Abstract
Urocortin 1 (UCN) and adrenomedullin (AM) are two neuropeptides that have emerged as potential endogenous anti-inflammatory factors based on their production by and binding to immune cells. Because human septic shock involves excessive inflammatory cytokine production, we investigated the effect of UCN and AM in the production of inflammatory mediators and their therapeutic actions in two models of septic shock. Both peptides down-regulated the production of inflammatory mediators by endotoxin-activated macrophages. The administration of UCN or AM protected against lethality after cecal ligation and puncture or after injection of bacterial endotoxin and prevented septic shock-associated histopathology, such as infiltration of inflammatory cells and intravascularly disseminated coagulation in various target organs. The therapeutic effect of UCN and AM was mediated by decreasing the local and systemic levels of a wide spectrum of inflammatory mediators, including cytokines, chemokines, and the acute phase protein serum amyloid A. Importantly, UCN or AM treatment was therapeutically effective in established endotoxemia. In conclusion, UCN and AM could represent two multistep therapeutic agents for human septic shock to be used in combination with other immunomodulatory agents or complementary as anti-inflammatory factors to other therapies.
Septic shock is a systemic response to severe bacterial infections generally caused by gram-negative bacterial endotoxins. The administration of the endotoxin lipopolysaccharide (LPS) in experimental animals leads to pathophysiologic changes similar to human septic shock syndrome, and lethal endotoxemia has been extensively used as an experimental model of gram-negative septic shock.1 The severe pathological consequences of the septic shock syndrome give rise to a hyperactive and out-of-balance network of endogenous pro-inflammatory cytokines, including tumor necrosis factor-α (TNF-α), interleukin (IL)-12, IL-6, and interferon-γ (IFNγ).2 The overproduction of inflammatory cytokines generates systemic activation, which affects vascular permeability and cardiac function, induces metabolic changes that can lead to tissue necrosis, and eventually progresses to multiple-organ failure and death. Despite significant progress in understanding its pathophysiology, septic shock continues as the most common cause of death and morbidity in intensive care units. Promising experimental results prompted large-scale randomized clinical trial with a variety of agents designed to neutralize one or more of the inflammatory mediators involved in its pathology.3,4 But unfortunately, despite some promising results during preliminary trial, all of the major clinical studies of immunomodulators in sepsis have yielded disappointing results. Because of the complex pathophysiology of human sepsis, consideration should be given to multidrug therapy, similar to the approach taken in cancer and acquired immune deficiency syndrome therapy.
Urocortin 1 (UCN) and adrenomedullin (AM) are two recently discovered neuropeptides that are structurally related to corticotropin-releasing factor (CRF) and calcitonin-gene-related peptide (CGRP), respectively.5,6 Although UCN and AM were initially known by their cardiovascular protective activities,6,7 several indications suggest that they could act as endogenous immunomodulatory factors, with predominant anti-inflammatory effects. UCN and AM and their receptors are expressed by several immune cells, including macrophages/monocytes and T cells, in lymphoid organs and the gastrointestinal tract, and their expressions increase on inflammatory conditions.5,6,8–15 UCN inhibits experimental autoimmune encephalomyelitis,16 endotoxin-induced TNF-α production by Kupffer cells,17 and inflammatory bowel disease.18 In addition, UCN present in the mucosa of patients suffering from Helicobacter pylori-induced gastritis increases during the stage of eradication and amelioration of inflammation, whereas in patients resistant to treatment, its levels remain low.19 On the other hand, AM inhibits TNF-α production by activated macrophages and ameliorates inflammation-induced colitis.13,18,20,21 Based on their potential anti-inflammatory actions, we investigate here the potential therapeutic effect of UCN and AM in two murine models of septic shock. We report that treatment of endotoxemic mice with UCN or AM significantly reduces the mortality and pathology by down-regulating a broad spectrum of inflammatory factors.
Materials and Methods
Induction of Endotoxemia and Study Design
To induce endotoxemia, BALB/c and C57BL/6 mice (6 to 8 weeks old; The Jackson Laboratories, Bar Harbor, ME) were injected intraperitoneally (i.p.) with different amounts (25 to 600 μg/mouse; 400 μg/mouse unless otherwise indicated) of LPS (from Salmonella enteridis; Sigma, St. Louis, MO). Animals were treated i.p. with medium (controls) or with different concentrations (0.05 to 5.0 nmol/mouse; 6 to 550 μg/kg) of UCN or AM (American Peptides Company, Sunnyvale, CA) 30 minutes after challenge with LPS. Heat-inactivated UCN, CGRP, CRF, or the AM fragment AM20–50 (2 nmol), administered 30 minutes after LPS injection, were used as control peptides. In addition, combinations of AM, UCN, and cortistatin were used in some LPS-induced endotoxemia experiments. To study the therapeutic effect of delayed administration of AM and UCN on established endotoxemia, the peptides were injected i.p. (2 nmol/mouse) 2 or 4 hours after endotoxin administration. Animals were monitored every 12 hours for survival and other clinical signs including ruffled fur, lethargy, appearance of diarrhea, and body weight loss. Animals were sacrificed at different times after LPS injection, blood samples were collected by cardiac puncture, peritoneal exudates were obtained as described below, and liver, lungs, and small intestines were collected. The blood samples were allowed to clot for 1 hour at room temperature, and serum was obtained after centrifugation for determination of cytokines, chemokines, and serum amyloid A (SAA). Tissue specimens were immediately frozen in liquid nitrogen for histological studies, protein extraction, cytokine determination, and myeloperoxidase (MPO) activity measurement. The peritoneal suspension was centrifuged for 5 minutes at 1800 × g, and cell-free supernatants (peritoneal fluid) were harvested and assayed for cytokine/chemokine production. Peritoneal cells were counted and adjusted in phosphate-buffered saline/3 mmol/L ethylenediamine tetraacetic acid medium at 3 × 106 cells/ml. The number of viable cells in the different peritoneal subpopulations was determined by flow cytometry (FACScan; BD Biosciences, Mountain View, CA). Briefly, peritoneal lymphocytes, macrophages, and polymorphonuclear cells (PMNs) were gated according to their different forward scatter and side scatter characteristics and counted. The large predominance of neutrophils (99%) in the PMN population was confirmed in cytospin preparations stained with May-Grunwald and Giemsa. For histopathological evaluation, freshly collected liver, lungs, and intestines were fixed in 10% phosphate-buffered formalin, sectioned, and stained with hematoxylin and eosin using standard techniques.
