Abstract
Objective:
To estimate the prevalence of residual pain 2 to 3 years after hernia surgery, to identify factors associated with its occurrence, and to assess the consequences for the patient.
Summary Background Data:
Iatrogenic chronic pain is a neglected problem that may totally annul the benefits from hernia repair.
Methods:
From the population-based Swedish Hernia Register 3000 patients aged 15 to 85 years were sampled from the 9280 patients registered as having undergone a primary groin hernia operation in the year 2000. Of these, the 2853 patients still alive in 2003 were requested to fill in a postal questionnaire.
Results:
After 2 reminders, 2456 patients (86%), 2299 men and 157 women responded. In response to a question about “worst perceived pain last week,” 758 patients (31%) reported pain to some extent. In 144 cases (6%), the pain interfered with daily activities. Age below median, a high level of pain before the operation, and occurrence of any postoperative complication were found to significantly and independently predict long-term pain in multivariate logistic analysis when “worst pain last week” was used as outcome variable. The same variables, along with a repair technique using anterior approach, were found to predict long-term pain with “pain right now” as outcome variable.
Conclusion:
Pain that is at least partly disabling appears to occur more often than recurrences. The prevalence of long-term pain can be reduced by preventing postoperative complications. The impact of repair technique on the risk of long-term pain shown in our study should be further assessed in randomized controlled trials.
Thirty-one percent of 2853 patients, who answered a postal questionnaire 2 to 3 years after inguinal hernia surgery, still had pain in the operated groin. Six percent had pain of such severity that it interfered with daily activities. Young age, preoperative pain level above average, postoperative complications, and anterior approach independently predicted long-term pain.
Until recently, research on the results of hernia surgery has focused mainly on recurrences. However, with the introduction of mesh techniques and presumably an increased awareness of the importance of systematic quality control, the recurrence rate has decreased dramatically.1 Hence, now that recurrences are no longer a pressing clinical problem, there has been a recent upsurge in interest in chronic pain as an adverse outcome. But the level of quantification of pain has often been limited in studies addressing the risk of long-term pain, and pain has sometimes been treated merely as a dichotomous (yes/no) phenomenon.2 As a result, the clinical and public health significance of reported prevalence rates of residual pain (ranging between 0% and 37%) remains uncertain.3
With the main purpose of evaluating long-term pain as an alternative endpoint in research on the outcome of hernia surgery, we used a validated pain questionnaire to investigate pain behavior rather than imaginary descriptors of pain intensity in an essentially population-based series of patients operated on 59 hospitals.
MATERIALS AND METHODS
In the Swedish Hernia Register (SHR),4 detailed information on more than 100,000 groin hernia repairs has been compiled since 1992. Every inguinal or femoral hernia operation in patients of ages 15 years or older at participating departments are recorded according to a standardized protocol. Recorded variables include age, gender, mode of admission, time on waiting list, type of hernia as noted during operation, size of the defect, method of repair, postoperative complications and reoperation for recurrence.4 Methods of repair using anterior approach include Liechtenstein, Shouldice, Bassini, plug procedures, and other methods through groin incision. Methods of repair using posterior approach include laparoscopic, Stoppa, and Nyhus techniques. Information on clinical follow-up is not mandatory, but any complication observed by the operating unit up to 30 days after surgery has to be recorded in the database.5 Every Swedish resident has a unique National Registration Number that is universally used in official contexts, including entries in population and health registers, as well as in medical case records. The National Registration Number makes follow-up possible through cross-linkages within the SHR and also through record linkages to the Swedish Cause of Death Register (CDR) and the continuously updated and virtually complete national Inpatient Register.
