Abstract
Pneumorrhachis (PR), the presence of intraspinal air, is an exceptional but eminent radiographic finding, accompanied by different aetiologies and possible pathways of air entry into the spinal canal. By reviewing the literature and analysing a personal case of traumatic cervical PR after head injury, we present current data regarding the pathoanatomy, clinical and radiological presentation, diagnosis and differential diagnosis and treatment modalities of patients with PR and associated pathologies to highlight this uncommon phenomenon and outline aetiology-based guidelines for the practical management of PR. Air within the spinal canal can be divided into primary and secondary PR, descriptively classified into extra- or intradural PR and aetiologically subsumed into iatrogenic, traumatic and nontraumatic PR. Intraspinal air is usually found isolated not only in the cervical, thoracic and, less frequently, the lumbosacral regions but can also be located in the entire spinal canal. PR is almost exceptional associated with further air distributions in the body. The pathogenesis and aetiologies of PR are multifold and can be a diagnostic challenge. The diagnostic procedure should include spinal CT, the imaging tool of choice. PR has to be differentiated from free intraspinal gas collections and the coexistence of air and gas within the spinal canal has to be considered differential diagnostically. PR usually represents an asymptomatic epiphenomenon but can also be symptomatic by itself as well as by its underlying pathology. The latter, although often severe, might be concealed and has to be examined carefully to enable adequate patient treatment. The management of PR has to be individualized and frequently requires a multidisciplinary regime.
Keywords: Pneumorrhachis, Intraspinal air, Spinal canal
Introduction
Pneumorrhachis (PR), the phenomenon of intraspinal air, is an exceptional imaging finding, caused by various, mainly traumatic and iatrogenic aetiologies. It is associated with different pathologies and possible pathways of air entry into the spinal canal. Although PR has been previously described, mainly in the radiological literature, spine specialists are less acquainted with this unusual pathological entity.
Therefore, based on a complete review of the medical literature and the analysis of a personal case description, we offer contemporary theories of the development of PR and current management strategies for this uncommon epiphenomenon of coincident underlying injuries and diseases to elucidate this rare phenomenon and to raise awareness to PR and possible coexisting pathologies.
Materials and methods
A comprehensive literature search of the U.S. National Library of Medicine’s Medline bibliographic database was conducted and the international medical literature up to December 2005 has been reviewed for the term “pneumo(r)rhachis” and related appropriate medical subject headings such as intraspinal air, intraspinal pneumoc(o)ele, spinal epidural and subarachnoid pneumatosis, spinal and epidural emphysema, aerorachia, pneumosaccus, air myelogram, pneumomyelogram or pneumomyelography.
Each bibliography and retrieved article were then obtained in complete form, analysed and searched for further citations. Pertinent references cited in the identified articles and other relevant literature were also scanned. Further references of each text were identified, and the text was obtained in complete form and analysed. A new case of cervical PR due to severe head injury was added.
Results
After application of the methods and criteria described above, only isolated case reports and no series of more than three cases of this condition could be found. In total, 71 articles were identified that reported on 86 cases. In addition, we describe a previously unreported case of traumatic cervical PR, which was diagnosed in our department.
Illustrative case
A 51-year-old woman was admitted comatose after an automobile accident and attempted unsuccessful endotracheal intubation with prolonged insufficient mask ventilation. Multiple skin lacerations were present as were blunt thoracic trauma with several rib fractures and severe head injury. The patient was decerebrated with bilateral fixed and dilated pupils. Cranial computerized tomography (CT) examination (Fig. 1) revealed a dislocated left occipital skull fracture radiating into the foramen magnum and petrosal bone and a fracture of the sphenoid sinus accompanied by a large acute right hemispheric subdural haematoma causing midline brain shift, traumatic subarachnoid haemorrhage, cerebral oedema and signs of hypoxemia. Internal pneumocephalus with diffuse air distribution in the basal, prepontine and perimesencephal cisterns and fourth ventricle could be detected. Additional spinal CT (Figs. 2, 3) demonstrated air lucency in the cervical vertebral column indicating extradural PR. Intraspinal air was caused by the transphenoid sinus and petrosal bone fractures thus allowing direct communication of pneumatized air containing cavities with the intracranial space. The penetrated air was then forced caudally due to the elevated intracranial pressure resulting from severe brain injury with diminution of capacity of the intracranial space. Horizontal and head-down position of the patient finally allowed the entrapped air to pass through the foramen magnum into the spinal canal.
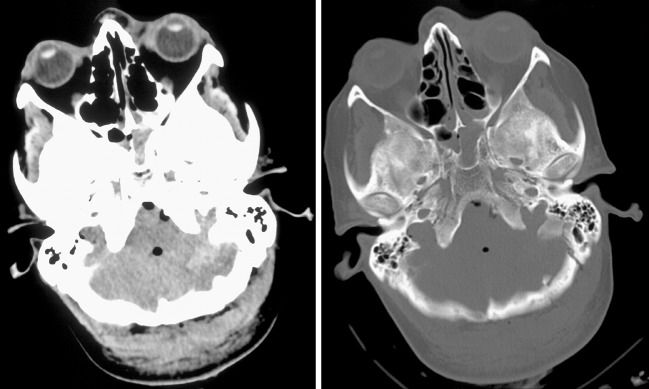
Fig. 1.
