Since the beginning of the 1990s, the number of human cases of plague has been rising, and outbreaks are reappearing in various countries after decades of quiescence. Plague is therefore categorized as a reemerging disease. Until recently, Yersinia pestis was considered as uniformly susceptible to agents that are active against gram-negative bacteria. The isolation in Madagascar of two multidrug-resistant strains of Y. pestis, one resistant to all of the antimicrobial agents recommended for treatment and prophylaxis of plague and the other resistant to a smaller array of drugs, is worrisome. The demonstration that horizontal gene transfer in the flea midgut may be the source of antibiotic-resistant Y. pestis strains is of great concern and indicates that such a clinically ominous event may occur again. There is also concern that a biological attack with Y. pestis might employ a natural or engineered antimicrobial-resistant strain. Surveillance of antibiotic resistance in Y. pestis should therefore become systematic worldwide.
BRIEF OVERVIEW OF PLAGUE
Plague is a zoonosis that primarily affects rodents, but several animal species such as cats, rabbits, camels, and humans can also be infected. Sporadically or periodically, explosive outbreaks occur among populations of susceptible rodents. The disease is transmitted from rodent to rodent via flea bites. In nature, the maintenance of plague is absolutely dependent upon cyclic transmission between fleas and mammals. Rodent-to-human transmission most commonly occurs by infected fleas of peridomestic animals (rats, cats) or wild rodents, thus causing bubonic plague, the most common form of the disease. Clinically, bubonic plague is characterized by the appearance of a tender and swollen lymph node, the bubo. In most cases, the bacterium disseminates via the lymphatic and blood vessels to the spleen and the liver and causes a rapidly fatal septicemia. In the absence of adequate treatment, the mortality rate of bubonic plague ranges from 40 to 70%. Human-to-human transmission can occur, either through the bite of the so-called human flea, Pulex irritans (bubonic plague), or respiratory droplets, causing an overwhelming infection called pneumonic plague. The pneumonic plague would be the form most likely implicated in the event of a bioterrorism attack. Without early and effective antimicrobial therapy, the outcome of pneumonic plague is invariably fatal, usually less than 3 days (19).
PLAGUE TODAY
Despite a significant reduction in the morbidity and mortality of plague infections during the 20th century, the disease has not been eradicated. Nowadays, endemic plague foci persist in many countries in Africa; the former Soviet Union; the Americas, including the southwestern United States; and parts of Asia. Over the last documented 15-year period, 38,310 human plague cases and 2,845 deaths have been reported to the World Health Organization by 25 countries (28). No plague cases have been recently reported in Europe or Oceania. The worldwide numbers are most likely underestimated because of unrecognized cases and the failure of countries to report plague cases. During the last 10 years, at least three geographical areas experienced outbreaks of human plague after silent periods of 30 to 50 years: India in 1994, Zambia in 1996, Indonesia in 1997, and Algeria in 2003 (28). These features have led to categorization of plague as a reemerging disease (22). The reasons for the recent and worldwide reemergence of plague are not clear but may be partly attributable to a global falling off of surveillance (9). The epidemiology of plague resulting from a bioterrorism attack would be different from that of natural outbreaks, the microorganism being most likely released as an aerosol and in large amounts.
PLAGUE TREATMENT
The use of antimicrobial agents for the treatment of plague started in 1938 with sulfonamide and in 1946 with streptomycin (19). These therapies led to a dramatic drop in human mortality. Today, the worldwide fatality rate attributable to plague has fallen to less than 8%. Classically, Y. pestis isolates are uniformly susceptible to all antimicrobial agents active against gram-negative bacteria (10, 11, 15, 20, 24). The three main antimicrobial agents recommended to treat plague are streptomycin, tetracycline, and chloramphenicol (1). Streptomycin remains the drug of choice, whereas chloramphenicol is most often restricted to the treatment of meningitis. However, due to the limited availability of streptomycin in some countries, gentamicin has been used as a substitute, and it was determined that gentamicin alone or in combination with a tetracycline could effectively treat human plague (4). Based on in vitro data (10, 11, 15) and murine models (5, 25) in which their efficacy was demonstrated to be similar to that of aminoglycosides, fluoroquinolones represent an important alternative for plague therapy. However, with the exception of a single reported case of plague successfully treated with ciprofloxacin (18), there are no data concerning the efficacy of that drug as a prophylactic agent on a large scale. Administration of mono-, bi-, or tritherapies depends on the severity of the symptoms. The chances of a patient's survival are directly linked to the precocity of antibiotic treatment, especially in the more severe pneumonic and septicemic forms.
