Abstract
Ambruticins are a family of polyketides. The antifungal activity of an ambruticin, KOSN-2079, was tested in the mouse model of invasive aspergillosis. KOSN-2079 significantly reduced pulmonary fungal burdens and improved survival over that with the vehicle control. These results support the continued development of ambruticins as antifungal agents.
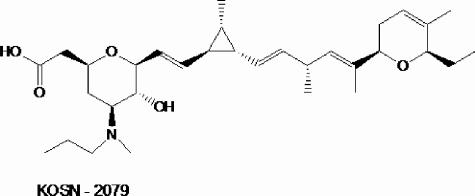
The ambruticins are a family of polyketides that are produced from the soil myxobacterium Sorangium cellulosum. They were first discovered in the 1970s (4), and the VS structural class was discovered in the 1990s (2). Ambruticins exert their antifungal effects through activation of the osmolarity response (3), mediated through activation of the HOG pathway (L. Katz, unpublished results), leading to the overproduction of intracellular glycerol, which results in the influx of water, swelling of the cells, and ultimate cessation of growth. One group of ambruticins had modest activity against Aspergillus species in vitro but was not tested on animals. We made a series of analogs of the VS series and tested their activities against a variety of fungi (Z.-Q. Tian et al., manuscript in preparation). One of the more potent compounds, (5-N)-isopropylambruticin VS4, designated KOSN-2079 (Fig. 1), a derivative of the natural product ambruticin VS4, was used in the studies reported here.
FIG. 1.
Structure of KOSN-2079.
Aspergillus fumigatus strain Af293, a clinical isolate, was generously provided by P. T. Magee (University of Minnesota). Strain 204305, also a clinical isolate, was obtained from the American Type Culture Collection (Manassas, Va.). The strains were grown on Sabouraud dextrose agar plates for 10 days at 37°C. Conidia were harvested by flooding the plates with sterile phosphate-buffered saline containing 0.2% (vol/vol) Tween 80 (Sigma-Aldrich, St. Louis, Mo.), concentrated by centrifugation, and enumerated using a hemacytometer. The susceptibilities of these strains to KOSN-2079 and amphotericin B were determined using the Clinical and Laboratory Standards Institute (formerly NCCLS) protocol M-38A (1). The MIC of each drug was defined as the concentration that resulted in a >90% reduction in turbidity (determined with a spectrophotometer) after a 48-h incubation relative to the turbidity of the untreated control. To test the effects of serum on the antifungal activities of the drugs, the susceptibility assays were also performed in RPMI 1640 medium supplemented with 10% mouse serum. All assays were performed at least twice.
Mice in an inhalation chamber were infected with A. fumigatus as previously described (5). Briefly, male BALB/c mice (National Cancer Institute, Bethesda, Md.) were immunosuppressed with cyclophosphamide, 250 mg/kg of body weight administered intraperitoneally on day −2 (relative to infection) and 200 mg/kg on day +3. They also received cortisone acetate, 250 mg/kg subcutaneously, on both days. While the mice were neutropenic, they received ceftazidime, 5 mg/day subcutaneously, to prevent bacterial infection. The mice were infected with A. fumigatus Af293 by being placed for 1 h in an inhalational chamber in which 1.2 × 1010 conidia were aerosolized. The inoculum received by the mice was confirmed by sacrificing three mice immediately after removal from the chamber and quantitatively culturing their lungs. The median inoculum was 3,350 organisms per mouse (interquartile range, 2,550 to 4,825). Each animal experiment was performed once and was approved by the institutional animal care and use committee, according to the National Institutes of Health guidelines for animal housing and care.
The antifungal activity of KOSN-2079 was investigated initially using pulmonary fungal burden as the end point. After infection, groups of eight mice were randomly assigned to two different dosing regimens: 40 mg/kg/day and 200 mg/kg/day. KOSN-2079 was dissolved in 12% hydroxypropyl-β-cyclodextrin in phosphate-buffered saline (pH 7.5) and administered by gavage twice a day. A group of eight infected control mice received the vehicle alone by gavage, and another group received amphotericin B, 3 mg/kg/day, intraperitoneally. Treatment was started on the day after infection and continued for 4 days. One day after the last dose of drug, the mice were sacrificed, and then their lungs were harvested and quantitatively cultured on Sabouraud dextrose agar.