Axial cranial CT scans (corresponding soft-tissue and bone window setting) revealing severe head injury accompanied by traumatic internal pneumocephalus with air distributed prepontine, perimesencephally and intraventricullary accompanied by skull fractures of the sphenoid, left occipital and petrosal bone leading to PR
Fig. 2.
Sagittal multiplanar reformatted spinal CT images (corresponding soft-tissue and bone window setting) demonstrating traumatic cervical PR
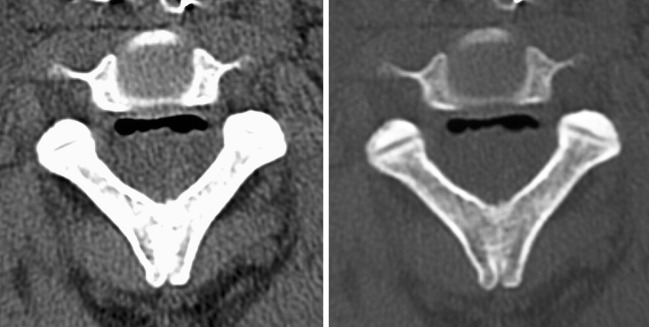
Fig. 3.
Axial CT scans of the cervical spine (corresponding soft-tissue and bone window setting) showing extradural air collection within the ventral spinal canal
The patient remained decerebrated, was transferred to the intensive care unit, considered brain death after adequate examinations and devoted to organ donation.
Discussion
Pathogenesis
Definition and classification
Free air surrounding the dura mater spinalis is an uncommon phenomenon that was primarily reported by Gordon et al. [30] in 1977 and described under various terms such as intraspinal pneumocele [28, 38, 50] or pneumocoele [78], spinal epidural and subarachnoid pneumatosis [4–6, 9, 18, 19, 32–34, 41, 47, 61, 74], spinal and epidural emphysema [4, 11, 23, 27, 28, 33, 59, 65, 69, 70, 72, 77], aerorachia [18, 22, 28, 34], pneumosaccus [9, 28, 62], air myelogram [2, 30, 76], pneumomyelogram [2, 3, 12, 17, 20, 28, 30, 76] or pneumomyelography [26]. The term PR itself was first coined 10 years later by Newbold and co-workers [54]. PR per se usually represents an asymptomatic, probably underdiagnosed epiphenomenon of coincident underlying injuries and diseases. As imaging techniques improve, this pathologic entity has become somewhat more often diagnosed.
PR can be classified descriptively into internal, intradural (intraspinal air within the subdural or subarachnoid space) and external, extradural (intraspinal, epidural air) PR. External PR by itself is usually innocuous, whereas internal traumatic PR frequently is associated with major trauma and believed to be a marker of severe injury [28].
Pathomechanism and aetiology
Apart from artificial, usually traumatic spinal leaks and penetrating spine injuries as a possible explanation for a direct route of intraspinal entry, air may entrap due to a one-way air valve mechanism and dissect indirectly between the paraspinal soft tissues into the epidural space of the spinal canal via the neural foramina and along the vascular and nerve root sheaths, and vice versa, thereby producing PR.
Various conditions may directly or indirectly produce PR including trauma [1–3, 9, 10, 12, 13, 17, 20–22, 26–28, 30, 32, 37–42, 45, 50, 51, 54, 60, 62, 64, 66–68, 73, 74, 76, 78], respiratory complications and conditions that produce high intrathoracic pressure and barotraumas [5, 6, 11, 14, 19, 22–24, 33, 40, 47, 55, 56, 58, 59, 61, 69, 70, 72, 77], recent iatrogenic manipulations during surgical, anaesthesiological and diagnostic interventions [7, 9, 15, 18, 31, 33, 35, 36, 44, 48, 52, 53, 57, 65, 71], malignancy and its associated therapy [29, 49, 63, 75] or it may occur spontaneously [4, 24]. In some cases, PR is an accidental discovery [2] and the conditions and lesions causing PR remain unclear or undetected [12]. The pathologies leading to PR can be generally subsumed and further classified into iatrogenic, traumatic and nontraumatic causes [28].
Thirteen cases are found in the literature describing PR caused by violent coughing due to bronchial asthma or acute bronchitis [11, 14, 23, 24, 40, 55, 56, 58, 59, 70, 72], single cases of PR after cardiopulmonary resuscitation [58], airway obstruction due to foreign body aspiration [69] and two cases each of PR after physical exertion [19, 77] and inhalational drug abuse of 3,4-methylenedioxymethamphetamine (“Ecstasy”) [6] or marijuana [34]. Furthermore, three cases of PR because of prolonged and forceful emesis with diabetic ketoacidosis were documented [5, 47, 61]. Other authors describe PR secondary to traumatic causes including isolated head [3, 10, 17, 30, 38, 39, 62, 68, 50, 76, 78], cervical [2], thoracic [21, 22, 40, 60, 64, 66], abdominal [42] and pelvic injuries [13] or combinations of different injury patterns including spinal trauma [1, 9, 12, 20, 26, 27, 32, 37, 41, 45, 51, 54, 67, 73, 74].
