Abstract
In order to avoid the morbidity from autogenous bone harvesting, bone graft substitutes are being used more frequently in spinal surgery. There is indirect radiological evidence that bone graft substitutes are efficacious in humans. The purpose of this four-case study was to visually, manually, and histologically assess the quality of a fusion mass produced by a collagen hydroxyapatite scaffold impregnated with autologous bone marrow aspirate for posterolateral fusion. Four patients sustained an acute thoracolumbar fracture and were treated by short posterior segment fusion using the AO fixateur interne. Autologous bone marrow (iliac crest) impregnated hydroxyapatite-collagen scaffold was laid on the decorticated posterior elements. Routine implant removal was performed after a mean of 15.3 months (12–20). During this second surgery, fusion mass was assessed visually and manually. A bone biopsy was sent for histological analysis of all four cases. Fusion was confirmed in all four patients intraoperatively and sagittal stress testing confirmed mechanical adequacy of the fusion mass. Three out of the four (cases 2–4) had their implants removed between 12 and 15 months after the index surgery. All their histological cuts showed evidence of newly formed bone and presence of active membranous and/or enchondral ossification foci. The last patient (case 1) underwent implant removal at 20 months and his histological cuts showed mature bone, but no active ossification foci. This four-case report suggests that the fusion mass produced by a mineralized collagen matrix graft soaked in aspirated bone marrow is histologically and mechanically adequate in a thoracolumbar fracture model. A larger patient series and/or randomized controlled studies are warranted to confirm these initial results.
Keywords: Thoracolumbar spine, Fracture, Fusion, Bone graft substitute
Introduction
Effectiveness of a bone graft can be described as having three core properties: osteoinductivity, osteoconductivity and osteogenicity [25, 28]. Autogenous bone graft is the only biological structure simultaneously possessing all three properties. However, the long-term morbidity due to autogenous bone harvesting can be as high as 30%, although improved technique has probably lowered the incidence [1, 2, 10, 26]. Allograft bone is the primary alternative to autograft for a number of spinal fusion procedures. However, allograft bone is a poor posterior onlay graft with rates of fusion reported to be consistently lower than autograft except in cases of pediatric deformity [4, 12, 17, 18]. Therefore, there has been an increasing shift in the past decade to the use of bone graft substitutes for spinal fusion.
One commercially available bone graft substitute comprised a Type I mineralized collagen matrix (MCM), coated with hydroxyapatite (Healos® Bone Graft Substitute, DePuy Spine, Inc, Raynham, MA, USA). Kraiwattanapong et al. [21] reported a 0% fusion rate for posterolateral fusion with MCM and bone marrow in rabbits. However, in that study, bone marrow was harvested from the iliac crest which is not a rich source of osteoprogenitor cells in rabbits. Despite these unique findings, the efficacy of this bone graft substitute has been demonstrated in a previous rabbit study of posterolateral fusion preformed by Tay et al. [29] harvesting bone marrow from rabbit tibiae, with a fusion rate of 100%. Autogenous bone marrow aspirate has been successfully used in the treatment of congenital and post-traumatic pseudarthrosis [7, 11, 28]. The effectiveness of this method has been further enhanced by the use of a three-dimensional scaffold which avoids wash out of osteogenic bone marrow cells by blood circulation. In humans, Kitchel has recently reported two lumbar posterolateral fusion studies [19, 20] demonstrating equivalent rates of fusion for MCM to autograft using CT scans for assessment.
The current understanding of fracture healing is primarily based on animal histological and radiological studies. The majority of human studies discussing fusion rates are based on radiological fusion criteria which are not completely reliable, even when CT scans are utilized [6]. In a 1993 study involving spinal implant removal following fusion, Blumenthal et al. [3] found an overall agreement between preoperative radiographs and surgical findings in only 69% of the cases. Brodsky et al. [5] found a similar overall agreement in their study published in 1991. The ultimate method to assess the quality of a fusion is perioperative manual palpation and histological analysis of a bone biopsy following implant removal.