Alternatively, sepsis was induced by cecal ligation and puncture (CLP). Briefly, C57BL/6 mice were anesthetized with ketamine (75 mg/kg, intramuscular injection) and xylazine (20 mg/kg, intramuscular injection), and a small abdominal midline incision was made. The cecum was exposed, mobilized, and ligated below the ileocecal valve and punctured twice with a 22-gauge needle, and the stool was extruded (1 mm). The cecum was then placed back into its normal intra-abdominal position, and the abdomen was closed with a running suture of 6-0 prolene. All animals received subcutaneous resuscitative normal saline (20 ml/kg body weight) 4 hours after surgery. Medium (controls), UCN (2 nmol), or AM (2 nmol) was administered i.p. twice at 6-hour intervals beginning 4 hours after CLP. Survival was monitored twice daily for 10 days.
Cytokine, SAA, and Nitric Oxide Determination
For cytokine determination in tissues, protein extracts were isolated by homogenization of lung, liver, and small intestine pieces (0.5 mg tissue/ml) in 50 mmol/L Tris-HCl, pH 7.4, with 0.5 mmol/L dithiothreitol and 10 μg/ml of a cocktail of proteinase inhibitors containing phenylmethylsulfonyl fluoride, pepstatin, and leupeptin (Sigma). Samples were centrifuged at 30,000 × g for 20 minutes and stored at −80°C until cytokine determination. Cytokine and chemokine levels in the serum, tissue protein extracts, and culture supernatants were determined by a specific sandwich enzyme-linked immunosorbent assay (ELISA) by using capture/biotinylated detection antibodies from BD Pharmingen (San Diego, CA) and Preprotech (Rocky Hill, NJ) according to the manufacturers’ recommendations. SAA levels were determined in serum samples by a murine ELISA kit (Tridelta Development, Wicklow, Ireland). The amount of nitric oxide (NO) formed was estimated from the accumulation of the stable NO metabolite nitrite by the Griess assay. Equal volumes of culture supernatants (90 μl) and Griess reagents (90 μl of 1% sulfanilamide/0.1% N-[naphthyl]ethyl-enediamine dihydrochloride in 2.5% H3PO4) were mixed, and the absorbance was measured at 550 nm. The amount of nitrite was calculated from a NaNO2 standard curve.
MPO Assay
Neutrophil infiltration in the lungs, liver, and small intestines was monitored by measuring MPO activity. Briefly, tissue specimens were homogenized at 50 mg/ml in phosphate buffer (50 mmol/L, pH 6.0) with 0.5% hexadecyltrimethylammonium bromide. Samples were frozen and thawed three times and centrifuged at 30,000 × g for 20 minutes. The supernatants were diluted 1:30 with assay buffer consisting in 50 mmol/L phosphate buffer, pH 6.0, with 0.167 mg/ml o-dianisidine (Sigma) and 0.0005% H2O2, and the colorimetric reaction was measured at 450 nm between 1 and 3 minutes in a spectrophotometer (Beckman Instruments, Irvine, CA). MPO activity per gram of wet tissue was calculated as follows: MPO activity (U/g wet tissue) = (A450) (13.5)/tissue weight (g), where A450 is the change in the absorbance of 450 nm light from 1 to 3 minutes after the initiation of the reaction. The coefficient 13.5 was empirically determined such that 1 U of MPO activity is the amount of enzyme that will reduce 1 μmol peroxide/minute.
Macrophage Cultures
Resident macrophages were obtained by peritoneal lavage with RPMI 1640. Peritoneal cells were washed in cold medium and incubated in complete medium (RPMI 1640 supplemented with 100 U/ml penicillin/streptomycin, 2 mmol/L L-glutamine, 50 μmol/L 2-mercaptoethanol, and 10% heat-inactivated fetal calf serum) at a concentration of 106 cells/ml. After 2 hours at 37°C, nonadherent cells were removed by extensive washing. At least 95% of the adherent cells were macrophages as judged by morphological and phagocytic criteria and by flow cytometry. Macrophage monolayers were incubated with complete medium in the absence (unstimulated) or presence of LPS (1 μg/ml, from Escherichia coli serotype 055:B5; Sigma). UCN or AM were added at different concentrations (from 10−7 to 10−13 mol/L) at the initiation of the culture. Cell-free supernatants were collected at different times, and cytokine/chemokine levels were determined as described above.
Data Analysis
All values are expressed as mean ± SD of mice per experiment. The differences between groups were analyzed by Mann-Whitney U-test and, if appropriate, by Kruskal-Wallis analysis of variance test. Survival curves were analyzed by the Kaplan-Meyer log-rank test.
Results
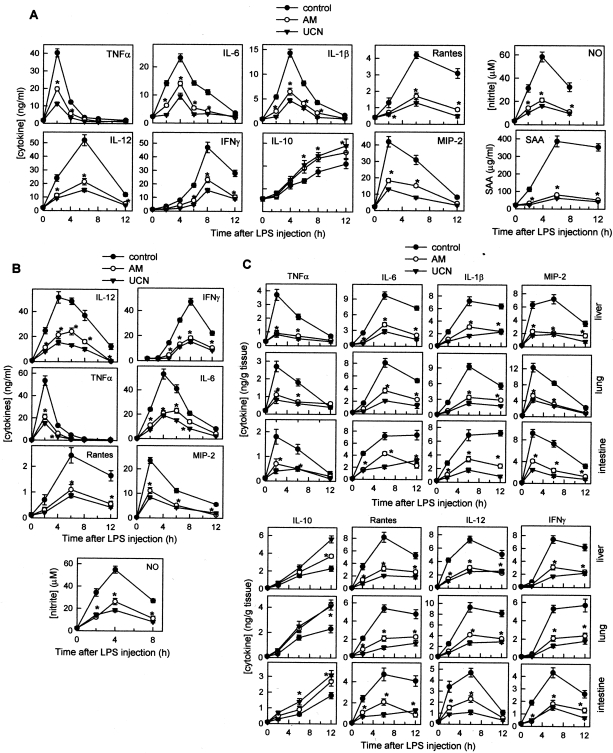
UCN and AM Inhibit the Production of Inflammatory Mediators by Activated Macrophages in Vitro
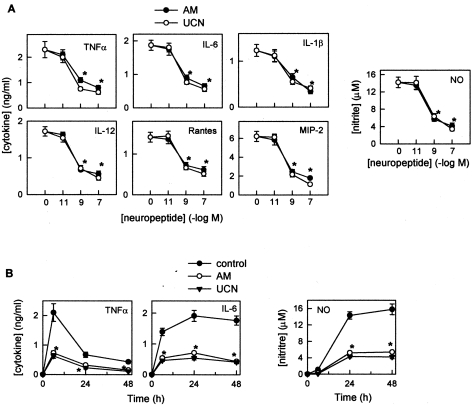
Macrophages, major participants in innate immunity, contribute to the initiation of the inflammatory response by killing pathogens through phagocytosis, release of cytotoxic oxygen and nitrogen intermediates, and release of chemokines and cytokines that attract and activate other immune cells. Despite the beneficial role of inflammatory factors in host defense, their sustained production can lead to serious pathological conditions. Therefore, although necessary for the elimination of pathogens, macrophage activation leads to serious deleterious effects in the host if left unchecked. To investigate the potential anti-inflammatory effect of AM and UCN, we evaluated first the effects of both peptides on the production of several inflammatory mediators by peritoneal macrophages. UCN and AM inhibited the production of the pro-inflammatory factors TNF-α, IL-6, and NO by activated macrophages (Figure 1). This effect was dose dependent with a maximal effect at 10−8 mol/L (not shown), a concentration that is within the physiological range.5–7,9,13
Figure 1.