Invasive tumour progression and postradiation changes [29, 49, 63, 75], surgical interventions [33, 36, 65, 71], nasotracheal intubation [18] and peri- or epidural anaesthesia involving a lumbar puncture [7, 9, 15, 31, 35, 44, 48, 52, 53, 57] have also been reported as a cause of PR. Introduction of air as a negative contrast medium into the lumbar subarachnoid space for diagnostic pneumoencephalography or pneumomyelogram, first performed and described by Dandy in 1919, is now only of historical interest [16].
Localization and distribution
Two documented cases with air in the entire spinal canal [12, 55, 56], single cases of air bubbles distributed in the cervical, thoracic and lumbar region [35], and in the cervical and lumbar spine [10], six cases of air in the thoracic and lumbar region [7, 9, 15, 26, 57] and eight cases with both cervical and thoracic PR were previously described [1, 11, 26, 32, 47, 52, 63, 77]. Most cases demonstrate isolated PR of the cervical [2, 3, 5, 10, 17, 20, 30, 38, 39, 45, 50, 51, 54, 60, 66, 68, 69, 74, 76, 78], thoracic [4, 6, 14, 18, 19, 21–24, 27, 29, 33, 34, 37, 40–42, 49, 58, 59, 61, 64, 65, 67, 70–75] or lumbosacral region [9, 10, 13, 31, 36, 44, 48, 53, 57, 62, 70, 72, 74]. Nevertheless, this might be due to the fact that in some cases of PR not a complete examination of the whole spine was carried out. Furthermore, location and distribution of air within the spinal canal is probably depending on the site of air dissection, rate and volume of intraspinal air with large volumes spreading widely, capacity of intraspinal space and positioning of the patient. In cases of external PR, because of the lower resistance from the loose connective tissue, as compared with the rich vascular network that is present anteriorly, the epidural air usually collects in the posterior epidural space [6].
PR may be primary or secondary depending on whether intraspinal air is the cause and origin or effect of associated further occurrence of air in the body.
Almost exceptionally, PR is found in combination with associated air distribution in other compartments and cavities of the body: particularly, in conjunction with pneumocephalus, pneumothorax, pneumomediastinum, peumopericardium or subcutaneous emphysema [3–6, 9–11, 13, 14, 17–24, 26, 27, 29, 30, 32–34, 36–39, 42, 47, 49–51, 54–56, 58–66, 68–70, 72–74, 76–78]. Thus, diagnosis of PR implicates the possibility of the coincidence of associated and hidden further air distributions in the body. Especially, patients with traumatic cervical and intradural PR will almost certainly have injuries of the anterior cranial fossa usually causing subdural PR and skull base or middle and posterior cranial fossae fractures with intracranial subarachnoid air and pneumocephalus, but also penetrating spinal injuries may cause isolated subarachnoid PR without accompanying head injury [2, 17, 76].
Diagnosis
Diagnostic procedures
Since intraspinal air is usually asymptomatic and clinically unspecific, PR is primarily a radiographic and not a clinical diagnosis. The diagnostic work-up of patients with PR should include plain roentgenograms and CT scanning of the spine.
X-ray may be helpful as an initial examination for the early detection of possible associated injuries and to detect larger amounts of intraspinal air [28, 56]. A linear lucency along the spinal canal on a lateral chest radiograph was described as a useful sign in the detection of PR [6]. Moreover, PR itself to some extent acts as a negative contrast agent to delineate canal morphology [78].
The diagnostic tool of choice for a reliable and prompt detection of PR is CT [9, 11, 49, 56]. Nevertheless, on CT, intra- and extradural PR may be difficult to differentiate [28, 60, 67]. Since PR is often combined with air distribution in other parts of the body and traumatic PR is a marker of severe injury, these observations suggest a wider indication for the application of CT, and if necessary, even a systematic total body CT scan or magnetic resonance imaging (MRI). After the initial CT examination follow-up of patients with PR should primarily rely on clinical observations.
Other, not only more sensitive but also more extensive diagnostic techniques such as MRI or myelography are indicated for determining coexisting aetiologies of PR and differential diagnostically examinations [56].
Differential diagnosis
Intraspinal air has to be clearly differentiated from free intraspinal gas collections due to degenerative [25], malignant [43], inflammatory [8] and infectious diseases by gas-forming organisms [46]. It has been demonstrated gas-chromatographically that in cases associated with the so-called vacuum disc phenomenon, the gas collection contains up to 92% nitrogen combined with oxygen, carbon dioxide and other trace gases, in contrast to atmospheric air with a lower nitrogen (78%) and a higher oxygen composition (21%) [25].
Intraspinal gas, which usually has the same low density as air collections on CT, cannot be clearly differentiated by CT examination. It can simulate PR and therefore has to be included in the differential diagnosis of PR. Furthermore, the coincidence of PR and intraspinal gas has to be considered.
Management
Symptomatology
PR in itself usually is asymptomatic, does not tend to migrate and reabsorbs spontaneously and completely with the air being passed directly into the blood in several days without recurrence [3, 4, 6, 10–14, 16, 19, 22–24, 27, 34, 36, 69, 70, 74]. Therefore, patients with PR usually are managed conservatively. As the entrapped air occupies parts of the cerebrospinal compartment thus may cause syndromes of both intracranial and intraspinal hypertension as well as hypotension secondary to either an increase or decrease of intracranial and intraspinal pressure.
