Abstract
Objective
Physicians-in-training today are learning in an ethical environment that is unprecedented in its complexity. There is a call for new approaches in preparing medical students and residents for the ethical and professional issues they will encounter. The perspectives of physicians-in-training at different levels regarding the level of curricular attention needed for emerging bioethics concepts, practical informed consent considerations, and the care of special populations are unknown.
Method
The authors performed a hypothesis-driven, confidential survey study to assess perceived needs and preferences among medical students and residents related to medical ethics education at the University of New Mexico School of Medicine.
Results
A total of 336 physicians-in-training volunteered (62% response rate). Overall, strong interest was expressed for increased curricular attention to the domains of bioethics principles, informed consent, and care of special populations. Women students expressed greater interest generally. For certain domains, clinical students expressed relatively less curricular need and psychiatry and primary care residents expressed relatively greater curricular need. Two of the four hypotheses were supported, a third received partial support, and a fourth was not supported by the findings.
Discussion
To be valuable and effective, new ethics curricular approaches must be responsive to the current complex ethical environment and attentive to the preferences of medical students and residents of both genders, at different stages of training, with different patient care responsibilities. This hypothesis-driven study provides guidance for the inclusion of novel and important ethics domains in training curricula across medical school and diverse residency programs.
There have been significant changes in the health care system since bioethics education first became an essential part of medical school curricula in the 1980s.1 The extraordinary growth in technology, the dominance of managed care in health delivery systems, the expanding cultural diversity of the American population, and changing commitment to the care of underserved and uninsured groups by academic medical centers have raised novel ethical questions and new educational needs.2,3 Physicians-in-training today are learning in an ethical environment that is characterized by exceptional complexity.4
Across undergraduate and graduate medical education, there is a call for more substantive preparation for the ethical challenges encountered by medical students and residents during training and in future professional duties.5–9 There have been significant efforts to respond to this imperative in medical education, and emerging approaches differ from prior endeavors in several respects.
First, new ethics education approaches are informed by an evolving understanding of professionalism and core bioethics principles. The recently issued position document, “Medical Professionalism in the New Millennium: A Physician Charter” by the American Board of Internal Medicine, the American College of Physicians, and the European Federation of Internal Medicine signals a major shift in thinking about the bioethical principles underlying health care in the United States and Europe. In this new formulation, the responsibilities of the physician combine traditional obligations to the individual patient with substantial duties to society.10 Some have characterized the trend in philosophical bioethics over the past two decades as the progression from beneficence, to autonomy, to justice and there is a corresponding evolution in the themes in medical ethics curricula.11
Second, new curricular approaches focus on demonstrable domains of professional competence, i.e., measurable knowledge and observable skills essential to fulfilling optimal standards of care and representing the ideals of the profession of medicine behaviorally.12 In 1999, the Accreditation Council for Graduate Medical Education introduced a new mandate that required each residency program in each specialty across the United States, in order to be accredited, show appropriate measures of competence in six domains, all of which contain ethically important components, with an entire domain explicitly dedicated to professionalism.13 This requirement has long been foreshadowed in the published ethics education literature.1,14,15 For example, Sulmasy et al.16 reported that an ethics education curriculum focused on treating patients with do-not-resuscitate orders was successful in improving residents’ attention to writing do-not-resuscitate orders, and the rationale and consent for obtaining such orders increased. Similarly, we utilized a standardized patient scenario to evaluate the performance of 79 seniors to obtain informed consent for HIV testing. Ninety-six percent of students demonstrated competence in the station.16,17 In this new model, medical students and residents must demonstrate the ability to perform certain professional duties, such as obtaining informed consent and providing astute and sensitive care to persons who derive from distinct cultural and ethnic backgrounds, who are members of defined “special populations,” or who have different potential sources of vulnerability in the clinical situation (e.g., those who are uninsured, immigrant, rural, or terminally ill).17–21
Third, new approaches to ethics and professionalism education reflect greater attunement to sequential developmental issues experienced by physicians-in-training.22,23 This effort is reflected in “white coat ceremonies” that have been introduced in many medical schools and have stimulated an increased focus on self-appraisal and personal health care in professional development.24–27 Developmental attunement has been viewed as necessary because of emerging evidence that medical students and residents face unique ethical conflicts that are related to their stage of training and that ethics training needs and preferences also evolve.28–31 Residents in several studies have expressed a preference for clinically oriented ethics education to prepare them for the day-to-day ethical tasks encountered in their work duties.32,33 There are also a series of more worrisome studies suggesting that the training process fosters cynicism and physical, psychological, and moral exhaustion, which interferes with ethical conduct and decision making by physicians-in-training over time.1,34–37
Fourth, there is increasingly greater emphasis on the distinct ethical problems encountered in each primary care and specialty field.33,38–40 Jacobson et al.41 surveyed 323 internal medicine residents in six programs on their preferences for ethics education and found that legal and end-of-life issues were two of the topics identified as meriting more attention among these advanced, specialized trainees. More recently, a structured review of surgery residencies identified five areas requiring more instruction: withdrawing and withholding treatment, advance directives, do-not-resuscitate orders, informed consent, and communicating bad news. Nearly all of the 20 surgical residents surveyed felt ethics was important and felt their confidence in addressing ethical issues improved after a specially designed teaching program targeting the five areas.42 A study of pediatric residents in five training programs demonstrated heightened need for attention to withholding and withdrawing life support, child abuse and neglect, and disputes about patient care occurring across hospital services.43
Finally, data gathered over the past three decades suggest that key differences exist in how men and women professionals approach health care ethics decision making.44–46 Several studies indicate that women physicians-in-training perceive greater need for ethics preparation, value it more, and see benefit in a more diverse set of educational methods than men.47,48 For example, a study involving 181 psychiatry residents in 10 training programs, conducted in part by one of us (L.W.R.), showed that women had stronger general interest in ethics training, across 26 specific curricular topics, and identified multiple valuable learning strategies.33 In a qualitative project, Shapiro and Miller49 asked 92 medical students to identify and resolve a clinical ethical dilemma. Narrative analysis revealed that the women students were more focused on psychosocial and societal issues, and they used the rights of patients and families as a basis for argument. Beyond content differences, they also used both abstract and personal modes of analysis. Men, in contrast, gave more emphasis to issues of responsibility, authority, and control, utilizing utilitarian arguments and engaging in more formal abstract analytical methods.