UCN and AM inhibit the production of inflammatory mediators by activated macrophages in vitro. A: Peritoneal macrophages were stimulated with LPS (1 μg/ml) in the absence or presence of different concentrations of AM or UCN. After different times (6 hours for TNF-α and 24 hours for IL-6, IL-12, IL-1β, RANTES, and MIP-2), pro-inflammatory mediators were assayed as described in Materials and Methods (n = 6). B: Peritoneal macrophages were stimulated with LPS (1 μg/ml) in the absence (control) or presence of AM or UCN (10−8 mol/L) for different times, and the inflammatory factors were determined in the supernatants (n = 6). *P < 0.001 versus untreated control mice.
Treatment with UCN and AM Protects against Lethal Endotoxemia and Reduces the Related Histopathology
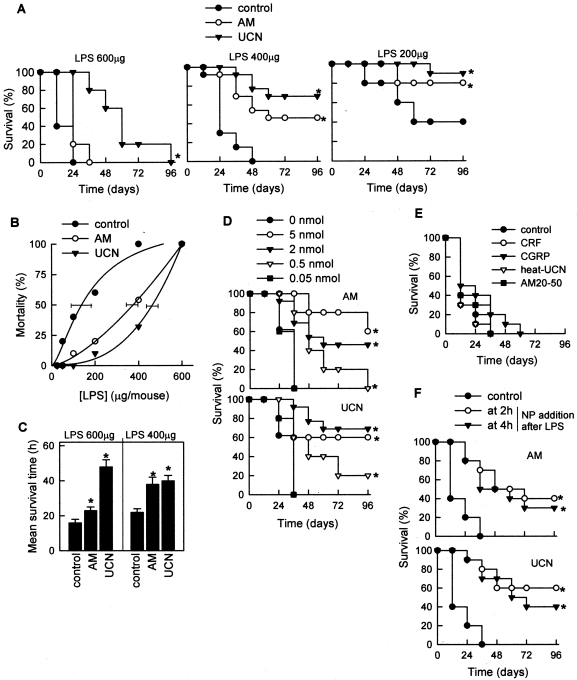
Because UCN or AM inhibits the production of pro-inflammatory macrophage-derived factors crucial for the development of septic shock, we expected a protective effect in high-dose endotoxemia, a murine model for septic shock syndrome. Mice were injected with different doses of LPS and treated 30 minutes later with UCN or AM (2 nmol/mouse; 400 μg/kg), and the survival was monitored. Treatment with UCN or AM significantly protected against the lethal effect of LPS (Figure 2A). This effect was not exclusive of BALB/c mice, and similar protective effects were obtained when C57BL/6 mice were used (not shown). The protective effect was observed over a wide range of LPS doses, with UCN and AM shifting the LPS dose causing 50% mortality (LD50) from 100 to 350 and 450 μg of LPS, respectively (Figure 2B). Animals injected with UCN or AM had a survival rate of 70 and 50%, respectively; even for the nonsurvivors, UCN and AM almost doubled the time until death (Figure 2C). The effect of both peptides was dose dependent, with doses as low as 0.5 nmol (100 μg/kg) being partially protective (Figure 2D). In contrast, CRF (a UCN-related peptide), CGRP (an AM-related peptide), heat-inactivated UCN, or the AM fragment AM20–50 (both used as control peptides) was not protective (Figure 2E). Our results demonstrate a slightly, although no significantly, higher effect of UCN than AM in preventing endotoxemia. These differences could be due to different expression levels of the receptors for UCN and AM in the cells involved in this response, to different pathway-coupling efficiencies, or to different peptide degradation rates in circulation or tissues.
Figure 2.
Treatment with UCN or AM protects against lethal endotoxemia. A–C: BALB/c mice were injected i.p. with different doses of LPS (control). AM or UCN (2 nmol/mouse) was injected i.p. 30 minutes after LPS administration. Survival was monitored over the next 96 hours. Similar results were obtained in three identical independent experiments or when C57BL/6 mice were used. Mortality curves in B were used to calculate LD50, and horizontal bars indicate the 95% confidence limits of LD50 determinations. In C, the average survival time was calculated for nonsurvivors in both the untreated and UCN/AM-treated groups. D: Mice were injected i.p. with 400 μg of LPS and different doses of UCN or AM (from 0 to 5 nmol/animal). E: Mice were injected i.p. with 400 μg of LPS and 30 minutes later, treated with medium (control), CRF, CGRP, or heat-inactivated UCN or the AM-fragment AM20–50 (2 nmol/mouse). Survival was monitored over the next 96 hours. F: UCN or AM (2 nmol/mouse) was injected i.p. 2 or 4 hours after LPS challenge. n = 12–20 mice/group. *P < 0.001 versus untreated control mice.
Because the production of inflammatory cytokines occurs in a rapid sequence starting with TNF-α, which reaches a maximum at 2 hours after LPS infusion (see below), we next investigated the therapeutic effect of UCN and AM on conditions of already established septic shock. Kinetic studies showed that both peptides exerted a full protective action when given up to 4 hours after shock induction (Figure 2F), with decreased protection for later UCN/AM administration (not shown). The ability of delayed administration of UCN and AM to ameliorate ongoing disease fulfills an essential prerequisite for any anti-endotoxemic agent, because treatment is started after the onset of sepsis in patients.