Rarely, PR per se is symptomatic and associated with discomfort and pain or even neurological deficits [29, 31, 35, 41, 44, 48, 52, 53, 57, 71, 78]. One case of traumatic PR leading to sensory symptoms has been reported. It was associated with pneumocephalus resulting from closed head injury and treated conservatively by the administration of supplemental oxygen [78]. A single case of a patient with progressive motor deficit of the lower limbs as a result of entrapped intraspinal air, which compressed the spinal cord due to presumptive introduction of air into the intraspinal arachnoid space after repeated lumbar puncture, was demonstrated by Uemura et al. [71]. Altered intrathecal pressure caused by the adhesion of the arachnoid following spinal surgery for lipoma of the thoracic spine may have caused PR in this case. The patient was reoperated with removal of the spinal compression and closure of the dural defect. Gonzales et al. [29] reported a case of reversible spinal cord and lower cervical root dysfunction caused by air dissection through a bronchopleural-epidural-cutaneous fistula likely due to tumour erosion and postradiation changes. The patient underwent surgical exploration of the chest with improvement of symptoms postoperatively. Identification of the epidural space through loss of resistance to air is a widely applied anaesthetic procedure during placement of an epidural catheter. In contrast, intraspinal air may cause undesirable inadequate analgesia during epidural anaesthesia [7, 15]. But injected air also can act as a space-occupying lesion and exert pressure on nervous structures within the spinal canal [7, 15, 31, 48, 52, 53, 57]. Eight cases with postanaesthetic neurological symptoms and pain thought to be complications associated with the application of intraspinal air were reported in the literature [31, 35, 44, 48, 52, 53, 57] including two case descriptions of accidentally injected air into the epidural space via a permanent epidural catheter for continuous epidural anaesthesia [35, 44]. The treatment consisted primarily of removal of the spinal catheter, bed rest and medication for pain relief, without permanent sequelae in most cases [31, 35, 48, 57]. Other treatment modalities included intravenous dexamethasone [53], decompression of the epidural space by percutaneous insertion of a Tuohy needle with air aspiration [44], administration of high concentrations of inspired oxygen with the idea of promoting reabsorption of air from the subdural space or even trials of hyperbaric oxygen therapy [34, 57].
Treatment
Because of the rareness and the different pathogenesis and aetiologies, no empiric guidelines for the treatment of PR and standards of care exist. PR is thought to be associated with an increased morbidity and mortality [14]. Therefore, the whole extent of the conditions causing PR has to be evaluated and the contributing causes leading to PR have to be appropriately treated. PR associated with decreased intraspinal pressure secondary to cerebrospinal fluid leakage usually has a more benign character, whereas entrapped intraspinal air under pressure entering the cranio-spinal compartment usually in combination with a one-way air valve mechanism might cause tension PR and pneumocephalus with nervous tissue compression requiring intervention. Therefore, the authors suggest recognizing the importance of differential diagnosis of the phenomenon of altered intraspinal pressure with either hypo- or hypertension of the cerebrospinal compartment to allow adequate management.
Because of the higher risk of possible meningitis, demonstrable cerebrospinal fluid leaks, if significant or persistent, may have to be repaired neurosurgically [50, 55] or treated by a temporary lumbar spinal catheter [38]. Furthermore, in some cases the underlying pathologies causing PR such as fistulous tracts between intrathoracic structures and the subarachnoid space (thoracoarachnoid fistulas) [29, 63], traumatic lung injury [66, 73] or lung herniation into the spinal canal [37] may require surgical intervention. Although operative repair usually may be uncomplicated, diagnosis and identification of the fistula remains challenging. Other treatment modalities include bronchoscopy for extraction of aspirated foreign bodies causing airway obstruction [69] and transient high concentration oxygen therapy to achieve nitrogen washout [17, 34, 78]. The use of application of prophylactic antibiotic treatment to prevent meningitis and its potential benefit is not instituted and discussed controversial [47, 78]. In principle, apart from antibiotic treatment of underlying infectious diseases such as acute bronchitis [11], even in traumatic PR, we do not recommend prophylactic management with antibiotics in cases of extradural PR and in patients with intradural PR without signs and symptoms of meningitis. The management of patients with PR has to be decided on an individual basis and frequently requires an inter- and multidisciplinary regime.
If intraspinal air is present, especially if caused by trauma, the spine physician has to consider PR as an initial sign of potentially associated, hidden and severe diseases or injuries [55, 56].
If general anaesthesia is required in a patient with PR, because of the presumptive diagnosis of a perforation of the dura mater and additional pneumocephalus, the involved anaesthetist should not use inhalational nitrous oxide, because it may cause expansion of intracavitary air and result in an increase in CSF pressure, as nitrous oxide diffuses into the air-filled space. In addition, pressurisation of the oro- and nasopharynx should be avoided, and alternative anaesthetic techniques such as intermitted positive pressure ventilation with transient high-concentration oxygen should be used, thus preventing an increase in the volume of any intraspinal and intracranial air and promote faster reabsorption of air [17, 34, 57].
The radiologist necessarily has to search for other pathological conditions during the evaluation of a patient with PR and should further investigate the underlying disease or whole extent of injuries. For further treatment of underlying pathologies, other disciplines such as internal medicine, thoracic surgery or ORL may have to be consulted.
The subjects of patients with severe and life-threatening causes leading to PR should be carefully monitored, followed-up and considered for admission to an intensive care unit.
