Abstract
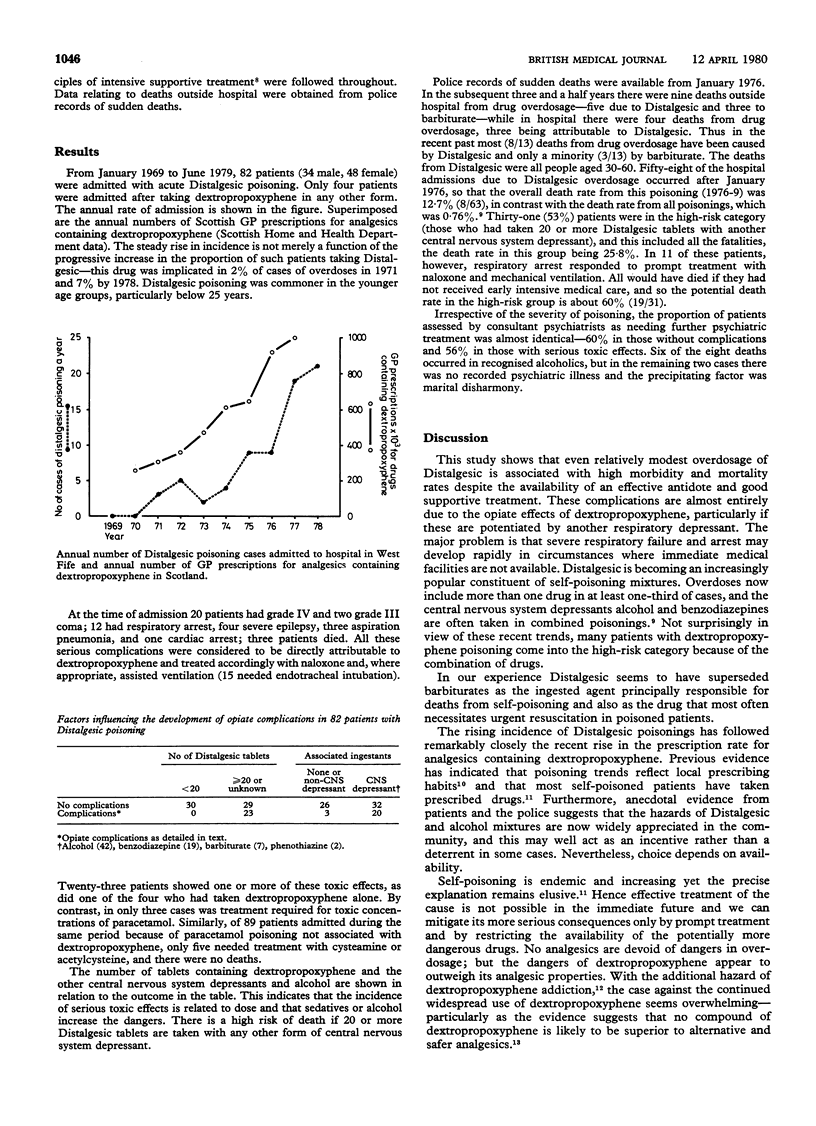
A review of all dextropropoxyphene poisoning episodes in a stable representative population during the past 10 years showed that Distalgesic accounts for most overdoses, and it has become an increasingly popular component of self-poisoning coktails. Sudden respiratory depression due to dextopropoxyphene potentiated by other common ingested agents is the main danger, and at least one-third of patients take a potentially lethal dose (20 tablets of Distalgesic and alcohol or benzodiazepine). Naloxone is an effective antagonist but, because of the rapidity of deterioration, 40% of patients sustain irreversible cerebral damage before reaching resuscitation facilities. Consequently Distalgesic has become the ingested agent principally responsible for self-poisoning deaths over the age of 12 years. This rise to prominence has paralleled a pronounced increase in prescriptions for the drug. The reason for the increased rise in selfpoisoning remains elusive. As effective treatment of the cause is not possible the only way to mitigate its serious consequences is prompt treatment and restrictions on the availability of the drug. No analgesics are devoid of danger in overdose, but in dextropropoxyphene the evidence suggests that its dangers outweigh its analgesic properties.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carson D. J. Fatal dextropropoxyphene poisoning in Northern Ireland. Review of 30 cases. Lancet. 1977 Apr 23;1(8017):894–897. doi: 10.1016/s0140-6736(77)91212-0. [DOI] [PubMed] [Google Scholar]
- Elmes P. C. The contribution of prescribed drugs to the incidence of accidental and deliberate poisoning in the community. Acta Pharmacol Toxicol (Copenh) 1977;41 (Suppl 2):517–521. [PubMed] [Google Scholar]
- Holding T. A., Buglass D., Duffy J. C., Kreitman N. Parasuicide in Edinburgh--a seven-year review 1968-74. Br J Psychiatry. 1977 Jun;130:534–543. doi: 10.1192/bjp.130.6.534. [DOI] [PubMed] [Google Scholar]
- Lawson A. A., McCallum C. J. Trends in acute poisoning in a District Medical Unit. Health Bull (Edinb) 1979 May;37(4):121–127. [PubMed] [Google Scholar]
- Miller R. R., Feingold A., Paxinos J. Propoxyphene hydrochloride. A critical review. JAMA. 1970 Aug 10;213(6):996–1006. [PubMed] [Google Scholar]
- Prescott L. F., Illingworth R. N., Critchley J. A., Stewart M. J., Adam R. D., Proudfoot A. T. Intravenous N-acetylcystine: the treatment of choice for paracetamol poisoning. Br Med J. 1979 Nov 3;2(6198):1097–1100. doi: 10.1136/bmj.2.6198.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarala R., Forrest J. A. Treatment of dextropropoxyphene poisoning. Br Med J. 1973 Jun 2;2(5865):550–550. doi: 10.1136/bmj.2.5865.550-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittington R. M. Dextropropoxyphene (Distalgesic) overdosage in the West Midlands. Br Med J. 1977 Jul 16;2(6080):172–173. doi: 10.1136/bmj.2.6080.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittington R. M. Dextropropoxyphene addiction. Lancet. 1979 Oct 6;2(8145):743–744. doi: 10.1016/s0140-6736(79)90670-6. [DOI] [PubMed] [Google Scholar]