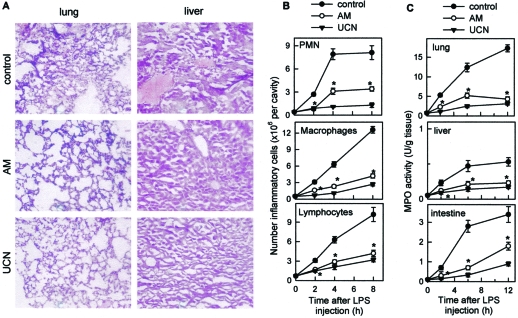
Endotoxemic animals suffered from disseminated intravascular coagulation with multiple organ failure as indicated by severe congestion, hemorrhage, hyperemia, fibrin deposits, edema, thrombosis, and massive accumulation of leukocytes in lungs (Figure 3A) and the intestinal tract (not shown), as well as severe congestion of the hepatic sinusoids and hepatocyte necrosis (Figure 3A) and segmental ischemia of the bowel with regions of hemorrhage or necrosis and an infracted cecum (not shown). Endotoxic shock induction was accompanied by an early granulocyte (mainly neutrophils) infiltration in the peritoneum, followed by later recruitment of macrophages and lymphocytes (Figure 3B). Neutrophil infiltration in the liver, lungs, and intestines of endotoxemic animals was confirmed through measurements of the MPO activity (Figure 3C). In contrast, animals treated with UCN or AM did not present any of the histopathological alterations associated with septic shock, such as disseminated intravascular coagulation, leukocyte infiltration, and inflammation in various organs and mesenteric ischemia, tissue congestion, and hemorrhage (Figure 3).
Figure 3.
AM and UCN reduce endotoxemia-associated histopathology. Mice were injected i.p. with LPS (control). UCN or AM (2 nmol/mouse) was administered i.p. 30 minutes after LPS administration. A: UCN and AM reduced inflammatory infiltration and disseminated coagulation in target organs. Histopathology analysis was determined in hematoxylin and eosin-stained sections of lung and liver obtained at 24 hours of disease (×150). B: UCN and AM reduce leukocyte recruitment in the peritoneal cavity. Peritoneal cell suspensions were obtained at different times after LPS injection, and numbers of macrophages, lymphocytes, and PMNs were determined by flow cytometry. C: UCN and AM decrease MPO activity in lungs, liver, and intestine. MPO content was determined at different times after LPS infusion. n = 8–12 mice/group. *P < 0.001 versus untreated control mice.
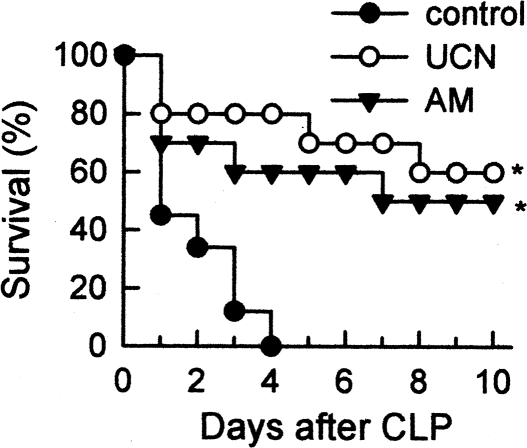
UCN and AM Improve Survival in Experimental Sepsis
We next investigated the potential therapeutic effect of UCN and AM in the murine model of CLP, a clinically relevant model for human sepsis because it causes lethal peritonitis produced by polymicrobial infection. Treatment with UCN or AM was started 4 hours after the induction of sepsis, at a time when mice show clear signs of sepsis, including lethargy, piloerection, diarrhea, huddling, fever, and malaise. UCN and AM treatments significantly improved survival (Figure 4) and attenuated the clinical manifestations of sepsis, such as lethargy, diarrhea, body weight loss, and hypothermia (not shown).
Figure 4.
UCN and AM protect against CLP-induced experimental sepsis. Sepsis was induced in C57BL/6 mice after CLP. UCN or AM (2 nmol) was administered i.p. twice at 6-hour intervals beginning 4 hours after CLP procedure. Survival was monitored over the next 8 days. n = 10 mice/group. *P < 0.001 versus untreated control mice.
Treatment with UCN or AM Reduces Local and Systemic Inflammatory Responses in Endotoxemic Mice
We next evaluated the effect of UCN or AM on the production of inflammatory mediators that are mechanistically linked to endotoxemia. The administration of UCN or AM reduced the levels of endotoxin-induced inflammatory cytokines (TNF-α, IFNγ, IL-6, IL-1β, and IL-12), chemokines (regulated upon activation normal T cells express sequence (RANTES) and macrophage inflammatory protein-2 (MIP-2)), and NO in serum (systemic) and in various target organs, including peritoneum, liver, lung, and intestine (Figure 5). In addition, UCN/AM administration increased the systemic and local levels of the anti-inflammatory cytokine IL-10 (Figure 5), which has been shown to be protective in endotoxic shock.22
Figure 5.
Treatment with UCN or AM reduces local and systemic inflammatory responses in endotoxemic mice. Endotoxemia was induced by i.p. injection of LPS (400 μg/mouse). Mice were treated 30 minutes later with medium (controls) or with UCN or AM (2 nmol/mouse). Serum (A), peritoneal fluid (B), and protein extracts from lungs, liver, and small intestines (C) were collected at various time points after endotoxin injection; and the cytokine/chemokine, NO, and SAA contents were determined as described in Materials and Methods. n = 6–8 mice/group. *P < 0.001 versus untreated control mice.
Coagulation abnormalities, especially disseminated intravascular coagulation and microthrombosis, are common features during sepsis.1–4,23 Acute phase proteins (APPs) are involved in the initiation of aberrant coagulation during endotoxic shock.23 Therefore, we also investigated the effect of UCN and AM on the production of the APP SAA during endotoxic shock. Both peptides dramatically decreased the systemic levels of SAA during septic shock (Figure 5A).
