Abstract
Objective:
Many patients with an inguinal hernia are asymptomatic or have little in the way of symptoms from their hernia. Repair is often associated with long-term chronic pain and has a recurrence rate of 5% to 10%. Our aim was to compare operation with a wait-and-see policy in patients with an asymptomatic hernia.
Methods:
A total of 160 male patients 55 years or older were randomly assigned to observation or operation. Patients were assessed clinically and sent questionnaires at 6 months and 1 year. The primary endpoint was pain and general health status at 12 months; other outcome measures included costs to the health service and the rate of operation for a new symptom or complication.
Results:
At 12 months, there were no significant differences between the randomized groups of observation or operation, in visual analogue pain scores at rest, 3.7 mm versus 5.2 mm (mean difference, −1.6; 95% confidence interval (CI), −4.8 to 1.6, P = 0.34), or on moving, 7.6 mm versus 5.7 mm (mean difference, −1.9; 95% CI, −6.1 to 2.4, P = 0.39). Also, the number of patients 29 versus 24 (difference in proportion, 8%; 95% CI, −7% to 23%, P = 0.31), who recorded pain on moving and the number taking regular analgesia, 9 versus 17 (difference in proportion, −10%; 95% CI, −21% to 2%, P = 0.14) was similar. At 6 months, there were significant improvements in most of the dimensions of the SF-36 for the operation group, while at 12 months although the trend remained the same the differences were only significant for change in health (mean difference, 7.3; 95% CI, 0.4 to 14.3, P = 0.039). The rate of crossover from observation to operation 23 patients at a median follow-up of 574 days was higher than predicted. The observation group also suffered 3 serious hernia-related adverse events compared with none in the operation group.
Conclusions:
Repair of an asymptomatic inguinal hernia does not affect the rate of long-term chronic pain and may be beneficial to patients in improving overall health and reducing potentially serious morbidity.
Concern exists that repair of an asymptomatic inguinal hernia may lead to chronic groin pain. Results from this study indicate that there is no difference in chronic pain following operation or observation at the 1-year follow-up. Instead, operation may be of benefit to patients in improving general health and reducing serious morbidity.
Repair of an inguinal hernia is one of the most common operations performed in general surgery with significant costs to health care and society. Rates of repair are increasing annually and have the potential to double over the coming years.1 The most common symptom patients have from their hernia is pain that is usually mild to moderate and generally does not affect work or leisure activities. Up to one third of patients are asymptomatic or have very little in the way of symptoms from their hernia.2 For those that undergo repair, around 10% will have a significant wound infection or hematoma, 3% will have severe chronic pain, and 5% to 10% will develop a recurrent hernia.3
One of the most common reasons for recommending inguinal hernia repair to patients is the risk of strangulation. Strangulation is associated with an increased morbidity and mortality; however, it is uncommon with only around 1 in 400 of all patients presenting with an inguinal hernia requiring bowel resection for this complication.2 Using life-table analyses based on 2 population groups, Fitzgibbons et al estimated that the lifetime risk of strangulation for an 18-year-old with an inguinal hernia is 0.272% (or 1 in 368) while that for a 72-year-old is 0.034% (or 1 in 2941).4
It is not known what the risk of pain or strangulation from an asymptomatic inguinal hernia is or if these patients are likely to develop warning symptoms before the latter event occurs. If this were the case, then there may be a window of opportunity to operate before a serious complication arises. This study examines patient outcome comparing operation with a wait-and-see policy in patients with an asymptomatic inguinal hernia.
