Abstract
Renal malformations are common human birth defects that sometimes occur in the context of the caudal regression syndrome. Here, we found that exposure of pregnant mice to all-trans retinoic acid, at a time when the metanephros has yet to form, causes a failure of kidney development along with caudal regression. Maternal treatment with Am580 (retinoic acid receptor α agonist) also induced similar patterns of kidney maldevelopment in the fetus. In metanephroi from retinoic acid-treated pregnancies, renal mesenchyme condensed around the ureteric bud but then failed to differentiate into nephrons, instead undergoing involution by fulminant apoptosis to produce a renal agenesis phenotype. Results of whole organ cultures in serum-free medium, and also tissue recombination experiments, showed that the nephrogenic defect was intrinsic to the kidney and that it resided in the metanephric mesenchyme and not the ureteric bud. Renal mesenchyme from control embryos expressed Wilms’ tumor 1 (Wt1), but this transcription factor, which is indispensable for kidney development, failed to express in metanephroi of retinoic acid-exposed embryos. Wt1 expression and organogenesis were both restored, however, when metanephroi from retinoic acid-treated pregnancies were grown in serum-containing media. Our data illuminate the pathobiology of a severe, teratogen-induced kidney malformation.
Renal malformations are among one of the most common congenital malformations in humans and are the major cause of chronic renal failure in children.1 Renal agenesis represents the most severe phenotype, with bilateral agenesis occurring in ∼1 in 10,000 births, and unilateral agenesis occurs in ∼1 in 1000 individuals. Strictly speaking, agenesis implies that the metanephric kidney precursor has never formed; it is now recognized, however, that an agenesis-like phenotype can be the end-result of prenatal involution of malformed embryonic kidneys,2,3 a process probably driven by excessive apoptosis.4 Other types of malformation include renal hypoplasia (too few glomeruli and nephron tubules) and dysplasia (incomplete and metaplastic differentiation, often with cysts); in addition, the polycystic kidney diseases can be considered a failure of terminal epithelial differentiation and some types manifest antenatally.
There are three general causes of renal malformations:1 1) mutation in genes expressed during metanephric development such as the Wilms’ tumor 1 (Wt1)5 and Paired box 2 (PAX2)6 transcription factors; 2) impairment of fetal urinary flow caused by physical obstruction in lower urinary outflow tract;7,8 and 3) changes in the embryonic milieu associated with exposure to formal teratogens9 or more subtle factors, such as alterations in maternal diet.10 In many cases, the renal malformation is not an isolated anomaly, but occurs as part of a multiorgan congenital syndrome. For instance, renal agenesis and other renal malformations can occur in the context of the caudal regression syndrome,11–13 which is defined by a characteristic pattern of malformations including agenesis of the lower vertebral column, imperforate anus, and caudal spinal cord malformations that often appear as a terminal myelomeningocele.12,14–16 However, the reason for, and the mechanism of, this particular association are unclear.
There is emerging evidence that retinoids play an essential role in renal organogenesis. Vitamin A (retinol) is transferred to the embryo from the maternal circulation and then converted into its bioactive metabolite all-trans retinoic acid (RA). The RA signal is then transduced via nuclear RA receptors (RARs) that form heterodimers with retinoid x receptors (RXRs) to activate or suppress transcription of target genes. Rats made severely vitamin A-deficient delivered pups with renal malformations,17 which could be rescued by restoration with vitamin A during gestation.18 Renal agenesis occurs in RARαγ−/− mouse double mutants, whereas renal hypoplasia occurs in RARαβ2−/− and RXRα/RARα−/− embryos,19,20 showing that retinoid signal is involved in various developmental processes during kidney development. RARs have also been implicated in embryonic modeling of the lower urinary tract, including ureter and bladder trigone.21 Batourina and colleagues22 reported that RARs expressed in the stromal mesenchyme were involved in a reciprocal signaling loop with RET, a receptor for glial cell line-derived neurotrophic factor (GDNF). Ret is expressed in ureteric bud (UB) branch tips and is up-regulated by exposure of murine metanephric explants to vitamin A or RA; the same maneuvers enhance UB branching and nephron formation in a dose-dependent manner.22–24 It has also been found in the rat that the number of nephrons per kidney correlated positively with circulating vitamin A concentrations and that mild vitamin A deficiency leads to an inborn nephron deficit.25 Such experimental observations, which suggest that the vitamin A axis can modify nephron number, would have major clinical implications if applicable to humans because it is established that mild hypoplasia (ie, having approximately half the normal number of nephrons per kidney) is associated with arterial hypertension.26
Although vitamin A or RA deficiency will lead to a spectrum of malformations affecting a number of organ systems, such as the kidney, heart, eye, and nervous system,17,27–29 there is evidence for both humans and animal models that high vitamin A or RA intake is teratogenic for the same organ systems, including the kidney.30–33 Moreover, disturbing retinoid signaling either by homologous disruption of retinoid receptors19,20 or by maternal treatment with RAR selective agonists34 can induce renal malformations in the fetus. Taken together, these findings indicate that the level of retinoid signal is required to be tightly regulated for normal kidney development; when RA concentrations deviate from normal, in either direction, abnormal development occurs. Recently, our laboratory has demonstrated that pregnant mice treated with RA at mid-gestation gave birth to fetuses with a spectrum of malformations, including lower vertebral agenesis, imperforate anus, and terminal myelomeningocele,35 which closely resembled caudal regression syndrome in humans. In these experiments, it was also noted (A.S.W.S., personal observation) that renal malformations, including renal agenesis, were generated. In the current study, we have used the RA-induced caudal regression mouse model to study the cellular and molecular bases of severe renal malformations.
Materials and Methods
Animals
Guidelines for the use and care of laboratory animals, as set by The Chinese University of Hong Kong, were followed. Except for experiments to determine the dose response of Wt1 mutants to RA, all experiments were conducted using ICR (Institute of Cancer Research) mice housed at The Chinese University of Hong Kong under a light-dark cycle with the dark period from 1:00 a.m. to 11:00 a.m. Timed mating was performed by pairing mice for 2 hours immediately before commencement of the light cycle. Fertilization was assumed to occur at 10:00 a.m., which was regarded as embryonic day (E) 0. Wt1(+/−) mutant mice in C57/BL6 background were maintained at the MRC Human Genetics Unit. Fetuses were obtained from timed mating between Wt1(+/−) male and wild-type C57/BL6 female mice. In the Wt1 mutant allele, 10 bp in the Wt1 gene are replaced by the neomycin cassette.5 The genotype of the fetus was determined by amplification of DNA prepared from the liver using polymerase chain reaction (PCR), with primers that detected part of the neomycin cassette and part of Wt1.36
Dose and Time Response
To determine the stage specificity of the effect of RA on kidney development, a single dose of 100 mg/kg body weight of RA (Sigma, St. Louis, MO) suspended in peanut oil was injected intraperitoneally into pregnant ICR female mice at 4-hour intervals from 8 days 20 hours to 9 days 16 hours, whereas control mice received an equivalent volume of suspension vehicle. To determine a dose response, pregnant ICR female mice received a dose of 10, 50, 100, or 125 mg/kg body weight of RA or Am580 (RARα agonists)34,37 suspended in peanut oil, whereas pregnant C57/BL6 female mice received 50 mg/kg body weight of RA at 9 days 0 hours. To perform an initial assessment of effects on renal development, E18 fetuses were delivered by cesarean section and examined for anomalies. Kidney phenotypes were designated, using gross external morphology and paraffin sections (data not shown) as either: normal, agenesis (ie, no kidney tissue was found at E18), or nonagenesis renal malformation; the latter comprised a variety of phenotypes including hypoplasia (small kidneys containing normal-looking structures), dysplasia (kidneys containing poorly differentiated structures), or polycystic-like kidneys (differentiation appeared normal apart from cystic tubules). Injection of 125 mg/kg RA at 9 days 0 hours resulted in bilateral absence of kidneys in all fetuses, and hence this dosage and time point were used in all subsequent experiments to determine the cellular and molecular mechanisms of RA-induced renal agenesis.
Histology and Staining of Apoptotic Cells
Embryos at different developmental stages were fixed in Bouin’s solution and prepared as 7-μm-thick paraffin sections stained with hematoxylin and eosin (H&E) for histological examination of early kidney development. To identify the nature of cell death in the metanephros of the embryo at E11.00, embryos were fixed in 4% paraformaldehyde and prepared as 10-μm-thick paraffin sections cut transversely through the hindlimb bud region. Apoptotic cells with DNA breaks were stained by the terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) method, using fluorescein-conjugated avidin to detect the biotinylated dUTP-antibody complex according to Gavrieli and colleagues,38 with modifications as described in Shum and colleagues.35 DNA was counterstained using propidium iodide. At least five embryos were examined in each group.