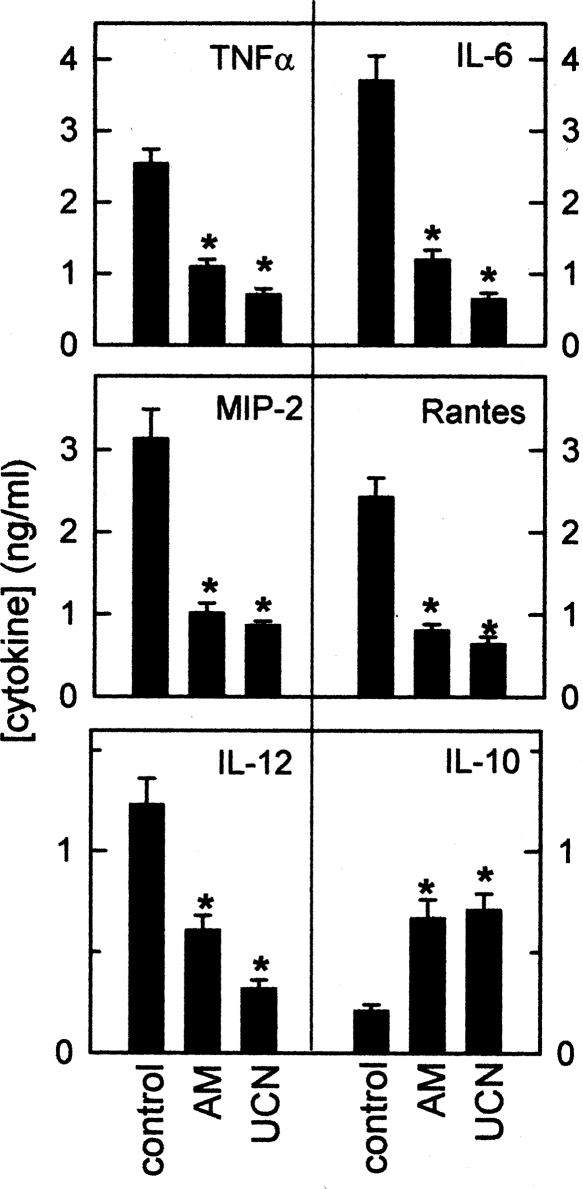
UCN and AM Deactivate Peritoneal Macrophages during Endotoxemia
The UCN/AM-induced decrease in the levels of inflammatory factors in the target organs could result from the reduction in inflammatory cell infiltration. However, the fact that both peptides down-regulate the in vitro production of various inflammatory factors by activated macrophages (Figure 1) argues against this hypothesis. We determined the capacity of peritoneal macrophages isolated from untreated or UCN/AM-treated endotoxemic mice to produce inflammatory mediators ex vivo. Although macrophages from mice with septic shock produced spontaneously high amounts of TNF-α, IL-6, IL-12, RANTES, and MIP-2, macrophages isolated from UCN/AM-treated animals produced significantly lower levels of pro-inflammatory cytokines and secreted high amounts of IL-10 (Figure 6). Therefore, it is plausible that the deactivation of resident and infiltrating macrophages is the major mechanism in the anti-inflammatory action of UCN and AM.
Figure 6.
Treatment with UCN or AM deactivates peritoneal macrophages during endotoxemia. Mice were injected i.p. with LPS (control) and treated i.p. with UCN or AM (2 nmol/mouse) 30 minutes later. Peritoneal macrophages were isolated 8 hours after LPS injection. Recovered macrophages (12 × 106 cells for control, 3 × 106 cells for UCN/AM) were cultured with medium alone at 5 × 105 cells/ml for 48 hours, and the concentration of inflammatory mediators in the culture supernatants was determined by ELISA. n = 5–6 mice/group. *P < 0.001 versus untreated control mice.
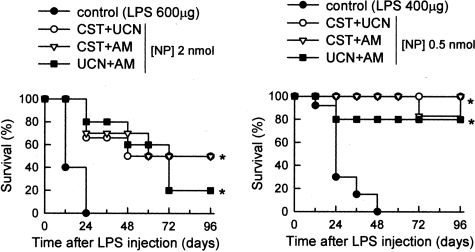
The Combined Therapy of UCN, AM, and Cortistatin Protects against Lethal Endotoxemia
We next evaluated the effect of the combined treatment with UCN, AM, and another endogenous anti-inflammatory peptide,24 cortistatin. Administration of UCN together with AM significantly prevented the lethality (20% survival) induced by a high dose of LPS (600 μg/mouse) (Figure 7, left), compared with mice treated with UCN or AM alone (Figure 2A). In addition, although endotoxic mice treated with cortistatin alone did not survive (not shown), the combined treatment with cortistatin and UCN or cortistatin and AM increased survival to 50% (Figure 7, left). This combined treatment permits reduction of the effective therapeutic dose to 0.5 nmol UCN/AM (Figure 7, right). This synergistic effect of UCN, AM, and cortistatin could be the result of effects on different cells or of the involvement of different signal transduction pathways in the same target cell. In the case of cortistatin, we favor the latter because activated macrophages are the major players in the anti-inflammatory activity of the three peptides, and both UCN and AM act through cAMP-dependent pathways,5,6 whereas the cortistatin effect is partially cAMP independent.25 However, because receptors for AM and UCN are ubiquitously present in monocytes/macrophages, dendritic cells, neutrophils, and endothelial cells (M. Delgado, unpublished data),5,6,13 the participation of cells other than macrophages in such anti-inflammatory action cannot be excluded, and if so, AM and UCN could differentially affect these cells.
Figure 7.
Combined therapy of UCN, AM, and cortistatin protects against lethal endotoxemia. Septic shock was induced by i.p. injection of LPS (600 or 400 μg/mouse). Mice were treated 30 minutes later with medium (controls) or with various combinations of the neuropeptides UCN, AM, and cortistatin (CST) (2 or 0.5 nmol/mouse). Survival was monitored over 96 hours. n = 8–10 mice/group. *P < 0.001 versus mice treated with cortistatin, UCN, or AM alone.
Discussion
The present work proposes a new therapy for endotoxemia based on the use of the neuropeptides UCN and AM. The administration of UCN or AM protected against endotoxin-induced lethality. In addition, treatment with UCN or AM improved survival in a “true infection” model resembling sepsis in humans, such as cecal ligation and puncture. UCN and AM prevented septic shock-associated histopathology, including inflammatory cell infiltration and multiorgan intravascular disseminated coagulation. The therapeutic effect of both peptides seems to be mediated through the decrease in the local and systemic levels of a wide spectrum of inflammatory mediators, including cytokines (TNF-α, IL-6, IL-1β, IFNγ, and IL-12), chemokines (MIP-2 and RANTES), and SAA. Our results suggest that deactivation of resident and infiltrating macrophages is the major mechanism in the anti-inflammatory action of UCN or AM in septic shock. In agreement with our results, UCN and AM were previously reported to decrease the production of TNF-α by macrophages and Kupffer cells.13,17,20,21 Although AM has been found to increase IL-6 in a macrophage cell line,20 in agreement with our results, AM reduces IL-6 production by synovial cells from rheumatoid arthritis patients and decreases serum IL-6 levels on human sepsis.26,27
Among the pro-inflammatory cytokines involved in endotoxic shock, TNF-α appears to play a central role. Increased serum TNF-α levels appear during endotoxemia, and TNF-α enhances procoagulant activity of vascular endothelial cells, activates neutrophils and macrophages, and increases adherent molecule expression, which in turn enhances neutrophil/monocyte infiltration and contributes to tissue injury.28 However, the central importance of inflammatory cytokines other than TNF-α in its pathogenesis is still debatable.29–33 IL-6 appears to be a better predictor for survival in patients with septic shock. In this sense, the fact that UCN or AM showed therapeutic effects administered 4 hours after induction of endotoxemia, once the TNF-α peak occurred suggests that both peptides could exert their effects independently of TNF-α inhibition. Thus, UCN and AM decrease the production of IL-6, NO, and various chemokines in endotoxemic mice. The UCN/AM-induced decrease of serum NO is beneficial because it should avoid the NO-mediated hypotension and cytotoxicity, two pathological hallmarks of septic shock.1–4 The fact that UCN or AM reduced local and systemic levels of the chemokines MIP-2 (chemotactic for neutrophils) and RANTES (chemotactic for macrophages/monocytes) partially explains the absence of inflammatory infiltrates in the affected organs. An additional mechanism is the UCN/AM-induced increase of IL-10, a delayed production of anti-inflammatory cytokine therapeutic for sepsis syndromes.34 Moreover, UCN and AM decreased the systemic levels of SAA, a hepatic APP that contributes to the disseminated intravascular coagulation and microthrombosis observed in sepsis.1–4,23 Therefore, the regulation by UCN and AM of this wide range of inflammatory mediators at both local and systemic levels, including mediators that appear later during the inflammatory response, explains the protection against established endotoxemia by UCN and AM and might offer a therapeutic advantage over current therapies using neutralizing antibodies directed against a single mediator. Additional mechanisms other than the anti-inflammatory effect could contribute to the therapeutic action of both peptides in endotoxic shock. For example, based in their vasodilatory properties promoting hyperdinamic circulation, AM and UCN could reduce the circulatory collapse and organ damage characteristic of sepsis.13,35–37 In addition, the infusion of UCN and AM increase the levels of β-adrenergic agonists,38,39 widely recognized as potent anti-inflammatory factors.