PATIENTS AND METHODS
Informed consent was obtained from male patients 55 years or older with an asymptomatic inguinal hernia to randomization to hernia repair or observation. The trial had ethical approval and patients who were unfit for local anesthetic repair or had an irreducible hernia were excluded. Patients were asked to complete a visual analogue pain scale and those that had an inguinal hernia that was reducible on lying down or with minimal applied pressure and registered no pain at rest or movement from their hernia were considered for inclusion into the trial. All hernias were categorized into direct and indirect, and the size of the hernia was measured by the degree of protrusion and the diameter of the defect. The duration the hernia was present was also recorded, as were details on whether it was primary or recurrent. All participants were asked to complete a questionnaire on general health status (SF-36). The SF-36 covers 8 health concepts: physical functioning, bodily pain, role limitations owing to physical or emotional problems, general mental health, social functioning, energy/fatigue, and general health perceptions. It also includes a single item that provides an indication of perceived change in health. The score for each scale is calculated as the sum of the scores for each item (ranging from 0 to 4 on a 5-point Likert scale) and transformed linearly into a range from 0 to 100; a higher score denotes a better level of functioning. We used disability as assessed with the Barthel Index to measure any adverse effects the patients hernia may have on activities of daily living.5
Patients randomized to operation had a tension free mesh repair under local or general anesthetic. Patients in the observation arm were given a contact number to telephone should their hernia become symptomatic or complicated. These patients were advised operation only if the hernia became acutely irreducible, developed pain, or increased in size such that interfered with work or leisure activities. Participants in both groups were examined at 6 months, 12 months, and annually thereafter at a single Research Clinic at the Western Infirmary, Glasgow. Visual analogue pain scores and general health questionnaires were also completed at those times.
The impact of a shift in policy of not operating on an asymptomatic inguinal hernia was also assessed from an economic perspective. This included hospital and patient costs as well as the cost of any significant complication. Costing was also assessed from a societal perspective in terms of differences in cost and quality of life scores. SF-36 data were converted to utility values using an algorithm supplied by the Health Economics Department School of Health and Related Research, University of Sheffield.6
Statistical Considerations
The study was powered to address the primary endpoint of pain at 1 year. At the time of the original power calculation, previous studies have shown that a reasonable assumption was for at least one third of patients to report pain at the hernia repair site 1 year following open mesh repair.7 We also calculated that if 15% of asymptomatic patients were to develop pain or a complication that required operation each year, then most of the population would end up having their hernia operation delayed rather than not operated on. Therefore, with 125 subjects in each of the randomized groups, the study would have an over 80% power at the 5% level of significance to detect an absolute difference in pain at 1 year of 16% between groups (from 31% to 15%). After 1 year of the study, we had not recruited as quickly as we anticipated in the first year, but a revised power calculation indicated that 80 subjects per group would give the study over 80% power to detect a slightly larger difference of 20% (from 35% to 15%), and that we could achieve this number in the scheduled recruitment window given the recruitment rate experienced in the first year. We therefore modified the design of the study to recruit 160 patients in total.
The primary analysis was according to the intention-to-treat principle. Baseline data were tabulated by randomized treatment groups (observation or operation). Categorical data at 6 and 12 months (such as taking regular analgesia, yes/no; pain at rest/at movement, yes/no) were compared between the 2 randomized groups by χ2 tests. Continuous data (such as the SF-36 Health dimensions, and the VAS pain at rest and at movement scores) at 6 and 12 months were given as mean (standard deviation) and compared using linear models that adjusted for the baseline measure of the outcome under consideration. Additional linear models, which further adjusted for other baseline covariates, were fitted (age, hernia type, duration, side of hernia, and degree of protrusion). For the pain outcomes, a linear model adjusted for both the baseline and the 6- or 12-month variable measuring whether the participant was taking regular analgesia. In those randomized to observation, a Kaplan-Meier time to crossover from observation to surgery curve was plotted, and univariate and multivariate Cox proportional hazards models fitted to investigate the influence of the baseline covariates on the propensity to transition to surgery.
For the SF-36 Change in Health component outcome, and for the pain scores at rest and on moving, secondary supporting analyses to the intention-to-treat analysis was performed reclassifying the subjects according to what intervention they had actually received (observation or operation) at 6 and then at 12 months regardless of their randomized allocation. For those randomized to observation, we also compared the pain scores (at rest and on moving) for those who transitioned to surgery against those that remained on observation. We compared the most recent pain score before surgery with the 12-month pain scores in those that remained on observation, using a linear model that adjusted for baseline pain score and other baseline covariates, including age.
