Abstract
The authors report the successful outcome of a six-level corpectomy across the cervico-thoracic spine with circumferential reconstruction in a patient with extensive osteomyelitis of the cervical and upper thoracic spine. To the authors’ knowledge, this is the first report of a corpectomy extending across six levels of the cervico-thoracic spine. Clinical relevance: the authors recommend anterior cage and plate-assisted reconstruction and additional posterior instrumentation using modern spinal surgical techniques and implants.
Keywords: Corpectomy, Cervical spine, Fusion, Internal fixation, Reconstruction
Introduction
Multi (two or more)-level disease of the anterior cervical and upper thoracic spine can occur from degenerative, traumatic, infectious, and neoplastic causes. Successful treatment is dependent upon adequate decompression, immediate spinal reconstruction, and ultimately, the achievement of bony fusion. Decompression of the anterior cervical spinal canal can be achieved either by anterior cervical discectomy and fusion (ACDF) or anterior corpectomy and fusion (ACF). Across multiple levels, ACF offers several advantages over ACDF, including wider decompression and more complete removal of pathology causing spinal cord compression, and fewer graft-host interfaces that must consolidate for successful bony fusion. Corpectomies of the cervical and cervico-thoracic spine have been reported to extend across as many as four levels [5, 15, 16]. More extensive corpectomies have not been reported perhaps because of concerns for instrumentation failure and expected difficulty in obtaining adequate exposure of the anterior cervicothoracic spine.
We present a successful six-level cervicothoracic corpectomy and circumferential reconstruction in a patient with vertebral osteomyelitis and epidural abscess.
Case report
History and presentation
A 50-year-old HIV-positive woman with a history of alcohol and drug abuse presented to our institution with a 7-month history of progressive neck pain, dysphagia, and radiculomyelopathy. Her past medical history was also significant for hepatitis B and multiple episodes of alcohol-induced acute pancreatitis. She denied a history of opportunistic infections. She had not been compliant with anti-retroviral therapy.
Physical examination
On physical examination, the patient was unable to extend her neck above the horizon and demonstrated 4+ out of 5 motor strength throughout all muscle groups. Preoperative halo traction was not applied as the patient reported an intolerable amount of pain with any manipulation of her cervical spine.
Imaging studies
Plain radiographs and computed tomography (CT) imaging demonstrated extensive bony destruction and a marked kyphotic angulation of the cervicothoracic spine (Fig. 1). Magnetic resonance imaging revealed extensive prevertebral and epidural enhancement surrounding the cervical and upper thoracic spinal cord resulting in circumferential narrowing of the thecal sac (Fig. 2). These findings were consistent with the diagnosis of vertebral osteomyelitis/discitis and epidural abscess.
Fig. 1.
(Left) Swimmer’s view radiograph demonstrating kyphosis related to C4–T2 osteomyelitis. (Right) Sagittal reformatted CT scan demonstrating extensive osseous erosion with kyphotic angulation from C6–T2. Note that the apex of the kyphotic deformity is at the junction of the cervical and thoracic spine
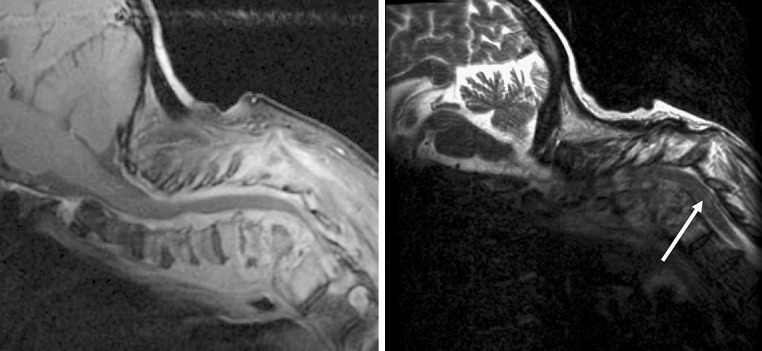
Fig. 2.