Major academic organizations and medical education leaders have begun to respond to these important new directions in ethics education, but there are many challenges and unresolved curricular issues.5,23,50 For instance, there is little consensus on how to implement the requirements of the new ACGME “Professionalism” competence domain, on how to optimally address the erosion of ethically important attitudes during training, and the negative impact of the “hidden, informal, and disavowed” curriculum in which students and residents are given negative and conflicting messages about ethical conduct in medicine.12,30,51,52 Moreover, a recent study of syllabi on ethics education from 87 medical schools found great heterogeneity in objectives, readings, assessments, teaching, and content methods, underscoring the need for improved curriculum development.53 Several studies have shown that medical students and residents do not experience past and current approaches to medical ethics and professionalism as sufficient to help them address the challenges they face.33,54,55 Finally, there are several gaps in the existing literature that help to represent the perspectives of physicians-in-training, the most critically important stakeholders, on “best practices” for medical ethics and professionalism preparation.
To date there has not been a systematic study assessing, in a single analysis, the perspectives of physicians-in-training across different levels, including residents from different postgraduate specialty areas, regarding several areas that have emerged as especially important in light of the current ethical environment. These areas are 1) the role of bioethics principles, including more “justice”-related concepts, in curricular training; 2) salient considerations in obtaining informed consent such as the involvement of surrogate decision-makers, approaches to informed refusal, and informed consent with individuals who speak a different language; and 3) ethical challenges in caring for the needs of persons who derive from special groups (e.g., children, immigrants) or who have certain sources of vulnerability (e.g., abuse and domestic violence victims). Given the current ethical training environment and evolving trends in ethics education, understanding the ideas and preferences of medical students and residents will be instrumental in the construction of novel, responsive, and responsible curricula.
For this reason, we performed a survey at the University of New Mexico School of Medicine to better understand these issues. We hypothesized that 1) medical students and residents would endorse the need for greater curricular attention to bioethics principles, informed consent topics, and special population needs; 2) women would more strongly endorse these curricular needs; 3) psychiatry residents would more strongly endorse curricular needs than other residents; and 4) there would be increased perceived need in these ethics curricular domains among trainees who were at more advanced stages of training.
METHOD
Participants and Context
All medical students (N = 308) and PGY1-3 residents (N = 233) at the University of New Mexico School of Medicine were invited in the spring of 2000 to participate in this survey study. Professionalism and ethics at the University of New Mexico School of Medicine are taught through didactics, small group sessions, and individual supervision. We estimate that medical students received 4–12 hours of formal instruction on ethics and professionalism-related topics each year, with residents receiving 2–4 hours of such instruction. We cannot accurately estimate the number of hours of individual supervision that gave emphasis to these topics. At the time of this study, professionalism and ethics were evaluated during three performance-based examinations of medical students.56,57 The performance-based examinations encompassed topics such as confidentiality, informed consent, health disparities, and access to care. Professionalism and ethics were part of all supervisor evaluations for medical students and residents, consistent with the Accreditation Council on Graduate Medical Education competence guidelines.
Survey and Procedure
Three of us (L.W.R., T.D.W., C.M.A.G.) developed a survey to assess views of professionalism and ethics preparation and their assessment in medical education. The survey included eight demographic questions and 124 content items in 10 domains. Content items were each rated on 9-point scales appropriately labeled. The domains of education needs concerning bioethics principles, informed consent, and care of vulnerable patients are reported here, with other elements (e.g., preferred methods of learning) published elsewhere.58
The survey was sent via campus mail with a cover letter indicating the purpose of the study, confidentiality procedures, and institutional review board approval. Two follow-up mailings were sent to nonrespondents at 1-month intervals. Medical students received $10 in compensation for time and effort; residents received $20.
Data Analysis
A random subset of 30 respondents completed the survey again 7 weeks later to assess reliability. Retest correlations ranged from 0.03 to 0.79 (mean r = 0.52, p<0.05), with correlations above 0.32 for 20 of 22 items.
Responses were subjected to repeated measures multivariate analyses of variance (MANOVA) with items as repeated measures and gender and training level (preclinical medical students versus clinical medical students versus residents) as independent variables. Further analyses examined residency program group (psychiatry versus other specialties versus primary care programs) as additional independent variables.
RESULTS
Respondent Characteristics
Sixty-two percent of trainees (N = 336) responded (Table 1). Fifty-one percent of the respondents were women; 20% were Hispanic American, 61% were “Anglo/white,” and 19% were other (e.g., African American [1%], Asian American [5%], and Native American [4%]) or unreported. Training level groups did not differ significantly by gender or ethnicity. The proportion of respondents married or living with a partner increased with advancing training level (preclinical students: 40%, clinical students: 61%, residents: 63%; χ2 = 13.51, df = 2, p<0.01) as did mean age (27.8 [SD = 4.0], 29.5 [SD = 4.7], and 32.5 [SD = 4.8], respectively; F = 31.23, df = 2, 330, p<0.01). Fifty percent of residents were in primary care departments, 13% were in psychiatry, and 38% were in other specialty departments.
TABLE 1.
Characteristics of Physician-in-Training Survey Respondents, by Gender
|
Gender |
||||
|---|---|---|---|---|
|
Women (N = 171) |
Men (N = 165) |
|||
| Characteristic | N | % | N | % |
| Training level | ||||
| Preclinical phase medical students | 59 | 35 | 39 | 23 |
| Clinical phase medical students | 50 | 29 | 52 | 32 |
| Residents, PGY 1–3 | 62 | 36 | 74 | 45 |
| Resident departmenta | ||||
| Primary careb | 36 | 58 | 32 | 43 |
| Psychiatry | 10 | 16 | 7 | 10 |
| Other specialtiesc | 16 | 26 | 35 | 47 |
| Ethnicity | ||||
| Hispanic American | 38 | 22 | 30 | 18 |
| Anglo/white | 102 | 60 | 103 | 62 |
| Other or not reported | 31 | 18 | 32 | 19 |
Significant gender difference in resident department composition (χ2 = 6.84, df = 2, p<0.04).
Family practice, internal medicine, and pediatrics.
Anesthesiology, emergency medicine, obstetrics/gynecology, pathology, radiology, and surgery.