There are no reports in the literature of the histological behavior of this bone graft substitute in humans. We present here our findings of radiological and histological results on four patients that had surgery performed for an acute thoracolumbar fracture without neurologic deficit.
Materials and methods
Five consecutive patients underwent surgical management for an acute vertebral fracture of the thoracolumbar spine without neurologic deficit. There were three females and two male patients, and the mean age was 47 years (range 30–64). Three patients sustained their fracture after a fall from a horse, one patient after a fall from a scaffold, the last after a fall from a tree. All patients were initially admitted to our institution, which is a level one trauma facility. Initial management was applied according to Advanced Trauma Life Support (ATLS®) guidelines. Four out of the five patients were diagnosed with no other lesion than the vertebral fracture. The patient who fell from a scaffold was also diagnosed with pulmonary contusions and severe tibial pilon fractures, open type IIIA according to Gustilo’s classification [13, 14]. All patients were worked-up under standard hospital protocol which included plain anteroposterior and lateral radiographs as well as a CT scan of the spine.
The AO classification was used to characterize the type of fracture in each patient [23]. Three patients sustained an L1 fracture: two patients had a type A2.3 (Burst-split), one patient had a type B1.2 fracture (flexion-distraction). One patient sustained a type C2.1 fracture (flexion-distraction with rotation) of T12. The fifth patient sustained a type A3.1 fracture of L2 (lateral burst).
All patients were conscious and given the choice between non-surgical and surgical management of their fracture after discussing with each of them the advantages and disadvantages of each treatment method, and alternatives. All patients signed an informed written consent to be included in this pilot study. All surgeries were performed by two fellowship trained surgeons (AAF and AJK).
Surgical technique
The short segment fusion-stabilization technique as described originally by Lindsey and Dick [9, 22] was utilized. The spine was approached posteriorly with a midline incision. Musculature was detached subperiosteally and the fracture was exposed posteriorly, both inferiorly and superiorly, to immediately adjacent vertebrae, taking care to preserve the facet joints of the intact segment. Following this, pedicle screws were placed in one vertebra above and one vertebra below the fracture under fluoroscopic control. Whenever possible, the authors attempted to stabilize (and fuse) only one segment if pedicle screws could be placed in the fractured vertebra, typically hemiburst fractures (AO classification type A3.1) where the inferior part of the vertebral body is primarily intact. This was not possible in either of the patients with type A fractures in this study. Following pedicle screw placement, careful decortication of the facet joints and posterior arch of the fractured vertebra was performed. Typically, transverse processes are not decorticated unless a laminectomy to achieve decompression is necessary.
Percutaneous aspiration of 10 cc of autogenous bone marrow from the posterior iliac crest was performed. Two 5 cc rectangles of the MCM graft were saturated with the bone marrow aspirate and laid bilaterally on the posterior elements previously decorticated. No other bone, bone graft extender, or substitute was placed as part of the graft. In the patient who sustained a lateral burst fracture, we performed a transpedicular bone grafting of the vertebral body, but no other graft substitute other than Healos® was used for the posterior fusion stabilization. Rods were connected to the pedicle screws and fracture reduction in the sagittal plane, and when necessary coronal plane, was achieved by means of ligamentotaxis through the “fixateur interne” (USS®: Universal Spine System, Synthes Spine, Paoli, PA, USA) as described by Walter Dick [9, 22].
Standard procedure with this instrumentation is to remove it at 12 months following surgery when radiological and clinical healing is evident. There are two major reasons for this: (1) implant removal allows the fixed but non-fused segment to recover some mobility which may protect the adjacent segment from accelerated degeneration; (2) in general, after the fracture is radiologically healed, patients experience some discomfort when trying to increase their physical activity. Patients clearly differentiate this discomfort from the pain they had from the fracture and during the healing period. The USS system is in fact a very bulky implant, which the authors believe, is eventually responsible for this discomfort.