(Left) Sagittal T1 post-gadolinium MR sequence revealing extensive prevertebral and circumferential enhancing epidural abscess and enhancing vertebrae, compatible with osteomyelitis. (Right) Sagittal T2-weighted MR image demonstrating abnormal T2 signal within the spinal cord at the T1–2 level (arrow)
Operation
An anterior approach to the cervical spine was performed first. The patient was positioned supine with traction on a halo ring in extension to partially reduce the kyphotic deformity. Next, a longitudinal incision along the medial border of the right sternocleidomastoid muscle was made and connected to a median sternotomy which was performed for exposure of the T1–T3 vertebral bodies. Wide exposure of the C3–T3 vertebral bodies was then carried out. Leksell rongeurs were used to remove the C4, C5, C6, C7, T1 and T2 vertebral bodies down to the posterior longitudinal ligament. Next, an appropriately-sized lordotic titanium cage (Pyramesh; Medtronic Sofamor Danek, Memphis, TN, USA) was packed with iliac crest autograft and recombinant human bone morphogenic protein (rhBMP) and impacted into position. A slotted dynamic Aesculap ABC plate (Aesculap AG, Tutlingen, Germany, and Aesculap Instrument Corp., South San Francisco, CA, USA) was then affixed to the spine with variable-angle screws into the C3 and T3 bodies.
Next, the patient was turned prone and the halo head holder secured to a Mayfield frame. The posterior spine was dissected out from C1–T5 and Stealth image guidance (Medtronic Sofamor Danek, Memphis, TN, USA) was then used to place pedicle screws bilaterally at C2 and from T1–T4. Next, lateral mass screws were placed bilaterally at C3 and C4 and on the left side at C5. A laminectomy was performed from C4–T2. Tapered rods were then attached to the lateral mass and pedicle screws and secured bilaterally. Thorough decortication of the facet joints from C2–T4 was performed. Additional rhBMP and autograft was packed into the decorticated facets and lateral gutters. A lateral radiograph was obtained before closure to confirm satisfactory graft and hardware placement. After removal from the Mayfield frame, the halo brace and vest were then secured on the patient. Total blood loss was 2,000 cc and the total operating time was 8 h.
Postoperative course
Postoperative AP and lateral plain radiographs showed good hardware positioning with correction of the kyphotic deformity (Fig. 3). The patient was kept in the halo brace postoperatively. She began ambulating with physical therapy on postoperative day (POD) #3. She experienced improvement in her neurological symptoms during the hospitalization. Due to the extensive dissection of her anterior cervical spine, a feeding tube was placed in the immediate postoperative period and was removed on POD #15. She was discharged to home on POD #30 in good condition to complete a 6-week course of intravenous antibiotics for Staphylococcus aureus osteomyelitis.
Fig. 3.
Postoperative AP and lateral radiographs after six-level corpectomy from C4–T2, anterior interbody contoured cage and anterior plating from C3–T3. Posterior screw-rod fusion is evident from C2–T4. Note that the T1 pedicle screws have been shortened to avoid breeching into the cage anteriorly
Follow-up
At 4-month follow-up, the patient’s neurological exam was improved from presentation and she demonstrated full strength throughout all muscle groups, normal sensation and resolution of neck pain. She was able to ambulate without assistance and denied any problems with breathing or swallowing. Plain flexion-extension radiographs of the cervico-thoracic spine were obtained after the patient was removed from the Halo vest (Fig. 4). At last follow-up (2.5 years), the patient continued to remain neurologically intact without neck pain and no evidence of hardware failure.