Patients
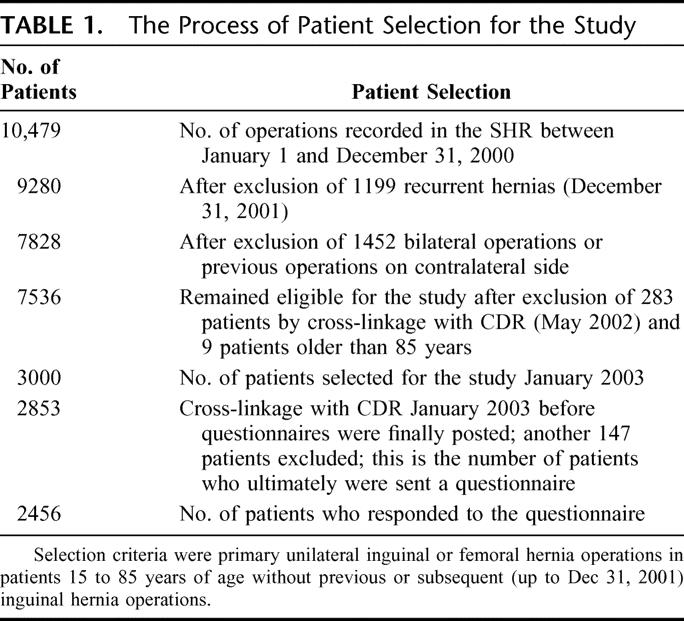
Between January 1 and December 31, 2000, 10,479 hernia operations at 59 hospitals, constituting 60% of all operating units in Sweden, were recorded in the SHR. Of these, 9280 were primary hernia repairs. After exclusion of patients with bilateral repairs, previous hernia operations on the contralateral side (served as reference for pain), subsequent hernia operations on either side, and patients below 15 years or above 85 years of age, 7828 patients were eligible for investigation. By cross-linkage with CDR (May 2002), 7536 patients were found to be still alive. From this cohort, we randomly selected 3000 patients who had undergone a unilateral repair of a primary inguinal or femoral hernia.
There were 2787 (92.9%) men and 213 (7.1%) women in the sample, with a mean age of 58.2 years. Before the questionnaires were mailed, a final record linkage with the CDR was performed in January 2003, and this revealed that 147 of these patients had died, leaving 2853 still alive and available for contact (Table 1). These patients received a postal questionnaire about the occurrence and daily life consequences of inguinal pain before and after the operation. Two reminding letters were sent after 5 and 10 weeks, respectively, to those who had not responded.
TABLE 1. The Process of Patient Selection for the Study
Questionnaire
The self-recording instrument used in the questionnaire was a 7-step fixed point scale with steps operationally linked to behavioral events, including additional monitoring of painduration, termed the “duration-intensity-behavior-scale” (DIBS). The DIBS scale has previously been evaluated regarding compliance, authenticity, reliability, and sensitivity among patients with functional abdominal pain.6 By defining pain operationally in terms of behavior necessitated by the pain, the DIBS instrument escapes, at least to some extent, the dilemma of pain definition and standardization, and the impact on daily life activities is easily inferred. Pain in the contralateral (thus not operated) groin was used as a reference. The entire questionnaire has also recently been validated (submitted manuscript) and found to have high validity and reliability as an instrument for measuring chronic pain following hernia surgery. The validation also included a comparison between the operated and contralateral groin. There was a baseline level of pain in the contralateral groin, but the level of pain was significantly higher in the operated groin.
Statistical Methods
Age-specific prevalence of pain in 10-year age strata at the time of the questionnaire survey was expressed as the number of patients with answers fulfilling our criteria of persistent pain, divided by the total number of patients who gave interpretable answers in the respective age stratum. We calculated 95% confidence intervals (CI) according to the method proposed by Wilson.7
Factors associated with residual pain were determined in multivariate unconditional logistic regression models, with the following independent variables: age in quartiles based on the distribution among subjects with no pain, sex, hernia reducibility on admission (yes/no), type of hernia (lateral, medial, femoral, or combined), size of the defect (>/≤3 cm), level of pain before the operation (≥/< “interferes with concentration on chores and activities”), method of repair (Shouldice, Lichtenstein, Plug techniques, other open mesh techniques, open preperitoneal mesh techniques, other open mesh techniques, Trans Abdominal Pre Peritoneal laparoscopic repair [TAPP] and Total Extra Peritoneal laparoscopic repair[TEP]), techniques not involving exploration of the groin grouped together (TEP, TAPP, and open preperitoneal mesh techniques), recorded postoperative complications (yes/no), hernia surgery volume at the hospital (≥/<200 operations per year), and number of surgeons who performed the operation (1 or 2). The dependent variable was log (p/1 − p), where p was the probability of having any pain (ie, “pain present but can easily be ignored” or more). Separate models were built for “pain right now” and “worst pain last week.” The models were constructed by stepwise selection with entry testing based on the significance of the score statistic, and removal testing based on the likelihood-ratio statistic.