UCN is structurally related to CRF. Depending on the site of secretion, CRF has shown both pro- and anti-inflammatory actions. Central secretion of CRF activates the hypothalamus-pituitary-adrenal axis that ultimately induces the release of corticosteroids and subsequent anti-inflammatory actions.40–42 In contrast, peripherally secreted CRF is largely pro-inflammatory.43–45 In contrast to CRF, the anti-inflammatory effect of UCN in systemic inflammation and experimental autoimmune encephalomyelitis is corticosteroid independent.17 The present study and other evidence suggest that UCN may counteract the pro-inflammatory effects of CRF at inflammation sites.35 Interestingly, UCN preferentially binds to the CRF receptor type 2, and the distribution of UCN but not of CRF correlates with the distribution of the CRF receptor type 2 in the periphery.5
AM is structurally related to CGRP and binds to the calcitonin-related-like receptor (CRLR).6 Because patients and animals with sepsis show increased serum CGRP levels,46 CGRP has been suspected as an immunomodulatory factor. However, in contrast to AM, CGRP does not efficiently down-regulate the inflammatory response and fails preventing sepsis (Figure 2).47,48 The different effectiveness showed by AM and CGRP could reside in the differential binding of both peptides to different binding complexes, composed by the CRLR and various receptor activity-modifying proteins (RAMP1, RAMP2, and RAMP2). Thus, CGRP specifically binds to the CRLR-RAPM1 complex, whereas AM preferentially binds to CRLR associated to RAMP2 and RAMP3.6 We have recently observed that murine macrophages specifically express CRLR-RAMP2/3 complexes (E. Gonzalez-Rey, unpublished data). This partially explains the higher potency of AM versus CGRP on the inflammatory response.
Of physiological relevance is the observation that the expression of UCN and AM is increased in activated inflammatory cells5,6,9–15 and in several inflammatory conditions, including rheumatoid arthritis, gastritis, ulcerative colitis, and endotoxemia.13,19,45 Therefore, it is tempting to speculate that the body responds to an exacerbated inflammatory response by increasing the peripheral production of endogenous anti-inflammatory factors, including UCN and AM, in an attempt to restore homeostasis. Extending the use of UCN and AM to the human system, however, will depend on the peptide dosage and the expression of UCN/AM receptors in human immune cells, because species-related differences in expression have been found. In this sense, the widespread presence of UCN and AM receptors in all tissues of the body could limit their therapeutic application, because both peptides have differing actions affecting the cardiovascular system, stress and anxiety. However, we and others5,6 have not observed any adverse effects of the peptides, in terms of hypotension and anxiety-like behavior, at the concentrations used, probably because a short period of treatment with the peptides is enough to get a significant disease remission.
In summary, this work identifies UCN and AM as potent immunomodulatory factors with the capacity to deactivate the inflammatory response. UCN and AM might represent multistep therapeutic agents for human septic shock for use in combination with other immunomodulatory agents or complementary to other nonimmunomodulatory therapies.
Acknowledgments
We thank Dr. D. Ganea for advice and critical reading of the manuscript.
Footnotes
Address reprint requests to Mario Delgado, Instituto de Parasitologia y Biomedicina, Consejo Superior de Investigaciones Cientificas, Avd. Conocimiento, Parque Tecnologico Ciencias de la Salud, Granada 18100, Spain. E-mail: mdelgado@ipb.csic.es.
Supported by grants from the Spanish Ministry of Health (PI04/0674) and from Ramon Areces Foundation.