Prophylactic therapy consists of the administration of sulfonamide, trimethoprim-sulfamethoxazole, or tetracycline. Prophylactic drugs are administered to close contacts of pneumonic plague patients or to relatives of bubonic plague patients living in the same house or in the neighborhood.
In the case of an aerosolized plague weapon, the United States Working Group of Civilian Biodefense recommended streptomycin or gentamicin as the preferred choice in a contained casualty setting (i.e., modest numbers of patients requiring treatment), with doxycycline, ciprofloxacin, or chloramphenicol as alternative choices. For a mass casualty situation, oral therapy with doxycycline, tetracycline, or ciprofloxacin has been recommended (16). Prevention of human-to-human transmission from patients with plague pneumonia can be achieved by implementing standard isolation procedures until at least 4 days after the initiation of antibiotic treatment (3).
Although cephalosporins have been sometimes considered as ineffective in the treatment of human plague (8, 17), this inefficacy has never been documented. Furthermore, this antimicrobial agent demonstrated an efficacy against Y. pestis similar to that of fluoroquinolones and aminoglycosides in in vitro tests (10, 15, 24) and murine models (2, 5).
CHARACTERISTICS OF THE ANTIBIOTIC-RESISTANT STRAINS
In 1995, high-level resistance to antimicrobial agents, including to all of the drugs recommended for plague prophylaxis and therapy, was observed in a clinical isolate of Y. pestis (12). This strain (17/95) was isolated in the Ambalavao district of Madagascar from a 16-year-old male presenting with symptoms of bubonic plague. The second strain (16/95) (13) with high-level resistance to streptomycin was isolated the same year in the Ampitana district of Madagascar. This isolate was obtained from a 14-year-old patient presenting with bubonic plague. Both patients recovered after antibiotic therapy consisting of intramuscular injections of streptomycin (2 g per day for 4 days) and oral administration of trimethoprim-sulfamethoxazole (2 g per day for 10 days).
Yersinia pestis 17/95.
Strain 17/95 exhibited high-level resistance to eight antimicrobial agents, including not only those recommended for therapy (streptomycin, chloramphenicol, and tetracycline) and prophylaxis (sulfonamide and tetracycline) of plague but also drugs that may have represented alternatives to classical therapy, such as ampicillin, kanamycin, and spectinomycin. Resistance to ampicillin, chloramphenicol, kanamycin, sulfonamide, and streptomycin-spectinomycin was due to the production of a TEM-1 penicillinase (blaTEM-1), a type I chloramphenicol acetyltransferase (catI), a type I 3′-O-aminoglycoside phosphotransferase [aph(3′)-I], a drug-resistant dihydropteroate synthase (sul1), and a 3"-9-O-aminoglycoside adenylyltransferase (ant3"9), respectively. Resistance to tetracycline was by efflux [tet(D)]. The isolate remained susceptible to cephalosporins, other aminoglycosides, quinolones, and trimethoprim. Most likely, the activity of trimethoprim, despite lack of synergism with sulfonamide, accounted for the patient's recovery.
