Abstract
Although research on body dysmorphic disorder (BDD) has increased in recent years, this disorder’s comorbidity has received little empirical attention. Further work in this area is needed, as it appears that most patients with BDD have at least one comorbid disorder. This study examined axis I comorbidity and clinical correlates of comorbidity in 293 patients with DSM-IV BDD, 175 of whom participated in a phenomenology study and 118 of whom participated in treatment studies of BDD. Subjects were evaluated with the Structured Clinical Interview for DSM-III-R (SCID-P) and a semistructured instrument to obtain information on clinical correlates. Comorbidity was common, with a mean of more than two lifetime comorbid axis I disorders in both the phenomenology and treatment groups. In both groups, the most common lifetime comorbid axis I disorders were major depression, social phobia, obsessive compulsive disorder (OCD), and substance use disorders. Social phobia usually began before onset of BDD, whereas depression and substance use disorders typically developed after onset of BDD. A greater number of comorbid disorders was associated with greater functional impairment and morbidity in a number of domains. Thus, axis I comorbidity is common in BDD patients and associated with significant functional impairment.
BODY DYSMORPHIC DISORDER (BDD), also known as dysmorphophobia, is a somatoform disorder characterized by a preoccupation with an imagined or slight defect in appearance that causes significant distress or functional impairment. BDD is relatively common,1,2 frequently results in impairment in psychosocial functioning,3 and is associated with high levels of perceived stress4 and suicide attempts.3,5 Patients with BDD report notably poor mental health-related quality of life.6 Outpatients with BDD have more severe depression and lower Global Assessment of Functioning scores than outpatients without BDD.7
Although BDD has been increasingly researched in recent years, its comorbidity has received little attention. Further examination of this issue is needed, as studies suggest that a majority, and perhaps nearly all, BDD patients have at least one comorbid condition.8–10 In one study, BDD patients were more likely than other psychiatric outpatients to have three or more comorbid axis I disorders.7
Mood and anxiety disorders frequently coexist with BDD (Table 1). In the largest published study of BDD that reported lifetime axis I comorbidity rates (N = 188), 88% of subjects met criteria for a mood disorder and 60% for an anxiety disorder on the Structured Clinical Interview for DSM-III-R (SCID-P).8 The most common lifetime axis I disorders were major depression (82%), social phobia (38%), substance use disorders (36%), and obsessive compulsive disorder (OCD; 30%). As shown in Table 1, other studies, using various assessment methods, have also generally found that these disorders are often comorbid with BDD. Veale et al., however, found low rates of these disorders5 for reasons that are unclear. Axis II disorders also appear relatively common in patients with BDD; reported rates range from 57% to 100%, with avoidant personality disorder most common.5,11–13
Table 1.
Lifetime Axis I Comorbidity Rates (%) in Published Studies of Body Dysmorphic Disorder
| Study | N | Assessment Instrument and Criteria | Major Depression | OCD | Social Phobia | Substance Use Disorder |
|---|---|---|---|---|---|---|
| Hollander et al. (1993)9 | 50 | Clinical interview; DSM-III-R | 68 | 78 | 12 | 22 |
| Veale et al. (1996)5 | 50 | SCID-P; DSM-III-R | 8 | 6 | 16 | 2 |
| Phillips & Diaz (1997)8* | 188 | SCID-P; DSM-III-R | 82 | 30 | 38 | 36 |
| Perugi et al. (1997)10 | 58 | “Semistructured clinical interview”; DSM-III-R | 41 | 41 | 12 | –† |
| Zimmerman & Mattia (1998)7 | 16 | SCID-P; DSM-IV | 69 | 38 | 69 | 6 |
To the best of our knowledge, there are no reports of other aspects of axis I comorbidity in individuals with BDD. No previous study, for example, has examined the number and pattern of comorbid disorders, age of onset of BDD versus that of comorbid conditions, or clinical correlates of comorbidity. In addition, no study has reported the percentage of BDD patients without any comorbid conditions or differences in comorbidity rates between BDD patients who do and do not participate in treatment studies. In this study, we extend our previous work3,8,14 by assessing axis I comorbidity rates in a larger sample (N = 293) and examining these previously unstudied aspects of comorbidity. Due to differences in recruitment procedures, we anticipated that participants in treatment studies would have lower rates of bipolar disorder and substance use disorders than phenomenology study participants. We also hypothesized that subjects with multiple comorbid disorders would have greater functional impairment and a higher number of suicide attempts and psychiatric hospitalizations than subjects with fewer or no comorbid disorders. This hypothesis was based on studies of other psychiatric populations indicating that greater axis I comorbidity is associated with increased suicide attempts and lethality of the attempt,15,16 as well as greater impairment in functioning.17–19
METHOD
Subjects were referred from a variety of sources to a BDD research program for evaluation or treatment of BDD. All participants met DSM-IV criteria for BDD or its delusional variant (a type of delusional disorder, somatic type), which may be double-coded with BDD according to DSM-IV. There were 293 participants: 175 participated in a phenomenology study of BDD’s clinical features,3 31 in an open-label study of fluvoxamine for BDD,20 and 87 in placebo-controlled pharmacotherapy studies of BDD.21 One hundred sixty-one (54.9%) subjects were females; the mean age was 31.3 ± 11.1 years. Written informed consent was obtained from all subjects.