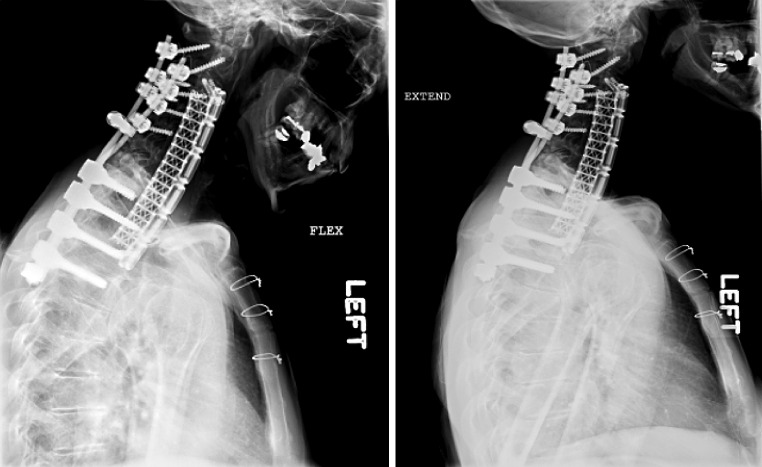
Fig. 4.
Flexion (left) and extension (right) plain radiographs obtained at 4-month follow-up demonstrate good hardware positioning without graft dislodgment. Note that the significant correction of sagittal plane alignment is maintained. There is no motion of the instrumented spinal levels
Discussion
Anterior corpectomy and fusion is perhaps the most effective procedure for wide spinal cord decompression in patients with severe canal stenosis or pathology of the anterior spine [16]. Compared to more conventional surgical techniques for spinal cord decompression, such as ACDF, laminectomy, and laminoplasty, patients treated with ACF have better neurological recovery, less axial neck pain, and lower incidences of postoperative loss of sagittal plane alignment [21, 24, 25]. Extensive ACF involving three or more levels; however, involves more complicated surgical exposure and has been associated with increased rates of graft-related complications, including graft dislodgment, spinal cord compression, and pseudoarthrosis [12, 19, 20, 22]. That the anterior graft is subject to significant compressive forces after extensive ACF has been confirmed in biomechanical studies [8, 23]. Although each surgeon must take into account the clinical indications, risks and benefits of ACF in every patient, it seems logical to assert that the reported experience with ACF has been limited to four or fewer levels out of concern for these potential complications. Reconstruction after extensive ACF, therefore, is critical to prevent graft failure and allow for successful bony fusion.
Anterior column reconstruction after extensive ACF may be performed using strut grafts or titanium mesh cages. Allo- or auto-graft struts may subside into the adjacent vertebral bodies or dislodge and cause cord compression [6, 12, 26]. Titanium mesh cages offer several advantages over strut grafts, including better correction of sagittal alignment (with pre-contoured cages), better endplate purchase, variable height and diameter options, and the ability to be packed with auto- or allograft bone [4, 7, 13]. Indeed, we were able to achieve significant correction of sagittal alignment in our patient with the use of a lordotic titanium cage. The addition of anterior plate fixation after interbody grafting enhances the rigidity and stability of the construct and therefore lowers the risk of graft-related complications [3, 5, 9, 16, 20]. Supplemental posterolateral fixation after extensive ACF has been found to further decrease the rates of graft-related complications, deformity correction loss, and pseudoarthrosis rates [8, 10, 16, 18, 20, 23]. Nevertheless, even with posterolateral fixation, in our experience there is inevitably a certain amount of subsidence of the anterior graft after extensive ACF. We used a slotted dynamic plate that allows for changes in the angle and alignment of the vertebral body screws to accommodate this expected subsidence (Fig. 4). Other options to prevent subsidence-related failure of the anterior plate include using a cage only (no plate), buttress plates, or creating flanges in the cage that overlap the adjacent vertebral bodies and are secured with non-constraining screws [1].
It is important to note; however, that we did not perform postoperative CT to demonstrate bridging trabecular bone and therefore cannot definitively conclude that successfully bony fusion occurred in our patient. Nevertheless, we believe the absence of hardware motion on flexion-extension plain radiographs at 4-month follow-up does demonstrate the stability of this patient’s extensive construct. Our patient has subsequently been lost to follow-up and it must be recognized that a pseudoarthrosis may manifest only after several years with a slowly progressive kyphosis.