All of the resistance genes were carried by a conjugative plasmid of approximately 150 kb, designated pIP1202. The entire nucleotide sequence of this plasmid is currently being determined (http://www.tigr.org/tdb/mdb/mdbinprogress.html) and should be released soon. Plasmid pIP1202 could be transferred by conjugation from Y. pestis 17/95 to Y. pestis and Escherichia coli at frequencies of approximately 1 × 10−2 per donor CFU. Retransfer of pIP1202 from E. coli to Y. pestis and to E. coli occurred at frequencies of 1.1 × 10−4 and 5.7 × 10−5, respectively (12). The lower frequency of transfer of this replicon from E. coli to other enterobacterial strains was attributable to a low stability of pIP1202 in E. coli. Plasmid pIP1202 belonged to incompatibility group Inc6-C and contained a structure similar to that of integrons of Tn21-like elements (12).
Several observations, such as the spontaneous loss en bloc of some resistant determinants and the presence of a segment conserved in integrons of Tn21-like elements that are carried by large conjugative plasmids, strongly argue for an origin of pIP1202 in a member of the Enterobacteriaceae family. The resistance genes carried were closely related in structure to plasmid-borne determinants found commonly in enterobacteria. The Inc6-C origin of replication of pIP1202 was typical of plasmids of this group of bacteria with a broad range of hosts, and the plasmid was easily transferred in vitro from E. coli to Y. pestis (12).
Yersinia pestis 16/95.
Strain 16/95 was resistant to streptomycin but remained susceptible to spectinomycin and other antimicrobial agents, including those recommended for plague therapy and prophylaxis. The MICs of streptomycin and spectinomycin for this strain were 1,024 and 16 mg/liter, respectively (13).
The resistance genes were carried by a plasmid of approximately 40 kb, pIP1203, that could conjugate to other Y. pestis isolates. Transfer of streptomycin resistance from Y. pestis 16/95 occurred at high frequencies (3 × 10−1 per donor CFU) to Y. pestis and Yersinia pseudotuberculosis and at lower frequencies to E. coli; transfer to Yersinia enterocolitica was not detected. Retransfer of pIP1203 from Y. pestis and Y. pseudotuberculosis transconjugants to Y. pestis and Y. pseudotuberculosis also occurred at high frequencies (3 × 10−2) (13).
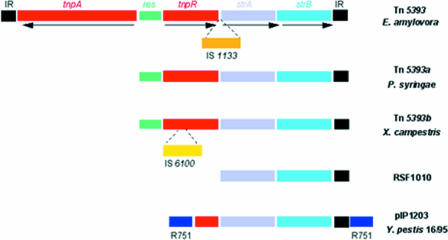
High-level resistance was due to the presence of the strA and strB genes that encode aminoglycoside 3"-O- and 6-O-phosphotransferase activities, respectively (23). The str genes were originally described in the small, nonconjugative, broad-host-range IncQ plasmid RSF1010 (21). They have been subsequently found as part of transposon Tn5393 and related elements in Erwinia amylovora, Pseudomonas syringae pv. papulans, and Xanthomonas campestris pv. vesicatoria (7, 26). An 81-bp sequence identical to the inverted terminal repeat (IR) of Tn5393 was identified downstream from pIP1203 strA-strB genes (Fig. 1). This IR is always present at the same position in the various genetic structures that carry the str genes. Upstream from strA, the sequence was identical to a portion of the tnpR resolvase repressor gene of Tn5393, and the identity was interrupted within the 3′ end of tnpR (Fig. 1). The streptomycin resistance genes in pIP1203 are part of the tnpR-strA-strB-IR cluster characteristic of the Tn5393 group of transposons (7, 26). This portion of the element is inserted in R751, a broad-host-range plasmid belonging to the IncP group (Fig. 1). The sequences flanking the tnpR-strA-strB-IR region in pIP1203 are separated by approximately 6 kb in the original R751 backbone (27). This organization suggests that insertion of a Tn5393-like element was associated with concomitant (or subsequent) loss of a region involved in the control of plasmid stability. Despite this deletion, pIP1203 appears to be highly stable in both Y. pestis and E. coli.
FIG. 1.
