Abstract
In UM-X7.1 hamster model of human dilated cardiomyopathy, heart failure progressively develops and causes 50% mortality by 30 weeks of age. Through ultrastructural analysis, we found that many cardiomyocytes of this model contain typical autophagic vacuoles including degraded mitochondria, glycogen granules, and myelin-like figures. In addition, ubiquitin, cathepsin D, and Rab7 were overexpressed as determined by immunoassays. Importantly, most cardiomyocytes with leaky plasma membranes were positive for cathepsin D, suggesting a direct link between autophagic degeneration and cell death. Meanwhile, cardiomyocyte apoptosis appeared insignificant. Granulocyte colony-stimulating factor (10 μg/kg/day), injected 5 days/week from 15 to 30 weeks of age, improved survival among 30-week-old hamsters (100% versus 53% in the untreated hamsters, P < 0.0001); ventricular function and remodeling, increased cardiomyocyte size, and reduced myocardial fibrosis followed by a dramatic reduction in the autophagic findings were also seen. Granulocyte colony-stimulating factor also down-regulated tumor necrosis factor-α and increased activities of Akt signal transducer and activator of transcription-3, and matrix metalloproteinases. However, there was no clear evidence of transdifferentiation from bone marrow cells into cardiomyocytes. In conclusion, autophagic death is important for cardiomyocyte loss in the cardiomyopathic hamster, and the beneficial effect of granulocyte colony-stimulating factor acts mainly via an anti-autophagic mechanism rather than anti-apoptosis or regeneration.
Autophagy was originally defined as the process of sequestration of intracellular components and their subsequent degradation by lysosomal vacuoles.1 Although autophagy is ongoing as a normal process, abnormal autophagy can cause various neuromuscular degenerative diseases such as Alzheimer’s disease, Parkinson’s disease, and distal type myopathy.1 In a specific type of cardiomyopathy (Danon disease), cardiomyocytes include marked autophagic vacuoles in the cytoplasm,2 where dysfunction of the autophagic process is suggested by deficiency of the lysosomal protein Lamp-2.3,4 Dilated cardiomyopathy (DCM) is a major cause of morbidity and mortality among congestive heart failure (CHF) patients and is associated with a continuous loss of cardiomyocytes.5 At present, the mechanism of cardiomyocyte death in DCM is controversial, with apoptosis proposed by some researchers6–8 but no apoptosis by others, including us.9–11 Recent studies reported autophagic vacuoles in myocytes of heart diseases with failure such as DCM and aortic stenosis of the terminal stage,11–14 but the pathophysiological significance in those diseases is still undetermined. Importantly, a basic issue such as the linkage between autophagic degeneration and cell death has not been evidenced in cardiomyocytes of failing hearts.
The UM-X7.1 hamster is an animal model of autosomal recessive cardiomyopathy and muscular dystrophy that is caused by lack of the δ-sarcoglycan gene and that develops a progressive cardiomyocyte death.15,16 The condition begins at ∼4 weeks of age and then worsens throughout subsequent weeks. Cardiac hypertrophy is seen by the time the animals are ∼20 weeks of age and is followed by progressive ventricular remodeling and fibrosis with CHF. Approximately half of these animals die by the time they are 30 weeks old. Notably, one family and two sporadic cases of human DCM were recently identified in which the patients presented with mutations in the δ-sarcoglycan gene.17
It is widely accepted that granulocyte colony-stimulating factor (G-CSF), a regeneration- and/or repair-related cytokine, can alleviate postmyocardial infarction cardiac dysfunction and remodeling.18–22 Recently, we reported that postinfarction treatment with G-CSF accelerated the healing process of myocardial infarction through augmenting macrophage accumulation in the infarcted area, up-regulating the matrix metalloproteinase (MMP) family, and inducing transdifferentiation of bone marrow cells into cardiomyocytes, although the incidence of transdifferentiation was small.21 However, it is unknown whether the G-CSF treatment is effective against cardiac dysfunction due to nonischemic origin. Therefore, the aims of the present study were to define the mode of death of cardiomyocytes in UM-X7.1 hamster and to examine whether G-CSF exerts beneficial effects on the nonischemic failing hearts.
Materials and Methods
Animals
Male UM-X7.1 hamsters were provided by Drs. T. Ohkusa and M. Matsuzaki of Yamaguchi University School of Medicine, Ube, Japan. Male golden hamsters were chosen as the control without heart disease (Clea Japan, Shizuoka, Japan). The animals were housed in an air-conditioned room with an automatic 12:12 hours day-night cycle and maintained on a normal laboratory diet with free access to tap water. All animals received humane care in accordance with the Guide for the Care and Use of Laboratory Animals (NIH publication no. 8523, revised 1985).
Experimental Protocols
Protocol I: Examination of Autophagy
Male UM-X7.1 hamsters and the sex-matched golden hamster controls were sacrificed at the age of 30 weeks (n = 8 each).
Protocol II: Effect of G-CSF on Hamsters
Recombinant human G-CSF (Chugai Pharmaceutical Co., Tokyo, Japan) was administered at a dosage of 10 μg/kg/day to 16 male UM-X7.1 hamsters by subcutaneous injection on the first 5 days of each week. The injections were begun when the animals reached 15 weeks of age and were continued for 15 weeks, until the animals were 30 weeks of age. In the untreated group of UM-X7.1 hamsters, the same volume of distilled water (∼50 μl per animal) was given to 15 age- and sex-matched hamsters throughout the same period. Age- and sex-matched golden hamsters were similarly treated with G-CSF (n = 8) or with distilled water (n = 6).
In another set of experiments, we examined the possibility of bone marrow-derived myocardial regeneration. Bone marrow cells were aspirated from the femoral bones of 12 UM-X7.1 hamsters at the age of 15 weeks and labeled by incubation for 30 minutes at 37°C with fluorescent carbocyanine 1,1′-dioctadecyl-1-3,3,3′,3′-tetramethyllindocarbocyanine perchlorate (DiI; Molecular Probes, Eugene, OR) as previously described.23 Approximately 3 × 105 labeled mononuclear cells were then autologously returned to the bone marrow space of the femurs,24 after which G-CSF or distilled water (n = 6 each) was administered to the animals as described above. Fifteen weeks later, hearts of hamsters assigned to this protocol were used exclusively to prepare cryosections.
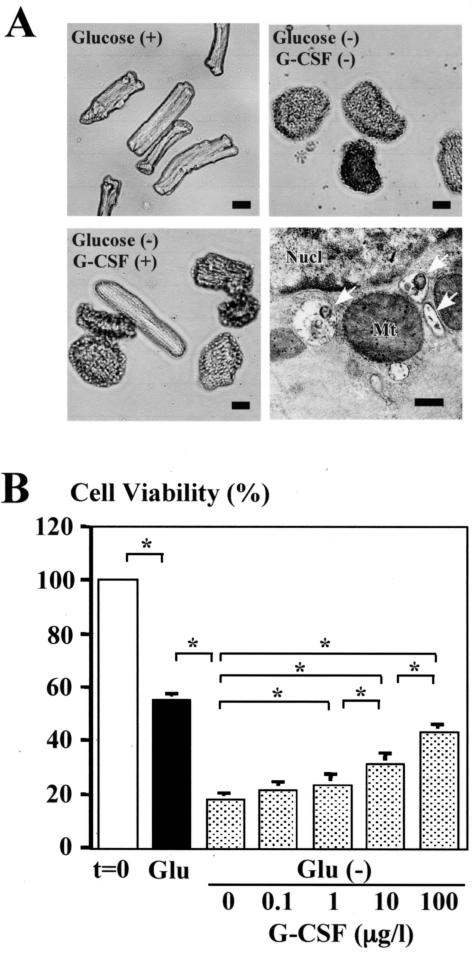
Protocol III: In Vitro Cell Death Assay
Ventricular cardiomyocytes were isolated from 8-week-old male Sprague-Dawley rats and cultured overnight by the method previously described.25,26 Culture media were replaced with glucose-depleted and 100 mmol/L mannitol-supplemented on the next day, as starvation is known to cause autophagic degeneration/death in various organs including the heart (glucose-starvation model).27,28 G-CSF (0, 0.1, 1, 10, or 100 μg/L) was simultaneously added to the media, and the cardiomyocytes were cultured for 96 hours. Cell viability was assessed by cellular rod shape with trypan blue dye exclusion.26
Blood Sampling
Blood used for hemocounts was drawn from the retro-orbital sinus before treatment and from the inferior vena cava at sacrifice.
