Abstract
This report describes a case of spondylodiscitis occurring adjacent to levels at which anterior cervical discectomy and fusion was performed. The objective is to describe a rare cause of spondylodiscitis and discuss its successful management. Post-operative discitis involving the same level is a known occurrence. We report an interesting case of spondylodiscitis occurring at the adjacent level of fusion, and to our knowledge this is the first such case reported in literature. A two-level decompression and fusion was performed at C5–6 and C6–7 levels with PEEK cages and anterior cervical plating in a middle-aged gentleman for persistent axial neck pain and left-sided radiculopathy involving C6 and C7 distribution. After 6 weeks, the patient presented to us with complaints of mild paresthesia in the abdomen and extremities. Radiological investigations including plain radiographs and MRI revealed a surprising finding of discitis at C4–5 level with an associated epidural abscess. In view of the patient’s myelopathic symptoms, surgical debridement and decompression of the spinal cord was performed. The plate and screws were removed, the cages were left intact, and the C4–5 disc level was reconstructed with tricortical iliac crest autograft. No further instrumentation was performed. The biopsy specimen from the disc at C4–5 level grew Serratia marcescens. It was contemplated that C4–5 discitis was initiated by inoculation of bacteria at the superior endplate of C5 by contaminated vertebral pins/drill-bit or screws. Adjacent level discitis is a rare but potentially serious complication of anterior cervical fusion. A high index of suspicion of infection is necessary if the patient complains of new symptoms after anterior cervical fusion. Thorough assessment and aggressive treatment is necessary for successful management.
Keywords: Adjacent level discitis, Cervical spondylodiscitis, Serratia marcescens, Cervical spine, Epidural abscess
Introduction
Post-operative discitis occurring at the operated level is a known complication of spinal surgery. The most common organisms implicated in the pathogenesis are Staphylococcus aureus and Staphylococcus epidermidis. Degeneration occurring at the adjacent level is also a well-established phenomenon after spinal fusion. We present a unique case of discitis occurring at a level adjacent to the levels that underwent anterior cervical fusion. The case becomes interesting because of numerous factors e.g. the site of involvement, the likely etiology, the organism concerned, the subtle nature of the symptoms, problems with diagnosis and its management.
Case report
A healthy 56-year-old male patient presented with neck pain of 6 months duration and associated radicular pain and numbness in the left upper-limb. The history was negative for fever, night pain or constitutional symptoms. MRI revealed left-sided foraminal stenosis at C5–6 and C6–7 levels secondary to disc herniation. A decision to perform surgical decompression and stabilization was taken after a failure of conservative trial of 12 weeks. A standard anterior cervical discectomy and fusion (ACDF) was performed at both levels using a right-sided approach. Based on anatomical landmarks and radiological guidance, adequate care was taken to expose only the presumed C5–6 and C6–7 disc levels and avoid inadvertent injury to other discs. The Casper distractor system was subsequently utilized throughout the surgery by obtaining anchorage of the Casper vertebral pins in the C5 and C7 vertebral bodies. Iliac crest autograft-packed PEEK (Solis, Stryker, Allendale, NJ, USA) cages were placed at both levels and cervical plating (Orion, Medtronic-Sofamor-Danek, Memphis, TN, USA) was performed. Prophylactic intravenous antiobiotics (cefazolin) was administered 1 h before surgery and continued for 48 h post-surgery. The immediate post-operative period was uneventful and the patient had good recovery from his neurological symptoms.