Educational Needs for Complex Issues Surrounding Bioethics Principles
On a scale of 1–9 (in which 1 = “much less,” 5 = “same,” and 9 = “much more”), trainees rated educational attention needed for the complex ethical, social, and legal issues surrounding bioethics principles compared with the amount currently provided (Table 2). Trainees indicated a need for more attention to all of the principles (overall mean = 6.06), with the most attention requested for the principle of respect for human dignity, some requested for compassion for suffering, community responsibility, and nondiscrimination, and the least additional attention requested for justice, truth-telling, scientific integrity, and respecting the law.
TABLE 2.
Physician-in-Training Ratings of Educational Attention Needs for the Complex Ethical, Social, and Legal Issues Surrounding Bioethics Principles
|
Gender |
|||||||
|---|---|---|---|---|---|---|---|
|
Women (N = 168) |
Men (N = 163) |
Overall (N = 331) |
|||||
| Bioethics Principle | Mean Ratinga | SD | Mean Ratinga | SD | Differenceb | Mean Ratinga | SD |
| Respect for human dignity | 6.64 | 1.55 | 6.17 | 1.60 | 0.30 | 6.41 | 1.57 |
| Compassion for suffering | 6.38 | 1.66 | 6.03 | 1.71 | 0.23 | 6.21 | 1.69 |
| Responsibility to improve community | 6.48 | 1.59 | 5.87 | 1.64 | 0.39* | 6.18 | 1.61 |
| Non-discrimination | 6.50 | 1.71 | 5.79 | 1.76 | 0.46** | 6.15 | 1.73 |
| Justice | 6.15 | 1.41 | 5.87 | 1.45 | 0.18 | 6.01 | 1.43 |
| Truth-telling and honesty | 6.12 | 1.45 | 5.68 | 1.49 | 0.29 | 5.90 | 1.47 |
| Scientific integrity and research | 6.04 | 1.47 | 5.66 | 1.52 | 0.25 | 5.85 | 1.49 |
| Respecting the law | 5.93 | 1.42 | 5.71 | 1.46 | 0.14 | 5.82 | 1.44 |
| Meanc | 6.28 | 1.14 | 5.85 | 1.18 | 0.37*** | 6.06 | 1.16 |
Represents response on a 9-point scale indicating attention needed (1 = ‘‘much less’’ to 9 = ‘‘much more’’) relative to the amount currently provided.
Standardized mean difference (pooled SD = 1.56) for gender comparisons for an item. Gender means are significantly different for indicated items at p<0.10 (*), p<0.05 (**), or p<0.01(***) by Fisher’s least significant difference for items and by analysis main effect for means.
From a MANOVA with item as a repeated measure and gender and training level as independent variables. Significant main effects were seen for gender (F = 11.60, df = 1, 325, p<0.01; d = 0.37) and item (F = 9.84, df = 7, 319, p<0.0001; maximum Cohen’s d = 0.38). Overall item differences > 0.19 and within-gender item differences >0.26 are significantly different (p<0.05) by Fisher’s least significant difference.
Women expressed greater need than did men for additional education on all topics (Table 2), particularly for nondiscrimination (p<0.05) and responsibility to improve community (p<0.09). Clinical phase medical students expressed marginally less need for additional attention to principles (mean = 5.86) than did preclinical medical students (mean = 6.14) or residents (mean = 6.20) (main effect of training level: F = 2.67, df = 2, 325, p<0.08; maximum d = 0.30).
Educational Needs for Complex Issues Surrounding Informed Consent
On a scale of 1–9 (in which 1 = “much less,” 5 = “same,” and 9 = “much more”), trainees rated educational attention needed for the issues surrounding informed consent compared with the amount currently provided (Table 3). Trainees indicated need for more attention to all issues, with the most additional attention requested for the issues of obtaining informed consent from patients with compromised decisional capacity, surrogate decision-makers, non-English speaking patients, and patients declining recommended treatment; some additional attention for negotiating alternatives and withholding information; and the least additional attention for deciding how much clinical information to share with decisionally capable patients.
TABLE 3.
Physician-in-Training Ratings of Educational Attention Needs for Issues Surrounding Informed Consent
|
Gender |
|||||||
|---|---|---|---|---|---|---|---|
|
Women (N = 167) |
Men (N = 161) |
Overall (N = 328) |
|||||
| Informed Consent Issue | Mean Ratinga | SD | Mean Ratinga | SD | Differenceb | Mean Ratinga | SD |
| Obtaining informed consent from patients whose decisional capacity is compromised | 7.14 | 1.41 | 6.78 | 1.46 | 0.25 | 6.96 | 1.43 |
| Obtaining informed consent or refusal from surrogate decision-makers | 7.24 | 1.34 | 6.66 | 1.38 | 0.41* | 6.95 | 1.36 |
| Obtaining informed consent from non-English speaking patients | 7.19 | 1.44 | 6.67 | 1.49 | 0.37 | 6.93 | 1.47 |
| Obtaining informed refusal from patients who decline recommended treatment | 7.25 | 1.34 | 6.57 | 1.39 | 0.49** | 6.91 | 1.37 |
| Reviewing alternatives to recommended treatment | 6.86 | 1.43 | 6.46 | 1.48 | 0.29 | 6.66 | 1.45 |
| Deciding when to withhold information | 6.86 | 1.36 | 6.18 | 1.40 | 0.49** | 6.52 | 1.38 |
| Deciding how much clinical information to share | 6.61 | 1.24 | 5.99 | 1.28 | 0.44* | 6.30 | 1.26 |
| Obtaining informed consent from patients who are capable of making decisions | 6.27 | 1.44 | 5.99 | 1.49 | 0.20 | 6.13 | 1.47 |
| Meanc | 6.93 | 1.04 | 6.41 | 1.08 | 0.49*** | 6.67 | 1.06 |
Represents response on a 9-point scale indicating attention needed (1 = ‘‘much less’’ to 9 = ‘‘much more’’) relative to the amount currently provided.
Standardized mean difference (pooled SD = 1.40) for gender comparisons for an item. Gender means are significantly different for indicated items at p<0.10 (*), p<0.05 (**), or p<0.01(***) by Fisher’s least significant difference for items and by analysis main effect for means.