Assessment of Cardiac Function
Echocardiography and cardiac catheterization were performed before sacrifice as previously described.29
Tissue Processing and Histology
One day before sacrifice, Evans blue dye (1% v/v; Sigma, St. Louis, MO) was intraperitoneally injected to the randomly chosen animals (n = 3 from each group). This was to detect cardiomyocytes with increased membrane permeability.29 The heart was transversely cut at the center between the atrioventricular groove and the apex. The basal half was fixed with 10% buffered formalin for histological examination. From the apical half, a small portion was removed and prepared as specimens for cryosections and for electron microscopy, and the rest was quickly immersed in liquid nitrogen for Western blotting and zymographic analyses. Other main organs including lungs and livers were excised and histologically examined.
On preparations taken from the center of the ventricle and stained with Masson’s trichrome, the percent fibrotic area (expressed by blue areas) was measured using a multipurpose color image processor LUZEX F (Nireco, Kyoto, Japan) by searching the entire ventricular slices. Cardiomyocyte size (as the transverse diameter of the cardiomyocyte cut at the nucleus level) was measured in the cells present in 20 randomly chosen high-power fields of the left ventricular free wall in each section. Numbers of cardiomyocytes, leukocytes, and macrophages were counted in a whole ventricular slice stained with hematoxylin and eosin.
In the animals injected with Evans blue dye 1 day before examination, the hearts were excised and cryosections were examined under a confocal microscope (LSM510; Zeiss, Jena, Germany) after nuclear staining with Hoechst 33342 (Sigma). The percentage of Evans blue-positive cells was calculated in 20 randomly chosen high-power fields in each section. We also examined Evans blue-positive cells without a nucleus to check whether those cells were actually dying.
Immunohistochemistry
The cardiac sections were incubated with a primary antibody against ubiquitin (DAKO Japan, Kyoto, Japan), cathepsin D (DAKO), Rab7 (Santa Cruz Biotechnology, Santa Cruz, CA),30 von Willebrand factor (DAKO), phosphorylated Akt (p-Akt; Cell Signaling, Beverly, MA), or phosphorylated signal transducer and activator of transcription-3 (p-Stat3, Cell Signaling). An ABC kit (Vector Laboratories, Burlingame, CA) was used for the immunostaining of the deparaffinized sections with diaminobenzidine as the chromogen and nuclei were stained with hematoxylin. Positive control sections for autophagic degeneration were obtained from mouse liver after 24 hours of starvation.27 For immunofluorescence, Alexa Fluor 488 (Molecular Probes) was the secondary antibody and nuclei were then stained with Hoechst 33342. After immunofluorescence the sections were observed under the confocal microscope.
In situ nick end-labeling assays were performed to detect apoptotic cells using an ApopTag kit (Chemicon Int., Temecula, CA) according to the manufacturer’s instructions. Positive control sections were from mouse mammary gland. The percentage of immunopositive cells was calculated in 20 randomly chosen high-power fields in each section.
Using hearts from the animals receiving autologous implantation of the DiI-labeled bone marrow cells 15 weeks before, the ventricles were cut into three transverse blocks. At least 20 cryosections (6-μm thick) from each block, and thus more than 60 cryosections from each heart, were made. They were then immunostained using the primary antibody against troponin I (Chemicon), von Willebrand factor (DAKO), or α-smooth muscle actin (Sigma). In a preliminary study, we checked the pattern of DiI uptake by bone marrow cells and by cultured adult rat ventricular cardiomyocytes that were obtained by the method previously described.25,26 For all sections, unanimous interpretation of the staining was acquired from two observers blinded to the specimen’s group.
Electron Microscopy
Cardiac specimens or cultured cardiomyocytes were fixed with phosphate-buffered 2.5% glutaraldehyde (pH 7.4) and postfixed with 1% osmium tetroxide, after which they were conventionally processed for electron microscopy (H700; Hitachi, Tokyo, Japan). Terminal dUTP nick-end labeling (TUNEL) assay at the electron microscopic level (EM-TUNEL) was performed on ultrathin sections as previously described.9
Western Blotting
Proteins (100 μg) extracted from hearts were subjected to polyacrylamide gel electrophoresis and then transferred onto polyvinylidene difluoride membranes. The membranes were then probed using the antibody against ubiquitin, cathepsin D, Rab7, p-Akt, p-Stat3, phosphorylated extracellular signal-regulated kinase (p-ERK, Cell Signaling), or tumor necrosis factor-α (TNF-α; eBioscience, San Diego, CA), and the blots were visualized by means of enhanced chemiluminescence (Amersham Biosciences, Piscataway, NJ). The signals were quantified by densitometry. α-Tubulin (analyzed using antibody from Sigma) was a loading control.
Gelatin Zymography
The activity of MMP was measured using the gelatin-zymography kit (Yagai Research Center, Yamagata, Japan).
Statistical Analyses
Values are presented as means ± SEM. Analysis of survival was evaluated using the Kaplan-Meier method with the log-rank Cox-Mantel method. The significance of differences in the findings was evaluated using Student’s t-test or one-way analysis of variance followed by the Newman-Keul’s multiple comparison test. Values of P < 0.05 were considered significant.
Results
Cardiomyocyte Degeneration and Death in UM-X7.1 Hamsters
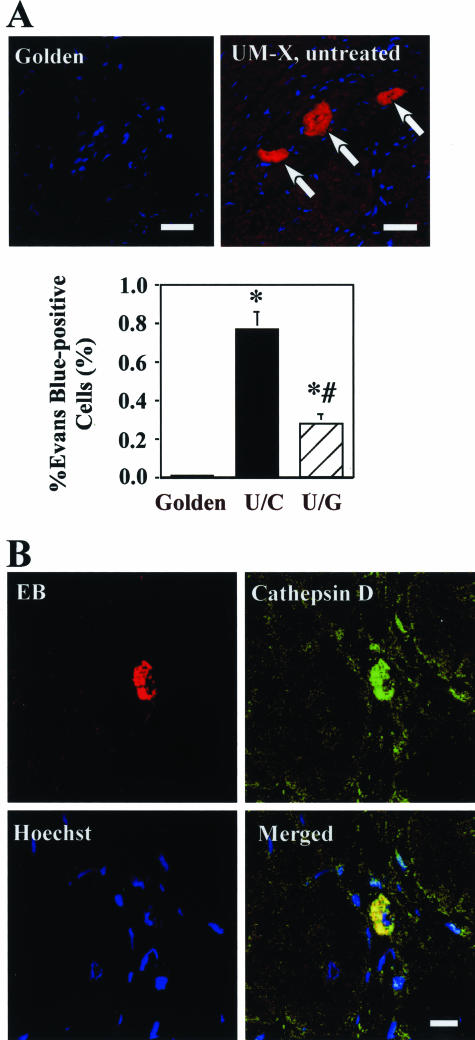
Spontaneous cardiomyocyte degeneration occurs in this strain.15,16 Sarcolemmal integrity was assessed by living staining with Evans blue dye. The dye is excluded by cardiomyocytes with normal sarcolemmal permeability but taken up by cardiomyopathic cells with leaky cell membranes.29 No cardiomyocyte was found to include Evans blue in golden hamsters. However, the hearts of UM-X7.1 hamsters exhibited extensive dye uptake (Figure 1A). Nuclei were absent in 6.7 ± 0.7% of Evans blue-positive cardiomyocytes in the untreated UM-X7.1 hearts, implying ongoing death in those cells.