Due to surgeon and patient availability, the time to instrumentation removal is often variable, but always performed at a minimum of 12 months following the index surgery at our institution. When radiological and clinical healing was achieved, implant removal was performed in four patients. The fifth patient declined implant removal following healing of the fracture because she did not experience any discomfort. Technically, the second surgery required a very short general anesthesia and lasted approximately 30 min from skin incision to skin suture.
During the second surgery, the mechanical stability of the fused segment was tested using thin curettes introduced in the pedicle screw tracts and manual stress was applied sagittally. A bone biopsy was performed in the heart of the fusion mass which was clearly distinguishable from the lamina and sent for histological analysis. Biopsies were sent in formalin to the institution’s pathology department. They were then decalcified in formic acid, embedded in paraffin and cut in 3-μm slices with a microtome. They were further colored with hematoxylin–eosin and analyzed under a microscope at magnifications ranging from 20× to 400×.
Radiological assessment
Anteroposterior and lateral radiographs were taken in the supine position immediately after surgery, in the standing position a few days after surgery, then at approximately 6 weeks, 3, 6, and 12 months following the index surgery, as well as following implant removal. Assessment of healing radiographically was based only on the remodeling of the vertebral body. Overall fusion assessment was based on radiographic healing of the vertebral body as well as patient pain, function, and activity level. Fusion of the posterior elements could not be assessed radiologically. CT scan was not used because it would not have been possible to assess fusion status of the posterior elements due to metallic artifacts from implants. When smoothening of bony edges and some sclerosis of the fractured vertebral body became visible, the fracture was considered to be healed. This was also based on the patient’s subjective appreciation. When fracture and surgery pain regressed and the patient felt he or she could go back to almost all previous all day activity, the fracture was considered clinically healed. No specific clinical outcome scale was used in this limited patient sample.
Results
The four patients who had the secondary surgery underwent implant removal after a mean period of 15.3 months from the index surgery (12–20). All patients had returned to their previous activity at latest follow-up, except one who was involved in worker’s compensation litigation.
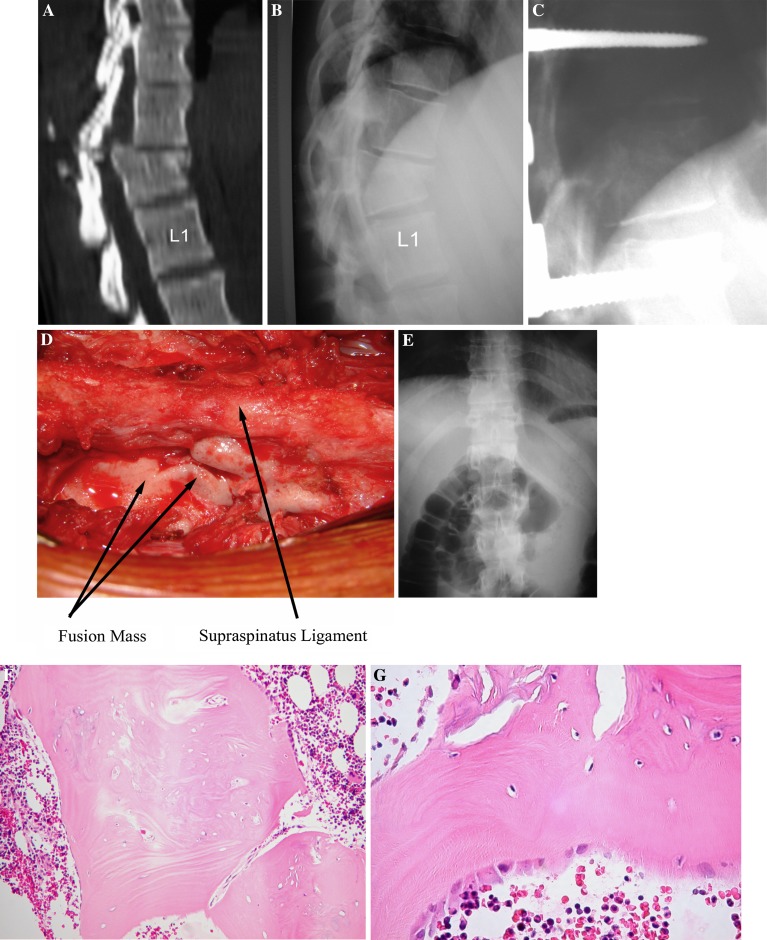
During the second surgery, we visually confirmed that the resorbable matrix had been replaced by new bone (Fig. 1) and that this new bone had formed at the location where the MCM graft had been laid. Manual palpation and sagittal stress through curettes placed in the pedicle tracts demonstrated that no movement could be detected visually in any of the four patients.