In Situ Hybridization and Real-Time Quantitative Reverse Transcription-Polymerase Chain Reaction (RT-PCR)
The expression of Wt1,39 Pax2,40 Gdnf,41 and c-Ret42 in embryos at E11.00 was studied by whole mount in situ hybridization using digoxigenin-labeled probes according to Wilkinson.43 At least 12 embryos were examined in each group. Hybridized embryos were embedded in gelatin and cut into 50-μm-thick vibratome sections for detailed examination of spatial distribution patterns of these genes. To confirm whether Wt1 and Gdnf mRNA transcripts could be detected in metanephroi at E11.00 and E12.00, isolated metanephroi of embryos from the same litter were pooled together; total RNA was extracted using the RNeasy mini kit (Qiagen, Hilden, Germany) and reverse-transcribed into cDNA using SuperScript III reverse transcriptase (Invitrogen, Carlsbad, CA) according to the manufacturer’s instruction. The cDNA was then amplified by real-time quantitative PCR (40 cycles comprising of denaturation at 95°C for 15 seconds and annealing at 54°C for 1 minute) using SYBR Green PCR Master Mix (Applied Biosystems, Warrington, UK) and the following primers: Wt1 (forward: 5′-CAG ATG TAA TTC TAC AGG CGA TTG-3′; reverse: 5′-TCC CTA CAT ACT TGC AGA TTC AAA-3′), Gdnf (forward: 5′-CCT GAA GAT TAT CCT GAC CA-3′; reverse: 5′-CTT TCC CTC TGG AAT TCT CT-3′), and β-actin (forward: 5′-TGT TAC CCA CTG GGA CGA CA-3′; reverse: 5′-GGG GTG TTG AAG GTC TCA AA-3′) as internal control. The fluorescent-labeled PCR products were detected by ABI Prism 7000 sequence detection system (Applied Biosystems). The standard curve was prepared by using the threshold cycle (CT values) from dilutions of known concentrations of DNA obtained from respective cDNA plasmids. Three separate trials of PCR were performed for each sample. Each sample consisted of one litter of embryos. Three to four litters of embryos in each group were assessed.
Tissue Recombination and Co-Culture
Embryos were dissected out in L-15 medium (Life Technologies Inc., Carlsbad, CA) at E11.00, when the UB had just penetrated into the metanephric mesenchyme (MM) but not yet branched. The metanephros was isolated with the aid of a 25-gauge needle fitted into a 1-ml syringe. After enzymatic digestion with 0.05% trypsin (Sigma) and 0.01% pancreatin (Sigma) in Dulbecco’s modified Eagle’s medium/F12 medium (Life Technologies Inc.) at room temperature for 10 to 15 minutes, the MM and UB were mechanically separated with a pair of electrically sharpened tungsten needles. Different modes of tissue recombination, consisting of RA-treated and control tissues, were performed, with three pieces of MM from RA-exposed or control embryos placed in close proximity to one UB. The recombinants were cultured on the Millicell-CM 0.4-μm culture plate insert (Millipore, Bedford, MA) in a hormonally defined serum-free medium composed of Dulbecco’s modified Eagle’s medium/F12 medium supplemented with HEPES (15 mmol/L; Life Technologies Inc.), transferrin (5 μg/ml; Sigma), triiodothyronine (3.2 pg/ml; Sigma), prostaglandin E1 (25 ng/ml; Sigma), hydrocortisone (5 μg/ml; Sigma) and insulin (5 μg/ml; Sigma) at the air-medium interphase at 37°C in a 5% CO2 incubator. This medium could support normal metanephros differentiation.44 The recombinants were cultured for 7 days and the culture medium was refreshed every 48 hours. The first day of culture was designated day 0. In another set of experiments, three pieces of isolated control or RA-treated MM were placed in close proximity to a piece of spinal cord obtained from the cervical region of normal embryo at E11.00. The recombinants were cultured in the same conditions as described above. At least six recombinants were examined in each group.
Metanephric Explant Culture
To study the development of the metanephros in the absence of any influence from surrounding tissues, metanephroi were dissected out from control and RA-exposed embryos between E11.25 and E15.25 at 1-day intervals and cultured in the hormonally defined medium alone or supplemented with 10% or 20% fetal bovine serum (Life Technologies Inc.), under the same conditions as the recombinants, except the culture was terminated after 2 or 5 days. The explants were analyzed in either one of the following ways. To determine whether there was any mesenchymal differentiation, after 5 days in culture, the explant was fixed in Bouin’s fixative overnight and prepared as 7-μm-thick paraffin sections stained with H&E, and analyzed by light microscopy. To examine branching of the UB, after 5 days in culture, the explant was fixed in a mixture of methanol:acetone (1:1) for 20 minutes at −20°C. The ureteric epithelium was labeled by a mouse monoclonal antibody against calbindin-D (1:250, C-8666; Sigma), followed by detection using fluorescein-conjugated anti-mouse IgG secondary antibody (1:200; Jackson ImmunoResearch, West Grove, PA), and then examined by confocal microscopy. To measure the expression levels of Wt1 and β-actin (internal control) mRNA at 2 day after culture, real-time quantitative RT-PCR was performed as described above. Three separate trials of PCR were performed for each sample. Each sample consisted of 7 to 22 explants obtained in the same batch of culture. There were three to six samples in each group.
Statistical Analyses
The frequency and severity of renal malformations in response to RA or Am580 treatment at different dosages and time points were analyzed by Jonckheere-Terpstra test using StatXact 4 for Windows software (Cytel Software Corp., Cambridge, MA). The susceptibility of Wt1 mutant and wild-type embryos to RA-induced renal malformations was analyzed by Fisher’s exact test (two-sided) using StatXact4 for Windows software. The expression levels of Wt1 and Gdnf, relative to β-actin, between different treatment groups were analyzed by Student’s t-test using SPSS software (SPSS, Chicago, IL). The significance level was set at a P value of <0.05.
Results
RA Induced Renal Malformations within a Critical Developmental Window
We have previously found that the severity of caudal regression induced by RA, measured in terms of the body axial level being truncated, was highly developmental stage- and dose-dependent.35 To determine the stage when kidney development might be most sensitive to the teratogenic effect of RA, a time-response study was conducted. We found that treatment of pregnant mice with 100 mg/kg of RA between 8 days 20 hours and 9 days 12 hours, other than inducing caudal regression, also resulted in a spectrum of renal malformations in fetuses examined at E18 (Table 1). The frequency of malformations was dependent on the time of RA treatment, such that teratogen administration at earlier time points resulted in a significantly higher (P < 0.0001) percentage of embryos with renal malformations; moreover, later injections significantly (P < 0.0001) shifted the spectrum of renal anomalies from a lack of identifiable renal tissue, which we called the agenesis phenotype, toward the less severe malformations, such as hypoplastic, dysplastic, or polycystic-like kidneys, which we classified as nonagenesis renal malformations. Because injection at 8 days 20 hours led to high resorption rate, a somewhat more advanced stage (9 days 0 hours) with a lower resorption rate was chosen for a dose-response study. Results showed that increasing the dose of RA from 10 to 125 mg/kg, also significantly increased the frequency (P < 0.0001) and severity (P < 0.0001) of renal malformations in fetuses examined at E18 (Table 2).
Table 1.
Effect of Treatment with 100 mg/kg RA at Various Time Points on Kidney Development Assessed at E18
| Time of RA administration | 8 days, 20 hours | 9 days, 0 hours | 9 days, 4 hours | 9 days, 8 hours | 9 days, 12 hours | 9 days, 16 hours |
|---|---|---|---|---|---|---|
| Number of litters examined | 6 | 18 | 12 | 7 | 8 | 7 |
| Number of fetuses that underwent resorption | 12 | 17 | 8 | 2 | 4 | 3 |
| (% total fetuses) | (20) | (9) | (5) | (3) | (4) | (4) |
| Number of live fetuses | 47 | 172 | 147 | 77 | 100 | 76 |
| % Live fetuses with any renal malformation | 100 | 88 | 63 | 34 | 11 | 0 |
| % Live fetuses with bilateral renal agenesis | 92 | 66 | 32 | 8 | 0 | 0 |
| % Live fetuses with unilateral renal agenesis* | 8 | 16 | 0 | 4 | 0 | 0 |
| % Live fetuses with nonagenesis renal malformations† | 0 | 6 | 31 | 22 | 11 | 0 |
Contralateral kidney either normal or with nonagenesis renal malformations.
Bilateral or unilateral with contralateral kidney being normal.
Table 2.