Genetic organization of the streptomycin resistance genes. Schematic representation of the regions of transposons Tn5393 and derivatives and of plasmids RSF1010 and pIP1203 carrying the strA and strB genes. IR, inverted repeat; tnpA, transposase; res, resolution site; tnpR, resolvase; IS1133 and IS6100, insertion sequences; R751, portions of plasmid R751. Arrows indicate direction of transcription.
The two resistant strains differ in several aspects. (i) They were isolated in two districts of Madagascar that are 80 miles apart. (ii) Strain 17/95 is of the typical ribotype B, whereas strain 16/95 is of the newly described, Madagascar-specific, ribotype Q (14). (iii) Plasmid pIP1202 carries multiple antimicrobial agent resistance genes, belongs to the Inc6-C group, and is 150 kb in size, whereas pIP1203 carries only streptomycin resistance determinants, belongs to the IncP group, and is 40 kb in size. (iv) Finally, streptomycin resistance is due to adenylylation of the drug in strain 17/95 and to phosphorylation in strain 16/95. These data indicate that the two antibiotic-resistant Y. pestis strains arose independently.
SOURCE OF ANTIBIOTIC-RESISTANT Y. PESTIS
The genesis of the two antibiotic-resistant Y. pestis strains cannot be determined retrospectively, but it has been speculated that the initial conjugative transfers occurred in a rat or a human (6, 8, 12, 13). Y. pestis is an obligate parasite that alternates between mammals (principally rodents) and fleas; its life cycle does not include a free-living stage. In the mammal, Y. pestis infects the dermis, lymphoid tissue, and blood, sites that are normally sterile. Opportunities for conjugative genetic exchange would be rare, occurring only during simultaneous infections with Y. pestis and another invasive bacterium, and then only if close contact between donor and recipient were subsequently established. In contrast, in the nonsterile digestive tract of its flea vector Y. pestis forms dense aggregates to produce a transmissible infection (16).
This was recently confirmed by feeding Xenopsylla cheopis, the principal vector of plague in Madagascar, on blood containing E. coli (pIP1203). Five to 7 days after the first infectious blood meal, the same fleas were secondarily infected with a streptomycin-sensitive, nonvirulent Y. pestis strain (12). Unrelated coinfecting bacteria in the flea midgut are readily incorporated into the aggregates, and this close physical contact favors high-frequency conjugative genetic exchange. Transfer of the antimicrobial agent resistance plasmid pIP1203 from E. coli to Y. pestis occurred in the flea midgut at a frequency of 1 × 10−3 after only 3 days of coinfection, a value close to the conjugation frequency of 6 × 10−2 between E. coli and Y. pestis observed in vitro under optimal filter-mating conditions (13). After 4 weeks, 95% of fleas carried Y. pestis that had acquired the streptomycin-resistant plasmid pIP1203. Thus, transit in its arthropod vector exposes Y. pestis to favorable conditions for efficient genetic exchange with microbial flora of the flea gut. Horizontal gene transfer in the flea may be the source of antibiotic-resistant Y. pestis strains isolated from plague patients in Madagascar (16).
CONCLUSIONS
Since the date of their discovery, a careful surveillance of all Y. pestis isolates from humans, rats, and fleas has been performed, and no other specimen of these two isolates could be found locally or in other parts of Madagascar (6). During the 3 following years (1996 to 1998), singly resistant strains were found in the Mahajanga harbor (one each of ampicillin-resistant and chloramphenicol-resistant clinical isolate) and in the capital, Antananarivo (one tetracycline-resistant rat isolate and two ampicillin-resistant flea isolates) (6).
The separate appearance of two distinct strains of antibiotic-resistant Y. pestis during the current outbreak in Madagascar suggests that conjugative tranfer of antimicrobial agent resistance plasmids to Y. pestis in its natural environment is not an isolated phenomenon. The potential for continued emergence and dissemination to other parts of the world of Y. pestis strains that have acquired antimicrobial agent resistance genes or other new virulence factors poses a global threat to public health.
