bush C. A., Lewis R. P. Comparative systemic and regional hemodynamic effects of dopamine and dobutamine in patients with cardiomyopathic heart failure. Circulation. 1978 Sep;58(3 Pt 1):466–475. doi: 10.1161/01.cir.58.3.466. [DOI] [PubMed] [Google Scholar]
- Mehta J., Iacona M., Feldman R. L., Pepine C. J., Conti C. R. Comparative hemodynamic effects of intravenous nitroprusside and oral prazosin in refractory heart failure. Am J Cardiol. 1978 May 1;41(5):925–930. doi: 10.1016/0002-9149(78)90735-x. [DOI] [PubMed] [Google Scholar]
- Poole-Wilson P. A., Lewis G., Angerpointer T., Malcolm A. D., Williams B. T. Haemodynamic effects of salbutamol and nitroprusside after cardiac surgery. Br Heart J. 1977 Jul;39(7):721–725. doi: 10.1136/hrt.39.7.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma B., Goodwin J. F. Beneficial effect of salbutamol on cardiac function in severe congestive cardiomyopathy. Effect on systolic and diastolic function of the left ventricle. Circulation. 1978 Sep;58(3 Pt 1):449–460. doi: 10.1161/01.cir.58.3.449. [DOI] [PubMed] [Google Scholar]
- Sonnenblick E. H., Ross J., Jr, Covell J. W., Kaiser G. A., Braunwald E. Velocity of contraction as a determinant of myocardial oxygen consumption. Am J Physiol. 1965 Nov;209(5):919–927. doi: 10.1152/ajplegacy.1965.209.5.919. [DOI] [PubMed] [Google Scholar]
- Wyse S. D., Gibson D. G., Branthwaite M. A. Haemodynamic effects of salbutamol in patients needing circulatory support after open-heart surgery. Br Med J. 1974 Aug 24;3(5929):502–503. doi: 10.1136/bmj.3.5929.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yacoub M. H., Boyland E. Cardiovascular effects of intravenous salbutamol after open heart operations. Lancet. 1973 Jun 2;1(7814):1260–1261. doi: 10.1016/s0140-6736(73)90583-7. [DOI] [PubMed] [Google Scholar]