From a MANOVA with item as a repeated measure and gender and training level as independent variables. Significant main effects were seen for gender (F = 19.32, df = 1, 322, p<0.0001; d = 0.49), item (F = 29.58, df = 7, 316, p<0.0001; maximum d = 0.59), and training level (F = 3.66, df = 2, 322, p<0.03; maximum d = 0.36). There was also a significant item-by-gender interaction (F = 2.06, df = 7, 316, p<0.05). Overall item differences >0.17 and within-gender item differences >0.24 are significantly different (p<0.05) by Fisher’s least significant difference.
Women expressed greater need for additional education than did men for all topics (Table 3), with the widest differences concerning patients declining recommended treatment (p<0.04), deciding when to withhold information (p<0.04), deciding how much information to share (p<0.06), and surrogate decision-makers (p<0.08). There was also a significant training level effect: clinical phase medical students and residents expressed slightly less need for additional education attention to informed consent issues than did preclinical medical students.
Educational Needs for Complex Issues Surrounding Vulnerable Populations
On a scale of 1–9 (in which 1 = “much less,” 5 = “same,” and 9 = “much more”), trainees rated educational attention needed for the complex ethical, social, and legal issues surrounding vulnerable populations compared with the amount currently provided (Table 4). Trainees indicated need for more attention for all vulnerable groups, with the most additional attention to abused children and situations of domestic violence, and chronically, critically, or terminally ill patients; some additional attention for patients with potentially stigmatizing illnesses and children, adolescents, elderly and pregnant patients, and patients who are indigent, non-English speaking, from other cultures, or in rural areas; and the least additional attention for adult men and women.
TABLE 4.
Physician-in-Training Ratings of Educational Attention Needs for the Complex Ethical, Social, and Legal Issues Surrounding Care of Special Populations Compared With Adults in General
|
Gender |
|||||||
|---|---|---|---|---|---|---|---|
|
Women (N = 163) |
Men (N = 160) |
Overall (N = 323) |
|||||
| Special Population | Mean Ratinga | SD | Mean Ratinga | SD | Differenceb | Mean Ratinga | SD |
| Abused children and situations of domestic violence (alpha = 0.84) | 7.29 | 1.30 | 6.86 | 1.33 | 0.36 | 7.08 | 1.31 |
| Chronically, critically, and terminally ill patients (alpha = 0.89) | 6.98 | 1.28 | 6.52 | 1.31 | 0.39* | 6.75 | 1.29 |
| Patients with potentially stigmatizing illnesses (HIV,infectious diseases with public health consequences, mental illness, suicidal, violent, substance abuse, or at risk forgenetic disorders) (alpha = 0.88) | 6.76 | 1.03 | 6.21 | 1.06 | 0.46** | 6.48 | 1.05 |
| Children, adolescents, elderly, and pregnant patients (alpha = 0.83) | 6.60 | 1.08 | 6.14 | 1.11 | 0.38* | 6.37 | 1.09 |
| Patients who are indigent, non-English speaking, from other cultures, or in rural areas (alpha = 0.83) | 6.45 | 1.19 | 5.99 | 1.22 | 0.39* | 6.22 | 1.20 |
| Adults (women and men) (alpha = 0.68) | 6.12 | 1.14 | 5.77 | 1.17 | 0.30 | 5.94 | 1.15 |
| Meanc | 6.70 | 0.97 | 6.25 | 1.00 | 0.46*** | 6.47 | 0.99 |
Represents response on a 9-point scale indicating attention needed (1 = ‘‘much less’’ to 9 = ‘‘much more’’) relative to the amount currently provided.
Standardized mean difference (pooled SD = 1.19). Gender means are significantly different for indicated items at p<0.10 (*), p<0.05 (**), or p<0.01(***) by Fisher’s least significant difference for items and by analysis main effect for means.
From a MANOVA with item as a repeated measure and gender and training level as independent variables. Significant main effects were seen for gender (F = 16.96, df = 1, 317, p<0.0001; d = 0.46), item (F = 70.94, df = 5, 313, effect p<0.0001; maximum d = 0.96), and training level (F = 2.88, df = 2, 317, p<0.06; d = 0.30). Overall item differences >0.12, and within-gender item differences >0.17 are significantly different (p<0.05) by Fisher’s least significant difference.
Women expressed greater need for additional education than did men for all special or vulnerable populations (Table 4), particularly for patients with potentially stigmatizing illnesses (p<0.04); chronically, critically, and terminally ill patients (p<0.09); children, adolescents, elderly, and pregnant patients (p<0.09); and patients who are indigent, non-English speaking, from other cultures, or in rural areas (p<0.09). There was also a significant training level effect: clinical phase medical students and residents expressed slightly less need for additional education attention to vulnerable populations than did preclinical medical students.
Residency Program Comparisons
Resident trainee responses in the domains of education needs concerning bioethics principles, informed consent, and care of vulnerable patients were analyzed with residency program group (psychiatry versus other specialties versus primary care programs) and gender as independent variables. Overall mean ratings for bioethics principles (items in Table 2) did not reach significant differences across program groups (psychiatry: 6.42, primary care: 6.24, other specialties: 5.89; maximum d = 0.47, p<0.15). Overall mean ratings for informed consent topics (items in Table 3) also generalized across program groups (psychiatry: 6.78, primary care: 6.68, other specialties: 6.27; maximum d = 0.48, p<0.09). On the other hand, residents in primary care and psychiatry programs indicated greater need for additional education concerning care of persons who derive from special groups or have heightened sources of vulnerability (primary care: 6.55, psychiatry: 6.62) than did residents in other specialty programs (overall mean rating: 6.04) (maximum d = 0.58, p<0.02). Overall, as noted in Figure 1, there was an ordering pattern in which the expressed interest in additional curricular training was greatest among psychiatry residents followed by primary care and other specialty residents.
FIGURE 1. Residency Program Differences in Ratings of Educational Attention Needs for the Complex Ethical, Social, and Legal Issues Surrounding Care of Special Populations.