REFERENCES
- 1.Bames, A. M., and T. J. Quan. 1992. Plague, p 1285-1291. In S. L. Gorbach, J. G. Bartlett, and N. R. Blacklow (ed.), Infectious diseases. W. B. Saunders Company. Philadelphia, Pa.
- 2.Bonacorsi, S. P., M. R. Scavizzi, A. Guiyoule, J. H. Amouroux, and E. Carniel. 1994. Assessment of a fluoroquinolone, three β-lactams, two aminoglycosides, and a cycline in treatment of murine Yersinia pestis infection. Antimicrob. Agents Chemother. 38:481-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bossi, P., A. Tegnell, A. Baka, F. Van Loock, J. Hendriks, A. Werner, H. Maidhof, and G. Gouvras. December. 2004. Bichat guidelines for the clinical management of plague and bioterrorism-related plague. Euro. Surveill. 9:12. [Online.] http://www.eurosurveillance.org/em/v09n12/0912-232.asp [DOI] [PubMed] [Google Scholar]
- 4.Boulanger, L. L., P. Ettestad, J. D. Fogarty, D. T. Dennis, D. Romig, and G. Mertz. 2004. Gentamicin and tetracyclines for the treatment of human plague: review of 75 cases in New Mexico, 1985-1999. Clin. Infect. Dis. 38:663-669. [DOI] [PubMed] [Google Scholar]
- 5.Byrne, W. R., S. L. Welkos, M. L. Pitt, K. J. Davis, R. P. Brueckner, J. W. Ezzell, G. O. Nelson, J. R. Vaccaro, L. C. Battersby, and A. M. Friedlander. 1998. Antibiotic treatment of experimental pneumonic plague in mice. Antimicrob. Agents Chemother. 42:675-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chanteau, S., M. Ratsitorahina, L. Rahalison, B. Rasoamanana, F. Chan, P. Boisier, D. Rabeson, and J. Roux. 2000. Current epidemiology of human plague in Madagascar. Microbes Infect. 2:25-31. [DOI] [PubMed] [Google Scholar]
- 7.Chiou, C.-S., and A. L. Jones. 1993. Nucleotide sequence analysis of a transposon (Tn5393) carrying streptomycin resistance genes in Erwinia amylovora and other gram-negative bacteria. J. Bacteriol. 175:732-740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dennis, D. T. 1997. Multidrug resistance in plague. N. Engl. J. Med. 337:702-704. [DOI] [PubMed] [Google Scholar]
- 9.Duplantier, J.-M., J.-B. Duchemin, S. Chanteau, and E. Carniel. 2005. From the recent lessons of the Malagasy foci towards a global understanding of the factors involved in plague reemergence. Vet. Res. 36:437-453. [DOI] [PubMed] [Google Scholar]
- 10.Frean, J. A., L. Arntzen, T. Capper, A. Bryskier, and K. P. Klugman. 1996. In vitro activities of 14 antibiotics against 100 human isolates of Yersinia pestis from a southern African plague focus. Antimicrob. Agents Chemother. 40:2646-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frean, J., K. P. Klugman, L. Arntzen, and S. Bukofzer. 2003. Susceptibility of Yersinia pestis to novel and conventional antimicrobial agents. J. Antimicrob. Chemother. 52:294-296. [DOI] [PubMed] [Google Scholar]
- 12.Galimand, M., A. Guiyoule, G. Gerbaud, B. Rasoamanana, S. Chanteau, E. Carniel, and P. Courvalin. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337:677-680. [DOI] [PubMed] [Google Scholar]
- 13.Guiyoule, A., G. Gerbaud, C. Buchrieser, M. Galimand, L. Rahalison, S. Chanteau, P. Courvalin, and E. Carniel. 2001. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg. Infect. Dis. 7:43-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guiyoule, A., B. Rasoamanana, C. Buchrieser, P. Michel, S. Chanteau, and E. Carniel. 1997. Recent emergence of new variants of Yersinia pestis in Madagascar. J. Clin. Microbiol. 35:2826-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hernandez, E., M. Girardet, F. Ramisse, D. Vidal, and J.-D. Cavallo. 2003. Antibiotic susceptibilities of 64 isolates of Yersinia pestis to 24 antimicrobial agents. J. Antimicrob. Chemother. 52:1029-1031. [DOI] [PubMed] [Google Scholar]