Finally, both in vitro and in vivo studies have shown that BMP and rhBMP can promote bony fusion and arthrodesis [2, 11, 14, 17, 27]. While fusion-promoting agents such as rhBMP are expensive and their use in the cervicothoracic spine is ‘off-label, we believe it may improve the likelihood of fusion after the very extensive bone removal and instrumentation during this procedure and their use is therefore justified.
Conclusions
A six-level corpectomy across the cervico-thoracic spine can be safely performed by combining a traditional longitudinal exposure of the cervical spine with a median sternotomy. Circumferential reconstruction with modern implants, such as an anterior contoured titanium cage-dynamic plate construct and posterior screw-rod fixation, is necessary to provide sufficient stability of the cervico-thoracic spine to allow for correction of sagittal alignment and to achieve bony fusion. While the lack of a CT scan demonstrating bridging trabecular bone precludes a conclusion that radiographic fusion occurred in our patient, we believe that the absence of new or worsening clinical symptoms at 2.5-year follow-up demonstrates the long-term stability and potential for successful fusion of this reconstruction. Fusion-promoting agents may be used to increase the fusion rate of these kinds of constructs with substantial bone loss and use of extensive instrumentation systems.
References
- 1.Bilsky MH, Boakye M, Collignon F, Kraus D, Boland P. Operative management of metastatic and malignant primary subaxial cervical tumors. J Neurosurg Spine. 2005;2:256–264. doi: 10.3171/spi.2005.2.3.0256. [DOI] [PubMed] [Google Scholar]
- 2.Cheng H, Jiang W, Phillips FM, Haydon RC, Peng Y, Zhou L, Luu HH, An N, Breyer B, Vanichakarn P, Szatkowski JP, Park JY, He TC. Osteogenic activity of the fourteen types of human bone morphogenetic proteins (BMPs) J Bone Joint Surg Am. 2003;85:1544–1552. doi: 10.2106/00004623-200308000-00017. [DOI] [PubMed] [Google Scholar]
- 3.DiAngelo DJ, Foley KT, Vossel KA, Rampersaud YR, Jansen TH. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine. 2000;25:783–795. doi: 10.1097/00007632-200004010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Eck KR, Bridwell KH, Ungacta FF, Lapp MA, Lenke LG, Riew KD. Analysis of titanium mesh cages in adults with minimum two-year follow-up. Spine. 2000;25:2407–2415. doi: 10.1097/00007632-200009150-00023. [DOI] [PubMed] [Google Scholar]
- 5.Epstein NE. The value of anterior cervical plating in preventing vertebral fracture and graft extrusion after multilevel anterior cervical corpectomy with posterior wiring and fusion: indications, results, and complications. J Spinal Disord. 2000;13:9–15. doi: 10.1097/00002517-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Fernyhough JC, White JI, LaRocca H. Fusion rates in multilevel cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine. 1991;16:S561–S564. doi: 10.1097/00007632-199110001-00022. [DOI] [PubMed] [Google Scholar]
- 7.Hoshijima K, Nightingale RW, Yu JR, Richardson WJ, Harper KD, Yamamoto H, Myers BS. Strength and stability of posterior lumbar interbody fusion. Comparison of titanium fiber mesh implant and tricortical bone graft. Spine. 1997;22:1181–1188. doi: 10.1097/00007632-199706010-00002. [DOI] [PubMed] [Google Scholar]
- 8.Isomi T, Panjabi MM, Wang JL, Vaccaro AR, Garfin SR, Patel T. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine. 1999;24:2219–2223. doi: 10.1097/00007632-199911010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Kanayama M, Cunningham BW, Weis JC, Parker LM, Kaneda K, McAfee PC. The effects of rigid spinal instrumentation and solid bony fusion on spinal kinematics. A posterolateral spinal arthrodesis model. Spine. 1998;23:767–773. doi: 10.1097/00007632-199804010-00004. [DOI] [PubMed] [Google Scholar]