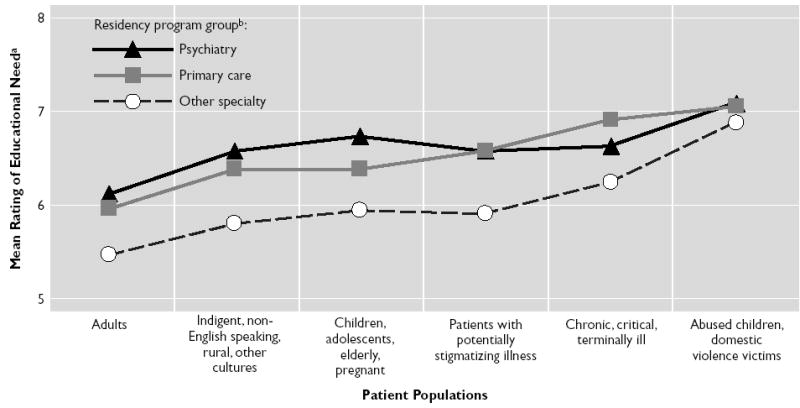
aRated on a 9-point scale indicating attention needed (1 = “much less” to 9 = “much more”) relative to the amount currently provided. Means are from a MANOVA with method as a repeated measure and residency group and gender as independent variables. Residency group main effect p<0.02.
bPrimary care departments are family practice, pediatrics, and internal medicine; other specialty departments are anesthesiology, emergency medicine, obstetrics/gynecology, pathology, radiology, and surgery.
DISCUSSION
To prepare medical students and residents for the ethical challenges they face now and will encounter in the future, ethics curricula will incorporate an evolving understanding of bioethics, demonstrable competence in performing ethically important tasks, professional developmental issues, specialty-specific training, and differential values and learning preferences of students. This study uniquely contributes to this constructive process for two reasons. It explicitly assesses stakeholder perspectives at three distinct developmental stages of training in a single analysis and permits the testing of hypotheses that are useful in crafting valuable educational approaches. It also focuses on topics that have not been previously addressed in the published literature but are reflective of the actual issues and conflicts extant in the current ethical environment. In this section, we will organize our comments around the four hypotheses informing our study. We found full support for two of our four hypotheses, partial support for a third, and the fourth hypothesis was not supported by our findings.
Endorsement of Overall Curricular NeedFully Supported Hypothesis
Medical students and residents strongly expressed their interest in greater curricular attention to bioethics principles, informed consent-related topics, and special population issues in their training. The high ratings on these items indicate strong support for our hypothesis. The global impression of perceived importance of, and increased need for, ethics preparation among early career physicians replicates findings of other studies.33,41–43,59,60 Traditional topics such as respect for human dignity and compassion for suffering were seen as important, as were several topics related to expanded professional duties in society including responsibility to community, nondiscrimination, justice, truth-telling and honesty, and respecting the law. Scientific integrity and research ethics issues were also ranked as requiring greater emphasis.
It is interesting that every informed consent-related topic was endorsed as requiring more curricular attention. This set encompassed several practical clinical ethics challenges, including obtaining informed consent with persons with decision-making deficits, with surrogate decision makers, with persons who do not speak English, and with persons who decline recommended treatment. Given our aging, more culturally diverse, and often more proactive patient population, each of these issues will increase in importance in coming years. On an encouraging note, the physician-in-training responses to subtler informed consent issues—such as discussions around treatment alternatives, deciding when to withhold information, and deciding how much information to share—reveal that our early career colleagues do not view informed consent merely as a procedure by which a signature is obtained.
The perceived needs around the care of special populations and persons who have sources of vulnerability in the clinical context were considerable. The increased attention to health care disparity issues nationally has heightened awareness of the challenges inherent to the care of these unique patient groups.61 Medical students and residents identified the need for greater ethics preparation in caring for abused children, persons affected by domestic violence, persons with serious and terminal illnesses, persons whose health conditions are especially stigmatizing, different age groups, and persons who derive from diverse socioeconomic and cultural contexts. Some greater focus on ethical considerations in treating adult men and women was also requested. To our knowledge, this is the first time that a systematic assessment of ethics educational needs perceived by trainee stakeholders related to special populations has been documented empirically, although it is a concept frequently advanced by advocates and policy statements in the published literature.62–65
Greater Perceived Need Among Women Respondents—Fully Supported Hypothesis
We predicted that women would more strongly endorse ethics curricular needs, and this was a consistent pattern across all three topic domains and all three training levels we examined. The statistically significant differences across multiple measures indicate strong support for this hypothesis. Women placed greater emphasis on certain topics such as nondiscrimination, obtaining “informed refusal,” deciding when to withhold information from patients, and caring for persons with potentially stigmatizing illnesses. In understanding this pattern, it is important to note that when ethics teaching was first consistently introduced into medical school curricula in the late 1980s, women represented only one-third of applicants and graduates of medical training. As of 2003, women represent 49% of all applicants to medical school, 45% of medical school graduates, and as many as 74% of residents in some postgraduate specialty training programs.66 Women are therefore an increasingly important stakeholder group in academic medical settings, and in our study—as with others—they expressed vigorous need for ethics preparation.67,68 In light of theoretical and empirical work that has shown women as placing a greater emphasis on relationships, values, compassion, and an overall “ethics of care” in clinical ethics decision making relative to men, who often express narrower rationales or more rule-based approaches, it is likely that the predominant paradigms for decision making may evolve.45,69
Greater Perceived Need Among Psychiatry Resident Respondents—Partially Supported Hypothesis
On the basis of the patient populations they serve and consistent with our own and others’ earlier work, we anticipated that psychiatry residents would more strongly endorse curricular needs related to all topic areas.33,40,41,70 We did, in fact, find this general pattern, but the differences did not reach significance except in relation to the special populations ethics issues. Thus, only partial support for the hypothesis was obtained. Possible explanations for the lack of full support for this hypothesis include the relatively small number of psychiatry residents in the study sample, the overall level of enthusiasm expressed by residents across all programs, and the observation that the psychiatry residency program provided significant ethics teaching for its trainees at the time of the survey. Future work will continue to help clarify whether there are differential ethics preparation needs of residents in diverse fields of medicine.
Greater Perceived Need Among More Advanced Trainees—Unsupported Hypothesis
We predicted that an increasing need for curricular attention would be perceived by individuals at later stages of training. We based this prediction on evidence that residents have considerable unmet need for ethics training as assessed in other studies (and that residents deal daily with very complex clinical and ethical issues).13,71 This hypothesis was also predicated on the view that residency ethics education is often the least well developed from a curricular perspective.32,72 This pattern did not emerge in our indings, and so we conclude that the hypothesis was not supported, although trainees at all levels did identify curricular needs in all domains. For the first domain related to bioethics principles, however, a marginal (p<0.08) training level effect was found in which preclinical students identified the greatest needs and clinical students the least, with residents in between. For informed consent, residents expressed least need and preclinical students the greatest, with clinical students in between (p<0.03). For special populations ethics issues, preclinical students had the greatest perceived need for increased curricular attention and clinical and resident needs were assessed as the same (p<0.06). In other words, depending on the topic, perceived needs at different levels of training differed.