Figure 1.
Confocal micrographs. A: Myocardium from the golden (left) and untreated UM-X7.1 (right) hamsters injected with Evans blue dye. Red fluorescence (arrows) indicates uptake of Evans blue; blue fluorescence shows nucleus. Percentages of cells taking up Evans blue are compared in the bar graph on the right. C, untreated golden hamster; C-U, untreated UM-X7.1 hamster; and U-G, G-CSF-treated UM-X hamster. *P < 0.05. B: Myocardium from the untreated UM-X7.1 hamster injected with Evans blue (red) and immunostained for cathepsin D (green). Nuclei (blue) are counterstained with Hoechst 33342. Scale bars, 50 μm (A); 10 μm (B).
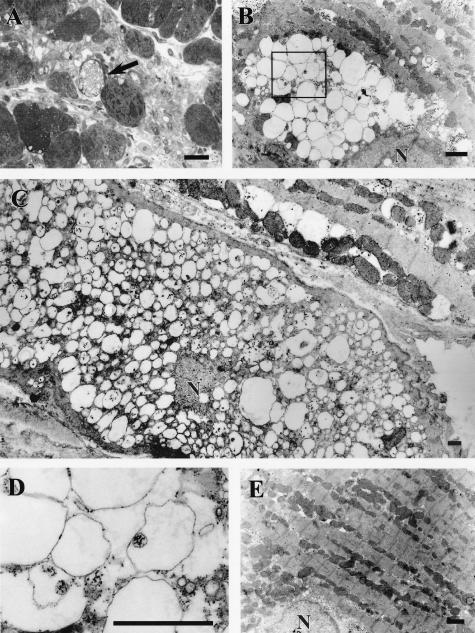
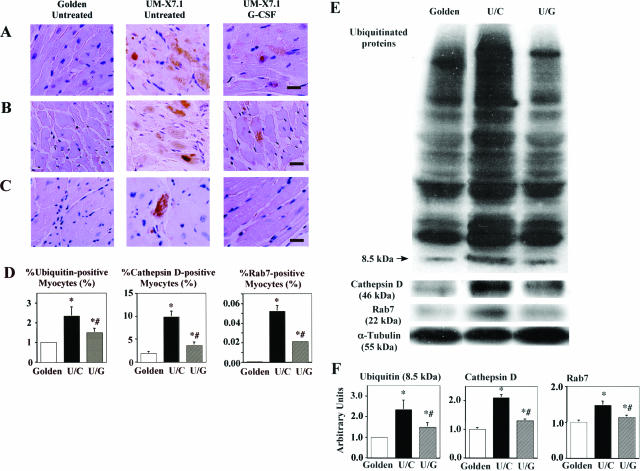
Ultrastructural analysis of the hearts revealed various grades of autophagic degenerative changes in cardiomyocytes (Figure 2, A–D). By contrast, we found no clear evidence of interstitial cell degeneration/death in the UM-X7.1 hearts. In addition, immunostaining for ubiquitin, cathepsin D, and Rab7 revealed significantly higher incidences of cardiomyocytes in the UM-X7.1 hamsters than in the hearts of golden hamsters (Figure 3, A–D). In particular, ubiquitin and cathepsin D were expressed as granular cytoplasmic inclusions (Figure 3, A and B). Western blotting confirmed up-regulation of ubiquitin, cathepsin D, and Rab7 in the hearts of UM-X7.1 hamsters (Figure 3, E and F). Next, to examine whether such degeneration may be causatively related with cell death, we observed the hearts of animals injected with Evans blue after immunostaining for cathepsin D. We found that almost all Evans blue-positive cardiomyocytes were also positive for cathepsin D (Figure 1B), suggesting a direct linkage between autophagic degeneration and death in cardiomyopathic cells.
Figure 2.
A to D: Light and electron micrographs showing severe vacuolar degeneration in cardiomyocytes from untreated UM-X7.1 hearts. A: A semithin section showing a cardiomyocyte with severe vacuolar degeneration (arrow). B and D: The vacuoles contained degraded subcellular organelles (eg, mitochondria) as indicated by arrows in D and thus appeared autophagic vacuoles. C: An example of a cardiomyocyte in which the cytoplasm is almost replaced by vacuoles. Arrows indicate barely remaining myofibrils. Such degenerative changes were attenuated in the G-CSF-treated group (E). Nucl, nucleus. Scale bars, 10 μm (A); 1 μm (B–E).
Figure 3.
Immunohistochemistry and Western blotting for markers of autophagy. A–C: Immunostaining for ubiquitin (A), cathepsin D (B), and Rab7 (C) in the myocardium. D: Percentages of the immunopositive cells are compared in the bar graphs. E and F: Western blots for myocardial ubiquitin, cathepsin D, and Rab7 (E) and graphs showing densitometry (F). In ubiquitin blotting, the whole gel image is shown to demonstrate the distribution of ubiquitinated substrates. P < 0.05 compared with the value of untreated golden hamsters (∗) or that of untreated UM-X7.1 hamsters (#). Scale bars, 20 μm.
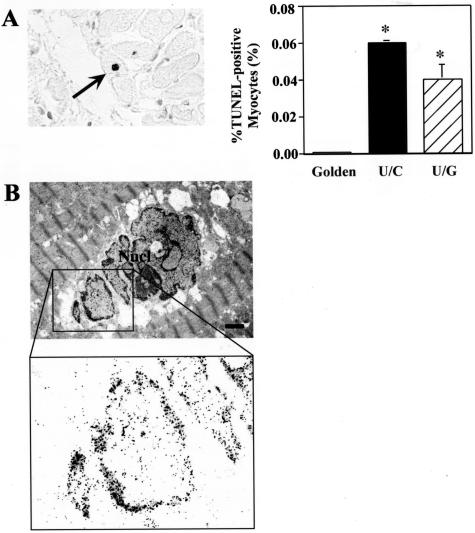
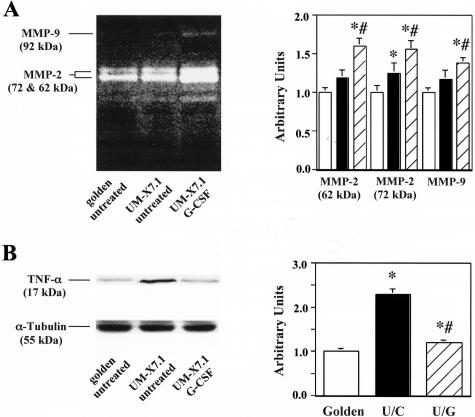
Rare TUNEL-positive cardiomyocytes were found, although significantly more in UM-X7.1 hamsters than in golden hamsters (Figure 4A). EM-TUNEL revealed that TUNEL-positive cardiomyocytes exhibited not apoptotic ultrastructure but hypertrophied nuclei (Figure 4B). This finding was consistent with human DCM, as previously reported,9 and suggests a false-positive TUNEL reaction as apoptosis. Catalytic activity of both MMP-2 and MMP-9 in the heart was significantly higher in the UM-X7.1 hamsters compared with the golden hamsters (Figure 5A). Cardiac TNF-α levels were up-regulated in the 30-week-old UM-X7.1 hamsters (Figure 5B).
Figure 4.
TUNEL and EM-TUNEL assays. A: Photograph of a TUNEL-positive cardiomyocyte (arrow) in the heart of untreated UM-X7.1 hamster and graph showing the percentage of TUNEL-positive cardiomyocytes among groups. *P < 0.05 compared with untreated golden hamsters. B: An EM-TUNEL-positive cardiomyocyte reveals that such a cell is not ultrastructurally apoptotic, suggesting a false-positive TUNEL reaction as apoptosis.
Figure 5.
Effect of G-CSF on MMP catalytic activity and expression of TNF-α protein in hearts. A: Gelatin zymogram. B: Western blot for TNF-α. The bar graphs summarize the quantifications by densitometry. P < 0.05 compared with the value of untreated golden hamsters (∗) or that of untreated UM-X7.1 hamsters (#).