Fig. 1.
This 30-year-old female sustained an AO type C2.1 fracture of T12 after a fall from a horse. Initial work-up in the ER did not show any other lesion. She was neurologically intact. We performed a T11-L1 posterior short segment fusion as previously described. Implant removal was performed 14 months following the index surgery. The biopsy demonstrated irregular bony trabeculae, foci of enchondral ossification and numerous osteoblasts, all characteristic elements of ongoing bone remodeling. Several aggregates of lymphoplasmocytes were observed and have been attributed to a foreign body inflammatory type of response. a Preoperative sagittal CT. b Preoperative lateral radiograph. c Lateral radiograph at 5 months postop. d Perioperative image of extensive new bone growth during the secondary surgery. e AP radiograph 15 months following the index surgery after implant removal. f Histology at 100× magnification. g Histology at 400× magnification
Histological analysis of these four cases showed clear evidence of newly formed bone. Patients 1, 3, and 4 had implant removal performed between 12 and 15 months follow-up. Their histological cuts also showed several foci of active membranous and/or enchondral ossification. Interestingly, patient 2 had implant removal performed at 20 months of follow-up and though his histology cuts showed newly formed bone, he had no visible active ossification focus. Patient 3 had implant removal performed at 14 months. His histology showed newly formed bone and active ossification foci.
Discussion
Autogenous graft harvesting site morbidity is a significant issue, and the incidence may be underestimated [15]. Other substitutes such as hydroxyapatite [30–33] and other ceramics have had variable results when used for spinal fusion or other orthopedic applications. Disease transmission through allograft though remote, still remains a possibility. The effectiveness of bone morphogenetic proteins (BMPs) has been shown in human clinical trials. But high cost, unknown potential long-term biological effects, and issues with carriers and dosing may alter widespread clinical use, at least in the short term [16, 27].
Autogenous bone marrow aspirate has been successfully used in the treatment of congenital and post-traumatic pseudarthrosis [7, 8, 11, 25, 28]. In 1997, Muschler et al. [24] studied the prevalence and concentration of osteoblastic progenitors in marrow aspirates from the anterior iliac crest of 32 patients without systemic disease. They determined the number of alkaline phosphatase-positive colony-forming units that grew after placing the bone-marrow derived cells into tissue-culture medium. Three important conclusions have been drawn from this study: (1) the authors estimated that 80% of the cells found in the first 2 ml of aspirated bone marrow have a prevalence of alkaline phosphatase-positive colony-forming of one for 35,000 nucleated cells; (2) the bone marrow derived cells concentration decreases with the volume of aspirate due to dilution; (3) the cellularity of bone marrow and the prevalence of osteoblastic progenitor cells significantly differ between humans. The prevalence of osteogenic precursors cells, can be increased by centrifugation [7] or using a three-dimensional structure to which these cells can attach [25]. MCM is such a three-dimensional matrix.
As described previously, implant removal was performed usually as soon as there was radiological evidence of vertebral body fracture healing and the patient could return to all-day activity, but not earlier than 12 months after surgery. Patient 2, who suffered from a polytrauma, underwent repeat surgery for his open pilon fractures and was bound to a wheelchair for a long period. This is the reason why implant removal has been done later than in other patients, almost 2 years after index surgery (20 months).