All analyses were carried out in SAS 9.1 for Windows. No adjustment has been made for multiple comparisons.
RESULTS
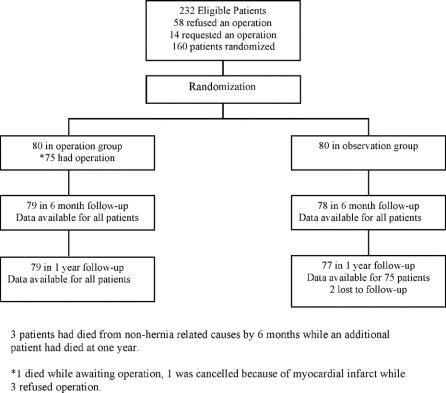
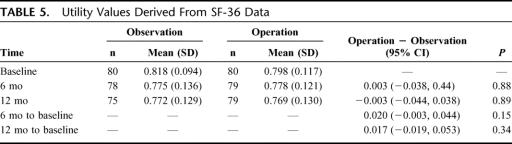
During the study period, there were 232 eligible patients with an asymptomatic hernia, 160 of whom agreed to randomization. The reasons for patients not participating in the trial were refusal to have an operation (58) or request for an operation (14) (Fig. 1). All patients in both groups completed baseline data and visual analogue pain scores at rest and on movement. While all had no pain from their hernia, some patients in both groups recorded a pain score at rest and on moving, which they related to osteoarthritis. Baseline characteristics of participants in both groups are detailed in Table 1. There is a tendency for the operation group to have slightly worse SF-36 scores at baseline consistently across all components, with slightly larger hernias, which have been endured for slightly longer. These differences are due to chance. Of the 80 participants randomized to operation, 75 underwent hernia repair. One patient died of cancer while awaiting repair, 1 had a serious cardiac event and repair was canceled, while 3 refused multiple admission dates for repair. The mean (standard deviation) time from randomization to surgery for the 75 of 80 participants in the operation group who proceeded to surgery was 103 (97) days (range, 8–486 days; median, 78 days; interquartile range, 36–134 days).
FIGURE 1. Trial profile.
TABLE 1. Baseline Characteristics
Pain at 6 and at 12 Months
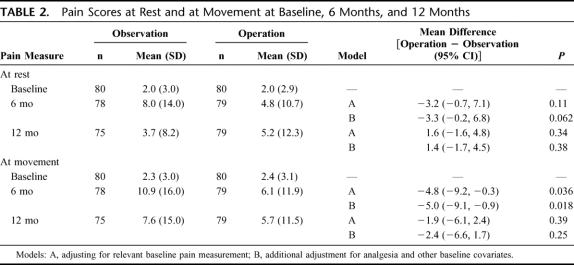
Visual analogue pain scores at rest and on movement were similar in both groups at 6 and 12 months following randomization (Table 2). At 6 months, 34 (44%) in the observation group recorded pain (at least 2 mm on the 10-cm Visual Analogue Scale) at the hernia site at rest compared with 29 (37%) in the operation group (difference in proportions, observation to surgery, 7%; 95% confidence interval [CI], −8% to 22%; P = 0.42). The respective numbers for pain on movement were 40 (51%) and 32 (41%) (difference, 11%; 95% CI, −5% to 26%; P = 0.20). At 1 year, the numbers had reduced to 21 (28%) in the observation group and 24 (30%) in the operation group at rest (difference, −2%; 95% CI, −17% to 12%; P = 0.86) while on movement the respective figures were 29 (39%) and 24 (30%) (difference, 8%; 95% CI, −7% to 23%; P = 0.31). Only 6 (8%) patients has a VAS >10 mm at rest in the observation group at 1 year compared with 9 (11%) in the operation group (difference, −3%; 95% CI, −13% to 6%; P = 0.59). The respective numbers for VAS >10 mm on moving were 15 (20%) and 11 (14%) (difference, 6%; 95% CI, −6% to 18%; P = 0.39). At baseline, 5 (6%) participants in each randomized group were taking regular analgesia, while at 6 months this was 14 (18%) in the observation group and 13 (16%) in the operation group (difference, 2%; 95% CI, −10% to 14%; P = 0.84); by 12 months the respective numbers were 9 (12%) and 17 (22%) in the operation group (difference, −10%; 95% CI, −21% to 2%; P = 0.14).