Effect of G-CSF to UM-X7.1 Hamsters
Hemocount
Granulocyte counts in animals treated with G-CSF for 15 weeks reached 14,921 ± 1037 cells/μl, which was significantly greater than the counts obtained from untreated controls (774 ± 65 cells/μl) or the baseline counts obtained from the groups before the treatment (694 ± 168 cells/μl). There was no significant difference in red blood cell or platelet counts between the groups.
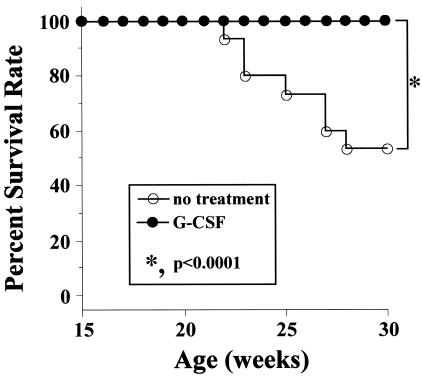
Improvement of Survival and Cardiac Function and Structure
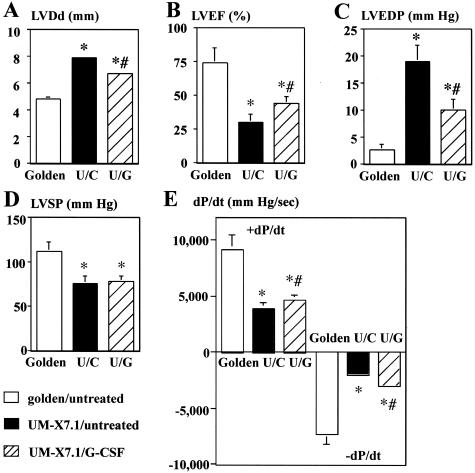
Although 7 of 15 untreated UM-X7.1 hamsters died by 30 weeks of age (survival rate, 53%), all 16 hamsters (100%) treated with G-CSF survived 30 weeks (Figure 6). All golden hamsters, with or without G-CSF-treatment, survived until the age of 30 weeks. At 30 weeks of age, all of the surviving animals underwent echocardiography and cardiac catheterization. The untreated UM-X7.1 hamsters showed severe left ventricular (LV) enlargement and signs of decreased cardiac function compared with the untreated golden hamsters (Figure 7): low LV ejection fraction (%EF), high LV end-diastolic pressure, and reduced ±dp/dt. All of those parameters were significantly improved in the G-CSF-treated animals (Figure 7). On the other hand, there was no difference in systolic LV pressure, diastolic aortic pressure, or heart rates between the untreated and G-CSF-treated UM-X7.1 hamsters. G-CSF did not affect cardiac function of golden hamsters (data not shown).
Figure 6.
Effect of G-CSF on the survival curve for cardiomyopathic hamsters. The treatment was started at 15 weeks of age and continued until 30 weeks of age.
Figure 7.
Effect of G-CSF on cardiac function based on echocardiography (A and B) and cardiac catheterization (C–E). C, untreated golden hamster; U/C, untreated UM-X7.1 hamster; U/G, G-CSF-treated UM-X7.1 hamster. LVDd, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LVEDP, left ventricular end-diastolic pressure; LVSP, left ventricular peak systolic pressure. P < 0.05 compared with the value of untreated golden hamsters (∗) or with that of untreated UM-X7.1 hamsters (#).
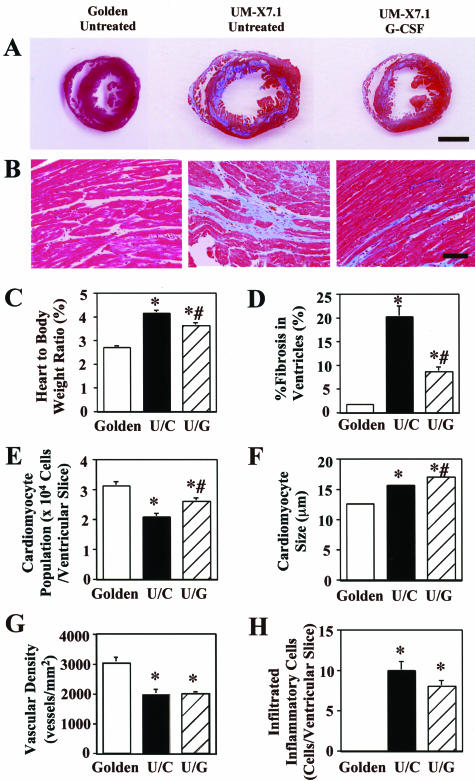
The hearts of untreated UM-X7.1 were bigger and heavier at necropsy than those of golden hamsters, but the degree was attenuated in the G-CSF-treated UM-X7.1 (Figure 8, A and C). Histologically, there were numerous fibrotic foci and abundant interstitial fibrosis in the ventricles of untreated UM-X7.1 hearts, which were significantly mitigated in the ventricles of G-CSF-treated hearts: percent area of ventricular fibrosis was 20.2 ± 2.3% in the untreated group versus 8.6 ± 1.0% in the G-CSF group of UM-X7.1 hamsters (Figure 8, B and D). In fact the percent area of fibrosis in the G-CSF group at 30 weeks of age was not different from that seen before treatment, when the animals were only 15 weeks of age (7.3 ± 1.3%, n = 6). Cardiomyocyte population per ventricular slice was smaller in the untreated UM-X7.1 compared with that in golden hamsters, which was partially restored by the G-CSF treatment (Figure 8E). Such an attenuated fibrosis and restored cardiomyocyte population in hearts suggest a protective effect of G-CSF against cardiomyocyte dropout in the cardiomyopathic hamster. The cardiomyocyte size of the untreated UM-X7.1 hamsters was greater than that of golden hamsters, and the increase in the size was significantly augmented by the G-CSF treatment (golden, 12.6 ± 0.24 μm; untreated UM-X7.1, 15.7 ± 0.27 μm; and G-CSF-treated UM-X7.1, 17.0 ± 0.19 μm; P < 0.05) (Figure 8F). Vascular density in myocardium was significantly reduced in UM-X7.1 hamsters, compared with golden hamsters. Treatment with G-CSF did not affect the density in UM-X7.1 hamsters (Figure 6G). Inflammatory cell infiltration into the myocardium was rare in both groups of UM-X7.1, although greater compared with that in golden hamsters, and the numbers of infiltrated inflammatory cells (granulocytes, lymphocytes, and macrophages) were similar between the untreated and G-CSF-treated UM-X7.1 (Figure 8H). When we examined the animals for adverse reactions, including splenic rupture, splenomegaly, thromboembolism, interstitial pneumonia, and atherosclerosis, we detected no notable adverse effect of G-CSF.
Figure 8.
Effect of G-CSF on cardiac pathology. A: Light micrographs of the whole ventricular slices. Masson’s trichrome stain. B: Highly magnified photographs of the myocardial tissue. C–E: Graphs showing the heart to body weight ratio, the percent areas of fibrosis in the ventricles, the numbers of cardiomyocytes in a whole ventricular slice, the size of cardiomyocytes, vascular density, and the infiltrated inflammatory cell population. P < 0.05 compared with the value of untreated golden hamsters (∗) or with that of untreated UM-X7.1 hamsters (#). Scale bars: 5 mm (A); 100 μm (B).
Preventive Effect of G-CSF on Autophagic Alteration but Not on Incidence of TUNEL-Positive Cardiomyocytes
The incidence of cardiomyocytes with Evans blue dye uptake was clearly decreased in the G-CSF-treated hearts of UM-X7.1 hamsters, compared to that of the untreated group (Figure 1A). Cardiomyocytes with autophagic degenerative ultrastructure were diminished in the G-CSF-treated group (Figure 2E). In addition, immunostaining for ubiquitin, cathepsin D, and Rab7 revealed significantly lower incidences of cardiomyocytes in the G-CSF-treated hearts (Figure 3, A–D). Western blotting confirmed these findings (Figure 3, E and F). These suggest that G-CSF exerts a protective effect against autophagic degeneration and death of cardiomyocytes. The incidence of TUNEL-positive cardiomyocytes was similar between the untreated and G-CSF-treated UM-X7.1 hamsters (untreated, 0.06 ± 0.001% versus G-CSF, 0.04 ± 0.008%, P = n.s.) (Figure 4A).