Our findings cannot be attributed simply to acquired mastery among advanced trainees or to specific curricular innovation within each domain, nor can they be tied to special developmental emphases at different stages. Because this study may be distinguished from most other published projects because of its cross-sectional design and inclusion of both medical students and residents, the intriguing pattern of differences may be more evident in this work. Further study is needed to clarify whether the responses in this study are generalizable.
Strengths and Limitations
The strengths of this study are its focus on three stages of training in a single analysis, permitting hypothesis-testing that lays groundwork for curricular planning and future empirical studies. It also places unique emphasis on contemporary ethical topics in medical education. The response rate of 62% is relatively strong. Nevertheless, its limitations relate to the self-report methodology and the fact that it took place at a single institution, raising potential questions about the applicability and generalizability of our findings to other settings. The distinct multicultural context of New Mexico may have contributed to the interest in greater curricular attention to special population issues, for example. For these reasons, we offer this work as the basis for future study.
CONCLUSION
This hypothesis-driven study provides evidence for the inclusion of bioethics concepts with increased societal emphasis, of multiple clinically and ethically important considerations in obtaining informed consent, and unique issues that arise in the care of persons who derive from special populations or have sources of vulnerability in clinical care contexts. It offers guidance for the inclusion of novel and important ethics domains in training curricula across medical school and diverse residency programs. For example, faculty responsible for ethics education may wish to review their curricula systematically to assure that certain topics have been included in their formal teaching program. In addition, faculty may wish to make sure that topics receive particular emphasis in some specialty areas or attend to the special interests of women trainees. To be valuable and effective, new ethics curricular approaches must be responsive to the current complex ethical environment and attentive to the preferences of medical students and residents of both genders, at different stages of training, with different patient care responsibilities. As we move into the 21st century, we will experience ethical complexity far greater and of a different quality than what we have witnessed in the past three decades of medical ethics education. It will therefore be crucial for medical educators to understand what ethical and professional domains are seen as salient to the ability to practice compassionate and competent medicine in this rapidly changing practice context from the perspective of our most critical “stakeholder” group—tomorrow’s physicians.73
Footnotes
The authors wish to thank Josh Reiher for his assistance in the preparation of this manuscript.
Supported by a grant from the Edwards Family Endowment for Communication Skills and an NIMH Career Development award (1KO2MH01918). The National Institute on Drug Abuse provided support for a related research project (1R01DA13139-01).
References
- 1.Miles SH, Lane LW, Bickel J, Walker RM, Cassel CK. Medical ethics education: coming of age. Acad Med. 1989;64:705–714. doi: 10.1097/00001888-198912000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bennahum D, editor. Cleveland, Ohio: Pilgrim Press; 1999. Managed Care: Financial, Legal, and Ethical Issues. [Google Scholar]
- 3.Center for Mental Health Services. Four Underserved/Underrepresented Racial/Ethnic Groups. Rockville, Md: CMHS; 2001. Cultural Competence Standards in Managed Care Mental Health Services. [Google Scholar]
- 4.The changing medical profession: implications for medical education. World Summit on Medical Education, Edinburgh, 8–12 Aug 1993 Med Educ; 1993. pp. 524–533. [PubMed] [Google Scholar]
- 5.Bickel J. Medical students’ professional ethics: defining the problems and developing resources. Acad Med. 1991;66:726–729. doi: 10.1097/00001888-199112000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Markakis KM, Beckman HB, Suchman AL, Frankel RM. The path to professionalism: cultivating humanistic values and attitudes in residency training. Acad Med. 2000;75:141–150. doi: 10.1097/00001888-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Cohen JJ. Nov 4, 2001. Our Compact with Tomorrow’s Doctors. Association of American Medical Colleges. press release retrieved Nov 13, 2001 ( http://www.aamc.org/newsroom/pressrel/011104a.htm) [DOI] [PubMed] [Google Scholar]
- 8.Wallace AG. Educating tomorrow’s doctors: the thing that really matters is that we care. Acad Med. 1997;72:253–258. doi: 10.1097/00001888-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Kasman DL, Fryer-Edwards K, Braddock CH., III Educating for professionalism: trainees’ emotional experiences on IM and pediatrics inpatient wards. Acad Med. 2003;78:730–741. doi: 10.1097/00001888-200307000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136:243–246. doi: 10.7326/0003-4819-136-3-200202050-00012. [DOI] [PubMed] [Google Scholar]
- 11.McCurdy L, Goode LD, Inui TS, Daugherty RM, Jr, Wilson DE, Wallace AG, Weinstein BM, Copeland EM., III Fulfilling the social contract between medical schools and the public. Acad Med. 1997;72:1063–1070. doi: 10.1097/00001888-199712000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Leach DC. Evaluation of competency: an ACGME perspective. accreditation council for graduate medical education. Am J Phys Med Rehabil. 2000;79:487–489. doi: 10.1097/00002060-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Graduate Medical Education. Chicago: ACGME; 2000. ACGME Outcome Project: General Competencies. [Google Scholar]
- 14.Basic curricular goals in medical ethics [letter] N Engl J Med. 1985;313:456–457. doi: 10.1056/NEJM198508153130720. [DOI] [PubMed] [Google Scholar]