The second author administered the SCID-P for DSM-III-R22,23 to all subjects to assess axis I disorders (a study of axis II disorders from this sample has previously been reported11). Not otherwise specified (NOS) diagnoses were not made because of their subjective nature. Because BDD is not included in the SCID for DSM-III-R, BDD was assessed using a reliable SCID-like semistructured interview based on DSM-IV criteria.24 Diagnoses of Tourette’s syndrome and trichotillomania were based on SCID-like semistructured modules developed to assess DSM-III-R criteria for these disorders. Diagnoses of delusional disorder or psychotic disorder NOS that were entirely attributable to delusional beliefs about appearance were not considered to constitute comorbid disorders.
Participants were also interviewed with a semistructured instrument (Phillips KA, unpublished) to obtain information on variables such as suicide attempts, psychiatric hospitalizations, and demographic characteristics (marital status, current employment status, economic independence, educational attainment, and residential independence [i.e., living independently]). Subjects younger than 19 were excluded from analyses of marital status, employment, economic independence, and residential independence.
Comorbidity and clinical correlate data were analyzed separately for treatment study and phenomenology study participants. This was done because the treatment studies excluded patients with a current substance use disorder, current or lifetime bipolar disorder, current clinically significant suicidality, or current inpatient status. In addition, a placebo-controlled treatment study (n = 74) excluded individuals for whom 13 weeks of placebo treatment was considered excessively risky.21 Compared to subjects in the treatment studies, those in the phenomenology study were more likely to be male (53% v 33%; χ2 = 15.2, df = 1, P = .001) and unmarried (86% v 71%; χ2 = 9.4, df = 1, P = .002). Subjects in the phenomenology group also had greater economic dependence (76% v 52%; χ2 = 14.3, df = 1, P = .001), greater residential dependence (50% v 26%; χ2 = 14.5, df = 1, P = .001), and a higher lifetime rate of psychiatric hospitalization (54% v 22%; χ2 = 26.1, df = 1, P = .001) and suicidal ideation (85% v 73%; χ2 = 5.3, df = 1, P = .02).
Between-group differences were tested using chi-square analysis for categorical variables and two-tailed t tests for continuous variables. Within-group effects for number of comorbid conditions were also tested using chi-square analyses. All missing data were excluded on a pairwise basis for analyses. Given the descriptive and exploratory nature of the analyses, we have reported all tests with significance values greater than 95% (P < .05). However, because of the number of significance tests conducted, caution should be used when interpreting significant results, as some of them, particularly those of only modest significance, may represent chance associations.
RESULTS
Lifetime comorbidity was common (Table 2). Among both phenomenology and treatment study participants, major depression was most frequent, followed by social phobia, OCD, and substance use disorders. Comorbidity rates were generally similar in the phenomenology and treatment groups. The lower rates of bipolar disorder and substance use disorders in the treatment group were expected because of the treatment studies’ exclusion criteria.
Table 2.