Severe acute postoperative pain is also recorded in the register as a postoperative complication but was not included in the analysis of risk factors for long-term pain since the distinction between acute and chronic postoperative pain is not clear enough to define them as independent and dependent variables in the same multivariate model, ie, acute pain could be considered as part of the causal chain between the operative procedure and the development of chronic pain.
RESULTS
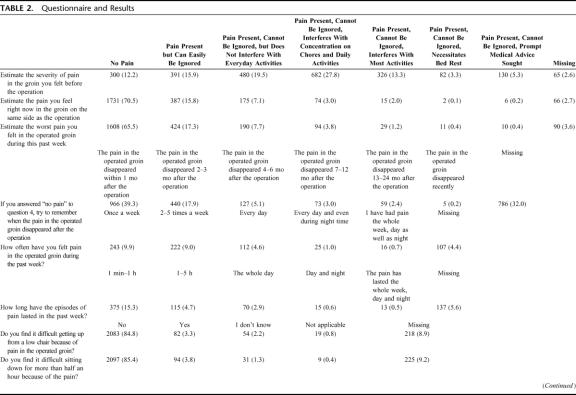
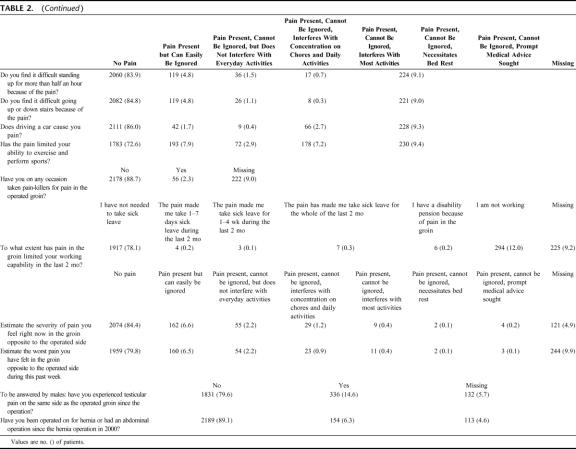
The distribution of answers is presented in Table 2. After 2 reminders, 2456 (86%) of the 2853 patients had responded (2299 men and 157 women). Their mean age at operation was 58.2 years. Reasons for not returning the questionnaire were unknown address in 32 (1%) and failure to respond in the other 365 (13%). There was no difference in age or in proportion of patients with complications or severe postoperative pain recorded in the SHR between patients who responded and those who did not. Postoperative complications included wound infections (n = 34, 1.4%), hematoma (n = 111, 4.4%), severe pain (n = 30, 1.2%), and other (n = 71, 2.9%). Postoperative complications are defined according to the standards of the SHR.4 The proportions of patients with residual pain 24 to 36 months after the operation, stratified for age, technique of repair, type of hernia, size of hernia defect, level of pain before the operation, and postoperative complications are shown in Figures 1 and 2. Since some patients did not answer all questions, the numbers of patients are not identical for “pain right now” and “worst pain last week.”
TABLE 2. Questionnaire and Results
TABLE 2. (Continued)
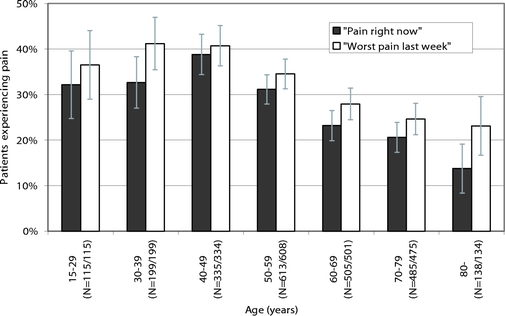
FIGURE 1. Prevalence of residual pain by age. Vertical bars indicate 95% confidence intervals. Numbers in brackets on the x-axis indicate number of responders to the 2 respective questions.