Effect of Treatment with Various Dosages of RA at 9 Days 0 Hours on Kidney Development Assessed at E18
| Dosage of RA (mg/kg body weight) | 0 | 10 | 50 | 100 | 125 |
| Number of litters examined | 7 | 6 | 6 | 18 | 12 |
| Number of fetuses that underwent resorption | 1 | 6 | 8 | 17 | 11 |
| (% total fetuses) | (1) | (7) | (11) | (9) | (10) |
| Number of live fetuses | 82 | 85 | 66 | 172 | 102 |
| % Live fetuses with any renal malformation | 0 | 9 | 68 | 88 | 100 |
| % Live fetuses with bilateral renal agenesis | 0 | 0 | 20 | 66 | 100 |
| % Live fetuses with unilateral renal agenesis* | 0 | 0 | 21 | 16 | 0 |
| % Live fetuses with nonagenesis renal malformations† | 0 | 9 | 27 | 6 | 0 |
Contralateral kidney either normal or with nonagenesis renal malformations.
Bilateral or unilateral with contralateral kidney being normal.
To confirm whether induction of renal malformations was a specific teratogenic effect of RA, we tested if transactivation of RARs with selective agonists could similarly induce renal malformations. Because RARα is involved in retinoid signaling during kidney devel-opment,19,20 we treated pregnant mice with various dosages of Am580, a RARα agonist that could be rapidly transferred to the embryo,37,45 at 9 days 0 hours. Indeed, it was found that Am580 closely mimicking the effect of RA. Besides inducing caudal regression (data not shown), Am580 also induced agenesis and nonagenesis types of renal malformations, such that increasing the dose of Am580 from 10 to 125 mg/kg significantly increased the frequency (P < 0.0001) and severity (P < 0.0001) of renal malformations in fetuses examined at E18 (Table 3), although the teratogenic response was lower when compared with RA. This is probably because RA teratogenicity can be potentiated by heterodimerization of RARα with other RAR subtypes or RXRs.19,20,46 Because the results of our study showed that RA, when given to pregnant mice at the dose of 125 mg/kg at 9 days 0 hours could consistently induce bilateral renal agenesis in all fetuses, this dosage and injection time point were adopted for studying the pathogenic mechanisms of RA-induced failure of nephrogenesis.
Table 3.
Effect of Treatment with Various Dosages of Am580 at 9 Days 0 Hours on Kidney Development Assessed at E18
| Dosage of Am580 (mg/kg body weight) | 0 | 10 | 50 | 100 | 125 |
| Number of litters examined | 7 | 6 | 9 | 6 | 6 |
| Number of fetuses that underwent resorption | 1 | 8 | 11 | 10 | 12 |
| (% total fetuses) | (1) | (14) | (10) | (15) | (21) |
| Number of live fetuses | 82 | 51 | 99 | 56 | 45 |
| % Live fetuses with any renal malformation | 0 | 6 | 62 | 89 | 100 |
| % Live fetuses with bilateral renal agenesis | 0 | 0 | 0 | 18 | 47 |
| % Live fetuses with unilateral renal agenesis* | 0 | 0 | 7 | 16 | 24 |
| % Live fetuses with nonagenesis renal malformations† | 0 | 6 | 55 | 55 | 29 |
Contralateral kidney either normal or with nonagenesis renal malformations.
Bilateral or unilateral with contralateral kidney being normal.
Extensive Apoptosis in the RA-Treated Metanephric Mesenchyme
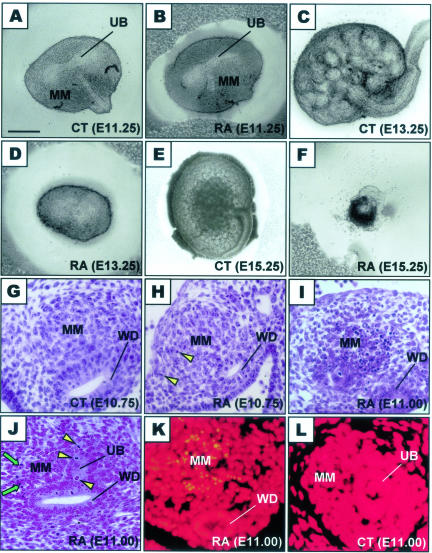
To determine whether the observed lack of renal tissue at E18 had resulted from complete failure of formation of the metanephros or degeneration of an existing organ, sets of control embryos, and those previously exposed to RA, were examined from E11.25 at 1-day intervals; typical appearances are described and shown from at least 25 embryos in each set. At E11.25, the metanephroi of RA-exposed embryos (Figure 1B) did not show any obvious morphological difference from the controls in which the mother was exposed to vehicle only (Figure 1A). In both, the UB had penetrated into the MM and formed the first T-shaped branches. However, thereafter, metanephroi from RA-exposed embryos halted in their development. The UB did not branch again, nor did the MM undergo nephrogenesis (Figure 1, compare C and D), by E15.25 they had regressed to a cluster of cells (Figure 1, compare E and F) and by E16.25, no renal tissue could be found. To determine whether there were any histological changes during early kidney development, serial sections of embryos were examined. Metanephric kidney development begins at E10.50, with condensation of mesenchymal cells adjacent to the caudal end of the Wolffian duct. The metanephric blastema enlarges as cells proliferate and it becomes more prominent by E10.75. Up to this stage, metanephroi from RA-exposed embryos (Figure 1H) looked similar histologically to time-matched controls (Figure 1G), eg, the size of the metanephric blastema was comparable and mitotic figures were evident. By E11.00, the UB had evaginated from the Wolffian duct and penetrated into the MM. It was at this stage that the metanephric rudiments from RA-exposed embryos showed the first histological abnormalities, with pyknotic nuclei being very prominent in the MM (Figure 1I). On the contrary, pyknotic nuclei were rare in the UB of these rudiments and mitoses were plentiful (Figure 1J). TUNEL staining confirmed that cell death in the RA-treated MM was mediated via fulminant apoptosis (Figure 1K); although the numbers of apoptotic nuclei were not formally quantified, programmed cell death was a rarer event in the normal metanephric kidney at the same stage (Figure 1L).
Figure 1.
Comparison of gross morphological and histological appearances of metanephroi from control and RA-exposed embryos. A to F: Metanephroi freshly isolated from control (CT; A, C, and E) and RA-exposed (RA; B, D, and F) embryos at E11.25 (A and B), E13.25 (C and D), and E15.25 (E and F). Note that RA-treated metanephroi (B) showed no apparent gross morphological difference from controls (A) at E11.25, with the UB having branched once and the MM yet to differentiate; in subsequent days, RA-treated metanephroi failed to progress (D) and then degenerated (F). G to L: Transverse histological metanephric sections of control (G and L) and RA-exposed embryos (H–K) at E10.75 (G and H) and E11.00 (I–L) stained by H&E (G–J) or TUNEL method (K and L). Note the condensation of cells around the Wolffian duct (WD) to form MM, which was actively proliferating with many mitotic figures (arrowhead, H) seen. The abundant pyknotic nuclei in the MM at the cranial region of the RA-treated metanephric rudiment (I) were apoptotic bodies (K). At the middle level of the RA-treated metanephric rudiment where the UB had evaginated from the WD and penetrated into the MM, there were many pyknotic nuclei (arrow) in the MM while UB cells were actively dividing (J). Scale bar: 0.2 mm (A–D, F); 0.5 mm (E); 0.05 mm (G–L).
Tissue Recombination Showed That the Primary Defect Resided in the RA-Treated Metanephric Mesenchyme
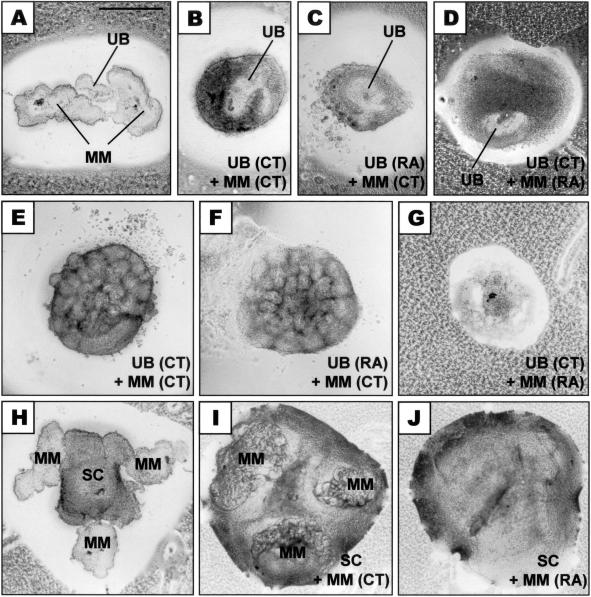
Kidney development is controlled by a series of reciprocal inductive interactions, in which the MM induces growth and repeated branching of the UB to give rise to the renal collecting system, whereas the tips of the branching UB induce the surrounding mesenchymal cells to condense into epithelial vesicles that differentiate into various segments of the nephron. In metanephroi from RA-exposed embryos, defective development was found in both the UB and MM lineages, ie, the bud failed to branch recurrently and the MM did not form nephrons. To address which compartment(s) might have a primary defect caused by the teratogen, tissue recombination experiments were performed such that UB and MM of RA-exposed embryos were separated from one another and then co-cultured in vitro with a normal (control) corresponding counterpart (Figure 2A). After 2 days in culture, the isolated control MM and UB from RA-exposed embryos had assembled into discrete structures that resembled early-stage metanephroi (Figure 2C), similar to that found in recombinants of control MM and control UB (Figure 2B). However, MM from RA-exposed embryos did not assemble with control UB but spread out (Figure 2D). After 7 days in culture, recombinants between control UB and control MM had undergone several rounds of UB branching with renal vesicles (nephron precursors) developing around branch tips (Figure 2E). Similar appearances were found in recombinants between the UB from RA-exposed embryos and control MM (Figure 2F), demonstrating first that the UB from teratogen-exposed embryos could respond to branching signals emanating from control MM and second that it was competent to induce nephrogenesis in control MM. On the contrary, when MM from RA-exposed embryos was recombined with control UB, the whole explant failed to differentiate and had degenerated after 1 week in culture (Figure 2G). Even when co-cultured with the 11-day embryonic cervical spinal cord (Figure 2H), an even more potent in vitro inducer of MM tubulogenesis than UB itself47 (Figure 2I), the MM from RA-exposed embryos still failed to differentiate and instead it regressed by 7 days of culture (Figure 2J). These findings supported the conclusion that the lack of UB branching and MM differentiation in the RA-treated metanephric kidney was due to a major defect in the MM. The MM could not respond to inducing signal from the UB to undergo differentiation, and neither was it competent to induce branching of the UB.