Comorbidity Rates in 293 Subjects With DSM-IV Body Dysmorphic Disorder
| Group Difference
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Phenomenology Group (n = 175)
|
Treatment Group* (n = 118)
|
Lifetime
|
Current
|
|||||
| Comorbid Disorder | Lifetime | Current | Lifetime | Current | χ2‡ | P | χ2‡ | P |
| Mood disorders | 157 (90%) | 121 (69%) | 99 (84%) | 64 (54%) | 2.16 | .14 | 4.12 | .04† |
| Major depression | 132 (75%) | 107 (61%) | 92 (78%) | 64 (54%) | 0.25 | .62 | 1.38 | .24 |
| Bipolar disorder | 16 (9%) | 14 (8%) | 0 (0%) | 0 (0%) | 11.42 | .01† | 9.91 | .0† |
| Dysthymia§ | 9 (5%) | — | 10 (9%) | — | 1.29 | .26 | — | — |
| Anxiety disorders | 116 (66%) | 99 (57%) | 71 (60%) | 62 (53%) | 1.14 | .29 | 0.46 | .50 |
| Panic disorder | 21 (12%) | 12 (7%) | 17 (14%) | 8 (7%) | 0.36 | .55 | 0.01 | .98 |
| Agoraphobia | 5 (3%) | 5 (3%) | 4 (3%) | 3 (3%) | 0.07 | .80 | 0.03 | .87 |
| Social phobia | 65 (37%) | 55 (31%) | 42 (36%) | 38 (32%) | 0.07 | .79 | 0.02 | .89 |
| Simple phobia | 13 (7%) | 10 (6%) | 17 (14%) | 14 (12%) | 3.73 | .05 | 3.55 | .06 |
| OCD | 53 (30%) | 43 (25%) | 41 (35%) | 29 (25%) | 0.64 | .42 | 0.01 | .99 |
| Psychotic disorders|| | 1 (.01%) | 1 (.01%) | 0 (0%) | 0 (0%) | 0.68 | .41 | 0.68 | .41 |
| Schizophrenia | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | — | — | — | — |
| Schizoaffective | 1 (.01%) | 1 (.01%) | 0 (0%) | 0 (0%) | 0.68 | .41 | 0.68 | .41 |
| Substance use disorders | 53 (30%) | 22 (13%) | 29 (25%) | 0 (0%) | 1.14 | .29 | 16.04 | .01† |
| Alcohol | 34 (19%) | 12 (7%) | 26 (22%) | 0 (0%) | 0.29 | .59 | 8.44 | .01† |
| Other drugs | 34 (19%) | 12 (7%) | 16 (14%) | 0 (0%) | 3.42 | .18 | 8.44 | .01† |
| Eating disorders | 13 (7%) | 7 (4%) | 16 (14%) | 5 (4%) | 2.97 | .09 | 0.01 | .92 |
| Anorexia | 4 (2%) | 2 (1%) | 5 (4%) | 0 (0%) | 0.90 | .34 | 1.36 | .24 |
| Bulimia | 10 (6%) | 5 (3%) | 13 (11%) | 5 (4%) | 2.74 | .10 | 0.41 | .52 |
| Somatoform disorders§ | 12 (7%) | — | 13 (11%) | — | 1.56 | .67 | — | — |
| Other disorders | ||||||||
| Trichotillomania¶ | — | — | 2 (2%) | 2 (2%) | — | — | — | — |
| Tourette’s syndrome¶ | — | — | 0 (0%) | 0 (0%) | ||||
NOTE. Results are presented as n (%) for each comorbid condition.
BDD patients with a current substance use disorder, current or lifetime bipolar disorder, who were actively suicidal, or were currently an inpatient were excluded from treatment studies.
Significant differences between phenomenology and treatment subjects.
df = 1.
The DSM-III-R SCID does not assess current rates of these disorders.
Delusional disorder and psychotic disorder NOS due to BDD were not considered comorbid conditions.
Trichotillomania and Tourette’s syndrome were not assessed in the phenomenology study.
Phenomenology study participants had 2.4 ± 1.5 lifetime comorbid axis I disorders (range, 0 to 7): 8.6% had no lifetime comorbid conditions, 21.7% had one, 28.6% had two, and 41.4% had three or more. The treatment study subjects had 2.5 ± 1.7 lifetime comorbid axis I disorders (range, 0 to 8): 6.8% had no comorbid conditions, 24.6% had one, 25.4% had two, and 43.2% had three or more. Regarding current comorbidity, the phenomenology study participants had 1.7 ± 1.2 comorbid axis I disorders (range, 0 to 5): 16.0% had no current comorbid axis I disorders, 32.6% had one, 29.7% had two, and 21.7% had three or more. Treatment study subjects had 1.4 ± 1.2 current comorbid axis I disorders (range, 0 to 5): 24.6% had no comorbid conditions, 36.4% had one, 24.6% had two, and 14.4% had three or more.