TABLE 2. Pain Scores at Rest and at Movement at Baseline, 6 Months, and 12 Months
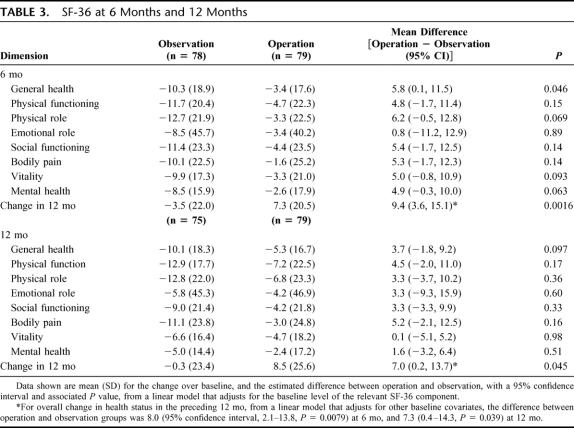
SF-36 at 6 and 12 Months
On an intention-to-treat analysis, there was a consistent trend to improvement of about 5 points in all of the dimensions (except emotional role) in the operation group compared with the observation group at 6 months (Table 3). The change in the previous 12 months was significantly increased in the operation group, with a mean difference of 8 (95% CI, 2 to 14; P = 0.0079). At 12 months, similar trends were observed but typically now about 3 units increase rather than 5. Change in health in the previous 12 months remained significantly increased with a mean difference of 7 (95% CI, 0 to 14; P = 0.039).
TABLE 3. SF-36 at 6 Months and 12 Months
Treatment Received Supporting Analyses
In practice, some participants randomized to observation had received surgery by 6 or 12 months post randomization, and some patients who were randomized to surgery became unable to have the surgery or had not yet had the surgery by either 6 or 12 months. In an analysis to complement the intention-to-treat analyses, we then compared the SF-36 Change in Health question according to whether the subjects had or had not received surgery at 12 months. This involved 8 participants randomized to surgery being reclassified to observation and 15 participants randomized to observation being reclassified to surgery. The difference between the operation and observation groups was then 9.9 (95% CI, 4.1 to 15.7; P = 0.0010), so confirming the intention-to-treat results.
The pain score analyses according to intervention received showed very similar results to the intention-to-treat analyses reported in Table 2 (data not shown). For those randomized to observation, we also compared the pain scores for the 15 who transitioned to surgery (using their most recent pain score before transition, that is, baseline if the transition occurred within the 1st 6 months, or the 6 month score if transition took place in the 2nd 6 months) against the 12-month pain score for the remaining 60 that remained on observation and had data at 12 months. For pain at rest, the mean scores were 13.5 and 3.7 (difference in means, 11.6; 95% CI, 5.3 to 17.8, adjusted for baseline pain and age; P = 0.0004), and for pain on moving, mean scores were 15.6 versus 7.1 (adjusted difference, 9.9; 95% CI, 1.4 to 18.4; P = 0.023).