- 10.Kirkpatrick JS, Levy JA, Carillo J, Moeini SR (1999) Reconstruction after multilevel corpectomy in the cervical spine. A sagittal plane biomechanical study. Spine 24:1186–1190;discussion 91 [DOI] [PubMed]
- 11.Konishi S, Nakamura H, Seki M, Nagayama R, Yamano Y. Hydroxyapatite granule graft combined with recombinant human bone morphogenic protein-2 for solid lumbar fusion. J Spinal Disord Tech. 2002;15:237–244. doi: 10.1097/00024720-200206000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Macdonald RL, Fehlings MG, Tator CH, Lozano A, Fleming JR, Gentili F, Bernstein M, Wallace MC, Tasker RR. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990–997. doi: 10.3171/jns.1997.86.6.0990. [DOI] [PubMed] [Google Scholar]
- 13.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine. 1999;24:1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 14.Muschik M, Schlenzka D, Ritsila V, Tennstedt C, Lewandrowski KU. Experimental anterior spine fusion using bovine bone morphogenetic protein: a study in rabbits. J Orthop Sci. 2000;5:165–170. doi: 10.1007/s007760050144. [DOI] [PubMed] [Google Scholar]
- 15.Saunders RL, Pikus HJ, Ball P. Four-level cervical corpectomy. Spine. 1998;23:2455–2461. doi: 10.1097/00007632-199811150-00022. [DOI] [PubMed] [Google Scholar]
- 16.Sevki K, Mehmet T, Ufuk T, Azmi H, Mercan S, Erkal B. Results of surgical treatment for degenerative cervical myelopathy: anterior cervical corpectomy and stabilization. Spine. 2004;29:2493–2500. doi: 10.1097/01.brs.0000145412.93407.c3. [DOI] [PubMed] [Google Scholar]
- 17.Sidhu KS, Prochnow TD, Schmitt P, Fischgrund J, Weisbrode S, Herkowitz HN. Anterior cervical interbody fusion with rhBMP-2 and tantalum in a goat model. Spine J. 2001;1:331–340. doi: 10.1016/S1529-9430(01)00113-9. [DOI] [PubMed] [Google Scholar]
- 18.Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2003) Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine 28:2352–2358;discussion 58 [DOI] [PubMed]
- 19.Swank ML, Lowery GL, Bhat AL, McDonough RF. Anterior cervical allograft arthrodesis and instrumentation: multilevel interbody grafting or strut graft reconstruction. Eur Spine J. 1997;6:138–143. doi: 10.1007/BF01358747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410–415. [PubMed] [Google Scholar]
- 21.Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K (2001) Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine 26:1443–1447;discussion 48 [DOI] [PubMed]
- 22.Wang JC, Hart RA, Emery SE, Bohlman HH (2003) Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine 28:1016–1021;discussion 21–22 [DOI] [PubMed]
- 23.Wang JL, Panjabi MM, Isomi T. The role of bone graft force in stabilizing the multilevel anterior cervical spine plate system. Spine. 2000;25:1649–1654. doi: 10.1097/00007632-200007010-00008. [DOI] [PubMed] [Google Scholar]
- 24.Yonenobu K, Fuji T, Ono K, Okada K, Yamamoto T, Harada N. Choice of surgical treatment for multisegmental cervical spondylotic myelopathy. Spine. 1985;10:710–716. doi: 10.1097/00007632-198510000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Yonenobu K, Hosono N, Iwasaki M, Asano M, Ono K. Laminoplasty versus subtotal corpectomy. A comparative study of results in multisegmental cervical spondylotic myelopathy. Spine. 1992;17:1281–1284. doi: 10.1097/00007632-199211000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Zdeblick TA, Bohlman HH. Cervical kyphosis and myelopathy. Treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg Am. 1989;71:170–182. [PubMed] [Google Scholar]
- 27.Zhang H, Sucato DJ, Welch RD. Recombinant human bone morphogenic protein-2-enhanced anterior spine fusion without bone encroachment into the spinal canal: a histomorphometric study in a thoracoscopically instrumented porcine model. Spine. 2005;30:512–518. doi: 10.1097/01.brs.0000154651.62088.e3. [DOI] [PubMed] [Google Scholar]