- 16.Hinnebusch, B. J., M.-L. Rosso, T. G. Schawn, and E. Carniel. 2002. High-frequency conjugative transfer of antibiotic resistance genes to Yersinia pestis in the flea midgut. Mol. Microbiol. 46:349-354. [DOI] [PubMed] [Google Scholar]
- 17.Inglesby, T. V., D. T. Dennis, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, J. F. Koerner, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, M. Schoch-Spana, K. Tonat, et al. 2000. Plague as a biological weapon: medical and public health management. JAMA 283:2281-2290. [DOI] [PubMed] [Google Scholar]
- 18.Kuberski, T., L. Robinson, and A. Schurgin. 2003. A case of plague successfully treated with ciprofloxacin and sympathetic blockade for treatment of gangrene. Clin. Infect. Dis. 36:521-523. [DOI] [PubMed] [Google Scholar]
- 19.Pollitzer, R. 1954. Plague. WHO Monograph Series 22. World Health Organization, Geneva, Switzerland.
- 20.Rasoamanana, B., F. Leroy, C. Raharimanana, and S. Chanteau. 1995. Surveillance de la sensibilité aux antibiotiques des souches de Yersinia pestis à Madagascar de 1989 à 1995. Arch. Inst. Pasteur Madagascar 62:108-110. [Google Scholar]
- 21.Scholz, P., V. Haring, B. Wittmann-Liebold, K. Ashman, M. Bagdasarian, and E. Scherzinger. 1989. Complete nucleotide sequence and gene organization of the broad-host-range plasmid RSF1010. Gene 75:271-288. [DOI] [PubMed] [Google Scholar]
- 22.Schrag, S. J., and P. Wiener. 1995. Emerging infectious diseases: what are the relative roles of ecology and evolution? Trends Evol. Ecol. 10:319-324. [DOI] [PubMed] [Google Scholar]
- 23.Shaw, K. J., P. N. Rather, R. S. Hare, and G. H. Miller. 1993. Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol. Rev. 57:138-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith, M. D., D. X. Vinh, N. T. T. Hoa, J. Wain, D. Thung, and N. J. White. 1995. In vitro antimicrobial susceptibilities of strains of Yersinia pestis. Antimicrob. Agents Chemother. 39:2153-2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steward, J., M. S. Lever, P. Russell, R. J. Beedham, A. J. Stagg, R. R. Taylor, and T. J. G. Brooks. 2004. Efficacy of the latest fluoroquinolones against experimental Yersinia pestis. Int. J. Antimicrob. Agents 24:609-612. [DOI] [PubMed] [Google Scholar]
- 26.Sundin, G. W., and C. L. Bender. 1995. Expression of strA-strB streptomycin resistance genes in Pseudomonas syringae and Xanthomonas campestris and characterization of IS6100 in X. campestris. Appl. Environ. Microbiol. 61:2891-2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorsted, P. B., D. P. Macartney, P. Akhtar, A. S. Haines, N. Ali, P. Davidson, T. Stafford, M. J. Pocklington, W. Pansegrau, B. M. Wilkins, E. Lanka, and C. M. Thomas. 1998. Complete sequence of the IncPβ plasmid R751: implications for evolution and organisation of the IncP backbone. J. Mol. Biol. 282:969-990. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. 2004. Human plague cases from 1989 to 2003. Wkly. Epidemiol. Rec. 79:301-306.15369044 [Google Scholar]