Conclusions
Pneumorrhachis can be caused by a multitude of sources and the evaluation of aetiologies of PR could be a diagnostic challenge. Although PR per se usually is self-limiting and without further therapeutic consequences, prompt recognition of the underlying cause is essential. The attending spine specialist has to carefully evaluate the associated pathologies leading to PR to enable adequate therapy.
Glossary
- CT
Computerized tomography
- MRI
Magnetic resonance imaging
- PR
Pneumorrhachis
References
- 1.Adams MT, Nadalo L, Dunn EL. Air in the spinal canal following blunt chest thoracic trauma. J Trauma. 2003;55:386. doi: 10.1097/01.TA.0000037744.83060.51. [DOI] [PubMed] [Google Scholar]
- 2.Alkan A, Baysal T, Saras K. Early MRI findings in stab wound of the cervical spine two case reports. Neuroradiology. 2002;44:64–66. doi: 10.1007/s002340100646. [DOI] [PubMed] [Google Scholar]
- 3.Amathieu R, Minville V, Poloujadoff MP. Pneumomyélogramme cervical post-traumatique: une entité à ne pas méconnaître. [Cervical post-traumatic pneumomyelogram: do not ignore this entity.] (In French) Ann Fr Anesth Reanim. 2004;23:1089–1092. doi: 10.1016/j.annfar.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Aribas OK, Gormus N, Aydogdu Kiresi D. Epidural emphysema associated with primary spontaneous pneumothorax. Eur J Cardiothorac Surg. 2001;20:645–646. doi: 10.1016/S1010-7940(01)00851-X. [DOI] [PubMed] [Google Scholar]
- 5.Balachandran S, Guinto FC, Goodman P. Epidural pneumatosis associated with spontaneous pneumomediastinum. AJNR Am J Neuroradiol. 1993;14:271–272. [PMC free article] [PubMed] [Google Scholar]
- 6.Bernaerts A, Verniest T, Vanhoenacker F. Pneumomediastinum and epidural pneumatosis after inhalation of “Ecstasy”. Eur Radiol. 2003;13:642–643. doi: 10.1007/s00330-002-1608-7. [DOI] [PubMed] [Google Scholar]
- 7.Boezaart AP, Levendig BJ. Epidural air-filled bubbles and unblocked segments. Can J Anaesth. 1989;36:603–604. doi: 10.1007/BF03005401. [DOI] [PubMed] [Google Scholar]
- 8.Burke V, Mall JC. Epidural gas: an unusual complication of Crohn disease. AJNR Am J Neuroradiol. 1984;5:105–106. [PMC free article] [PubMed] [Google Scholar]
- 9.Catalano O, Grassi R, Gargano V. Gas intraspinale: descrizione di due casi studiati con TC. [Intraspinal gas. CT findings in two cases.] (In Italian) Riv Neuroradiol. 1996;9:239–242. [Google Scholar]
- 10.Çayli SR, Koçak A, Kutlu R. Spinal pneumorrhachis. Br J Neurosurg. 2003;17:72–74. doi: 10.3109/02688690309177976. [DOI] [PubMed] [Google Scholar]
- 11.Chiba Y, Kakuta H. Massive subcutaneous emphysema, pneumomediastinum, and spinal epidural emphysema as complications of violent coughing: a case report. Auris Nasus Larynx. 1995;22:205–208. doi: 10.1016/s0385-8146(12)80061-7. [DOI] [PubMed] [Google Scholar]
- 12.Chibbaro S, Selem M, Tacconi L. Cervicothoracolumbar pneumorachis. Case report and review of the literature. Surg Neurol. 2005;64:80–82. doi: 10.1016/j.surneu.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 13.Chimon JL, Cantos EL. CT recognition of spinal epidural air after pelvic trauma. J Comput Assist Tomogr. 1990;14:795–796. doi: 10.1097/00004728-199009000-00023. [DOI] [PubMed] [Google Scholar]
- 14.Coniglio M, Santis M, Pizzi G. Pneumorachide associato a pneumomediastino spontaneo Desrizione di un caso. [Pneumorachis associated with spontaneous pneumomediastinum. A case report.] (In Italian) Radiol Med (Torino) 1997;94:531–532. [PubMed] [Google Scholar]
- 15.Dalens B, Bazin JE, Haberer JP. Epidural bubbles as a cause of incomplete analgesia during epidural anesthesia. Anesth Analg. 1987;66:679–683. [PubMed] [Google Scholar]
- 16.Dandy WE. Röntgenography of the brain after the injection of air into the spinal canal. Ann Surg. 1919;70:397–403. doi: 10.1097/00000658-191910000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Day CJE, Nolan JP, Tarver D. Traumatic pneumomyelogram. Implications for the anaesthetist. Anaesthesia. 1994;49:1061–1063. doi: 10.1111/j.1365-2044.1994.tb04357.x. [DOI] [PubMed] [Google Scholar]