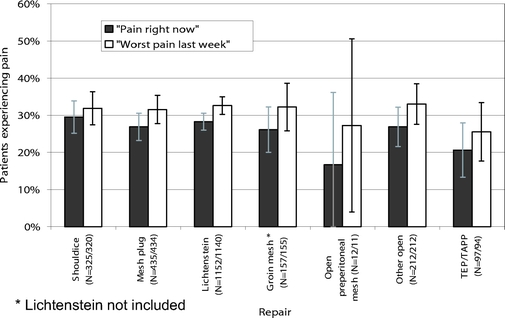
FIGURE 2. Prevalence of residual pain by technique of repair. Vertical bars indicate 95% confidence intervals. Numbers in brackets on the x-axis indicate number of responders to the 2 respective questions.
In answer to the question about “worst pain last week,” 758 patients (31%; 95% confidence interval [CI], 29%–33%) reported some form of pain, whereas 144 (6%; 95% CI, 5%–7%) had had severe pain that could not be ignored and interfered with their daily activities. When asked to estimate the severity of pain before the operation, 2091 (85%) reported some form of pain and 1220 (50%) severe pain. There was no significant association in type of repair and level of preoperative pain in χ2 analysis. In response to questions concerning daily activities, 82 (3.3%; 95% CI, 2.7%–4.1%) stated that it was difficult to get up from a low chair and 119 (4.8%; 95% CI, 4.1%–5.8%) had difficulty in standing up for more than 30 minutes and climbing stairs. In 193 patients (7.9%; 95% CI, 6.9%–9.0%), the pain limited their ability to perform sports. Some period of sick-leave had to be taken by 20 patients (0.8%; 95% CI, 0.5%–1.3%) in the last 2 months and 6 patients (0.2%; 95% CI, 0.1%–0.5%) claimed to be receiving a disability pension for pain in the surgically treated groin. The number of patients still at work in the cohort was 1937 (79%) (Table 3).
TABLE 3. Results of Multivariate Logistic Analysis of Risk Factors Predicting Any Level of Pain Versus No Pain Regarding “Pain Right Now”
In multivariate logistic analysis, a high level of pain before the operation (odds ratio [OR], 2.1; 95% CI, 1.8-2.6; P < 0.001) and postoperative complications (OR, 1.8; 95% CI, 1.2–2.5; P = 0.003) were found to significantly and independently predict residual pain, whereas “age above median” (OR, 0.7; 95% CI, 0.5–0.8; P < 0.001) predicted a decrease in residual pain when “worst pain last week” was used as the outcome variable. No specific technique of repair was significantly associated with an increased or decreased risk of residual pain in either of the 2 multivariate analyses, but the number of patients with long-term pain was small in each category, thus prohibiting statistical ascertainment of anything but very marked relationships. When the techniques were grouped into those that did or did not involve dissection of the groin, however, the latter techniques were associated with a significantly lower risk of long-term pain with “pain right now” as outcome variable (OR, 0.6; P = 0.033). When “worst pain last week” was used as the outcome variable, groin dissection was associated with a nonsignificant decrease of the risk for long-term pain.
DISCUSSION
Our results emphasize that residual pain should be viewed as an essential endpoint when investing the outcome of hernia surgery. After 24 to 36 months, nearly 30% of the patients reported some form of pain or discomfort and close to 6% of all patients reported inguinal pain of such intensity that it disturbed their concentration in activities of daily life during the week preceding follow-up. By contrast, the 6-year cumulative incidence of reoperation for recurrence was reported to be 4.5%.4 Furthermore, this pain caused social disability, interfering with such activities as walking, standing, and sitting in 11.3% to 14.2% of the surgically treated patients. The prevalence of long-term pain in this Swedish patient population conforms with the data reported by Bay-Nielsen and Poobalan3,8 but differs substantially from the experience of Condon9 who found that chronic pain occurred in less than 1%.