Figure 2.
Development of recombinants in culture. A–G: Co-culture of two pieces of MM with one piece of UB isolated from metanephroi of control (CT) or RA-exposed embryos (RA). Recombinants before (A), or after 2 days (B–D) or 7 days (E–G) in culture. Note that RA-treated UB when recombined with control MM (C and F) showed a similar pattern of growth and differentiation as recombinants between control UB and control MM (B and E). However, MM from embryos exposed to RA could not respond to control UB and degenerated (D and G). H–J: Co-culture of MM with embryonic spinal cord (SC). At the beginning of culture, three pieces of MM were placed in close proximity to one piece of SC (H). After 7 days in culture, while SC could induce tubulogenesis of control MM (I), MM from RA-exposed embryos could not respond to SC and degenerated (J). Scale bar, 0.5 mm.
Failure of Wt1 Expression in the RA-Treated Metanephric Mesenchyme
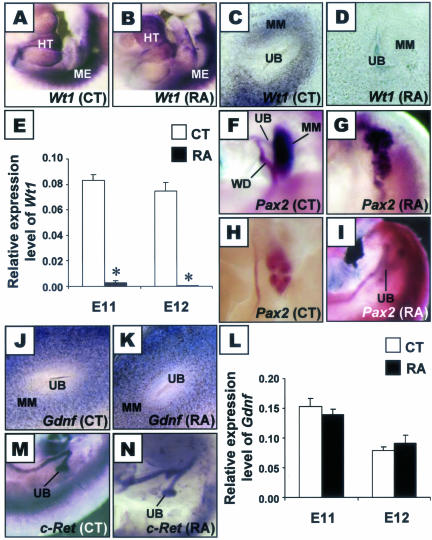
To understand the molecular changes in the RA-treated metanephros, we next investigated the expression of several regulatory genes that are critical for early kidney development.48 In particular, in mouse embryos with null mutation of Wt1, a transcription factor that begins to express at low levels in the uninduced MM at E11.00 and highly up-regulates as MM forms nephrogenic condensations,39 the MM fails to undergo any differentiation and instead involutes accompanied by fulminant MM apoptosis.5 This phenotype of the MM in Wt1-null mutant is in some aspects similar to that described in embryos of RA-treated pregnancies, although in the Wt1-null mutant, the UB did not penetrate into the MM.5 We performed in situ hybridization to investigate whether Wt1 expression in the MM was affected in embryos exposed to RA. When control and RA-exposed embryos at E11.00 were compared, there was no gross difference in the expression levels of Wt1 in the mesothelium of the heart and mesonephros (Figure 3, A and B), two other known sites where the gene is expressed.39 However, in the developing metanephros, while Wt1 was expressed in control MM (Figure 3C), no expression of Wt1 was detected, using the same methodology, in MM of embryos that has been exposed to RA (Figure 3D). When the more sensitive technique of real-time quantitative RT-PCR was used, only a very low and significantly reduced (P < 0.0001) level of Wt1 mRNA could be detected in the E11.00 metanephros from teratogen-exposed embryos, and Wt1 was barely detectable at the subsequent day (Figure 3E).
Figure 3.
Gene expression analysis. A–D, F–K, M, and N: In situ hybridization patterns of Wt1 (A–D), Pax2 (F–I), Gdnf (J and K), and c-Ret (M and N) in metanephroi from control (CT; A, C, F, H, J, and M) and RA-exposed embryos (RA; B, D, G, I, K, and N) at E11.00 (A–D, F, G, J, K, M, and N) or E12.00 (H and I). Whole mount view of embryos at the level of the developing heart (HT) and mesonephros (ME) (A and B), or at the level where the UB evaginated from the Wolffian duct (WD) and penetrated into the MM (F–I, M, and N). Some embryos were prepared as vibratome sections to examine the expression patterns in details (C, D, J, and K). E and L: Real-time quantitative RT-PCR analyses of gene expression levels of Wt1 (E) and Gdnf (L) relative to β-actin in metanephroi from control and RA-exposed embryos (*, P < 0.0001, CT versus RA at same stage; Student’s t-test).
It has been postulated that Wt1 and Pax2 act in a regulatory circuit in the developing kidney,49 hence the expression of Pax2 was determined. At E11.00, Pax2 expressed in the Wolffian duct and the UB in both the control (Figure 3F) and RA-exposed embryos (Figure 3G). However, although Pax2 was uniformly expressed throughout the control MM (Figure 3F), expression of Pax2 was patchy in MM from RA-exposed embryos (Figure 3G). As development proceeded, the expression of Pax2 was found in the condensing mesenchyme near tips of the UB in control embryos (Figure 3H), but Pax2 was no longer expressed in the MM of RA-exposed embryos, although it continued to express in the UB (Figure 3I). Next we assessed Gdnf which codes for a growth factor essential for the early inductive events of renal organogenesis.50 It was expressed in the MM of control and RA-exposed embryos at E11.00 in a similar pattern and intensity (Figure 3, J and K); measurement using real-time quantitative RT-PCR showed that there was no significant difference in the expression level of Gdnf between control and RA-exposed metanephroi (Figure 3L). Furthermore, in contrast to the failure in expression observed for Wt1, Gdnf continued to be expressed in E12.00 metanephroi of embryos exposed to RA (Figure 3L). c-Ret, the receptor of GDNF, was expressed in a similar pattern and intensity in the Wolffian duct and UB in control and RA-exposed embryos (Figure 3, M and N).
To further explore whether failure in Wt1 expression in MM might be implicated in the pathogenesis of the RA-induced failure of nephrogenesis, we next compared the susceptibility of Wt1 mutant embryos, with one nonfunctional allele, with wild-type embryos with regard to RA-induced renal malformations. Indeed, it was found that on maternal exposure of 50 mg/kg of RA at 9 days 0 hours, whereas 7 of 33 (21%) of Wt1(+/−) fetuses examined at E18 had renal malformations, only 2 of 36 (6%) of their wild-type littermates were affected (Table 4), thus embryos with loss of one functional Wt1 allele tended to have increased susceptibility to RA-induced renal malformations, although it had not yet reached a statistically significant level (P = 0.07); importantly, renal agenesis was observed only in the Wt1(+/−) genotype fetuses. It should be noted that: Wt1 heterozygous metanephroi have no gross renal defects, unlike the null mutant embryos,5 and the frequency of renal malformation generated in wild-type embryos in this experiment is somewhat lower than that found in ICR mice (see Table 2), perhaps because of the effects of (unknown) modifying polymorphisms present in the different strains. Collectively, the above data support that failure in Wt1 expression in the MM is directly involved in the pathogenic pathway of RA-induced renal malformation.
Table 4.
Comparison on Susceptibility of Wt1 Mutant and Wild-Type Embryos to RA-Induced Renal Malformations Assessed at E18
| Dosage of RA (mg/kg body weight) | 50 | |
| Number of litters examined | 8 | |
| Number of fetuses that underwent resorption | 0 | |
| Genotype | Wt1(+/+) | Wt1(+/−) |
| Number of live fetuses | 36 | 33 |
| % Live fetuses with any renal malformation | 6 | 21 |
| % Live fetuses with bilateral renal agenesis | 0 | 0 |
| % Live fetuses with unilateral renal agenesis* | 0 | 12 |
| % Live fetuses with nonagenesis renal malformations† | 6 | 9 |
Contralateral kidney either normal or with nonagenesis renal malformations.
Bilateral or unilateral with contralateral kidney being normal.