Conclusions
We conclude that this study shows some evidence that this MCM graft may be a valid bone substitute for posterior or posterolateral spinal fusion under favorable conditions: presence of bone marrow cells, presence of healthy bleeding bone and mechanical stability (provided by the AO fixateur interne in these cases). A larger patient series and/or randomized controlled studies are warranted to confirm these initial results.
References
- 1.Acocella A, Nardi P, Tedesco A, et al. Anterior iliac bone grafts: techniques and sequelae. Report on 107 cases and review of the literature. Minerva Stomatol. 2003;52:441–453. [PubMed] [Google Scholar]
- 2.Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine. 1995;20:1055–603. doi: 10.1097/00007632-199505000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal SL, Gill K. Can lumbar spine radiographs accurately determine fusion in postoperative patients? Correlation of routine radiographs with a second surgical look at lumbar fusions. Spine. 1993;18:1186–1189. doi: 10.1097/00007632-199307000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, O’Brien MF, Lenke LG, et al. Posterior spinal fusion supplemented with only allograft bone in paralytic scoliosis. Does it work? Spine. 1994;19:2658–2666. [PubMed] [Google Scholar]
- 5.Brodsky AE, Kovalsky ES, Khalil MA. Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine. 1991;16:S261–S265. doi: 10.1097/00007632-199106001-00017. [DOI] [PubMed] [Google Scholar]
- 6.Christensen FB, Laursen M, Gelineck J, et al. Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detailed classification system in posterolateral spinal fusion. Spine. 2001;26:538–544. doi: 10.1097/00007632-200103010-00018. [DOI] [PubMed] [Google Scholar]
- 7.Connolly JF, Guse R, Tiedeman J, et al. Autologous marrow injection as a substitute for operative grafting of tibial nonunions. Clin Orthop Relat Res. 1991;266:259–270. [PubMed] [Google Scholar]
- 8.Connolly JF, Guse R, Tiedeman J, et al. Autologous marrow injection for delayed unions of the tibia: a preliminary report. J Orthop Trauma. 1989;3:276–282. doi: 10.1097/00005131-198912000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Dick W, Kluger P, Magerl F, et al. A new device for internal fixation of thoracolumbar and lumbar spine fractures: the ‘fixateur interne’. Paraplegia. 1985;23:225–232. doi: 10.1038/sc.1985.38. [DOI] [PubMed] [Google Scholar]
- 10.Fernyhough JC, Schimandle JJ, Weigel MC, et al. Chronic donor site pain complicating bone graft harvesting from the posterior iliac crest for spinal fusion. Spine. 1992;17:1474–1480. doi: 10.1097/00007632-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Garg NK, Gaur S. Percutaneous autogenous bone-marrow grafting in congenital tibial pseudarthrosis. J Bone Joint Surg [Br] 1995;77:830–831. [PubMed] [Google Scholar]
- 12.Grogan DP, Kalen V, Ross TI, et al. Use of allograft bone for posterior spinal fusion in idiopathic scoliosis. Clin Orthop. 1999;369:273–278. doi: 10.1097/00003086-199912000-00028. [DOI] [PubMed] [Google Scholar]
- 13.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg [Am] 1976;58:453–458. [PubMed] [Google Scholar]
- 14.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Heary RF, Schlenk RP, Sacchieri TA, et al. Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery. 2002;50:510–517. doi: 10.1097/00006123-200203000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Issack PS, DiCesare PE. Recent advances toward the clinical application of bone morphogenetic proteins in bone and cartilage repair. Am J Orthop. 2003;32:429–436. [PubMed] [Google Scholar]