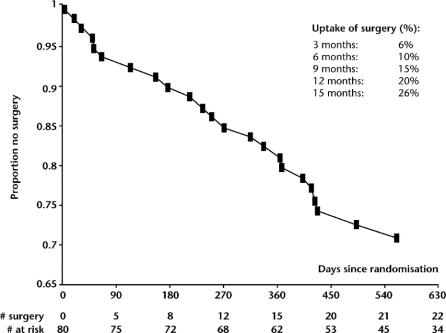
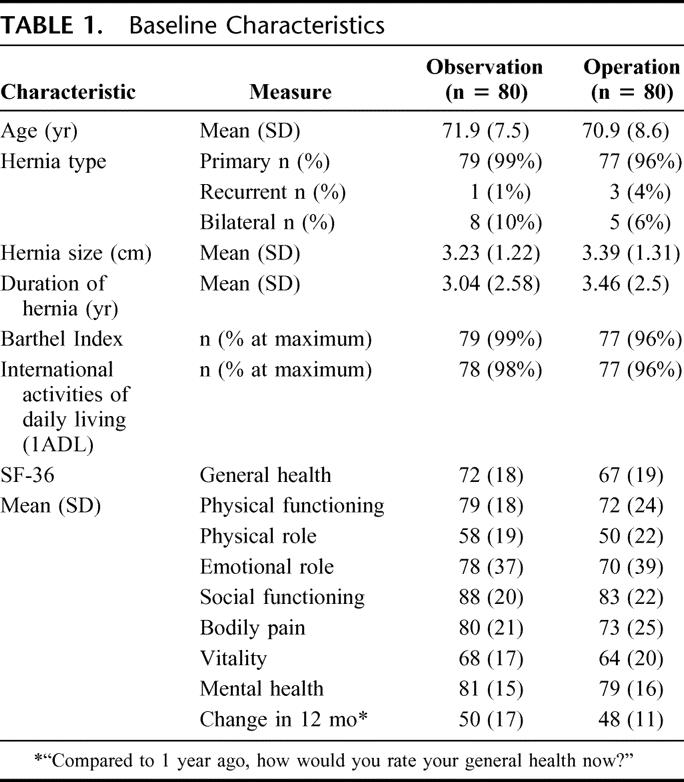
Crossovers From Observation to Surgery
At a median follow-up of 574 days 23 patients in the observation group have had an operation (Fig. 2). The reasons for operation were pain and an increase in hernia size: pain (11), increase in size (8), affecting work or leisure activities (3), and acute presentation (1). A Cox proportional hazards regression model (Table 4) to study the influence of baseline characteristics on crossover indicated that the degree of protrusion was the only factor that came close to predicting such an event. Hazard ratio on univariate analysis (95% CI) 1.29 (0.98 to 1.69) (P = 0.073), which in a multivariate model adjusting for all the other factors increased to 1.35 (1.00 to 1.83) (P = 0.053). All operations were performed by the same surgical unit that carried out surgery in the operation group. One patient had a postoperative myocardial infarct and died, whereas another had a cardiovascular accident in the observation group. No serious postoperative complications were noted in the operation group. A further 9 patients have died on follow-up: 4 in the observation group and 5 in the operation group. The causes of death has been cardiovascular disease (6) and cancer related (3).
FIGURE 2. Kaplan-Meier plot of time to decision for surgery in those participants randomized to the observation group.