- 15.Perkins HS. Teaching medical ethics during residency. Acad Med. 1989;64:262–266. doi: 10.1097/00001888-198905000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Sulmasy DP, Terry PB, Faden RR, Levine DM. Long-term effects of ethics education on the quality of care for patients who have do-not-resuscitate orders [see comments] J Gen Intern Med. 1994;9:622–626. doi: 10.1007/BF02600306. [DOI] [PubMed] [Google Scholar]
- 17.Roberts LW, Geppert C, McCarty T, Obenshain SS. Evaluating medical students’ skills in obtaining informed consent for HIV testing. J Gen Intern Med. 2003;18:112–119. doi: 10.1046/j.1525-1497.2003.10835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen DL, McCullough LB, Kessel RW, Apostolides AY, Heiderich KJ, Alden ER. A national survey concerning the ethical aspects of informed consent and role of medical students. J Med Educ. 1988;63:821–829. doi: 10.1097/00001888-198811000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Post SG, Botkin JR, Headrick LA. Medical students in a time of HIV: education and the duty to treat. Med Educ. 1995;29:128–132. doi: 10.1111/j.1365-2923.1995.tb02815.x. [DOI] [PubMed] [Google Scholar]
- 20.Fins JJ, Gentilesco BJ, Carver A, Lister P, Acres CA, Payne R, Storey-Johnson C. Reflective practice and palliative care education: a clerkship responds to the informal and hidden curricula. Acad Med. 2003;78:307–312. doi: 10.1097/00001888-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 21.McGrory BJ, McDowell DM, Muskin PR. Medical students’ attitudes toward AIDS, homosexual, and intravenous drug-abusing patients: a re-evaluation in New York City. Psychosomatics. 1990;31:426–433. doi: 10.1016/S0033-3182(90)72139-1. [DOI] [PubMed] [Google Scholar]
- 22.Christakis DA, Feudtner C. Temporary matters. The ethical consequences of transient social relationships in medical training [see comments] JAMA. 1997;278:739–743. doi: 10.1001/jama.278.9.739. [DOI] [PubMed] [Google Scholar]
- 23.Charon R, Fox RC. Critiques and remedies: medical students call for change in ethics teaching. JAMA. 1995;274:767. doi: 10.1001/jama.274.9.767. 771. [DOI] [PubMed] [Google Scholar]
- 24.Lundberg GD. Promoting professionalism through self-appraisal in this critical decade. JAMA. 1991;265:2859. [PubMed] [Google Scholar]
- 25.Lane LW. Residency ethics training in the United States: special considerations and early experience; Symposium ’90 Proceedings: medical ethics for postgraduate medical students; Westminster Institute for Ethics and Human Values. [Google Scholar]
- 26.Lane LW, Schiedermayer D, Spiro JH, Lane G, Siegler M. Caring for medical students as patients. Arch Intern Med. 1990;150:2249–2253. [PubMed] [Google Scholar]
- 27.Roberts LW, Warner TD, Lyketsos C, Frank E, Ganzini L, Carter D Collaborative Research Group on Medical Student Health. Perceptions of academic vulnerability associated with personal illness: a study of 1,027 students at nine medical schools. Compr Psychiatry. 2001;42:1–15. doi: 10.1053/comp.2001.19747. [DOI] [PubMed] [Google Scholar]
- 28.Christakis DA, Feudtner C. Ethics in a short white coat: the ethical dilemmas that medical students confront. Acad Med. 1993;68:249–254. doi: 10.1097/00001888-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Feudtner C, Christakis DA, Christakis NA. Do clinical clerks suffer ethical erosion? students’ perceptions of their ethical environment and personal development. Acad Med. 1994;69:670–679. doi: 10.1097/00001888-199408000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Hundert EM, Hafferty F, Christakis D. Characteristics of the informal curriculum and trainees’ ethical choices. Acad Med. 1996;71:624–642. doi: 10.1097/00001888-199606000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Howe KR. Medical students’ evaluations of different levels of medical ethics teaching: implications for curricula. Med Educ. 1987;21:340–349. doi: 10.1111/j.1365-2923.1987.tb00373.x. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell JJ. Residents’ desire for more clinical ethics education. Acad Med. 1993:68. [PubMed] [Google Scholar]
- 33.Roberts L, Teresita M, Lyketsos C, Hardee JT, Jacobson J, Walker R. What and how psychiatry residents at ten training programs wish to learn ethics. Acad Psychiatry. 1996;20:131–143. doi: 10.1007/BF03341563. [DOI] [PubMed] [Google Scholar]
- 34.Self DJ, Schrader DE, Baldwin DC, Jr, Wolinsky FD. The moral development of medical students: a pilot study of the possible influence of medical education. Med Educ. 1993;27:26–34. doi: 10.1111/j.1365-2923.1993.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 35.Self DJ, Baldwin DC, Jr, Wolinsky FD. Further exploration of the relationship between medical education and moral development. Camb Q Health Ethics. 1996;5:444–449. doi: 10.1017/s0963180100007271. [DOI] [PubMed] [Google Scholar]
- 36.Patenaude J, Niyonsenga T, Fafard D. Changes in the components of moral reasoning during students’ medical education: a pilot study. Med Educ. 2003;37:822–829. doi: 10.1046/j.1365-2923.2003.01593.x. [DOI] [PubMed] [Google Scholar]
- 37.Hayes RP, Stoudemire AS, Kinlaw K, Dell ML, Loomis A. Changing attitudes about end-of-life decision making of medical students during third-year clinical clerkships. Psychosomatics. 1999;40:205–211. doi: 10.1016/s0033-3182(99)71236-3. [DOI] [PubMed] [Google Scholar]
- 38.Wartman SA, Brock DW. The development of a medical ethics curriculum in a general internal medicine residency program. Acad Med. 1989;64:751–754. doi: 10.1097/00001888-198912000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Stevens NG, McCormick TR. Bringing the special perspective of the family physician to the teaching of clinical ethics. J Am Board Fam Pract. 1994;7:38–43. [PubMed] [Google Scholar]
- 40.Coverdale JH, Bayer T, Isbell P, Moffic S. Are we teaching psychiatrists to be ethical? Acad Psychiatry. 1992;16:199–205. doi: 10.1007/BF03341393. [DOI] [PubMed] [Google Scholar]
- 41.Jacobson JA, Tolle SW, Stocking C, Siegler M. Internal medicine residents’ preferences regarding medical ethics education. Acad Med. 1989;64:760–764. doi: 10.1097/00001888-198912000-00015. [DOI] [PubMed] [Google Scholar]