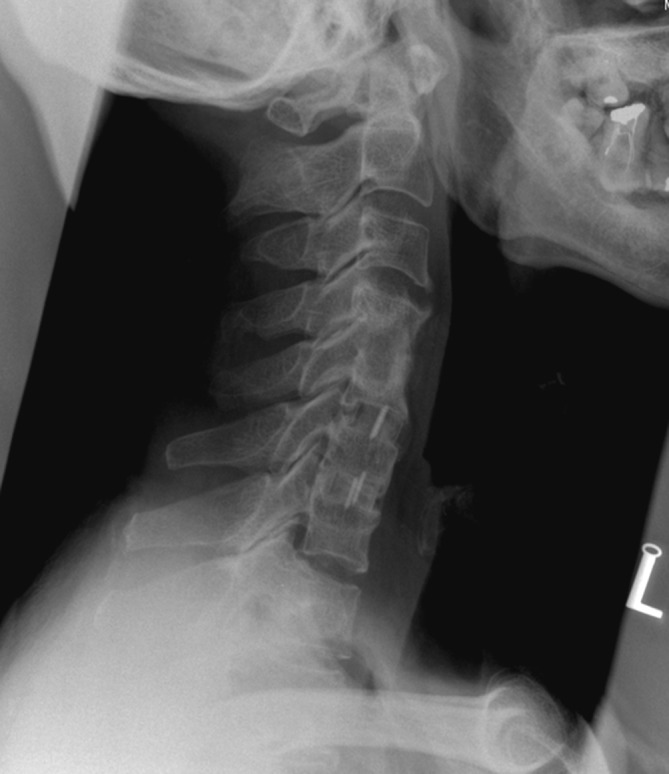
The patient presented 6 weeks later with mild neck and bilateral shoulder pain associated with paresthesia in his upper limbs, left lower limb and abdomen. On examination, the patient was afebrile and there was no warmth or tenderness in the region of the neck. The neck movements were terminally restricted, but there was no motor weakness. Hyperreflexia could be elicited in both lower limbs, Babinski’s sign was negative and there were no objective sensory deficits. Hematological investigations revealed a mild increase in ESR (30 mm/h), normal CRP (1.1 μg/ml) and a mild increase in total WBC count (8.18×109/l). Radiographs revealed persistently enlarged pre-vertebral soft-tissue shadow, decreased disc height at C4–5 level with erosion of end-plates and segmental C4–5 kyphosis, apart from the presence of halo around the screws as shown in Fig. 1. MRI revealed features of discitis at C4–5 level with associated pre-vertebral and epidural abscesses from C4 to C6 levels as well as artifacts secondary to instrumentation and cages as shown in Fig. 2a and b.
Fig. 1.

Lateral X-ray of cervical spine at 6 weeks after index surgery. Persistence of pre-vertebral soft-tissue shadow, erosion and irregularity of C4 and C5 end plates apart from segmental kyphosis and loosening of screws can be seen
Fig. 2.

a Sagittal T-2 weighted MRI image showing hyperintensity signal at C4–5 disc space. Anteriorly located epidural abscess at the same level can be appreciated. b Axial T-2 weighted MRI image displaying anterior compression of the spinal cord by the epidural abscess
The patient underwent an aggressive surgical debridement and stabilization through a left-sided approach. The loose screws and the plate were removed. A thorough decompression of the epidural abscess along with surgical debridement of C4–5 disc space was performed. No pus or evidence of infection was seen at the C5–6 and C6–7 levels and the cages were left behind as they appeared stable and secure. Tricortical iliac-crest autograft was impacted at the prepared C4–5 disc space and thorough lavage with antibiotic solution (cloxacillin and gentamycin) was carried out. The wound was then closed over a drain and an empirical course of intravenous antibiotic (cefazolin) was initiated. The drain was taken out after 3 days and the culture specimen grew Serratia marcescens, sensitive to ceftriaxone but resistant to the more commonly used antibiotics including cefazolin. Intravenous ceftriaxone was initiated for the first 3 weeks, and then the patient was discharged on oral antibiotics for another 3 weeks. The patient’s condition improved dramatically with complete neurological recovery within the first week. At the 8-month mark, he is asymptomatic and the X-rays performed after 5 months reveal solid fusion at all levels and obliteration of the pre-vertebral soft-tissue shadow as shown in Fig. 3.
Fig. 3.