TABLE 4. Univariate and Multivariate Cox Proportional Hazards Model for Baseline Predictors of Crossover From Observation to Surgery
Economics
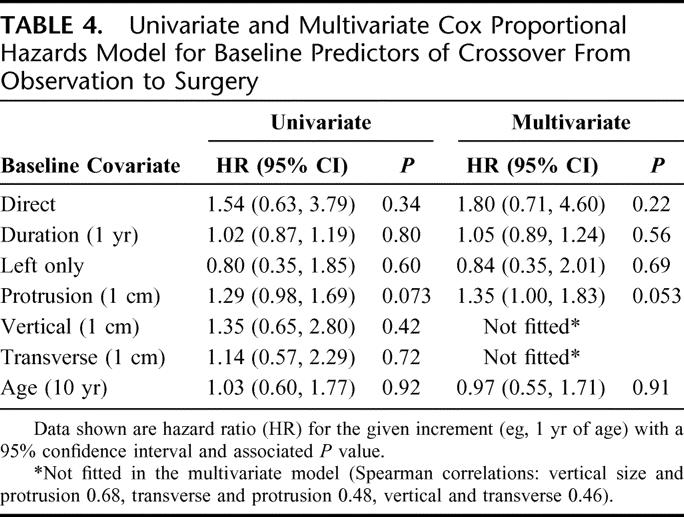
The cost to the Health Service was £401.9 per patient greater for the operation group at the median follow-up of 574 days. This took into account clinic and operative costs and the cost of complications for both groups.8–10 Despite improvements in general health, there was no significant quality-adjusted life year gain (QALY) for the operation group at 12 months (Table 5).
TABLE 5. Utility Values Derived From SF-36 Data
DISCUSSION
This study was set up against the background that operation on an asymptomatic hernia or a hernia that had little effect on the patient's social or daily activities may result in considerable chronic pain and discomfort. Interestingly, this was not the case, and on any parameter measured up to 1 year after randomization, pain scores, the number who reported pain, and analgesia consumption, there was no difference between those that were observed and those that had an operation. Moreover, patients that underwent operation perceived that their general health had improved, whereas those that were observed felt that their health had declined in keeping with increasing age in an elderly population.
There is one other clinical trial currently in progress that sets out to determine if watchful waiting is an acceptable alternative to routine hernia repair for patients with minimal or no hernia symptoms.4 As with our study, the primary outcome measures are pain or discomfort interfering with usual activities and the physical component summary score of the SF-36. The outcome variables are measured at 6 months, 12 months, and 2 years. The major difference between this and our trial is that the inclusion criteria are broader in that men of 18 years and older are considered eligible.
There were 3 serious adverse events in the observation group in this trial: 1 patient had an acute hernia, 1 had a postoperative stroke, and 1 had a myocardial infarction and died postoperatively. The patient with the acute hernia had it reduced at another hospital, whereas all had their operations on an urgent elective basis for pain. Serious morbidity and mortality are rare after elective hernia repair, even for elderly patients. The 30-day mortality for elective patients over 60 years of age was 0.48% from the Danish Hernia Database, whereas that for patients over 70 years was 0.32% for the corresponding Swedish Hernia Register.11,12 Interestingly the latter was lower than the standardized mortality rate for individuals of the same age in the Swedish population as a whole. In this context, it is clear from review of the patients' case records in this study that had a serious postoperative event, both had comorbid cardiovascular disease which had deteriorated significantly in the period under observation and had they had been operated on at presentation such an outcome may have been avoided.
Despite improvements in perioperative care, mortality from acute groin hernia surgery remains high. In the prospective nationwide study from Denmark, 7% of patients with an acute presentation died within 30 days of operation.11 This high mortality occurs mostly because of severe comorbid illness with only a small subset having strangulated bowel.13 While there are a number of reasons for this, a significant contribution is made by clinicians turning high-risk patients down for elective operation in the first instance.14 Given the safety and ease of local anesthetic groin hernia repair, this approach needs to change as most patients will be suitable for elective repair by this method irrespective of the nature or severity of any coexisting illness.
The rate of crossover to operation in this observation group was higher than expected in this study. This occurred at a steady rate over the period of observation and may indicate that such a tactic would merely delay rather than avoid operation. In our initial calculation based on expected survival for the age group, our estimate was that, if 15% of patients developed pain or a complication that required operation each year, then a nonoperative policy would not be viable. In the first year of follow-up, almost 20% have required an operation for such an event and a further 6% of the at risk population have been operated on 3 months into the second year of follow-up. Interestingly, the only factor to predict crossover from observation to operation was the degree of protrusion of the hernia. Factors such as the duration the hernia was present, whether the hernia was direct or indirect, the side of the hernia and age of the patient had no effect. However, these data need to be interpreted with caution as the study was not designed to look at predictors of crossover.