Of the variables that were independently associated with an increased risk of residual pain, ie, age, pain level before the operation, techniques involving anterior approach, and postoperative complications, only the operative technique and complications can potentially be controlled by the surgeon. Postoperative complications were found to be linked to an increased risk for long-term pain in our study. Others have not found this link.10 In most studies, however,3,8,11–15 complications do not seem to be evaluated at all in respect to residual pain. Our results indicate that postoperative complications may serve as an important intermediary variable,16 useful in systematic improvement systems aimed to decrease the risk for long-term postherniorrhaphy pain. However, it must be emphasized that the reported associations in this observational study do not necessarily represent causal relationships. Although nobody would dispute the desirability of reducing postoperative complications, data from sufficiently large randomized clinical trials are needed to prove that such efforts would also reduce the risk of long-term pain.
Operations by posterior approach (ie, laparoscopic and open posterior operations) have, in or study, shown to cause less pain than operations by groin incision. Our study did not have sufficient power to detect clinically important advantages of specific repair methods. Hence, differences might well exist. When combined into one category, surgical techniques not involving dissection of the groin were associated with a lower prevalence of residual pain after 24 to 36 months, compared with techniques requiring groin dissection. In view of the ad hoc character of this analysis, however, cautious interpretation is recommended. The results from recent randomized clinical trials comparing laparoscopic TEP or TAPP repair with open tension free mesh repair are conflicting. Some trials resulted in a lower prevalence of postoperative pain in the laparoscopic group,12,13,17 whereas others showed no difference between the treatment arms.11,14 Our finding, if true, should further be weighed against a possibly increased risk of recurrence with such techniques, as indicated in some studies.11,18
In our study, a high level of preoperative pain indicated an increased risk of long-term pain, as reported also by Poobalan et al8 and Courtney et al.15 This might suggest that the hernia disease was already complicated prior to surgery in some patients; stretching, entrapment, and/or inflammation of local nerves are conceivable mechanisms, but psychologic susceptibility or increased pain sensitivity may also play a role. Moreover, the pain prior to the operation may also have originated from other conditions than the hernia, and will then persist after the operation. A third possibility is that interindividual variations in the manner of communicating subjective feelings may have affected the observed relationship. A general inclination to report pain and other feelings in an exaggerated way will most likely persist both before and after the operation and so will a propensity for being stoical. However, a cautious interpretation of these results is needed since the answer to the question of preoperative pain is the patient's recollection of the pain level. The complexity of inguinal pain is underlined by the fact that a substantial proportion of patients also reported pain from the nontreated contralateral groin. Randomized intervention studies are required to answer the question whether special preoperative investigations and/or tailored management, for instance specially adapted analgesia and anesthesia or particularly atraumatic surgical techniques, may diminish the risk of long-term pain among patients with atypically high preoperative pain levels.
Strengths of our study include the population-based approach and the large sample size, albeit too small for precise estimates in relation to factors such as operative technique. The prevalence of residual pain after hernia surgery estimated in this study is considered to mirror population-based results in Sweden, since hospital-based health care, in practice, is population-based and referable only to mutually exclusive hospital catchment areas. An important drawback is that we did not include patients who underwent further inguinal surgery during the 24- to 36-month follow-up period. According to the register, the proportion of the year 2000 cohort that underwent reoperation during our follow-up period was 1.5%. Some of these reoperations might have been prompted by inguinal pain with or without noticeable hernia recurrence, which could lead to an underestimation of the prevalence of severe postoperative pain. Another limitation is the lack of clinical evaluation of the patients who reported residual pain. Although the questionnaire contained questions that were designed to capture obvious recurrences, some of the patients with residual pain may still have had a recurrent hernia.