To determine the ability of KOSN-2079 to prolong survival, the mice were infected and then groups of 16 animals received either KOSN-2079 at 200 mg/kg/day, the vehicle alone, or amphotericin B as in the pulmonary fungal burden experiment. The mice were treated for 7 days, starting on the day after infection. They were monitored twice daily for survival for 14 days.
In the absence of serum, KOSN-2079 was active against both strains of A. fumigatus in vitro, with a MIC of 1 μg/ml. However, when 10% serum was added to the medium, the MIC increased fourfold for strain Af293 and eightfold for strain 204305. In contrast, the MIC of amphotericin B was 1 μg/ml for both strains both in the presence and in the absence of serum.
The ability of KOSN-2079 to reduce pulmonary fungal burdens in mice with invasive aspergillosis was determined. Only the highest dose tested caused a significant reduction in fungal burdens (Fig. 2A). The magnitude of this reduction (0.65 log CFU/g) was similar to that for mice treated with amphotericin B (0.51 log CFU/g).
FIG. 2.
Antifungal activity of KOSN-2079 in the mouse model of pulmonary aspergillosis. (A) Groups of eight mice were infected with A. fumigatus strain Af293 and treated with the indicated drugs for 4 days, starting on the day after infection. Pulmonary fungal burdens were determined 1 day after the last dose of drug. Results are medians ± interquartile ranges from one experiment. *, P < 0.001 for comparison to the vehicle control group by the Wilcoxon rank sum test. (B) Survival of mice infected with A. fumigatus and treated with the indicated drugs (16 mice per group) for 7 days, starting on the day after infection. The dose of KOSN-2079 was 200 mg/kg/day, and the dose of amphotericin B was 3 mg/kg/day. *, P < 0.0001 for comparison to the vehicle control group by the log rank test. §, P = 0.02 for comparison to mice treated with KOSN-2079. Abbreviations: 2079, KOSN-2079; Ampho B, amphotericin B.
To verify the antifungal activity of KOSN-2079, we examined its capacity to prolong the survival of mice. Mice treated with high-dose KOSN-2079 had significantly improved survival compared to mice that received the vehicle alone (Fig. 2B). Mice treated with amphotericin B had improved survival compared to mice receiving either the vehicle control or KOSN-2079. The histopathology of the lungs of some of the mice receiving either KOSN-2079 or the vehicle alone that became moribund and were euthanized on day 7 during the survival experiment was determined by an observer who was blinded to the treatment the mice had received. As predicted by the fungal burden studies, the lungs of mice treated with KOSN-2079 contained markedly fewer foci of fungi, and these foci contained fewer organisms, than those of mice receiving the vehicle control. At the termination of the survival experiment (at day 14), we quantitatively cultured the lungs of the surviving mice to determine if they still contained A. fumigatus. The pulmonary fungal burdens of mice treated with KOSN-2079 and of mice treated with amphotericin B were similar (3.2 log CFU/g [interquartile range, 2.7 to 3.4 log CFU/g] for KOSN-2079-treated animals and 3.0 log CFU/g [interquartile range, 2.5 to 3.5 log CFU/g] for amphotericin B-treated animals). Thus, neither drug was able to sterilize the lungs of these mice.
It was noteworthy that during the survival experiment, the mice in the vehicle control and KOSN-2079 groups received cyclodextrin and developed diarrhea during the last 3 days of therapy. The mice treated with amphotericin B did not receive cyclodextrin and had no diarrhea. Cyclodextrin has been reported by others to cause diarrhea in immunocompromised mice (7). It is possible that this diarrhea contributed to the lower survival of the mice treated with KOSN-2079 compared to amphotericin B. All mice receiving the vehicle control succumbed during the experiment, whereas in our previous studies only 60% of untreated mice died of invasive aspergillosis (5). It is probable that the increased mortality of the mice receiving cyclodextrin alone, compared to historical controls, was also due to diarrhea.