References
- Danner RL, Elin RJ, Hosseini JM, Wesley RA, Reilly JM, Parillo JE. Endotoxemia in human septic shock. Chest. 1991;99:169–175. doi: 10.1378/chest.99.1.169. [DOI] [PubMed] [Google Scholar]
- Netea MG, van der Meer JW, van Deuren M, Kullberg BJ. Proinflammatory cytokines and sepsis syndrome: not enough, or too much of a good thing? Trends Immunol. 2003;24:254–258. doi: 10.1016/s1471-4906(03)00079-6. [DOI] [PubMed] [Google Scholar]
- Bochud PY, Calandra T. Pathogenesis of sepsis: new concepts and implications for future treatments. Br Med J. 2003;326:262–266. doi: 10.1136/bmj.326.7383.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sessler CN, Shepherd W. New concepts in sepsis. Curr Opin Crit Care. 2002;8:465–472. doi: 10.1097/00075198-200210000-00016. [DOI] [PubMed] [Google Scholar]
- Vaughan J, Donaldson C, Bittencourt J, Perrin MH, Lewis K, Sutton S, Chan R, Turnbull AV, Lovejoy D, Rivier C. Urocortin, a mammalian neuropeptide related to fish urotensin I and to corticotropin-releasing factor. Nature. 1995;378:287–292. doi: 10.1038/378287a0. [DOI] [PubMed] [Google Scholar]
- Hinson JP, Kapas S, Smith DM. Adrenomedullin, a multifunctional regulatory peptide. Endocr Rev. 2000;21:138–167. doi: 10.1210/edrv.21.2.0396. [DOI] [PubMed] [Google Scholar]
- Oki Y, Sasano H. Localization and physiological roles of urocortin. Peptides. 2004;25:1745–1749. doi: 10.1016/j.peptides.2004.06.023. [DOI] [PubMed] [Google Scholar]
- Muramatsu Y, Fukushima K, Iino K, Totsune K, Takahashi K, Suzuki T, Hirasawa G, Takeyama J, Ito M, Nose M, Tashiro A, Hongo M, Oki Y, Nagura H, Sasano H. Urocortin and corticotropin-releasing factor receptor expression in the human colonic mucosa. Peptides. 2000;21:1799–1809. doi: 10.1016/s0196-9781(00)00335-1. [DOI] [PubMed] [Google Scholar]
- Gravanis A, Margioris AN. The corticotropin-releasing factor (CRF) family of neuropeptides in inflammation: potential therapeutic applications. Curr Med Chem. 2005;12:1503–1512. doi: 10.2174/0929867054039008. [DOI] [PubMed] [Google Scholar]
- Tsatsanis C, Androulidaki A, Dermitzaki E, Charalampopoulos I, Spiess J, Gravanis A, Margioris AN. Urocortin 1 and urocortin 2 induce macrophage apoptosis via CRFR2. FEBS Lett. 2005;579:4259–4264. doi: 10.1016/j.febslet.2005.06.057. [DOI] [PubMed] [Google Scholar]
- Saruta M, Takahashi K, Suzuki T, Torii A, Kawakami M, Sasano H. Urocortin 1 in colonic mucosa in patients with ulcerative colitis. J Clin Endocrinol Metab. 2004;89:5352–5361. doi: 10.1210/jc.2004-0195. [DOI] [PubMed] [Google Scholar]
- Kageyama K, Bradbury MJ, Zhao L, Blount AL, Vale WW. Urocortin messenger ribonucleic acid: tissue distribution in the rat and regulation in thymus by lipopolysaccharide and glucocorticoids. Endocrinology. 1999;140:5651–5658. doi: 10.1210/endo.140.12.7223. [DOI] [PubMed] [Google Scholar]
- Elsasser TH, Kahl S. Adrenomedullin has multiple roles in disease stress: development and remission of the inflammatory response. Microsc Res Tech. 2002;57:120–129. doi: 10.1002/jemt.10058. [DOI] [PubMed] [Google Scholar]
- Ueda S, Nishio K, Minamino N, Kubo A, Akai Y, Kangawa K, Matsuo H, Fujimura Y, Yoshioka A, Masui K, Doi N, Murao Y, Miyamoto S. Increased plasma levels of adrenomedullin in patients with systemic inflammatory response syndrome. Am J Respir Crit Care Med. 1999;160:132–136. doi: 10.1164/ajrccm.160.1.9810006. [DOI] [PubMed] [Google Scholar]
- Kubo A, Minamino N, Isumi Y, Katafuchi T, Kangawa K, Dohi K, Matsuo H. Production of adrenomedullin in macrophage cell line and peritoneal macrophage. J Biol Chem. 1998;273:16730–16738. doi: 10.1074/jbc.273.27.16730. [DOI] [PubMed] [Google Scholar]
- Poliak S, Mor F, Conlon P, Wong T, Ling N, Rivier J, Vale W, Steinman L. Stress and autoimmunity: the neuropeptides corticotropin-releasing factor and urocortin suppress encephalomyelitis via effects on both the hypothalamic-pituitary-adrenal axis and the immune system. J Immunol. 1997;158:5751–5756. [PubMed] [Google Scholar]
- Agnello D, Bertini R, Sacco S, Meazza C, Villa P, Ghezzi P. Corticosteroid-independent inhibition of tumor necrosis factor production by the neuropeptide urocortin. Am J Physiol Endocrinol Metab. 1998;275:E757–E762. doi: 10.1152/ajpendo.1998.275.5.E757. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Rey E, Fernandez-Martin A, Chorny A, Delgado M: Therapeutic effect of urocortin and adrenomedullin in a murine model of Crohn’s disease. DOI: 10.1136/gut.2005.084525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzaki E, Charalampopoulos I, Leontidis C, Mouzas IA, Tzardi M, Tsatsanis C, Margioris AN, Gravanis A. Urocortin in human gastric mucosa: relationship to inflammatory activity. J Clin Endocrinol Metab. 2003;88:478–483. doi: 10.1210/jc.2002-020853. [DOI] [PubMed] [Google Scholar]
- Wong LY, Cheung BM, Li YY, Tang F. Adrenomedullin is both proinflammatory and antiinflammatory: its effects on gene expression and secretion of cytokines and macrophage migration inhibitory factor in NR8383 macrophage cell line. Endocrinology. 2005;146:1321–1327. doi: 10.1210/en.2004-1080. [DOI] [PubMed] [Google Scholar]
- Isumi Y, Kubo A, Katafuchi T, Kangawa K, Minanmino N. Adrenomedullin suppresses interleukin-1beta-induced tumor necrosis factor-alpha production in Swiss 3T3 cells. FEBS Lett. 1999;463:110–114. doi: 10.1016/s0014-5793(99)01615-4. [DOI] [PubMed] [Google Scholar]
- Howard M, Muchamuel T, Andrade S, Menon S. Interleukin 10 protects mice from lethal endotoxemia. J Exp Med. 1993;77:1205–1208. doi: 10.1084/jem.177.4.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhainaut J, Marin N, Mignon A, Vinsonneau C. Hepatic response to sepsis: interaction between coagulation and inflammatory processes. Crit Care Med. 2001;29:S42–S47. doi: 10.1097/00003246-200107001-00016. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Rey E, Chorny A, Robledo G, Delgado M. Cortistatin, a new anti-inflammatory peptide with therapeutic effect on lethal endotoxemia. J Exp Med. 2006;203:563–571. doi: 10.1084/jem.20052017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalm VA. Cortistatin rather than somatostatin as a potential endogenous ligand for somatostatin receptors in the human immune system. J Clin Endocrinol Metab. 2003;88:270–276. doi: 10.1210/jc.2002-020950. [DOI] [PubMed] [Google Scholar]