Hernia surgery has hitherto been focused on attempts to reduce the risk of recurrences, but prevention of long-term pain may require other approaches. To a certain extent, however, efforts aimed at reducing the recurrence rate are likely to coincide with those required to avoid residual pain. Consistent with this assumption is the fact that postoperative complications are a major risk factor for both recurrence19 and for long-term pain. Although unproven in controlled trials, a meticulous technique in the dissection probably will decrease the risk of recurrence as well as of pain. When considering other aspects of surgery, such as choice of repair, the risk of long-term pain may have to be weighed against the risk of recurrence. Furthermore, careful steps to control pain among younger patients and patients with a high level of preoperative pain are important potential fields of improvement and research. One obvious step that is necessary to make improvement possible regarding the endpoint long-term pain is to include evaluation of pain after some years in quality assurance systems for hernia surgery.
Footnotes
Supported by the National Board of Health and Welfare (Sweden).
Reprints: Ulf Fränneby, MD, Department of Surgery, Södersjukhuset, SE-118 83 Stockholm, Sweden. E-mail: ulf.franneby@sodersjukhuset.se.
REFERENCES
- 1.Nilsson E, Haapaniemi S. Hernia registers and specialization. Surg Clin North Am. 1998;78:1141–1155. [DOI] [PubMed] [Google Scholar]
- 2.Kehlet H, Bay-Nielsen M, Kingsnorth A. Chronic postherniorrhaphy pain: a call for uniform assessment. Hernia. 2002;6:178–181. [DOI] [PubMed] [Google Scholar]
- 3.Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg. 2001;233:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SBR (Swedish Hernia Register web site). May 8, 2005. Available at https://sbr.norrnod.se/html/welcome.stm.
- 5.Franneby U, Gunnarsson U, Wollert S, et al. Discordance between the patient's and surgeon's perception of complications following hernia surgery. Hernia. 2005;9:145–149. [DOI] [PubMed] [Google Scholar]
- 6.Sjödén PO, Bates S, Nyrén O. Continuous self-recording of epigastric pain with two rating scales: compliance, authenticity, reliability and sensitivity. J Behav Asess. 1983;5:327–344. [Google Scholar]
- 7.Altman DG, Gardner MJ. Statistics With Confidence. BMJ, 2000. [Google Scholar]
- 8.Poobalan AS, Bruce J, King PM, et al. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg. 2001;88:1122–1126. [DOI] [PubMed] [Google Scholar]
- 9.Condon RE. Groin pain after hernia repair. Ann Surg. 2001;233:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Post S, Weiss B, Willer M, et al. Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg. 2004;91:44–48. [DOI] [PubMed] [Google Scholar]
- 11.Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350:1819–1827. [DOI] [PubMed] [Google Scholar]
- 12.Douek M, Smith G, Oshowo A, et al. Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ. 2003;326:1012–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grant AM, Scott NW, O'Dwyer PJ. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg. 2004;91:1570–1574. [DOI] [PubMed] [Google Scholar]
- 14.Wright D, Paterson C, Scott N, et al. Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg. 2002;235:333–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Courtney CA, Duffy K, Serpell MG, et al. Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg. 2002;89:1310–1314. [DOI] [PubMed] [Google Scholar]
- 16.Gunnarsson U. Quality assurance in surgical oncology: colorectal cancer as an example. Eur J Surg Oncol. 2003;29:89–94. [DOI] [PubMed] [Google Scholar]
- 17.McCormack K, Go PM, Ross S, et al. Laparoscopic techniques versus open techniques for inguinal hernia repair: the Cochrane Library. Update Software (CD 1785), 2003. [DOI] [PMC free article] [PubMed]
- 18.Nordin P, Haapaniemi S, van der Linden W, et al. Choice of anesthesia and risk of reoperation for recurrence in groin hernia repair. Ann Surg. 2004;240:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nilsson E, Haapaniemi S, Gruber G, et al. Methods of repair and risk for reoperation in Swedish hernia surgery from 1992 to 1996. Br J Surg. 1998;85:1686–1691. [DOI] [PubMed] [Google Scholar]