We also examined patterns of co-occurrence among the most common lifetime comorbid disorders (Fig 1). Co-occurrence of social phobia and major depression was most frequent (32%; n = 94), followed by major depression plus OCD (25%; n = 73). There was also a high rate of co-occurring major depression and substance use disorders (25%; n = 73).
Fig 1.
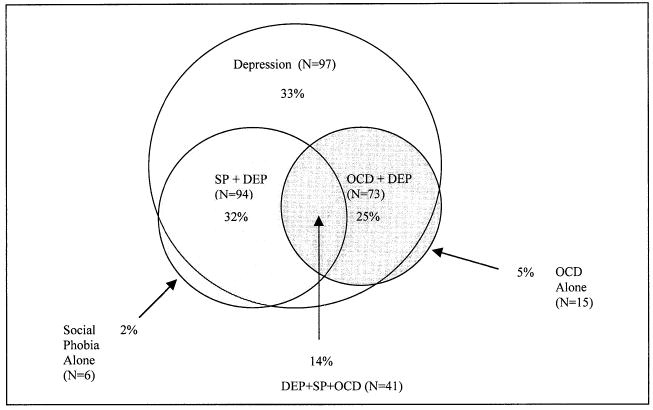
Percentage of 293 BDD patients with various combinations of lifetime depression, social phobia, and OCD. Circle sizes are roughly proportional to patient number with the respective disorder; 16% (n = 47) of BDD patients had comorbid social phobia and OCD without depression.
Age of onset data (Table 3) indicate that a majority of BDD subjects developed major depression and substance use disorders after onset of BDD, whereas a majority developed social phobia before onset of BDD.
Table 3.
Age of Onset of Comorbid Axis I Disorders Versus Body Dysmorphic Disorder
| Disorder | Age of Onset*† | Range | Pre-BDD‡ | Same Year | Post-BDD |
|---|---|---|---|---|---|
| BDD§ | 16.0 ± 6.9 | 4–43 | — | — | — |
| Major depression | 18.5 ± 7.2 | 4–48 | 22.4% | 21.8% | 55.9% |
| Bipolar disorder | 21.2 ± 9.9 | 12–42 | 22.2% | 11.1% | 66.7% |
| Dysthymia | 20.2 ± 8.0 | 10–32 | 27.3% | 18.2% | 54.5% |
| Panic disorder | 20.2 ± 9.3 | 4–42 | 33.3% | 9.5% | 57.1% |
| Agoraphobia | 22.5 ± 9.2 | 11–33 | 25.0% | 25.0% | 50.0% |
| Social phobia | 12.3 ± 5.8 | 4–35 | 60.2% | 18.1% | 21.7% |
| Simple phobia | 15.0 ± 8.7 | 5–42 | 52.6% | 5.3% | 42.1% |
| OCD | 16.8 ± 8.1 | 7–47 | 43.4% | 9.4% | 47.2% |
| Alcohol | 20.0 ± 7.3 | 11–54 | 23.4% | 12.8% | 63.8% |
| Other drugs | 17.4 ± 5.6 | 7–35 | 32.4% | 10.8% | 56.8% |
| Anorexia | 18.0 ± 10.0 | 13–33 | 50.0% | 0.0% | 50.0% |
| Bulimia | 15.1 ± 3.2 | 10–19 | 12.5% | 0.0% | 87.5% |
| Trichotillomania | 11.1 ± 1.0 | 10–12 | 50.0% | 0.0% | 50.0% |
Ages are presented as mean years ± standard deviation.
Given the similar ages of disorder onset in phenomenology and treatment study participants, age of onset data from these groups was combined.
“Pre-BDD”: the percentage of individuals who developed the comorbid disorder at least one year before developing BDD; “same year”: the percentage who developed the comorbid disorder during the same year as developing BDD; “post-BDD”: the percentage who developed the disorder at least one year after developing BDD.
Includes patients diagnosed with BDD or its delusional variant.