- Nanke Y, Katake S, Yonemoto K, Saito S, Tomatsu T, Kamatani N. Adrenomedullin in synovial fluids from patients with rheumatoid arthritis inhibits interleukin 6 production from synoviocytes. Ann Rheum Dis. 2003;62:82–83. doi: 10.1136/ard.62.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S, Zhou M, Fowler DE, Wang P. Mechanisms of the beneficial effect of adrenomedullin and adrenomedullin-binding protein-1 in sepsis: down-regulation of proinflammatory cytokines. Crit Care Med. 2002;30:2729–2735. doi: 10.1097/00003246-200212000-00018. [DOI] [PubMed] [Google Scholar]
- Tracey KJ, Beutler B, Lowry SF, Merryweather J, Wolpe S, Milsark IW, Hariri RJ, Fahey TJ, Zentella A, Albert JD. Shock and tissue injury induced by recombinant human cachectin. Science. 1986;234:470–473. doi: 10.1126/science.3764421. [DOI] [PubMed] [Google Scholar]
- Starnes HF, Pearce MK, Tewari A, Yim JH, Zou LC, Abrams JS. Anti-IL-6 monoclonal antibodies protect against lethal E. coli infection and lethal tumor necrosis factor-a challenge in mice. J Immunol. 1990;145:4185–4191. [PubMed] [Google Scholar]
- Doherty GM, Lange JR, Langstein HN, Alexander HR, Buresh CM, Norton JA. Evidence for IFN-g as a mediator of the lethality of endotoxin and tumor necrosis factor-a. J Immunol. 1992;149:1666–1670. [PubMed] [Google Scholar]
- Tracey KJ, Fong Y, Hesse DG, Manogue KR, Lee AT, Kuo GC, Lowry SF, Cerami A. Anti-cachectin rTNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987;330:662–664. doi: 10.1038/330662a0. [DOI] [PubMed] [Google Scholar]
- Heinzel FP, Rerko RM, Ling P, Hakimi J, Schoenhaut DS. Interleukin 12 is produced in vivo during endotoxemia and stimulates synthesis of gamma interferon. Infect Immun. 1994;62:4244–4249. doi: 10.1128/iai.62.10.4244-4249.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netea MG, Fantuzzi G, Kullberg BJ, Stuyt RJ, Pulido EJ, McIntyre RC, Jr, Joosten LA, Van der Meer JW, Dinarello CA. Neutralization of IL-18 reduces neutrophil tissue accumulation and protect mice against lethal Escherichia coli and Salmonella typhimurium endotoxemia. J Immunol. 2000;264:2644–2649. doi: 10.4049/jimmunol.164.5.2644. [DOI] [PubMed] [Google Scholar]
- Oberholzer A, Oberholzer C, Moldawer LL. Interluekin-10: a complex role in the pathogenesis of sepsis syndromes and its potential as an anti-inflammatory drug. Crit Care Med. 2002;30:S58–S63. [PubMed] [Google Scholar]
- Torpy DJ, Webster EL, Zachman EK, Aguilera G, Chrousos GP. Urocortin and inflammation: confounding effects of hypotension on measures of inflammation. Neuroimmunomodulation. 1999;6:182–186. doi: 10.1159/000026380. [DOI] [PubMed] [Google Scholar]
- Shindo R, Kurihara H, Maemura K, Kurihara Y, Kuwaki T, Izumida T, Minamino N, Ju K-H, Morita H, Oh-hashi Y, Kumada M, Kangawa K, Nagai R, Tazaki Y. Hypotension and resistance of lipopolysaccharide-induced shock in transgenic mice overexpressing adrenomedullin in their vasculature. Circulation. 2000;101:2309–2316. doi: 10.1161/01.cir.101.19.2309. [DOI] [PubMed] [Google Scholar]
- Westphal M, Stubbe H, Bone H-G, Daudel F, Vocke S, Van Aken H, Booke M. Hemodynamic effects of exogenous adrenomedullin in healthy and endotoxemic sheep. Biochem Biophys Res Commun. 2002;296:134–138. doi: 10.1016/s0006-291x(02)00821-5. [DOI] [PubMed] [Google Scholar]
- Yokotani K, Murakami Y, Okada S, Hirata M. Role of grain arachidonic acid cascade on central CRF1 receptor-mediated activation of sympatho-adrenomedullary outflow in rats. Eur J Pharmacol. 2001;419:183–189. doi: 10.1016/s0014-2999(01)00987-6. [DOI] [PubMed] [Google Scholar]
- Nicholls MG, Lainchbury JG, Lewis LK, McGregor DO, Richards AM, Troughton RW, Yandle TG. Bioactivity of adrenomedullin and proadrenomedullin N-terminal 20 peptide in man. Peptides. 2001;22:1745–1752. doi: 10.1016/s0196-9781(01)00508-3. [DOI] [PubMed] [Google Scholar]
- Correa SG, Riera CM, Spiess J, Bianco ID. Modulation of the inflammatory response by corticotropin-releasing factor. Eur J Pharmacol. 1997;319:85–90. doi: 10.1016/s0014-2999(96)00824-2. [DOI] [PubMed] [Google Scholar]
- Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332:1351–1362. doi: 10.1056/NEJM199505183322008. [DOI] [PubMed] [Google Scholar]
- Boehme SA, Gaur A, Crowe PD, Liu XJ, Tamraz S, Wong T, Pahuja A, Ling N, Vale W, De Souza EB, Conlon PJ. Immunosuppressive phenotype of corticotropin-releasing factor transgenic mice is reversed by adrenalectomy. Cell Immunol. 1997;176:103–112. doi: 10.1006/cimm.1997.1080. [DOI] [PubMed] [Google Scholar]
- Agelaki S, Tsatsanis C, Gravanis A, Margioris AN. Corticotropin-releasing hormone augments proinflammatory cytokine production from macrophages in vitro and in lipopolysaccharide-induced endotoxin shock in mice. Infect Immun. 2002;70:6068–6074. doi: 10.1128/IAI.70.11.6068-6074.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venihaki M, Dikkes P, Carrigan A, Karalis KP. Corticotropin-releasing hormone regulates IL-6 expression during inflammation. J Clin Invest. 2001;108:1159–1166. doi: 10.1172/JCI12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Fleur SE, Wick EC, Idumalla PS, Gray EF, Bhargava A. Role of peripheral corticotropin-releasing factor and urocortin II in intestinal inflammation and motility in terminal ileum. Proc Natl Acad Sci USA. 2005;102:7647–7652. doi: 10.1073/pnas.0408531102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnalich F, Hernanz A, Jimenez M, Lopez J, Tato E, Vazquez JJ, Montiel C. Relationship between circulating levels of calcitonin gene-related peptide, nitric oxide metabolites and hemodynamic changes in human septic shock. Regul Pept. 1996;65:115–121. doi: 10.1016/0167-0115(96)00080-8. [DOI] [PubMed] [Google Scholar]
- Monneret G, Pachot A, Laroche B, Picollet J, Bienvenu J. Procalcitonin and calcitonin-related peptide decrease LPS-induced TNF production by human circulating blood cells. Cytokine. 2000;12:762–764. doi: 10.1006/cyto.1999.0607. [DOI] [PubMed] [Google Scholar]
- Huttemeier PC, Ritter EF, Benveniste H. Calcitonin gene-related peptide mediates hypotension and tachycardia in endotoxic rats. Am J Physiol. 1993;265:H767–H769. doi: 10.1152/ajpheart.1993.265.2.H767. [DOI] [PubMed] [Google Scholar]