Lateral X-ray at 5 months after the revision surgery. Solid fusion at all levels and obliteration of the pre-vertebral soft-tissue shadow can be seen
Discussion
Post-operative discitis in cervical spine is not a frequent occurrence due to the rich vascularity and the routine use of antibiotic prophylaxis [5]. The prevalence ranges from 0 to 1.1%. The use of metal implants may increase the possibility of infection [4]. Discitis is a known complication of cervical discography [2, 11]. Occasional cases of cervical discitis secondary to a fishbone lodged in the throat have been reported [4, 7].
A case of post-operative discitis adjacent to the operated level has not been previously reported. The potential causes of adjacent level discitis at C4–5 were scrutinized. One of the possibilities was an accidental inoculation of bacteria into the C4–5 disc space intra-operatively by a contaminated spinal needle that was used as a radiological marker. When we reviewed the intra-operative localizing X-ray, it was evident that the needle was placed into the C5–6 intervertebral disc and hence this possibility was ruled out. The possibility of discitis secondary to an esophageal perforation was ruled out since the patient neither had dysphagia nor the severe systemic symptoms that usually accompany esophageal injury in the post-operative period. Additionally, no esophageal tear was noticed during the second surgery. Discitis secondary to annular injury of C4–5 intrevertebral disc was ruled out since great care was taken to avoid inadvertent exposure of uninvolved levels during surgery. Hematogenous spread is another possibility but the only positive cultures came from the C4–5 intervertebral disc during the operation. Other samples, e.g. blood, sputum, and urine cultures demonstrated no growth and chest X-ray appeared normal. The only other possibility could be inoculation of bacteria into the superior endplate of C5 and initiation of an infective process in the C4–5 peridiscal region. This could be through the contaminated Caspar pins or the drill-bit utilized to create holes for the screws used for anterior instrumentation. This is a possibility since the organism that was cultured (S. marcescens) is known to contaminate and breed in normal saline solution [3, 6], and the operative instruments in question are generally placed in seemingly sterile large bowls filled with normal saline during surgery.
Post-operative spinal infection due to S. marcescens is very rare. In a review of 2,391 consecutive index procedures on the spine, 46 cases of wound infection were identified [8]. Amongst them, only one case of Serratia infection was recognized and that was a part of mixed infection. Serratia spondylodiscitis has been reported recently involving the lumbar spine [3]. One of the patients had discitis at the same level that underwent a micro-discectomy. The second case was interesting in that her discitis occurred at the same level that had earlier undergone a posterior decompression (laminotomies and foraminotomies) but the disc was untouched. These two patients presented acutely within a week of index surgery with a fiery presentation, described as life threatening by the authors. The ESR, WBC counts and CRP levels were elevated and the blood culture grew S. marcescens. However, our patient had a subacute course and was afebrile throughout. The only abnormal features were subtle axial neck pain with subjective paresthesia in the extremities and abdomen. The ESR and WBC count were modestly raised but the CRP was normal. A high index of suspicion along with reliance on radiological investigations was essential to diagnose the condition and institute appropriate treatment. Persistence of pre-vertebral soft-tissue shadow apart from reduction in the C4–5 disc height, segmental kyphosis and irregularity of the endplates at C4–5 pointed towards a diagnosis of C4–5 discitis and prompted us to perform MRI in order to confirm the diagnosis and decide on the further management.
The literature is not very clear with respect to the duration of antibiotics to be given for spinal fusions. The protocols recommended range from no antibiotics for anterior spinal surgery [9] to 3 days of antibiotics for all spinal surgeries [10]. A meta-analysis performed to identify the efficacy of prophylactic antibiotics in spinal surgery found that there was no difference in the efficacies of various antibiotic regimens, provided at least one dose of pre-operative antibiotic with gram-positive coverage was administered [1]. Our protocol for antibiotic prophylaxis for spinal surgeries consists of a pre-operative dose followed by 2-day course of intravenous cefazolin. The protocol followed in our division is based on the fact that the drainage tube as well as the urinary catheter is removed by 48 h and hence the antibiotics are usually continued till then. S. marcescens is highly resistant to cefazolin and sensitive to third-generation cephalosporins [3], and this was evident in the culture sensitivity reports of our patient.