For the phenomenology study participants, having three or more lifetime comorbid axis I disorders was associated with a lower likelihood of being currently employed (χ2 = 6.5, df = 1, P = .01), a history of being housebound due to BDD (χ2 = 4.7, df = 1, P = .03), a history of suicidal ideation (χ2 = 4.6, df = 1, P = .03), and a history of BDD-related suicide attempts (χ2 = 4.5, df = 1, P = .03). Having three or more current axis I disorders was associated with a greater likelihood of being unmarried (χ2 = 4.9, df = 1, P = .03), a history of being housebound due to BDD (χ2 = 4.1, df = 1, P = .04), and a history of suicide attempts (χ2 = 4.7, df = 1, P = .03) and BDD-related suicide attempts (χ2 = 5.8, df = 1, P = .02).
Treatment study subjects with three or more lifetime comorbid conditions had lower educational attainment than those with fewer comorbid conditions (χ2 = 4.1, df = 1, P = .04) and a greater likelihood of psychiatric hospitalization (χ2 = 6.3, df = 1, P = .01). Having three or more current comorbid conditions was associated with a greater likelihood of BDD-related suicide attempts (χ2 = 3.9, df = 1, P = .05).
DISCUSSION
This study found that comorbidity is common in BDD patients, both in terms of the percentage of patients with at least one comorbid disorder and the mean number of comorbid disorders. Indeed, comorbidity is the rule rather than the exception, as is the case for many psychiatric disorders.25 While the differing comorbidity rates in our phenomenology and treatment studies were expected, these differences underscore that rates may vary in different samples. It is possible, for example, that comorbidity rates in BDD patients in a dermatology or primary care setting might differ from those in the current study. Also, studies from clinical settings tend to find higher comorbidity rates than studies from nonclinical settings, because having more than one disorder may increase the probability of seeking treatment.26 It is therefore important that comorbidity in BDD be studied in a variety of samples, including the general population. Comorbidity rates may also vary depending on the cohort’s age, as older cohorts will have had more time to pass through the period of risk for developing a mental disorder. BDD patients older than those in this study, for example, might evidence even higher rates of lifetime major depression or alcohol dependence.
The significance and meaning of the high comorbidity rates found in this study are unclear. It is unknown, for example, whether certain disorders have high base rates in the study setting and co-occur with BDD randomly, or whether they co-occur with BDD at greater than chance levels, reflecting a meaningful association.27 Various models have been proposed to explain comorbidity among disorders, such as chance association (random co-occurrence), symptom nonspecificity, and shared etiology/pathophysiology.28 In part based on its high comorbidity with OCD, the concept of shared etiology/pathophysiology with OCD is implied in proposals that BDD be considered an “OCD spectrum disorder”—i.e., related to OCD.29 Indeed, studies indicate that BDD and OCD have many similarities30 and that BDD occurs more frequently in first-degree relatives of OCD probands than control probands.1 However, BDD and OCD also have a number of differences30; in this regard, it is interesting that no BDD subjects in the current study had a history of Tourette’s syndrome, in contrast to the 5% to 10% rate reported for OCD.31 Because of its frequent comorbidity with depression, the question has also been raised of whether BDD is an affective spectrum disorder.32 From a somewhat different perspective, might the high co-occurrence of BDD with depression, social phobia, and OCD reflect a shared broad underlying dimension such as neuroticism, a trait highly characteristic of BDD?11 The very high comorbidity rates of these disorders with BDD in this study and others suggests that their co-occurrence with BDD is not random. However, to establish this, and to clarify their relationship to one another, further prevalence data as well as data from domains other than comorbidity are needed (e.g., family history, course of illness, and pathogenesis).33,34
Regarding age of onset, our finding that major depression usually began after BDD may simply reflect the fact that major depressive disorder typically begins in the mid-20s, whereas BDD usually begins in the early to middle teenage years. An alternative explanation is that major depression may reflect depressive symptoms and demoralization as a secondary complication of BDD. Although it cannot be determined whether one disorder causes another, our clinical impression is that the major depression that so frequently co-occurs with BDD is often due to BDD; however, this does not always appear to be the case. Indeed, in this study major depression preceded onset of BDD in 22% of cases. It is also worth noting that onset of social phobia usually preceded onset of BDD, as would be expected based on social phobia’s usual age of onset. This suggests that in this study, “primary” social phobia was differentiated from the marked social anxiety typically caused by BDD, which would be expected to begin at the time of, or after, onset of BDD. It is sometimes difficult clinically to differentiate primary social phobia from social anxiety secondary to BDD.