- 42.Angelos P, DaRosa DA, Derossis AM, Kim B. Medical ethics curriculum for surgical residents: results of a pilot project. Surgery. 1999;126:701–705. discussion 705–707. [PubMed] [Google Scholar]
- 43.White BD, Hickson GB, Theriot R, Zaner RM. A medical ethics issues survey of residents in five pediatric training programs. Am J Dis Child. 1991;145:161–164. doi: 10.1001/archpedi.1991.02160020051015. [DOI] [PubMed] [Google Scholar]
- 44.Gilligan C. Cambridge, Mass: Harvard University Press; 1993. In a Different Voice. [Google Scholar]
- 45.Carse AL. The “voice of care”: implications for bioethical education. J Med Philos. 1991;16:5–28. doi: 10.1093/jmp/16.1.5. [DOI] [PubMed] [Google Scholar]
- 46.Levitt C, Freedman B, Kaczorowski J, Adler P, Wilson R. Developing an ethics curriculum for a family practice residency. Acad Med. 1994;69:907–914. doi: 10.1097/00001888-199411000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Price J, Price D, Williams G, Hoffenberg R. Changes in medical student attitudes as they progress through a medical course. J Med Ethics. 1998;24:110–117. doi: 10.1136/jme.24.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elzubeir MA, Rizk DE. Exploring perceptions and attitudes of senior medical students and interns to academic integrity. Med Educ. 2003;37:589–596. doi: 10.1046/j.1365-2923.2003.01552.x. [DOI] [PubMed] [Google Scholar]
- 49.Shapiro J, Miller R. How medical students think about ethical issues. Acad Med. 1994;69:591–593. doi: 10.1097/00001888-199407000-00018. [DOI] [PubMed] [Google Scholar]
- 50.Stobo J, Blank L. ABIM’s project professionalism: staying ahead of the wave. Am J Med. 1995;97:1–3. [Google Scholar]
- 51.Leach DC. The ACGME competencies: substance or form? accreditation council for graduate medical education. J Am Coll Surg. 2001;192:396–398. doi: 10.1016/s1072-7515(01)00771-2. [DOI] [PubMed] [Google Scholar]
- 52.Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69:861–871. doi: 10.1097/00001888-199411000-00001. [DOI] [PubMed] [Google Scholar]
- 53.DuBois JM, Burkemper J. Ethics education in U.S. medical schools: a study of syllabi. Acad Med. 2002;77:432–437. doi: 10.1097/00001888-200205000-00019. [DOI] [PubMed] [Google Scholar]
- 54.Lynch DC, Pugno P, Beebe DK, Cullison SW, Lin JJ. Family practice graduate preparedness in the six ACGME competency areas: prequel. Fam Med. 2003;35:324–329. [PubMed] [Google Scholar]
- 55.Ginsburg S, Regehr G, Lingard L. The disavowed curriculum: understanding student’s reasoning in professionally challenging situations. J Gen Intern Med. 2003;18:1015–1022. doi: 10.1111/j.1525-1497.2003.21247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roberts LW. Subcommittee on Professional Attitudes and Values, Student Progress Assessment: Sequential assessment of medical student competence with respect to professional attitudes, values, and ethics. Acad Med. 1997;72:428–429. [PubMed] [Google Scholar]
- 57.Roberts LW, McCarty T, Obenshain S. Comprehensive performance examination gives insights into the “hidden curriculum. Acad Med. 1999;74:597–598. doi: 10.1097/00001888-199905000-00071. [DOI] [PubMed] [Google Scholar]
- 58.Roberts LW, Green-Hammond K, Geppert C, Warner TD. The positive role of professionalism and ethics training in medical education: a comparison of medical student and resident perspectives. Acad Psychiatry. 2004;28:170–182. doi: 10.1176/appi.ap.28.3.170. [DOI] [PubMed] [Google Scholar]
- 59.Olukoya AA. Attitudes of medical students to medical ethics in their curriculum. Med Educ. 1983;17:83–86. doi: 10.1111/j.1365-2923.1983.tb01104.x. [DOI] [PubMed] [Google Scholar]
- 60.Kao A, Lim M, Spevick J, Barzansky B. Teaching and evaluating students’ professionalism in US medical schools, 2002–2003. JAMA. 2003;290:1151–1152. doi: 10.1001/jama.290.9.1151. [DOI] [PubMed] [Google Scholar]
- 61.Agency for HealthCare Research and Quality. Natonal Healthcare Disparities. Rockville, Md: Department of Health and Human Services; 2003. [Google Scholar]
- 62.Department of Health and Human Services. Rockville, Md: Department of Health and Human Services; 1999. Mental Health: A Report of the Surgeon General. [Google Scholar]
- 63.Ramirez AG. Consumer-provider communication research with special populations. Patient Educ Couns. 2003;50:51–54. doi: 10.1016/s0738-3991(03)00080-6. [DOI] [PubMed] [Google Scholar]
- 64.Boyd KM. Implications of HIV infection and aids for medical education. Med Educ. 1994;28:488–491. doi: 10.1111/j.1365-2923.1994.tb02724.x. [DOI] [PubMed] [Google Scholar]
- 65.Fins JJ, Nilson EG. An approach to educating residents about palliative care and clinical ethics. Acad Med. 2000;75:662–665. doi: 10.1097/00001888-200006000-00021. [DOI] [PubMed] [Google Scholar]
- 66.Clark V, Yamagata H, Chapman W. Washington, DC: Association of American Medical Colleges; 2003. Women in U.S. Academic Medicine Statistics: 2002–2003. [Google Scholar]
- 67.Crosdale M. Washington, DC: AMA; 2004. More women than men seek entry to US medical schools, in American Medical News. [Google Scholar]
- 68.Shrier DK. A celebration of women in US medicine. Lancet. 2004;363:253. [Google Scholar]
- 69.Sharpe VA. Justice and care: the implications of the Kohlberg-Gilligan debate for medical ethics. Theor Med. 1992;13:295–318. doi: 10.1007/BF02126697. [DOI] [PubMed] [Google Scholar]
- 70.Morenz B, Sales B. Complexity of ethical decision making in psychiatry. Ethics Behav. 1997;7:1–14. doi: 10.1207/s15327019eb0701_1. [DOI] [PubMed] [Google Scholar]
- 71.Baldwin DC, Jr, Daugherty SR, Rowley BD. Unethical and unprofessional conduct observed by residents during their first year of training. Acad Med. 1998;73:1195–1200. doi: 10.1097/00001888-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 72.Barnard D. Residency ethics teaching: a critique of current trends. Arch Intern Med. 1988;148:1836–1838. [PubMed] [Google Scholar]
- 73.Douglas-Steele D, Hundert EM. Accounting for context: future directions in bioethics theory and research. Theor Med. 1996;17:101–119. doi: 10.1007/BF00539734. [DOI] [PubMed] [Google Scholar]