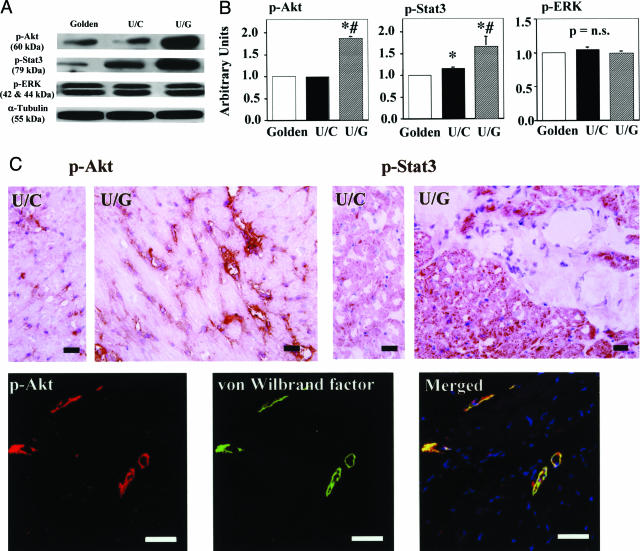
Activation of Downstream Signals of G-CSF
The binding of G-CSF to its receptor evokes signal transduction through activation of Janus kinase (Jak)/Stat; Akt kinase, which has been identified as a downstream target of phosphatidylinositol-3′-kinase (PI3K); and mitogen-activated protein kinase (MAPK)/ERK.21,31,32 Western blot analysis revealed that treatment with G-CSF resulted in a significant up-regulation of p-Stat3 and p-Akt, but not of p-ERK, in UM-X7.1 hearts (Figure 9, A and B).
Figure 9.
Downstream signals of G-CSF. A and B: Western blotting for myocardial p-Akt, p-Stat3, and p-ERK. The graphs show the densitometry (B). C: Immunohistochemistry for p-Akt and p-Stat3 in the untreated and G-CSF-treated UM-X7.1 hearts. P-Akt localized on endothelial cells whereas p-Stat3 localized on cardiomyocytes. Confocal images show p-Akt localization on von Willebrand factor-positive endothelial cells. Scale bars: 10 μm (C, top); 50 μm (C, bottom).
Immunohistochemistry revealed that p-Stat3 distributed on cardiomyocytes whereas p-Akt was exclusively on endothelial cells in the G-CSF-treated UM-X7.1 hearts (Figure 9C). And, both proteins appeared more intensely expressed in the G-CSF-treated hearts compared with the untreated ones. This suggests that Jak/Stat pathway may contribute for cardiomyocyte protection, consistent with the previous report.22
Increase in MMP Catalytic Activity and Decrease in TNF-α Content in the Heart
The MMP catalytic activity was significantly increased in the G-CSF-treated group, compared to that of the untreated group (Figure 5A). G-CSF significantly reduced cardiac TNF-α levels (Figure 5B).
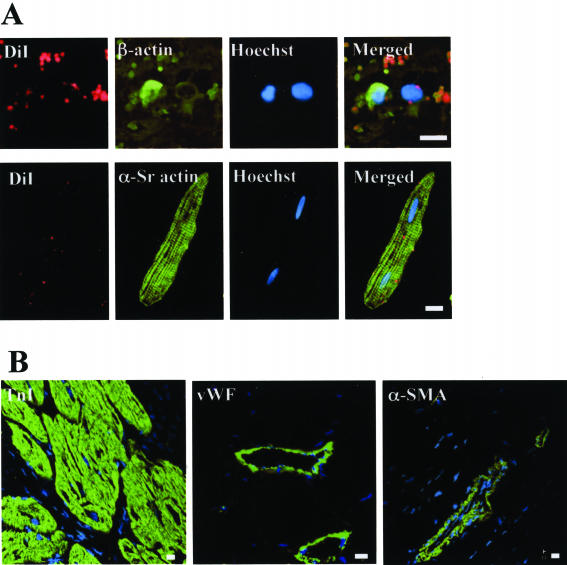
No DiI-Labeled (Bone Marrow-Derived) Cardiomyocytes and Vascular Cells
In another set of experiment, we evaluated the mobilization of DiI-labeled bone marrow cells into the heart. In our preliminary study, DiI was taken up by both bone marrow cells and cultured adult cardiomyocytes and was distributed in a spotty pattern (Figure 10A), similar to that seen previously in neuronal cells.23 Extensive examination by confocal microscopy revealed no cardiac cells, ie, cardiomyocytes, endothelial cells, vascular smooth muscle cells, or interstitial cells, were positive for DiI in any hearts, in the G-CSF-treated and untreated hearts (Figure 10B).
Figure 10.
Confocal photomicrographs. A: Merged images of DiI fluorescence (red), immunostaining of the indicated cellular protein (green), and Hoechst 33342 (blue). Top: Smear of bone marrow cells showing DiI labeling and immunostaining of β-actin (green) using anti-β-actin antibody (Sigma). Bottom: Cultured rat cardiomyocytes labeled with DiI and α-sarcomeric actin (green) detected by anti-α-sarcomeric actin antibody (DAKO). These are positive control sections for DiI. B: Myocardium from a G-CSF-treated UM-X7.1hamster. No DiI spots (red) are observed, merging with green fluorescence of troponin I, von Willebrand factor, or α-smooth muscle actin. Nuclei (blue) are counterstained with Hoechst 33342. Scale bars, 10 μm.
Effect of G-CSF on Cultured Adult Cardiomyocytes
After 96 hours, survival rate was markedly reduced when cardiomyocytes were cultured in glucose-depleted media (Figure 11A). Electron microscopy confirmed many autophagic vacuoles in the cardiomyocytes with glucose starvation (Figure 11A). Addition of G-CSF significantly improved the survival in a dose-dependent manner (Figure 11B).
Figure 11.
In vitro cell death assay. A: Light microphotographs of adult cardiomyocytes incubated for 96 hours in glucose-containing media (top left), glucose-depleted media without G-CSF (top right), and glucose-depleted media with 10 μg/L G-CSF (bottom left) and electron microphotograph showing autophagic vacuoles in a glucose-depleted cardiomyocyte (bottom right). Nucl, nucleus; Mt, mitochondria. White arrows indicate autophagic vacuoles. B: Survival rate of cultured cardiomyocytes after 96 hours of incubation. Glu, glucose. *P < 0.05. Scale bars: 10 μm (top); 0.5 μm (bottom).
Discussion
Autophagy as the Major Mode of Cardiomyocyte Death in Nonischemic Cardiomyopathy
In the present study, we found abundant autophagic degeneration in cardiomyocytes of the cardiomyopathic hamsters, in which cathepsin D and Rab7 were overexpressed. Importantly, we suggested that cardiomyocyte death succeeds to autophagic degeneration based on the finding that most of the cardiomyocytes with disrupted plasma membrane were positive for cathepsin D. Although TUNEL-positive cardiomyocytes were more frequently found in the cardiomyopathic hamsters than in the healthy hamsters, the positivity rate was very low and moreover, the false-positive reaction of TUNEL as apoptosis was suggested by the EM-TUNEL assay. This is consistent with a recent report indicating apoptosis does not significantly contribute to cardiomyocyte dropout in another DCM hamster model (glycoprotein-sarcoglycan deficiency) similar to ours.33 Thus, autophagy rather than apoptosis is the major mode of cardiomyocyte death of the present cardiomyopathic hamster.