While the operation strategy might not appear cost-effective within the follow-up period of this study, the time trends in the results all suggest that, with longer follow-up, it would become increasingly cost-effective. These include a growing number of patients in the observation group requiring operation, thereby reducing the cost difference and the cost of managing serious complications rising over time. For example, the average health services cost per patient of a stroke as occurred in the observation group in this trial have been calculated to be £15,306 over 5 years.7 This rises to £29,405 if the costs of informal care are included and £57,235 if these costs are based on home help rates rather than at the minimum wage.
Hernia repair in the patient with an asymptomatic inguinal hernia does not increase long-term pain. In addition, it may reduce serious morbidity and improve general health. Further clinical trials with longer follow-up are required to determine if such a strategy produces sufficient health gain to justify the additional health care costs.
Footnotes
Reprints: Patrick J. O'Dwyer, FRCS, University Department of Surgery, Western Infirmary, Glasgow G11 6NT, UK. E-mail: p.j.odwyer@clinmed.gla.ac.uk.
REFERENCES
- 1.Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362:1561–1571. [DOI] [PubMed] [Google Scholar]
- 2.Hair A, Paterson C, Wright D, et al. What effect has the duration of an inguinal hernia on patient's symptoms? J Am Coll Surg. 2001;193:125–129. [DOI] [PubMed] [Google Scholar]
- 3.Hair A, Duffy K, McLean J, et al. Groin hernia repair in Scotland. Br J Surg. 2000;87:1722–1726. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgibbons RJ, Jonasson O, Gibbs J, et al. The development of a clinical trial to determine if watchful waiting is an acceptable alternative to routine herniorrhaphy for patients with minimal or no hernia symptoms. J Am Coll Surg. 2003;196:5. [DOI] [PubMed] [Google Scholar]
- 5.Colin C, Wade DT, Davies S, et al. The Barthel ADL Index: a reliability study. Int Disab Study. 1988;10:61–63. [DOI] [PubMed] [Google Scholar]
- 6.Brazier J, Roberts J, Deveril M. The estimation of a preference-based measure on health from the SF-36. J Health Econ. 2002;21:271–292. [DOI] [PubMed] [Google Scholar]
- 7.MRC Laparoscopic Groin Hernia Trial Group. Laparoscopic versus open repair of groin hernia: a randomised comparison. Lancet. 1999;354:185–190. [PubMed] [Google Scholar]
- 8.Medical Research Council Laparoscopic Groin Hernia Trial Group. Cost-utility analysis of open versus laparoscopic groin hernia repair: results from a multicentre randomized clinical trial. Br J Surg. 2001;88:653–661. [DOI] [PubMed] [Google Scholar]
- 9.Information and Statistics Division, NHS Scotland. Scottish Health Service Costs, year ended March 2004. NHS Scotland.
- 10.Youman P, Wilson K, Harraf F, et al. The economic burden of stroke in the United Kingdom. Pharmacoeconomics. 2003;21(suppl 1):43–50. [DOI] [PubMed] [Google Scholar]
- 11.Bay-Nielsen M, Kehlet H, Strand L, et al. Quality assessment of 26 304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet. 2001;358:1124–1128. [DOI] [PubMed] [Google Scholar]
- 12.Haapaniemi S, Sandblom G, Nilsson E. Mortality after elective and emergency surgery for inguinal and femoral hernia. Hernia. 1999;4:205–208. [Google Scholar]
- 13.McGugan E, Burton H, Nixon SJ, et al. Deaths following hernia repair: room for improvement. J R Coll Surg Edin. 2000;45:183–186. [PubMed] [Google Scholar]
- 14.McEntee GP, Carroll AO, Mooney B, et al. Timing of strangulation in adult hernias. Br J Surg. 1989;76:725–726. [DOI] [PubMed] [Google Scholar]