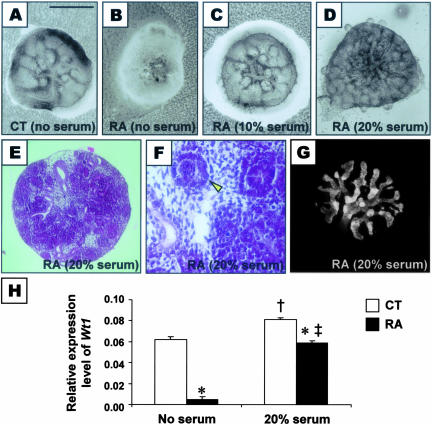
Autonomous Defect in the RA-Treated Metanephros Could Be Rescued
Although the tissue recombination and failure in Wt1 expression both suggested that a primary defect resided in the MM of RA-exposed embryos, it remained unclear whether the progressive failure of differentiation and involution was autonomous or due to the influence of surrounding tissues; in addition, we wanted to establish whether the failure of progression of nephrogenesis observed in vivo might be reversed or ameliorated. E11.25 metanephroi were isolated from control and RA-exposed embryos and cultured in vitro in a hormonally defined serum-free medium. Five days after culture, while the control metanephric explant had differentiated, with evidence of UB branching and early nephron formation by the MM (Figure 4A), the explants from embryos exposed to the teratogen did not grow but degenerated (Figure 4B), showing that the defect was autonomous. Nevertheless, when the culture medium was supplemented with fetal bovine serum, the metanephric explants from RA-exposed embryos were rescued from degeneration and began to differentiate (Figure 4, C and D). As assessed by histology of explants from RA-exposed embryos, the MM differentiated into condensates and primitive nephrons (Figure 4, E and F); calbindin immunostaining of whole mounts showed that the UB tree has undergone repeated branching in these explants (Figure 4G). As measured by real-time quantitative RT-PCR, after 2 days of culturing in serum-free media, Wt1 expressed at barely detectable levels in RA-exposed metanephric explants, which was significantly lower (P < 0.0001) than that of control explants (Figure 4H). However, with serum supplementation for 2 days, Wt1 expression levels were significantly increased (P < 0.005) not only in control metanephric explants, but were also significantly up-regulated (P < 0.0001) in RA-exposed explants (Figure 4H). However, serum treatment was only effective at rescuing metanephric explants isolated at E11.25 and E12.25, beyond which no ameliorating effect was noted (data not shown).
Figure 4.
Metanephric explants cultured in vitro for 5 days. A–D: Morphology of explanted metanephroi from control (CT) or RA-treated (RA) embryos cultured in serum-free medium (A and B), or medium supplemented with 10% (C) or 20% serum (D). E and F: Histological sections of RA-treated metanephric explants cultured in 20% serum showed that the rudiments had undergone differentiation, with formation of condensates, primitive tubules, and avascular glomeruli (arrowhead). G: Calbindin immunostaining of UB branch epithelium showed multiple branching in metanephric explants from RA-treated embryos after culture in 20% serum. H: Real-time quantitative RT-PCR analyses of expression levels of Wt1 relative to β-actin in metanephroi from control and RA-exposed embryos at 2 days after culture in serum-free medium or medium supplemented with 20% serum [*, P < 0.0001, CT versus RA in the same culture condition; †, P < 0.005, CT (no serum) versus CT (20% serum); ‡, P < 0.0001, RA (no serum) versus RA (20% serum); Student’s t-test]. Scale bar: 0.5 mm (A–D, G), 0.35 mm (E), 1.4 mm (F).
Discussion
In this study, we found that RA could induce renal malformations when administered in a critical developmental window before the appearance of the metanephric rudiments. The primary tissue affected was the MM, which could neither respond to inductive signals from the UB to undergo nephrogenesis nor could it stimulate UB branching. RA treatment was associated with a failure of Wt1 expression within the MM and the tissue underwent extensive apoptosis, with subsequent involution of the whole organ. What are the possible actions of RA that can lead to these defects in the MM?
RA is known to cause other congenital malformations by inducing death of progenitor cells. For example, it has been suggested that RA-induced facial dysmorphogenesis can be attributed to excessive death of mesenchymal cells in the mouse facial primordia.51 We have previously shown that the primitive streak/tail bud (PS/TB) at the caudal end of the embryo, which contains progenitor cells for forming the lower vertebrae and nervous tissue,52 was the direct target of RA-induced caudal regression.35 In a preliminary study, we found that the PS/TB of the embryo, taken from a stage when RA administration leads to renal malformations, could give rise to nephron tubule-like structures when transplanted into the nephrogenic zone of the neonatal kidney, which suggests that the PS/TB at that stage contains the progenitor cells of the metanephric kidney (A.S.W.S., unpublished data). These results, using transplantation into the nephrogenic kidney cortex,53 are consistent with previous observations by other investigators that mouse and chick PS/TB cells have the potential to form kidney structures after transplantation to ectopic sites.54,55 Putting these lines of evidence together, it is possible to speculate that excessive apoptosis in the tail bud simply kills off the kidney progenitor cells. Certainly, cell deletion within the PS/TB compartment may explain some of the loss of nonrenal tissues in the caudal regression phenotype; however, it is important to understand that RA treatment may also alter gene expressions and cell fates within the PS/TB, as noted for neural precursors.35 In fact, in the current teratogen-induced model of severe renal malformation, the metanephros does indeed begin to form but then fails to differentiate and then involutes. Therefore, the absence of kidneys found at E18 is not the result of a complete lack of nephrogenic precursor cells. Instead the RA-induced phenotype represents the untimely death of the just-formed embryonic kidney. In recent years, it has been noted that human dysplastic kidneys can completely regress,2,3 in association with an up-regulation of apoptotic cell death.4,56 In experimental genetic models of renal agenesis, a similar phenomenon has been documented; these include mice lacking the WT1 transcription factor5 and null mutants for FRAS1, a putative cell adhesion molecule that coats the interface of the MM and UB.57 Recently, it has been demonstrated that an up-regulation of apoptosis in the rat MM is associated with the generation of too few nephrons in the progeny of pregnant mothers exposed to low-protein diets,10 and enhanced programmed cell death is found in forming nephrons of fetal kidneys where the flow of fetal urine has been experimentally impaired.58 Thus, apoptosis is emerging as a contributing mechanism for kidney malformations associated with diverse genetic, physical, teratogenic, and dietary insults.
Apart from cell death, another mechanism by which RA can cause abnormal development is via altering gene expression that affects the identities of progenitor cells in a developing organ. For instance, RA altered Homeobox (Hox) codes of the mesodermal segments originally specified during gastrulation, which altered the migrating sclerotome cells before they were finally fixed in the cartilaginous vertebrae; this resulted in respecification of vertebral identities.59 Hox code is also important for specifying the metanephric blastema at the posterior end of the intermediate mesoderm.60 Although we have not assessed Hox gene expression within the kidney in the present study, we did not find any respecification of metanephric tissues, in that rudiments from RA-exposed embryos contained both MM and UB, as for normal metanephroi.
RA may also down-regulate master genes in the target tissue to disrupt development. For instance, we have shown that RA induced caudal regression via down-regulating Wnt-3a, a gene critical for tail bud development.35,61 In the current investigation, we elected to focus on the effects of RA on Wt1, which is regarded as a master gene in the early steps of nephrogenesis.5,39,62 We found that there was failure of induction and up-regulation of Wt1 expression specifically in the MM of RA-exposed embryos, whereas expression of Wt1 in other tissues, such as the mesothelium of the heart and the mesonephros was not affected. Our finding that embryos with heterozygous nonfunctional allele of Wt1 showed a tendency in increased susceptibility to RA-induced renal malformation supports the contention that a lack of Wt1 is important in the pathogenic pathway. There was a 2-day time lapse between the addition of exogenous RA at E9.00 and failure of induction of Wt1 expression at E11.00. It has been shown that a teratogenic dose of RA will be metabolized in the mouse embryo within 8 hours;63 therefore, exogenous RA almost certainly does not act directly to affect transcription of the Wt1 gene (or perhaps stability of Wt1 transcripts), but RA most probably affects a pathway that is required for induction and up-regulation of Wt1 expression in the MM. We concluded that the lack of Wt1 expression is autonomous. This was because, after the isolation of metanephroi from RA-exposed embryos, and cultured in a serum-free medium, the organs still proceeded to degenerate. On the other hand, control organs cultured in the same media underwent extensive MM and UB lineage differentiation. Wt1 has been implicated in enhancing the transcription of amphiregulin, a metanephric factor that enhances growth of this organ.64 Therefore, one can speculate that a lack of Wt1 would inhibit cell survival and differentiation by a lack of a critical growth factor produced by the metanephros. In this respect, it is of interest that we also found that the disappearance of rudiments from RA-exposed embryos could be halted in culture, and indeed their differentiation could be enhanced, by the addition of serum; the factor(s) responsible for this effect remains to be defined. It is established that the target sequences of Wt1 include promoters of a number of growth factors and their receptors that play a role in kidney development,65,66 and the Wilms’ tumor gene product WT1 can activate or suppress transcription through separate functional domains.67 The rescue effect of the serum was also associated with an up-regulation of Wt1 expression on prolonged organ culture. The effect is especially intriguing because, if such rescue could be performed in vivo, it suggests that malformed kidney may be driven toward a more normal fate by the use of extrinsic therapeutic agents such as growth factors.