- 17.Jones KC, Andrish J, Kuivila T, et al. Radiographic outcomes using freeze-dried cancellous allograft bone for posterior spinal fusion in pediatric idiopathic scoliosis. J Pediatr Orthop. 2002;22:285–289. doi: 10.1097/00004694-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Jorgenson SS, Lowe TG, France J, et al. A prospective analysis of autograft versus allograft in posterolateral lumbar fusion in the same patient. A minimum of 1-year follow-up in 144 patients. Spine. 1994;19:2048–2053. doi: 10.1097/00007632-199409150-00005. [DOI] [PubMed] [Google Scholar]
- 19.Kitchel S (2006) A preliminary comparative study of radiographic results using mineralized collagen and bone marrow aspirate vs. autologous bone in the same patients undergoing posterior lumbar interbody fusion with instrumented posterolateral lumbar fusion. Spine J (in press) [DOI] [PubMed]
- 20.Kitchel S (2005) A prospective study of mineralized collagen and bone marrow aspirate as a bone graft substitute in instrumented posterolateral lumbar fusions: 1 and 2 year follow-up. Presented at the 20th annual meeting of the AANS/CNS section on disorders of the spine and peripheral nerves. Phoenix, Arizona
- 21.Kraiwattanapong C, Boden SD, Louis-Ugbo J, et al. Comparison of Healos/bone marrow to INFUSE(rhBMP-2/ACS) with a collagen-ceramic sponge bulking agent as graft substitutes for lumbar spine fusion. Spine. 2005;30:1001–1007. doi: 10.1097/01.brs.0000160997.91502.3b. [DOI] [PubMed] [Google Scholar]
- 22.Lindsey RW, Dick W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine. 1991;16:S140–S145. doi: 10.1097/00007632-199103001-00020. [DOI] [PubMed] [Google Scholar]
- 23.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 24.Muschler GF, Boehm C, Easley K. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg [Am] 1997;79:1699–1709. doi: 10.2106/00004623-199711000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Muschler GF, Nitto H, Matsukura Y, et al. Spine fusion using cell matrix composites enriched in bone marrow-derived cells. Clin Orthop Relat Res. 2003;407:102–118. doi: 10.1097/00003086-200302000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robertson PA, Wray AC. Natural history of posterior iliac crest bone graft donation for spinal surgery: a prospective analysis of morbidity. Spine. 2001;26:1473–1476. doi: 10.1097/00007632-200107010-00018. [DOI] [PubMed] [Google Scholar]
- 27.Sandhu HS, Khan SN, Suh DY, et al. Demineralized bone matrix, bone morphogenetic proteins, and animal models of spine fusion: an overview. Eur Spine J. 2001;10(Suppl 2):S122–S131. doi: 10.1007/s005860100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takagi K, Urist MR. The role of bone marrow in bone morphogenetic protein-induced repair of femoral massive diaphyseal defects. Clin Orthop Relat Res. 1982;171:224–231. [PubMed] [Google Scholar]
- 29.Tay BK, Le AX, Heilman M, et al. Use of a collagen-hydroxyapatite matrix in spinal fusion. A rabbit model. Spine. 1998;23:2276–2281. doi: 10.1097/00007632-199811010-00005. [DOI] [PubMed] [Google Scholar]
- 30.Thalgott JS, Fritts K, Giuffre JM, et al. Anterior interbody fusion of the cervical spine with coralline hydroxyapatite. Spine. 1999;24:1295–1299. doi: 10.1097/00007632-199907010-00005. [DOI] [PubMed] [Google Scholar]
- 31.Thalgott JS, Giuffre JM, Fritts K, et al. Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J. 2001;1:131–137. doi: 10.1016/S1529-9430(01)00011-0. [DOI] [PubMed] [Google Scholar]
- 32.Thalgott JS, Giuffre JM, Klezl Z, et al. Anterior lumbar interbody fusion with titanium mesh cages, coralline hydroxyapatite, and demineralized bone matrix as part of a circumferential fusion. Spine J. 2002a;2:63–69. doi: 10.1016/S1529-9430(01)00155-3. [DOI] [PubMed] [Google Scholar]
- 33.Thalgott JS, Klezl Z, Timlin M, et al. Anterior lumbar interbody fusion with processed sea coral (coralline hydroxyapatite) as part of a circumferential fusion. Spine. 2002b;27:E518–E527. doi: 10.1097/00007632-200212150-00011. [DOI] [PubMed] [Google Scholar]