- 18.Defouilloy C, Galy C, Lobojoie E. Epidurual pneumatosis: a benign complication of benign pneumomediastinum. Eur Respir J. 1995;8:1806–1807. doi: 10.1183/09031936.95.08101806. [DOI] [PubMed] [Google Scholar]
- 19.Delabrousse E, Lerais JM, Jacob D. Pneumorachis spontané au cours d`un effort sportif à glotte fermée. [Spontaneous pneumorachis during sports exertion with a closed glottis.] (In French) J Radiol. 1999;80:1587–1588. [PubMed] [Google Scholar]
- 20.Delamarter RB, Heller J, Bohlman HH. Cervical pneumoyelogram secondary to a closed fracture-dislocation of the thoracic spine. A case report. Spine. 1989;14:1421–1422. doi: 10.1097/00007632-198912000-00025. [DOI] [PubMed] [Google Scholar]
- 21.Delval O, Fossati P, Tailboux L. Air épidural après traumatisme fermé du thorax. [Epidural air after closed thoracic trauma.] (In French) J Radiol. 1998;79:566–568. [PubMed] [Google Scholar]
- 22.Meulder A, Michaux L. Aerorachia. Intensive Care Med. 1990;16:275–276. doi: 10.1007/BF01705167. [DOI] [PubMed] [Google Scholar]
- 23.Dosios T, Fytas A, Zarifis G. Spontaneous epidural emphysema and pneumomediastinum. Eur J Cardiothorac Surg. 2000;18:123. doi: 10.1016/S1010-7940(00)00454-1. [DOI] [PubMed] [Google Scholar]
- 24.Drevelengas A, Kalaitzoglou I, Petridis A. Pneumorrhachis associated with spontaneous pneumomediastinum. Eur J Radiol. 1994;18:122–123. doi: 10.1016/0720-048X(94)90277-1. [DOI] [PubMed] [Google Scholar]
- 25.Ford LT, Gilula LA, Murphy WA. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol. 1977;128:1056–1057. doi: 10.2214/ajr.128.6.1056. [DOI] [PubMed] [Google Scholar]
- 26.Gertzbein SD. Traumatic pneumomyelography. A marker of spinal column injury in the face of innocuous spine fractures: two case reports. Spine. 1998;23:1283–1286. doi: 10.1097/00007632-199806010-00022. [DOI] [PubMed] [Google Scholar]
- 27.Goh BKP, Ng KK, Hoe MNY. Traumatic epidural emphysema. Spine. 2004;29:E528–530. doi: 10.1097/01.brs.0000144832.03555.f5. [DOI] [PubMed] [Google Scholar]
- 28.Goh BKP, Yeo AWY. Traumatic pneumorrhachis. J Trauma. 2005;58:875–879. doi: 10.1097/01.TA.0000158249.77176.9A. [DOI] [PubMed] [Google Scholar]
- 29.Gonzales GR, Payne R, Portenoy RK. Epidural air from a bronchopleural-epidural-cutaneous fistula producing reversible myelopathy and radiculopathy symptoms. Neurology. 1994;44:2409–2410. doi: 10.1212/wnl.44.12.2409. [DOI] [PubMed] [Google Scholar]
- 30.Gordon IJ, Hardman DR. The traumatic pneumomyelogram. A previously undescribed entity. Neuroradiology. 1977;13:107–108. doi: 10.1007/BF00339843. [DOI] [PubMed] [Google Scholar]
- 31.Gracia J, Gomar C, Riambau V. Radicular acute pain after epidural anaesthesia with the technique of loss of resistance with normal saline solution. Anaesthesia. 1998;54:166–171. doi: 10.1046/j.1365-2044.1999.00665.x. [DOI] [PubMed] [Google Scholar]
- 32.Harris PF, Abu-Hijleh MF, Grant CS. Brachial plexus palsy and spinal subarachnoid pneumatosis following trauma. Clin Anat. 1997;10:419–423. doi: 10.1002/(SICI)1098-2353(1997)10:6<419::AID-CA9>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 33.Harzheim A, Kostovic N, Peitz HG. Epidurale Luft im Spinalkanal bei Pneumomediastinum. [Epidural air in the spinal canal in pneumomediastinum.] (In German) Rofo. 1998;169:95–97. doi: 10.1055/s-2007-1015056. [DOI] [PubMed] [Google Scholar]
- 34.Hazouard E, Koninck JC, Attucci S. Pneumorachis and pneumomediastinum caused by repeated Müller`s maneuvers: complications of marijuana smoking. Ann Emerg Med. 2001;38:694–697. doi: 10.1067/mem.2001.118016. [DOI] [PubMed] [Google Scholar]
- 35.Hirsch M, Katz Y, Sasson A. Spinal cord compression by unusual epidural air accumulation after continuous epidural analgesia. AJR Am J Radiol. 1989;153:887–889. doi: 10.2214/ajr.153.4.887. [DOI] [PubMed] [Google Scholar]
- 36.Holton LH, Migaly J, Rolandelli RH. Pneumorrhachis, subcutaneous emphysema, pneumomediastinum, pneumopericardium, and pneumoretroperitoneum after proctocolectomy for ulcerative colitis. Report of a case. Dis Colon Rectum. 2002;45:567–570. doi: 10.1007/s10350-004-6241-x. [DOI] [PubMed] [Google Scholar]