TNF-α, which is elevated in patients with heart failure, is not only a cytotoxic cytokine that directly depresses cardiac function,34 it also up-regulates angiotensin II type 1 receptor, thereby contributing to angiotensin II-mediated organ fibrosis.35 In general, members of the MMP family are up-regulated in CHF, and in postmyocardial infarction models of CHF, their inhibition has a beneficial effect on cardiac remodeling and function.36 It is believed that increases in MMP can exacerbate heart failure by catalyzing collagen degradation. In addition to autophagy of cardiomyocytes, the up-regulation of these cytokines may play an important role as pathogenesis of cardiac heart failure in this model.
Beneficial Effect of G-CSF on Cardiomyopathic Hamsters and the Mechanisms
G-CSF treatment improved survival, cardiac function, and fibrosis. It reduced autophagic degeneration of cardiomyocytes as indicated by ultrastructure and immunopositivity for cathepsin D and Rab7. Although it is known that G-CSF can induce transdifferentiation of stem cells in bone marrow into cardiac cells, we could not find DiI-labeled cardiomyocytes and vascular cells in hearts. Our approach certainly underestimated the regenerative effect of G-CSF because only ∼3 × 105 bone marrow mononuclear cells were labeled with DiI and the others were not. Therefore, the negative finding does not deny bone marrow-derived myocardial regeneration. However, we would be able to say that the incidence may not be enough to explain the beneficial effects of G-CSF. In contrast, using an in vitro model, we have demonstrated that G-CSF directly protected cultured cardiomyocytes from glucose depletion-induced death. Thus, the beneficial effects of G-CSF may be associated with the cardiomyocyte protection against autophagic degeneration and death of cardiomyocytes rather than cardiac cell regeneration.
The G-CSF treatment induced a further increase in the size (transverse diameter) of cardiomyocytes, compared with the untreated UM-X7.1 where cardiomyocytes were already hypertrophied. Hypertrophic growth of the myocardium is thought to preserve pump function, although prolongation of the hypertrophic state is a leading predictor of arrhythmias, sudden death, and heart failure.37,38 However, not all forms of cardiac hypertrophy are necessarily pathological, as athletic conditioning can stimulate heart growth without deleterious consequence, ie, a physiological type of cardiac hypertrophy.39 The observed G-CSF-induced hypertrophy cannot be simply explained as a compensatory response because the hypertrophic reaction was more pronounced in G-CSF-treated hearts, which showed less severe heart failure than was seen in the untreated hearts. In the present study, moreover, we detected increased activation of both Akt and Stat3, ie, increased levels of phospho-Akt and phospho-Stat3, in the G-CSF-treated hearts. G-CSF is known to activate not only Akt, a serine threonine kinase and powerful survival signal in many systems,32 but also Stat3 in cardiomyocytes.22 In that regard, transgenic mice with cardiac-specific overexpression of active Akt not only exhibit hypertrophy but also enhanced LV function,40–42 as do transgenic mice with cardiac-specific overexpression of Stat3.43 Immunohistochemistry revealed that p-Stat3 was localized on cardiomyocytes in the present model. We therefore suggest that these downstream signals of G-CSF, Jak/Stat in particular, are associated with the cardiomyocyte hypertrophy observed in the G-CSF-treated hearts.
G-CSF resulted in a reduced heart weight despite causing cardiomyocyte hypertrophy. This apparent inconsistency may be partially reconciled by the reduction in fibrotic volume by the treatment. We also observed up-regulation of MMP catalytic activity, and down-regulation of TNF-α in the G-CSF-treated hearts. G-CSF was previously reported to induce both MMP-2 (gelatinase A/type IV collagenase) and MMP-9 (gelatinase B).44 The increases in MMP activity and down-regulation of TNF-α would be expected to contribute to the reduction in collagen content seen in G-CSF-treated hearts. It is well known that fibrosis, in particular interstitial fibrosis, often becomes excessive in DCM, accelerating cardiac remodeling and dysfunction, as is the case in the present model. Under those circumstances, an increase in MMP family proteins might exert a protective effect by catalyzing the degradation of the excessive collagen. Consistent with that idea, several earlier studies have shown that inhibition of MMP causes CHF,45 that targeted deletion of MMP-9 attenuates LV remodeling and collagen accumulation caused by overexpression of MMP-2 and MMP-13,46 and that an increase in MMP-1-induced by hepatocyte growth factor has a beneficial effect on postinfarction heart failure via its anti-fibrotic action.47
Coronary vascular abnormalities have been proposed as a primary defect of mice without δ-sarcoglycan.48 Although these vascular abnormalities could be secondary to the cardiomyocyte degeneration,49 verapamil effectively treated this animal model.50 Moreover, neovascularization seems to be an important part of G-CSF action in the case of a postmyocardial infarction model.20 In the present model, we noted reduced vascular density, compared with the control heart. However, we did not note its increase in the G-CSF-treated UM-X7.1 hearts even though more activated Akt, an angiogenetic factor, was confirmed in the present study.
G-CSF has already been confirmed to be safe and is widely used in patients with granulocytopenia, as well as in healthy individuals donating bone marrow for transplantation. The daily dose of G-CSF used in the present study (10 μg/kg/day) was well within the clinical dosage range used in humans.51 Thus, G-CSF administration may represent a new therapeutic strategy for prevention of development of heart failure, although it will certainly be necessary to confirm the safety of its long-term administration and to carefully construct the appropriate administrative protocols.
Acknowledgments
We thank Akiko Tsujimoto, Hatsue Ohshika, and the staff of Kyoto Women’s University (Hiroko Koyama, Noriko Koyoshi, Ayano Sasaki) for technical assistance.
Footnotes
Address reprint requests to Hisayoshi Fujiwara, M.D., Ph.D., Second Department of Internal Medicine, Gifu University School of Medicine, 1-1 Yanagido, Gifu 501-1194, Japan. E-mail: gifuim-gif@umin.ac.jp.
Supported in part by the Ministry of Education, Science, and Culture of Japan (research grants 15209027, 16590669, 16590721).