It is also established that Wt1 interacts with and regulates Pax2,49 which plays multiple roles in kidney development. The PAX2 transcription factor is an activator of GDNF, which signals through the c-RET receptor, and is therefore essential for UB morphogenesis, including its initial branching from the Wolffian duct.50,68,69 In the current study, we found that Pax2, Gdnf, and c-Ret were expressed in the MM and UB in the just-formed metanephroi of embryos exposed to RA, and this is consistent with the successful penetration of the UB into the MM. These findings are also similar to observations made in Wt1-null mutant embryos that Gdnf expressed at equivalent levels as wild-type embryos, and Pax2 was initially expressed in the metanephric rudiment,70 but later became undetectable,5 suggesting that Wt1 may be required for the maintenance, but not the initial induction, of Pax2 transcription during early metanephric kidney development.
As previously discussed, it is intriguing that both deficiency and excess in RA can lead to the same types of malformations of the kidney. The specific expression of RARs71 and the development of renal malformations, including renal agenesis, in double-null mutants of RARs19 indicate that RA is essential for kidney development. The key enzyme for RA synthesis in the embryo is retinaldehyde dehydrogenase type 2, RALDH2, which begins to express in the MM during early stages of renal development.72 It has been shown that a teratogenic dose of RA resulted in down-regulation of Raldh2 in caudal regions of the embryo for more than a day.72 Hence, it is possible to speculate that administration of exogenous RA as in this study may lead to prolonged down-regulation of Raldh2, such that 2 days after the teratogenic insult, while the exogenous RA has been fully metabolized, endogenous RA synthesis, which is essential for early kidney development and perhaps the induction of Wt1, has not yet restored. Thus, it may lead to renal malformations, similar to cases of RA deficiency.
In conclusion, our data illuminate the pathobiology of a severe, teratogen-induced kidney malformation. This mouse model will serve as a valuable tool to unravel the upstream regulatory pathways for the induction and up-regulation of Wt1 transcription during early kidney development, which at the moment remains primarily unclear, but disturbance of which will lead to renal malformations.
Acknowledgments
We thank Prof. K. Shudo for the gift of Am580; Prof. F. Costantini, Prof. G. Dressler, and Prof. K. Kiuchi for the mouse cDNA plasmids of c-Ret, Pax2, and Gdnf, respectively; Dr. P. Hardman for technical advice on recombination cultures; and Mr. Y.K. Tse (Centre for Clinical Trials and Epidemiological Research, CUHK) for performing statistical data analysis.
Footnotes
Address reprint requests to Alisa S.W. Shum, Department of Anatomy, The Chinese University of Hong Kong, Shatin, N.T., Hong Kong. E-mail: alisa-shum@cuhk.edu.hk.
Substantially supported by the Research Grants Council of the Hong Kong Special Administrative Region (CUHK4283/99M to A.S.W.S. and A.S.W.). Other sources of funding include United Kingdom/Hong Kong Joint Research Scheme (JRS 98/23 to A.S.W.S. and N.D.H.); CUHK Mainline Research Scheme (MR95/010 to A.S.W.S., J.A.G., and A.S.W.); the Wellcome Trust (project grant 073624 to A.S.W. and M/95/3/96 to A.L.M.); the Kidney Research Aid Fund (to A.S.W.); and the CUHK (postgraduate studentships to H.K.W.T. and M.B.W.L.).
Present address of A.L.M.: Central Haematology Laboratory, University Medical Centre St. Radboud, P.O. Box 9101, 6500 HB Nijimegen, The Netherlands.
Present address of J.A.G.: Division of Human Anatomy, Stanford University School of Medicine, 269 Campus Dr., Stanford, CA 94305-5140.
References
- Woolf AS, Welham SJM, Hermann MM, Winyard PJD. Maldevelopment of the human kidney and lower urinary tract: an overview. Vize PD, Woolf AS, Bard JBL, editors. Amsterdam: Elsevier Science/Academic Press,; The KidneyFrom Normal Development to Congenital Disease. 2003:pp 377–393. [Google Scholar]
- Belk RA, Thomas DFM, Mueller RF, Godbole P, Markham AF, Weston MJ. A familial study and the natural history of prenatally detected unilateral multicystic dysplastic kidney. J Urol. 2002;167:666–669. doi: 10.1016/S0022-5347(01)69120-1. [DOI] [PubMed] [Google Scholar]
- Hiraoka M, Tsukahara H, Ohshima Y, Kasuga K, Ishihara Y, Mayumi M. Renal aplasia is the predominant cause of congenital solitary kidneys. Kidney Int. 2002;61:1840–1844. doi: 10.1046/j.1523-1755.2002.00322.x. [DOI] [PubMed] [Google Scholar]
- Winyard PJD, Nauta J, Lirenman DS, Hardman P, Sams VR, Risdon AR, Woolf AS. Deregulation of cell survival in cystic and dysplastic renal development. Kidney Int. 1996;49:135–146. doi: 10.1038/ki.1996.18. [DOI] [PubMed] [Google Scholar]
- Kreidberg JA, Sariola H, Loring JM, Maeda M, Pelletier J, Housman D, Jaenisch R. WT1 is required for early kidney development. Cell. 1993;74:679–691. doi: 10.1016/0092-8674(93)90515-r. [DOI] [PubMed] [Google Scholar]
- Porteous S, Torban E, Cho NP, Cunliffe H, Chua L, McNoe L, Ward T, Souza C, Gus P, Giugliani R, Sato T, Yun K, Favor J, Sicotte M, Goodyer P, Eccles M. Primary renal hypoplasia in humans and mice with PAX2 mutations: evidence of increased apoptosis in fetal kidneys of Pax2(1Neu)+/− mutant mice. Hum Mol Genet. 2000;9:1–11. doi: 10.1093/hmg/9.1.1. [DOI] [PubMed] [Google Scholar]
- Woolf AS, Thiruchelvam N. Congenital obstructive uropathy—its origin and contribution to end-stage renal failure in children. Adv Ren Replace Ther. 2001;8:157–163. doi: 10.1053/jarr.2001.26348. [DOI] [PubMed] [Google Scholar]
- Nyirady P, Thiruchelvam N, Fry CH, Godley ML, Winyard PJD, Peebles DM, Woolf AS, Cuckow PM. Effects of in utero bladder outflow obstruction on fetal sheep detrusor contractility, compliance and innervation. J Urol. 2002;168:1615–1620. doi: 10.1016/S0022-5347(05)64530-2. [DOI] [PubMed] [Google Scholar]
- Nathanson S, Moreau E, Merlet-Benichou C, Gilbert T. In utero and in vitro exposure to β-lactams impairs kidney development in the rat. J Am Soc Nephrol. 2000;11:874–884. doi: 10.1681/ASN.V115874. [DOI] [PubMed] [Google Scholar]
- Welham SJM, Wade A, Woolf AS. Protein restriction in pregnancy is associated with increased apoptosis of mesenchymal cells at the start of rat metanephrogenesis. Kidney Int. 2002;61:1231–1242. doi: 10.1046/j.1523-1755.2002.00264.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein MA, Bucy JG. Caudal regression syndrome: the urologic implications. J Urol. 1975;114:934–937. doi: 10.1016/s0022-5347(17)67178-7. [DOI] [PubMed] [Google Scholar]
- Andrish J, Kalamchi A, MacEwen GD. Sacral agenesis: a clinical evaluation of its management, heredity, and associated anomalies. Clin Orthop Relat Res. 1979;139:52–57. [PubMed] [Google Scholar]
- Sparnon AL, Ahmed S. Urological anomalies in the caudal regression syndrome. Aust N Z J Surg. 1984;54:365–367. doi: 10.1111/j.1445-2197.1984.tb05335.x. [DOI] [PubMed] [Google Scholar]
- Carson JA, Barnes PD, Tunell WP, Smith EI, Jolley SG. Imperforate anus: the neurological implication of sacral abnormalities. J Pediatr Surg. 1984;19:838–842. doi: 10.1016/s0022-3468(84)80380-2. [DOI] [PubMed] [Google Scholar]