- 37.Hwang WC, Kim HC. CT demonstration of spinal epidural air after chest trauma. Eur Radiol. 2000;10:396–397. doi: 10.1007/s003300050064. [DOI] [PubMed] [Google Scholar]
- 38.Inamasu J, Nakamura Y, Saito R. Air in the spinal canal after skull base fracture. Am J Emerg Med. 2002;20:64–65. doi: 10.1053/ajem.2001.29554. [DOI] [PubMed] [Google Scholar]
- 39.Jarolimek AM, Harris JH., Jr Pneumorachis. Emerg Radiol. 1999;6:146–148. doi: 10.1007/s101400050041. [DOI] [Google Scholar]
- 40.Kakitsubata Y, Inatsu H, Kakitsubata S. CT manifestations of intraspinal air associated with pneumomediastinum. Acta Radiol. 1994;35:305–306. doi: 10.3109/02841859409172388. [DOI] [PubMed] [Google Scholar]
- 41.Kapur A, Sandhu S. Epidural pneumatosis: not necessarily benign. AJNR Am J Neuroradiol. 1994;15:195–196. [PMC free article] [PubMed] [Google Scholar]
- 42.Katz DS, Groskin SA, Wasenko JJ. Pneumorrhachis and pneumocephalus caused by pneumothorax and multiple thoracic vertebral fractures. Clin Imaging. 1994;18:85–87. doi: 10.1016/0899-7071(94)90154-6. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy C, Phillips R, Kendall B. Epidural gas: an unusual complication of metastatic oesophageal carcinoma. Neuroradiology. 1990;32:67–69. doi: 10.1007/BF00593947. [DOI] [PubMed] [Google Scholar]
- 44.Kennedy TM, Ullman DA, Harte FA. Lumbar root compression secondary to epidural air. Anesth Analg. 1988;67:1184–1186. doi: 10.1213/00000539-198812000-00015. [DOI] [PubMed] [Google Scholar]
- 45.Khodadadyan C, Hoffmann R, Neumann K. Unrecognized pneumothorax as a cause of intraspinal air. Spine. 1995;20:838–840. doi: 10.1097/00007632-199504000-00019. [DOI] [PubMed] [Google Scholar]
- 46.Kirzner H, Oh YK, Lee SH. Intraspinal air: a CT finding of epidural abscess. AJR Am J Roentgenol. 1988;151:1217–1218. doi: 10.2214/ajr.151.6.1217. [DOI] [PubMed] [Google Scholar]
- 47.Koelliker PD, Brannam LA. Epidural pneumatosis associated with spontaneous pneumomediastinum: case report and review of the literature. J Emerg Med. 1999;17:247–250. doi: 10.1016/S0736-4679(98)00162-0. [DOI] [PubMed] [Google Scholar]
- 48.Krishnam, Mallick A. Air in the epidural space leading to a neurological deficit. Anaesthesia. 2003;58:292–293. doi: 10.1046/j.1365-2044.2003.306721.x. [DOI] [PubMed] [Google Scholar]
- 49.Lerner EJ, Bilaniuk LT. Spontaneous bronchial-subarachnoidal fistula: an unusual cause of pneumocephalus. AJNR Am J Neuroradiol. 1989;10:S103. [PMC free article] [PubMed] [Google Scholar]
- 50.Mangiardi JR, Brisson P, Weitzner I. Traumatic intraspinal pneumocele. Surg Neurol. 1987;27:587–588. doi: 10.1016/0090-3019(87)90161-3. [DOI] [PubMed] [Google Scholar]
- 51.McCall CS, Nguyen TQ, Vines FS. Pneumocephalus secondary to tension pneumothorax associated with comminuted fracture of the thoracic spine. Neurosurgery. 1986;19:120–122. doi: 10.1097/00006123-198607000-00020. [DOI] [PubMed] [Google Scholar]
- 52.Miguel R, Morse S, Murtagh R. Epidural air associated with multiradicular syndrome. Anesth Analg. 1991;73:92–94. doi: 10.1213/00000539-199107000-00018. [DOI] [PubMed] [Google Scholar]
- 53.Nay PG, Milaszkiewicz R, Jothilingam S. Extradural air as a cause of paraplegia following lumbar analgesia. Anaesthesia. 1993;48:402–404. doi: 10.1111/j.1365-2044.1993.tb07013.x. [DOI] [PubMed] [Google Scholar]
- 54.Newbold RG, Wiener MD, Vogler JB., 3rd Traumatic pneumorrhachis. AJR Am J Roentgenol. 1987;148:615–616. doi: 10.2214/ajr.148.3.615. [DOI] [PubMed] [Google Scholar]
- 55.Oertel MF, Korinth MC, Reinges MHT. Pneumorrhachis of the entire spinal canal. J Neurol Neurosurg Psychiatry. 2005;76:1036. doi: 10.1136/jnnp.2004.044636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oertel MF, Korinth MC, Truong HT. Pneumorrhachis. Neuroradiology. 2004;46:S171. [Google Scholar]
- 57.Overdiek N, Grisales DA, Gravenstein D. Subdural air collection: a likely source of radicular pain after lumbar epidural. J Clin Anesth. 2001;13:392–397. doi: 10.1016/S0952-8180(01)00272-0. [DOI] [PubMed] [Google Scholar]
- 58.Pedicelli G, Santis M, Mattia P, et al. Pneumorachis following asthma-induced barotrauma CT recognition of an unusual manifestation of life-threatening asthma. Eur Radiol. 1997;7:S100. [Google Scholar]