An aggressive approach to debride the C4–5 disc space as well as to decompress the epidural space was necessary in the wake of myelopathic symptoms and in order to isolate the organism. The spine was approached from the opposite side (left side) for the second surgery since inadvertent esophageal or neurovascular injury as a result of post-operative scarring was a possibility on the right side. The issue of leaving the PEEK cages at C5–6 and C6–7 levels behind during the revision surgery is debatable. We did not replace them because of a number of reasons. The infection was principally arising from the C4–5 disc level, the cages were absolutely stable and we wanted to minimize graft site morbidity. Most importantly, we felt that infection would not thrive in the presence of stability. This approach has been advocated by other authors too [8]. In the second surgery, a plate was not utilized for instrumentation for the following reasons. Firstly, the bones were soft as a result of inflammatory edema resulting from infection and hence were not ideal for screw implantation. Secondly, since we were also not sure what the organism was and as most of the times it is Staphylococcus aureus, the risk of persistent infection as a result of glycocalyx membrane formation is high. Additionally, the construct appeared stable after the C4–5 level was impacted with the autologous iliac crest graft and the lower two levels were already stable as aforementioned.
Conclusions
The possibility of infection should be considered in patients with an alteration in the nature of their symptoms after index surgery. Unusual presentations can be a challenge to diagnose and treat and a high index of suspicion and aggressive approach are prudent for a successful outcome.
Acknowledgements
No benefits received or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Barker FG., II Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery. 2002;51:391–400. doi: 10.1097/00006123-200208000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Connor PM, Darden BV. Cervical discography complications and clinical efficacy. Spine. 1993;18:2035–2038. doi: 10.1097/00007632-199310001-00018. [DOI] [PubMed] [Google Scholar]
- 3.Hadjipavlou AG, Gaitanis IN, Papadopoulos CA, et al. Serratia spondylodiscitis after elective lumbar spine surgery: a report of two cases. Spine. 2002;27:E507–E512. doi: 10.1097/00007632-200212010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Hagadorn B, Smith HW, Rosnagle RS. Cervical spine osteomyelitis. Secondary to a foreign body in the hypopharynx. Arch Otolaryngol. 1972;95:578–580. doi: 10.1001/archotol.1972.00770080868014. [DOI] [PubMed] [Google Scholar]
- 5.Keiper G, Stambough JL (1998) Complications of cervical spine surgery, 3rd edn. In: The cervical spine. The Cervical Spine Research Society Editorial Committee: Lippincott-Raven Publishers, Philadelphia, pp 891–897
- 6.Russo TA (2005) Diseases caused by gram-negative enteric bacilli, 16th edn. In: Harrison’s principles of internal medicine, vol I. McGraw-Hill, pp 884
- 7.Ooij A, Manni JJ, Beuls EA, et al. Cervical spondylodiscitis after removal of a fishbone. A case report. Spine. 1999;24:574–577. doi: 10.1097/00007632-199903150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein MA, McCabe JP, Cammisa FP. Postoperative spinal wound infection: A review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13:422–426. doi: 10.1097/00002517-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord. 1998;11:124–128. [PubMed] [Google Scholar]
- 10.Wimmer C, Nogler M, Frischhut B. Influence of antibiotics on infection in spinal surgery: a prospective study of 110 patients. J Spinal Disord. 1998;11:498–500. [PubMed] [Google Scholar]
- 11.Zeidman SM, Thompson K, Ducker TB. Complications of cervical discography: analysis of 4400 diagnostic disc injections. Neurosurgery. 1995;37:414–417. doi: 10.1097/00006123-199509000-00007. [DOI] [PubMed] [Google Scholar]