- Bohring A, Lewin SO, Reynolds JF, Voigtländer T, Rittinger O, Carey JC, Köpernik M, Smith R, Zackai EH, Leonard NJ, Gritter HL, Bamforth JS, Okun N, McLeod DR, Super M, Powell P, Mundlos S, Hennekam RCM, van Langen IM, Viskochil DH, Wiedemann H-R, Opitz JM. Polytopic anomalies with agenesis of the lower vertebral column. Am J Med Genet. 1999;87:99–114. [PubMed] [Google Scholar]
- Pang D. Sacral agenesis and caudal spinal cord malformations. Neurosurgery. 1993;32:755–779. doi: 10.1227/00006123-199305000-00009. [DOI] [PubMed] [Google Scholar]
- Wilson JG, Warkany J. Malformations in the genito-urinary tract induced by maternal vitamin A deficiency in the rat. Am J Anat. 1948;83:357–407. doi: 10.1002/aja.1000830303. [DOI] [PubMed] [Google Scholar]
- Wilson JG, Roth CB, Warkany J. An analysis of the syndrome of malformations induced by maternal vitamin A deficiency. Effects of restoration of vitamin A at various times during gestation. Am J Anat. 1953;92:189–217. doi: 10.1002/aja.1000920202. [DOI] [PubMed] [Google Scholar]
- Mendelsohn C, Lohnes D, Décimo D, Lufkin T, LeMeur M, Chambon P, Mark M. Function of the retinoic acid receptors (RARs) during development (II). Multiple abnormalities at various stages of organogenesis in RAR double mutants. Development. 1994;120:2749–2771. doi: 10.1242/dev.120.10.2749. [DOI] [PubMed] [Google Scholar]
- Kastner P, Mark M, Ghyselinck N, Krezel W, Dupé V, Grondona JM, Chambon P. Genetic evidence that the retinoid signal is transduced by heterodimeric RXR/RAR functional units during mouse development. Development. 1997;124:313–326. doi: 10.1242/dev.124.2.313. [DOI] [PubMed] [Google Scholar]
- Batourina E, Choi C, Paragas N, Bello N, Hensle T, Costantini FD, Schuchardt A, Bacallao RJ, Mendelsohn CI. Distal ureter morphogenesis depends on epithelial cell remodelling mediated by vitamin A and Ret. Nat Genet. 2002;32:109–115. doi: 10.1038/ng952. [DOI] [PubMed] [Google Scholar]
- Batourina E, Gim S, Bello N, Shy M, Clagett-Dame M, Srinivas S, Costantini F, Mendelsohn C. Vitamin A controls epithelial/mesenchymal interactions through Ret expression. Nat Genet. 2001;27:74–78. doi: 10.1038/83792. [DOI] [PubMed] [Google Scholar]
- Vilar J, Gilbert T, Moreau E, Merlet-Bénichou A. Metanephros organogenesis is highly stimulated by vitamin A derivatives in organ culture. Kidney Int. 1996;49:1478–1487. doi: 10.1038/ki.1996.208. [DOI] [PubMed] [Google Scholar]
- Moreau E, Vilar J, Lelièvre-Pégorier M, Merlet-Bénichou C, Gilbert T. Regulation of c-ret expression by retinoic acid in rat metanephros: implications in nephron mass control. Am J Physiol. 1998;275:F938–F945. doi: 10.1152/ajprenal.1998.275.6.F938. [DOI] [PubMed] [Google Scholar]
- Lelièvre-Pégorier M, Vilar J, Ferrier M-L, Moreau E, Freund N, Gilbert T, Merlet-Bénichou C. Mild vitamin A deficiency leads to inborn nephron deficit in the rat. Kidney Int. 1998;54:1455–1462. doi: 10.1046/j.1523-1755.1998.00151.x. [DOI] [PubMed] [Google Scholar]
- Keller G, Zimmer G, Mall G, Ritz E, Amann K. Nephron number in patients with primary hypertension. N Engl J Med. 2003;348:101–108. doi: 10.1056/NEJMoa020549. [DOI] [PubMed] [Google Scholar]
- Warkany J, Roth C. Congenital malformations induced in rats by maternal vitamin A deficiency. II. Effect of varying the preparatory diet upon the yield of abnormal young. J Nutrition. 1948;35:1–12. [Google Scholar]
- Dickman EC, Thaller C, Smith SM. Temporally-regulated retinoic acid depletion produces specific neural crest, ocular and nervous system defects. Development. 1997;124:3111–3121. doi: 10.1242/dev.124.16.3111. [DOI] [PubMed] [Google Scholar]
- White JC, Highland M, Clagett-Dame M. Abnormal development of the sinuatrial venous valve and posterior hindbrain may contribute to late fetal resorption of vitamin A-deficient rat embryos. Teratology. 2000;62:374–384. doi: 10.1002/1096-9926(200012)62:6<374::AID-TERA4>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Robens JF. Teratogenic effects of hypervitaminosis A in the hamster and the guinea pig. Toxicol Appl Pharmacol. 1970;16:88–99. doi: 10.1016/0041-008x(70)90165-1. [DOI] [PubMed] [Google Scholar]
- Shenefelt RE. Morphogenesis of malformations in hamsters caused by retinoic acid: relation to dose and stage at treatment. Teratology. 1972;5:103–118. doi: 10.1002/tera.1420050115. [DOI] [PubMed] [Google Scholar]
- Bernhardt IB, Dorsey DJ. Hypervitaminosis A and congenital renal anomalies in a human infant. Obstet Gynecol. 1974;43:750–755. [PubMed] [Google Scholar]
- Rothman KJ, Moore LL, Singer MR, Nguyen US, Mannino S, Milunsky A. Teratogenicity of high vitamin A intake. N Engl J Med. 1995;333:1369–1373. doi: 10.1056/NEJM199511233332101. [DOI] [PubMed] [Google Scholar]
- Elmazar MMA, Reichert U, Shroot B, Nau H. Pattern of retinoid-induced teratogenic effects: possible relationship with relative selectivity for nuclear retinoid receptors RARα, RARβ, and RARγ. Teratology. 1996;53:158–167. doi: 10.1002/(SICI)1096-9926(199603)53:3<158::AID-TERA3>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Shum ASW, Poon LLM, Tang WWT, Koide T, Chan BWH, Leung YC, Shiroishi T, Copp AJ. Retinoic acid induces down-regulation of Wnt-3a, apoptosis and diversion of tail bud cells to a neural fate in the mouse embryo. Mech Dev. 1999;84:17–30. doi: 10.1016/s0925-4773(99)00059-3. [DOI] [PubMed] [Google Scholar]
- Menke AL, Ijpenberg A, Fleming S, Ross A, Medine CN, Patek CE, Spraggon L, Hughes J, Clarke AR, Hastie ND. The wt1-heterozygous mouse; a model to study the development of glomerular sclerosis. J Pathol. 2003;200:667–674. doi: 10.1002/path.1390. [DOI] [PubMed] [Google Scholar]
- Delescluse C, Cavey MT, Martin B, Bernard BA, Reichert U, Maignan J, Darmon M, Shroot B. Selective high affinity retinoic acid receptor α or β-γ ligands. Mol Pharmacol. 1991;40:556–562. [PubMed] [Google Scholar]
- Gavrieli Y, Sherman Y, Ben-Sasson SA. TdT mediated dUTP-biotin nick end labeling of tissue sections (TUNEL). J Cell Biol. 1992;119:493–501. doi: 10.1083/jcb.119.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong JF, Pritchard-Jones K, Bickmore WA, Hastie HD, Bard JBL. The expression of the Wilms’ tumor gene, WT1, in the developing mammalian embryo. Mech Dev. 1992;40:85–97. doi: 10.1016/0925-4773(93)90090-k. [DOI] [PubMed] [Google Scholar]
- Dressler GR, Deutsch U, Chowdhury K, Nornes HO, Gruss P. Pax2, a new murine paired-box-containing gene and its expression in the developing excretory system. Development. 1990;109:787–795. doi: 10.1242/dev.109.4.787. [DOI] [PubMed] [Google Scholar]
- Matsushita N, Fujita Y, Tanaka M, Nagatsu T, Kiuchi K. Cloning and structural organization of the gene encoding the mouse glial cell-line-derived neurotrophic factor, GDNF. Gene. 1997;203:149–157. doi: 10.1016/s0378-1119(97)00506-4. [DOI] [PubMed] [Google Scholar]
- Pachnis V, Mankoo B, Costantini F. Expression of the c-ret proto-oncogene during mouse embryogenesis. Development. 1993;119:1005–1017. doi: 10.1242/dev.119.4.1005. [DOI] [PubMed] [Google Scholar]
- Wilkinson DG. Whole mount in situ hybridisation of vertebrate embryos. Wilkinson DG, editor. Oxford: IRL Press,; In Situ Hybridisation. 1992:pp 75–83. [Google Scholar]