References
- Klionsky DJ, Emr SD. Autophagy as a regulated pathway of cellular degradation. Science. 2000;290:1717–1721. doi: 10.1126/science.290.5497.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danon MJ, Oh SJ, DiMauro S, Manaligod JR, Eastwood A, Naidu S, Schliselfeld LH. Lysosomal glycogen storage disease with normal acid maltase. Neurology. 1981;31:51–57. doi: 10.1212/wnl.31.1.51. [DOI] [PubMed] [Google Scholar]
- Tanaka Y, Guhde G, Suter A, Eskelinen EL, Hartmann D, Lullmann-Rauch R, Janssen PM, Blanz J, von Figura K, Saftig P. Accumulation of autophagic vacuoles and cardiomyopathy in LAMP-2-deficient mice. Nature. 2000;406:902–906. doi: 10.1038/35022595. [DOI] [PubMed] [Google Scholar]
- Nishino I, Fu J, Tanji K, Yamada T, Shimojo S, Koori T, Mora M, Riggs JE, Oh SJ, Koga Y, Sue CM, Yamamoto A, Murakami N, Shanske S, Byrne E, Bonilla E, Nonaka I, DiMauro S, Hirano M. Primary LAMP-2 deficiency causes X-linked vacuolar cardiomyopathy and myopathy (Danon disease). Nature. 2000;406:906–910. doi: 10.1038/35022604. [DOI] [PubMed] [Google Scholar]
- Maisch B, Ristic AD, Hufnagel G, Funck R, Alter P, Tontsch D, Pankuweit S. Dilated cardiomyopathies as a cause of congestive heart failure. Herz. 2002;27:113–134. doi: 10.1007/s00059-002-2373-8. [DOI] [PubMed] [Google Scholar]
- Narula J, Haider N, Virmani R, DiSalvo TG, Kolodgie FD, Hajjar RJ, Schmidt U, Semigran MJ, Dec GW, Khaw BA. Apoptosis in myocytes in end-stage heart failure. N Engl J Med. 1996;335:1182–1189. doi: 10.1056/NEJM199610173351603. [DOI] [PubMed] [Google Scholar]
- Olivetti G, Abbi R, Quaini F, Kajstura J, Cheng W, Nitahara JA, Quaini E, Di Loreto C, Beltrami CA, Krajewski S, Reed JC, Anversa P. Apoptosis in the failing human heart. N Engl J Med. 1997;336:1131–1141. doi: 10.1056/NEJM199704173361603. [DOI] [PubMed] [Google Scholar]
- Gill C, Mestril R, Samali A. Losing heart: the role of apoptosis in heart disease—a novel therapeutic target? FASEB J. 2002;16:135–146. doi: 10.1096/fj.01-0629com. [DOI] [PubMed] [Google Scholar]
- Kanoh M, Takemura G, Misao J, Hayakawa Y, Aoyama T, Nishigaki K, Noda T, Fujiwara T, Fukuda K, Minatoguchi S, Fujiwara H. Significance of myocytes with positive DNA in situ nick end-labeling (TUNEL) in hearts with dilated cardiomyopathy: not apoptosis but DNA repair. Circulation. 1999;99:2757–2764. doi: 10.1161/01.cir.99.21.2757. [DOI] [PubMed] [Google Scholar]
- Elsässer A, Suzuki K, Schaper J. Unresolved issues regarding the role of apoptosis in the pathogenesis of ischemic injury and heart failure. J Mol Cell Cardiol. 2000;32:711–724. doi: 10.1006/jmcc.2000.1125. [DOI] [PubMed] [Google Scholar]
- Knaapen MW, Davies MJ, De Bie M, Haven AJ, Martinet W, Kockx MM. Apoptotic versus autophagic cell death in heart failure. Cardiovasc Res. 2001;51:304–312. doi: 10.1016/s0008-6363(01)00290-5. [DOI] [PubMed] [Google Scholar]
- Shimomura H, Terasaki F, Hayashi T, Kitaura Y, Isomura T, Suma H. Autophagic degeneration as a possible mechanism of myocardial cell death in dilated cardiomyopathy. Jpn Circ J. 2001;65:965–968. doi: 10.1253/jcj.65.965. [DOI] [PubMed] [Google Scholar]
- Hein S, Arnon E, Kostin S, Schonburg M, Elsasser A, Polyakova V, Bauer EP, Klovekorn WP, Schaper J. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003;107:984–991. doi: 10.1161/01.cir.0000051865.66123.b7. [DOI] [PubMed] [Google Scholar]
- Kostin S, Pool L, Elsasser A, Hein S, Drexler HC, Arnon E, Hayakawa Y, Zimmermann R, Bauer E, Klovekorn WP, Schaper J. Myocytes die by multiple mechanisms in failing human hearts. Circ Res. 2003;92:715–724. doi: 10.1161/01.RES.0000067471.95890.5C. [DOI] [PubMed] [Google Scholar]
- Homburger F, Baker JR, Nixon CW, Wilgram G. New hereditary disease of Syrian hamsters. Primary, generalized polymyopathy and cardiac necrosis. Arch Intern Med. 1962;110:660–662. doi: 10.1001/archinte.1962.03620230106015. [DOI] [PubMed] [Google Scholar]
- Jasmin G, Proschek L. Hereditary polymyopathy and cardiomyopathy in the Syrian hamster. I. Progression of heart and skeletal muscle lesions in the UM-X71 line. Muscle Nerve. 1982;5:20–25. doi: 10.1002/mus.880050105. [DOI] [PubMed] [Google Scholar]
- Tsubata S, Bowles KR, Vatta M, Zintz C, Titus J, Muhonen L, Bowles NE, Towbin JA. Mutations in the human delta-sarcoglycan gene in familial and sporadic dilated cardiomyopathy. J Clin Invest. 2000;106:655–662. doi: 10.1172/JCI9224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlic D, Kajstura J, Chimenti S, Limana F, Jakoniuk I, Quaini F, Nadal-Ginard B, Bodine DM, Leri A, Anversa P. Mobilized bone marrow cells repair the infarcted heart, improving function and survival. Proc Natl Acad Sci USA. 2001;98:10344–10349. doi: 10.1073/pnas.181177898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocher AA, Schuster MD, Szabolcs MJ, Takuma S, Burkhoff D, Wang J, Homma S, Edwards NM, Itescu S. Neovascularization of ischemic myocardium by human bone-marrow-derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Nat Med. 2001;7:430–436. doi: 10.1038/86498. [DOI] [PubMed] [Google Scholar]
- Ohtsuka M, Takano H, Zou Y, Toko H, Akazawa H, Qin Y, Suzuki M, Hasegawa H, Nakaya H, Komuro I. Cytokine therapy prevents left ventricular remodeling and dysfunction after myocardial infarction through neovascularization. FASEB J. 2004;18:851–853. doi: 10.1096/fj.03-0637fje. [DOI] [PubMed] [Google Scholar]
- Minatoguchi S, Takemura G, Chen XH, Wang N, Uno Y, Koda M, Arai M, Misao Y, Lu C, Suzuki K, Goto K, Komada A, Takahashi T, Kosai K, Fujiwara T, Fujiwara H. Acceleration of the healing process and myocardial regeneration may be important as a mechanism of improvement of cardiac function and remodeling by postinfarction granulocyte colony-stimulating factor treatment. Circulation. 2004;109:2572–2780. doi: 10.1161/01.CIR.0000129770.93985.3E. [DOI] [PubMed] [Google Scholar]
- Harada M, Qin Y, Takano H, Minamino T, Zou Y, Toko H, Ohtsuka M, Matsuura K, Sano M, Nishi J, Iwanaga K, Akazawa H, Kunieda T, Zhu W, Hasegawa H, Kunisada K, Nagai T, Nakaya H, Yamauchi-Takihara K, Komuro I. G-CSF prevents cardiac remodeling after myocardial infarction by activating the Jak-Stat pathway in cardiomyocytes. Nat Med. 2005;11:305–311. doi: 10.1038/nm1199. [DOI] [PubMed] [Google Scholar]
- Honig MG, Hume RI. Fluorescent carbocyanine dyes allow living neurons of identified origin to be studied in long-term cultures. J Cell Biol. 1986;103:171–187. doi: 10.1083/jcb.103.1.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushida T, Inaba M, Hisha H, Ichioka N, Esumi T, Ogawa R, Iida H, Ikehara S. Intra-bone marrow injection of allogeneic bone marrow cells: a powerful new strategy for treatment of intractable autoimmune diseases in MRL/lpr mice. Blood. 2001;97:3292–3299. doi: 10.1182/blood.v97.10.3292. [DOI] [PubMed] [Google Scholar]
- Piper HM, Probst I, Schwartz P, Hutter FJ, Spieckermann PG. Culturing of calcium stable adult cardiac myocytes. J Mol Cell Cardiol. 1982;14:397–412. doi: 10.1016/0022-2828(82)90171-7. [DOI] [PubMed] [Google Scholar]