This is the first demonstration of the efficacy of an ambruticin in an animal model of invasive pulmonary aspergillosis. Mice treated with KOSN-2079 had both reduced pulmonary fungal burdens and increased survival compared to mice that received the vehicle alone. Although treatment with KOSN-2079 caused reductions in pulmonary fungal burdens similar to those caused by amphotericin B, treatment with KOSN-2079 was less effective at prolonging survival than treatment with amphotericin B. As mentioned above, our results may have underestimated the effect of KOSN-2079 on survival, because some of the deaths among mice treated with this drug were likely caused by diarrhea induced by the vehicle. Alternatively, amphotericin B treatment may have resulted in improved survival for another reason, such as the immunomodulating effects of this drug.
Of note, a considerably higher dose of KOSN-2079 than of amphotericin B was required to reduce pulmonary fungal burdens, even though the two drugs had similar antifungal activities in vitro. Part of this difference in antifungal efficacy may be due to the effects of serum. The in vitro antifungal activity of KOSN-2079 was reduced four- to eightfold in the presence of serum, whereas serum had no effect on the in vitro antifungal activity of amphotericin B. It is unlikely that pharmacokinetic differences contributed to the relatively low specific activity of KOSN-2079, because preliminary pharmacokinetic data indicate that KOSN-2079 has a large volume of distribution and a half-life of approximately 4 h in mice (6). Nonetheless, the data presented here demonstrate that one ambruticin analog has activity against invasive aspergillosis and suggest that additional ambruticin analogs should be explored for the treatment of this disease in humans.
Acknowledgments
We thank Norma Solis, Yasuki Kamai, and Darrin Craig for assistance with the animal studies.
This work was supported in part by federal funds from the National Institute of Allergy and Infectious Diseases under contract N01-AI-30041. L.Y.C. was supported by a postdoctoral fellowship grant from the American Heart Association, Western States Affiliate.
REFERENCES
- 1.Afeltra, J., E. Dannaoui, J. F. Meis, J. L. Rodriguez-Tudela, and P. E. Verweij. 2002. In vitro synergistic interaction between amphotericin B and pentamidine against Scedosporium prolificans. Antimicrob. Agents Chemother. 46:3323-3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Höfle, G., H. Steinmetz, K. Gerth, and H. Reichenbach. 1991. Ambruticins VS: new members of the antifungal ambruticin family from Sorangium cellulosum. Liebigs Ann. Chem. 1991:941-945. [Google Scholar]
- 3.Knauth, P., and H. Reichenbach. 2000. On the mechanism of action of the myxobacterial fungicide ambruticin. J. Antibiot. (Tokyo) 53:1182-1190. [DOI] [PubMed] [Google Scholar]
- 4.Ringel, S. M., R. C. Greenough, S. Roemer, D. Connor, A. L. Gutt, B. Blair, G. Kanter, and von Strandtmann. 1977. Ambruticin (W7783), a new antifungal antibiotic. J. Antibiot. (Tokyo) 30:371-375. [DOI] [PubMed] [Google Scholar]
- 5.Sheppard, D. C., G. Rieg, L. Y. Chiang, S. G. Filler, J. E. Edwards, Jr., and A. S. Ibrahim. 2004. Novel inhalational murine model of invasive pulmonary aspergillosis. Antimicrob. Agents Chemother. 48:1908-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shubitz, L. F., J. N. Galgiani, Z.-Q. Tian, Z. Zhong, P. Timmermans, and L. Katz. 2006. Efficacy of ambruticin analogs in a murine model of coccidioidomycosis. Antimicrob. Agents Chemother. 50:3467-3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun, Q. N., L. K. Najvar, R. Bocanegra, D. Loebenberg, and J. R. Graybill. 2002. In vivo activity of posaconazole against Mucor spp. in an immunosuppressed-mouse model. Antimicrob. Agents Chemother. 46:2310-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]