- Avner ED, Ellis D, Temple T, Jaffe R. Metanephric development in serum-free organ culture. In Vitro. 1982;18:675–682. doi: 10.1007/BF02796422. [DOI] [PubMed] [Google Scholar]
- Arafa HMM, Elmazar MMA, Hamada FMA, Reichert U, Shroot B, Nau H. Selective agonists of retinoic acid receptors: comparative toxicokinetics and embryonic exposure. Arch Toxicol. 2000;73:547–556. doi: 10.1007/s002040050007. [DOI] [PubMed] [Google Scholar]
- Elmazar MMA, Rühl R, Reichert U, Shroot B, Nau H. RARα-mediated teratogenicity in mice is potentiated by an RXR agonist and reduced by an RAR antagonist: dissection of retinoid receptor-induced pathways. Toxicol Appl Pharmacol. 1997;146:21–28. doi: 10.1006/taap.1997.8221. [DOI] [PubMed] [Google Scholar]
- Grobstein C. Inductive interaction in the development of the mouse metanephros. J Exp Zool. 1955;130:319–340. [Google Scholar]
- Carroll TJ, McMahon AP. Overview: the molecular basis of kidney development. Vize PD, Woolf AS, Bard JBL, editors. Amsterdam: Elsevier Science/Academic Press,; The KidneyFrom Normal Development to Congenital Disease. 2003:pp 343–376. [Google Scholar]
- Discenza MT, He S, Lee TH, Chu LL, Bolon B, Goodyer P, Eccles M, Pelletier J. WT1 is a modifier of the Pax2 mutant phenotype: cooperation and interaction between WT1 and Pax2. Oncogene. 2003;22:8145–8155. doi: 10.1038/sj.onc.1206997. [DOI] [PubMed] [Google Scholar]
- Sainio K, Suvanto P, Davies J, Wartiovaara J, Wartiovaara K, Saarma M, Arumäe U, Meng X, Lindahl M, Pachnis V, Sariola H. Glial-cell-line-derived neurotrophic factor is required for bud initiation from ureteric epithelium. Development. 1997;124:4077–4087. doi: 10.1242/dev.124.20.4077. [DOI] [PubMed] [Google Scholar]
- Osumi-Yamashita N, Iseki S, Noji S, Nohno T, Koyama E, Taniguchi S, Doi H, Eto K. Retinoic acid treatment induces the ectopic expression of retinoic acid receptor β gene and excessive cell death in the embryonic mouse face. Dev Growth Differ. 1992;34:199–209. doi: 10.1111/j.1440-169X.1992.tb00009.x. [DOI] [PubMed] [Google Scholar]
- Griffith CM, Wiley MJ, Sanders EJ. The vertebrate tail bud: three germ layers from one tissue. Anat Embryol. 1992;185:101–113. doi: 10.1007/BF00185911. [DOI] [PubMed] [Google Scholar]
- Woolf AS, Palmer SJ, Snow ML, Fine LG. Creation of a functioning chimeric mammalian kidney. Kidney Int. 1990;38:991–997. doi: 10.1038/ki.1990.303. [DOI] [PubMed] [Google Scholar]
- Tam PPL. The histogenetic capacity of tissues in the caudal end of the embryonic axis of the mouse. J Embryol Exp Morph. 1984;82:253–266. [PubMed] [Google Scholar]
- Griffith CM, Wiley MJ. Direct effects of retinoic acid on the development of the tail bud in chick embryos. Teratology. 1989;39:261–275. doi: 10.1002/tera.1420390308. [DOI] [PubMed] [Google Scholar]
- Granata C, Wang Y, Puri P, Tanaka K, O’Briain DS. Decreased bcl-2 expression in segmental renal dysplasia suggests a role in its morphogenesis. Br J Urol. 1997;80:140–144. doi: 10.1046/j.1464-410x.1997.00235.x. [DOI] [PubMed] [Google Scholar]
- McGregor L, Makela V, Darling SM, Vrontou S, Chalepakis G, Roberts C, Smart N, Rutland P, Prescott N, Hopkins J, Bentley E, Shaw A, Roberts E, Mueller R, Jadeja S, Philip N, Nelson J, Francannet C, Perez-Aytes A, Megarbane A, Kerr B, Wainwright B, Woolf AS, Winter RM, Scambler PJ. Fraser syndrome and mouse blebbed phenotype caused by mutations in FRAS1/Fras1 encoding a putative extracellular matrix protein. Nat Genet. 2003;34:203–208. doi: 10.1038/ng1142. [DOI] [PubMed] [Google Scholar]
- Attar R, Quinn F, Winyard PJD, Mouriquand PDE, Foxall P, Hanson MA, Woolf AS. Short-term urinary flow impairment deregulates PAX2 and PCNA expression and cell survival in fetal sheep kidneys. Am J Pathol. 1998;152:1225–1235. [PMC free article] [PubMed] [Google Scholar]
- Kessel M. Respecification of vertebral identities by retinoic acid. Development. 1992;115:487–501. doi: 10.1242/dev.115.2.487. [DOI] [PubMed] [Google Scholar]
- Davies AP, Witte DP, Hsieh-Li HM, Potter SS, Capecchi MR. Absence of radius and ulna in mice lacking hoax-11 and. hoxd-11. Nature. 1995;375:791–795. doi: 10.1038/375791a0. [DOI] [PubMed] [Google Scholar]
- Takada S, Stark KL, Shea MJ, Vassileva G, McMahon JA, MacMahon AP. Wnt-3a regulates somite and tailbud formation in the mouse embryo. Genes Dev. 1994;8:174–189. doi: 10.1101/gad.8.2.174. [DOI] [PubMed] [Google Scholar]
- Davies JA, Ladomery M, Hohenstein P, Michael L, Shafe A, Spraggon L, Hastie N. Development of an siRNA-based method for repressing specific genes in renal organ culture and its use to show that the Wt1 tumor suppressor is required for nephron differentiation. Hum Mol Genet. 2004;13:235–246. doi: 10.1093/hmg/ddh015. [DOI] [PubMed] [Google Scholar]
- Satre MA, Kochhar DM. Elevations in the endogenous levels of the putative morphogen retinoic acid in embryonic mouse limb-buds associated with limb dysmorphogenesis. Dev Biol. 1989;133:529–536. doi: 10.1016/0012-1606(89)90055-9. [DOI] [PubMed] [Google Scholar]
- Lee SB, Huang K, Palmer R, Truong VB, Herzlinger D, Kolquist KA, Wong J, Paulding C, Yoon SK, Gerald W, Oliner JD, Haber DA. The Wilms tumor suppressor WT1 encodes a transcriptional activator of amphiregulin. Cell. 1999;98:663–673. doi: 10.1016/s0092-8674(00)80053-7. [DOI] [PubMed] [Google Scholar]
- Little M, Holmes G, Walsh P. WT1: what has the last decade told us? BioEssays. 1999;21:191–202. doi: 10.1002/(SICI)1521-1878(199903)21:3<191::AID-BIES3>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Scharnhorst V, van der Eb AJ, Jochemsen AG. WT1 proteins: functions in growth and differentiation. Gene. 2001;273:141–161. doi: 10.1016/s0378-1119(01)00593-5. [DOI] [PubMed] [Google Scholar]
- Wang Z-Y, Qiu Q-Q, Deuel TF. The Wilms’ tumor gene product WT1 activates or suppresses transcription through separate functional domains. J Biol Chem. 1993;268:9172–9175. [PubMed] [Google Scholar]
- Srinivas S, Wu Z, Chen C-M, D’Agati V, Costantini F. Dominant effects of RET receptor misexpression and ligand-independent RET signalling on ureteric bud development. Development. 1999;126:1375–1386. doi: 10.1242/dev.126.7.1375. [DOI] [PubMed] [Google Scholar]
- Brophy PD, Ostrom L, Lang KM, Dressler GR. Regulation of ureteric bud outgrowth by Pax-2 dependent activation of the glial derived neurotrophic factor gene. Development. 2001;128:4747–4756. doi: 10.1242/dev.128.23.4747. [DOI] [PubMed] [Google Scholar]
- Donovan MJ, Natoli TA, Sainio K, Amstutz A, Jaenisch R, Sariola H, Kreidberg JA. Initial differentiation of the metanephric mesenchyme is independent of WT1 and the ureteric bud. Dev Genet. 1999;24:252–262. doi: 10.1002/(SICI)1520-6408(1999)24:3/4<252::AID-DVG8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Dollé P, Ruberte E, Leroy P, Morriss-Kay G, Chambon P. Retinoic acid receptors and cellular retinoid binding proteins. I. A systematic study of their differential pattern of transcription during mouse organogenesis. Development. 1990;110:1133–1151. doi: 10.1242/dev.110.4.1133. [DOI] [PubMed] [Google Scholar]
- Niederreither K, McCaffery P, Dräger UC, Chambon P, Dollé P. Restricted expression and retinoic acid-induced downregulation of the retinaldehyde dehydrogenase type 2 (RALDH-2) gene during mouse development. Mech Dev. 1997;62:67–78. doi: 10.1016/s0925-4773(96)00653-3. [DOI] [PubMed] [Google Scholar]