- Maruyama R, Takemura G, Aoyama T, Hayakawa K, Koda M, Kawase Y, Qiu X, Ohno Y, Minatoguchi S, Miyata K, Fujiwara T, Fujiwara H. Dynamic process of apoptosis in adult rat cardiomyocytes analyzed using 48-hour videomicroscopy and electron microscopy: beating and rate are associated with the apoptotic process. Am J Pathol. 2001;159:683–691. doi: 10.1016/S0002-9440(10)61739-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizushima N, Yamamoto A, Matsui M, Yoshimori T, Ohsumi Y. In vivo analysis of autophagy in response to nutrient starvation using transgenic mice expressing a fluorescent autophagosome marker. Mol Biol Cell. 2004;15:1101–1111. doi: 10.1091/mbc.E03-09-0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildenthal K, Dees JH, Buja LM. Cardiac lysosomal derangements in mouse heart after long-term exposure to nonmetabolizable sugars. Circ Res. 1977;40:26–35. doi: 10.1161/01.res.40.1.26. [DOI] [PubMed] [Google Scholar]
- Kawada T, Nakazawa M, Nakauchi S, Yamazaki K, Shimamoto R, Urabe M, Nakata J, Hemmi C, Masui F, Nakajima T, Suzuki J, Monahan J, Sato H, Masaki T, Ozawa K, Toyo-Oka T. Rescue of hereditary form of dilated cardiomyopathy by rAAV-mediated somatic gene therapy: amelioration of morphological findings, sarcolemmal permeability, cardiac performances, and the prognosis of TO-2 hamsters. Proc Natl Acad Sci USA. 2002;99:901–906. doi: 10.1073/pnas.022641799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez MG, Munafo DB, Beron W, Colombo MI. Rab7 is required for the normal progression of the autophagic pathway in mammalian cells. J Cell Sci. 2004;117:2687–2697. doi: 10.1242/jcs.01114. [DOI] [PubMed] [Google Scholar]
- Avalos BR. Molecular analysis of the granulocyte colony-stimulating factor receptor. Blood. 1996;88:761–777. [PubMed] [Google Scholar]
- Dong F, Larner AC. Activation of Akt kinase by granulocyte colony-stimulating factor (G-CSF): evidence for the role of a tyrosine kinase activity distinct from the Janus kinases. Blood. 2000;95:1656–1662. [PubMed] [Google Scholar]
- Ryoke T, Gu Y, Ikeda Y, Martone ME, Oh SS, Jeon ES, Knowlton KU, Ross J., Jr Apoptosis and oncosis in the early progression of left ventricular dysfunction in the cardiomyopathic hamster. Basic Res Cardiol. 2002;97:65–75. doi: 10.1007/s395-002-8389-4. [DOI] [PubMed] [Google Scholar]
- Mann DL. Inflammatory mediators and the failing heart: past, present, and the foreseeable future. Circ Res. 2002;91:988–998. doi: 10.1161/01.res.0000043825.01705.1b. [DOI] [PubMed] [Google Scholar]
- Peng J, Gurantz D, Tran V, Cowling RT, Greenberg BH. Tumor necrosis factor-alpha-induced AT1 receptor upregulation enhances angiotensin II-mediated cardiac fibroblast responses that favor fibrosis. Circ Res. 2002;91:1119–1126. doi: 10.1161/01.res.0000047090.08299.d5. [DOI] [PubMed] [Google Scholar]
- Spinale FG. Matrix metalloproteinases: regulation and dysregulation in the failing heart. Circ Res. 2002;90:520–530. doi: 10.1161/01.res.0000013290.12884.a3. [DOI] [PubMed] [Google Scholar]
- Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993;22:6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM. The risk of congestive heart failure: sobering lessons from the Framingham Heart Study. Curr Cardiol Rep. 2001;3:184–190. doi: 10.1007/s11886-001-0021-1. [DOI] [PubMed] [Google Scholar]
- Oakley D. General cardiology: the athlete’s heart. Heart. 2001;86:722–726. doi: 10.1136/heart.86.6.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMullen JR, Shioi T, Zhang L, Tarnavski O, Sherwood MC, Kang PM, Izumo S. Phosphoinositide 3-kinase(p110alpha) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. Proc Natl Acad Sci USA. 2003;100:12355–12360. doi: 10.1073/pnas.1934654100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka N, Ryoke T, Hongo M, Mao L, Rockman HA, Clark RG, Ross J., Jr Effects of growth hormone and IGF-I on cardiac hypertrophy and gene expression in mice. Am J Physiol. 1998;275:H393–H399. doi: 10.1152/ajpheart.1998.275.2.H393. [DOI] [PubMed] [Google Scholar]
- Kim YK, Kim SJ, Yatani A, Huang Y, Castelli G, Vatner DE, Liu J, Zhang Q, Diaz G, Zieba R, Thaisz J, Drusco A, Croce C, Sadoshima J, Condorelli G, Vatner SF. Mechanism of enhanced cardiac function in mice with hypertrophy induced by overexpressed Akt. J Biol Chem. 2003;278:47622–47628. doi: 10.1074/jbc.M305909200. [DOI] [PubMed] [Google Scholar]
- Kunisada K, Negoro S, Tone E, Funamoto M, Osugi T, Yamada S, Okabe M, Kishimoto T, Yamauchi-Takihara K. Signal transducer and activator of transcription 3 in the heart transduces not only a hypertrophic signal but a protective signal against doxorubicin-induced cardiomyopathy. Proc Natl Acad Sci USA. 2000;97:315–319. doi: 10.1073/pnas.97.1.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstanjen D, Ulbricht N, Iacone A, Regenfus M, Salama A. Matrix metalloproteinase-9 (gelatinase B) is elevated during mobilization of peripheral blood progenitor cells by G-CSF. Transfusion. 2002;42:588–596. doi: 10.1046/j.1537-2995.2002.00088.x. [DOI] [PubMed] [Google Scholar]
- Heymans S, Luttun A, Nuyens D, Theilmeier G, Creemers E, Moons L, Dyspersin GD, Cleutjens JP, Shipley M, Angellilo A, Levi M, Nube O, Baker A, Keshet E, Lupu F, Herbert JM, Smits JF, Shapiro SD, Baes M, Borgers M, Collen D, Daemen MJ, Carmeliet P. Inhibition of plasminogen activators or matrix metalloproteinases prevents cardiac rupture but impairs therapeutic angiogenesis and causes cardiac failure. Nat Med. 1999;5:1135–1142. doi: 10.1038/13459. [DOI] [PubMed] [Google Scholar]
- Ducharme A, Frantz S, Aikawa M, Rabkin E, Lindsey M, Rohde LE, Schoen FJ, Kelly RA, Werb Z, Libby P, Lee RT. Targeted deletion of matrix metalloproteinase-9 attenuates left ventricular enlargement and collagen accumulation after experimental myocardial infarction. J Clin Invest. 2000;106:55–62. doi: 10.1172/JCI8768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniyama Y, Morishita R, Nakagami H, Moriguchi A, Sakonjo H, Shokei-Kim, Matsumoto K, Nakamura T, Higaki J, Ogihara T. Potential contribution of a novel antifibrotic factor, hepatocyte growth factor, to prevention of myocardial fibrosis by angiotensin II blockade in cardiomyopathic hamsters. Circulation. 2000;102:246–252. doi: 10.1161/01.cir.102.2.246. [DOI] [PubMed] [Google Scholar]
- Coral-Vazquez R, Cohn RD, Moore SA, Hill JA, Weiss RM, Davisson RL, Straub V, Barresi R, Bansal D, Hrstka RF, Williamson R, Campbell KP. Disruption of the sarcoglycan-sarcospan complex in vascular smooth muscle: a novel mechanism for cardiomyopathy and muscular dystrophy. Cell. 1999;98:465–474. doi: 10.1016/s0092-8674(00)81975-3. [DOI] [PubMed] [Google Scholar]
- Wheeler MT, Allikian MJ, Heydemann A, Hadhazy M, Zarnegar S, McNally EM. Smooth muscle cell-extrinsic vascular spasm arises from cardiomyocyte degeneration in sarcoglycan-deficient cardiomyopathy. J Clin Invest. 2004;113:668–675. doi: 10.1172/JCI20410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn RD, Durbeej M, Moore SA, Coral-Vazquez R, Prouty S, Campbell KP. Prevention of cardiomyopathy in mouse models lacking the smooth muscle sarcoglycan-sarcospan complex. J Clin Invest. 2001;107:R1–R7. doi: 10.1172/JCI11642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroger N, Renges H, Kruger W, Gutensohn K, Loliger C, Carrero I, Cortes L, Zander AR. A randomized comparison of once versus twice daily recombinant human granulocyte colony-stimulating factor (filgrastim) for stem cell mobilization in healthy donors for allogeneic transplantation. Br J Haematol. 2000;111:761–765. [PubMed] [Google Scholar]