- 59.Pifferi M, Marrazzini G, Baldini G. Epidural emphysema in children with asthma. Pediatr Pulmonol. 1997;24:125–126. [PubMed] [Google Scholar]
- 60.Place JN, Pezzuti RT. Clinical significance of taumatic pneumorrhachis. AJR Am J Roentgenol. 1989;53:655. doi: 10.2214/ajr.153.3.655-a. [DOI] [PubMed] [Google Scholar]
- 61.Pooyan P, Puruckherr M, Summers JA. Pneumomediastinum, pneumopericardium, and epidural pneumatosis in DKA. J Diabetes Complications. 2004;18:242–247. doi: 10.1016/S1056-8727(03)00059-X. [DOI] [PubMed] [Google Scholar]
- 62.Prins TR, Vencken LM. Traumatic pneumosaccus. Neuroradiology. 1989;31:290. doi: 10.1007/BF00344366. [DOI] [PubMed] [Google Scholar]
- 63.Ristagno RL, Hiratzka LF, Rost RC., Jr An unusual case of pneumorrhachis following resection of lung carcinoma. Chest. 2002;121:1712–1714. doi: 10.1378/chest.121.5.1712. [DOI] [PubMed] [Google Scholar]
- 64.Romano L, Rossi G, Pinto A. Su un caso di rottura della trachea da trauma chiuso associata a pneumoretroperitoneo e a pneumorachide. [A case of tracheal rupture caused by blunt trauma associated with pneumoretroperitoneum and intraspinal gas.] (In Italian) Radiol Med (Torino) 1996;92:642–644. [PubMed] [Google Scholar]
- 65.Schneider LJ, Haller JO, Cao H. CT recognition of spinal epidural air after chest tube placement. Pediatr Radiol. 1995;25:228. doi: 10.1007/BF02021543. [DOI] [PubMed] [Google Scholar]
- 66.Scialdone CJ, Wagle W. Intraspinal air: an unusual manifestation of blunt chest trauma. Clin Imaging. 1990;14:59–60. doi: 10.1016/0899-7071(90)90121-Q. [DOI] [PubMed] [Google Scholar]
- 67.Silver SF, Nadel HR, Flodmark O. Pneumorrhachis after jejunal entrapment caused by a fracture dislocation of the lumbar spine. AJR Am J Roentgenol. 1988;150:1129–1130. doi: 10.2214/ajr.150.5.1129. [DOI] [PubMed] [Google Scholar]
- 68.Sinha PA, Mantle M. Cervical pneumorrhachis. Clin Radiol. 2000;55:569–570. doi: 10.1053/crad.1999.0099. [DOI] [PubMed] [Google Scholar]
- 69.Tambe P, Kasat LS, Tambe AP (2005) Epidural emphysema associated with subcutaneous emphysema following foreign body in the airway. Pediatr Surg Int 13;DOI 10.1007/s00383-005-1445-2 [DOI] [PubMed]
- 70.Tsuji H, Takazakura E, Terada Y. CT demonstration of spinal epidural emphysema complicating bronchial asthma and violent coughing. J Comput Assist Tomogr. 1989;13:38–39. doi: 10.1097/00004728-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 71.Uemura K, Behr R, Roosen K. Symptomatic intraspinal air entrapment. Br J Neurosurg. 2000;14:154–156. doi: 10.1080/02688690050004642. [DOI] [PubMed] [Google Scholar]
- 72.Klooster JM, Grootendorst AF, Ophof PJA. Pneumomediastinum: an unusual complication of bronchial asthma in a young man. Neth J Med. 1998;52:150–154. doi: 10.1016/S0300-2977(98)00012-6. [DOI] [PubMed] [Google Scholar]
- 73.Weber P, Vastmans J, Gartner C. Bronchusruptur kombiniert mit Brustwirbelsäulenluxationsfraktur durch direktes Trauma. [Bronchial rupture combined with luxation fracture of the thoracic spine following direct trauma.] (In German) Unfallchirurg. 2004;107:1093–1098. doi: 10.1007/s00113-004-0792-0. [DOI] [PubMed] [Google Scholar]
- 74.Willing SJ. Epidural pneumatosis: a benign entity in trauma patients. AJNR Am J Neuroradiol. 1991;12:345. [PMC free article] [PubMed] [Google Scholar]
- 75.Wippold FJ, Schnapf D, Bennet LL. Esophago-subarachnoid fistula an unusual complication of esophageal carcinoma. J Comp Assist Tomogr. 1982;6:147–149. doi: 10.1097/00004728-198202000-00024. [DOI] [PubMed] [Google Scholar]
- 76.Yip L, Sweeny PJ, McCarroll KA. The traumatic air myelogram. Am J Emerg Med. 1990;8:332–334. doi: 10.1016/0735-6757(90)90089-I. [DOI] [PubMed] [Google Scholar]
- 77.Yoshimura T, Takeo G, Souda M. CT demonstration of spinal epidural emphysema after strenuous exercise. J Comput Assist Tomogr. 1990;14:303–304. doi: 10.1097/00004728-199003000-00029. [DOI] [PubMed] [Google Scholar]
- 78.Yousaf I, Flynn P, McConnell R. Symptomatic intraspinal pneumocele resulting from closed head injury. Br J Neurosurg. 2003;7:248–269. doi: 10.1080/0268869031000153143. [DOI] [PubMed] [Google Scholar]