Greater comorbidity was associated with greater functional impairment, consistent with findings for other psychiatric disorders.17–19 This association was found primarily for the phenomenology study, which may in part reflect the treatment studies’ exclusion of inpatients, suicidal patients, and patients with a current substance use disorder; substance use disorders are associated with unemployment35 and suicide attempts.36
This study has several limitations. It did not include a control group, making it unclear how specific the findings are to BDD. All participants were assessed by the second author, without use of a consensus process to determine diagnoses. The inclusion of pharmacotherapy study participants may have introduced unknown biases that may have affected comorbidity; indeed, our finding that rates of bipolar disorder and substance related disorders were lower in the treatment sample, while expected, illustrates such a bias. Furthermore, recent findings indicate that depressed patients eligible for treatment trials represent only a subset of individuals with that disorder.37 Such findings encourage caution when generalizing results from treatment studies to clinical settings. In addition, subjects in the present study were obtained from a setting that specializes in BDD, and it is unclear how generalizable the results are to nonspecialty settings. Additional research is needed to identify possible differences between individuals in different settings.
Despite these limitations, our results, in the largest series of BDD patients to date, converge with previous findings in suggesting that axis I comorbidity is common in patients with BDD. Clinicians need to be mindful of the possible clinical impact of comorbid conditions—for example, their association with greater morbidity and the need to consider comorbidity in treatment planning.38,39 Because little is known about comorbidity in BDD, including implications for course of illness, prognosis, and treatment response, additional research is needed in a variety of settings to increase understanding of this important aspect of illness.
References
- 1.Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang KY, Cullen BAM. The relationship of obsessive-compulsive disorder to possible spectrum disorders: results from a family study. Biol Psychiatry. 2000;48:287–293. doi: 10.1016/s0006-3223(00)00831-3. [DOI] [PubMed] [Google Scholar]
- 2.Mayville S, Katz RC, Gipson MT, Cabral K. Assessing the prevalence of body dysmorphic disorder in an ethnically diverse group of adolescents. J Child Fam Stud. 1999;8:357–362. [Google Scholar]
- 3.Phillips KA, McElroy SL, Keck PE, Pope HG, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry. 1993;150:302–308. doi: 10.1176/ajp.150.2.302. [DOI] [PubMed] [Google Scholar]
- 4.DeMarco L, Li L, Phillips KA, McElroy SL. Perceived stress in body dysmorphic disorder. J Nerv Ment Dis. 1998;186:724–726. doi: 10.1097/00005053-199811000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Veale D, Boocock A, Gournay K, Dryden W, Shah F, Wilson R. Body dysmorphic disorder: a survey of fifty cases. Br J Psychiatry. 1996;169:196–201. doi: 10.1192/bjp.169.2.196. [DOI] [PubMed] [Google Scholar]
- 6.Phillips KA. Quality of life for patients with body dysmorphic disorder. J Nerv Ment Dis. 2000;188:170–175. doi: 10.1097/00005053-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman M, Mattia J. Body dysmorphic disorder in psychiatric outpatients: recognition, prevalence, comorbidity, demographic, and clinical correlates. Compr Psychiatry. 1998;39:265–270. doi: 10.1016/s0010-440x(98)90034-7. [DOI] [PubMed] [Google Scholar]
- 8.Phillips KA, Diaz S. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185:570–577. doi: 10.1097/00005053-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Hollander E, Cohen L, Simeon D. Body dysmorphic disorder. Psychiatr Ann. 1993;23:359–364. [Google Scholar]
- 10.Perugi G, Akiskal H, Giannotti D, Frare F, Di Vaio S, Cassano G. Gender-related differences in body dysmorphic disorder (dysmorphophobia) J Nerv Ment Dis. 1997;185:578–582. doi: 10.1097/00005053-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Phillips KA, McElroy SL. Personality disorders and traits in patients with body dysmorphic disorder. Compr Psychiatry. 2000;41:229–236. doi: 10.1053/comp.2000.7429. [DOI] [PubMed] [Google Scholar]
- 12.Neziroglu F, McKay D, Todaro J, Yaryura-Tobias JA. Effect of cognitive behavior therapy on persons with body dysmorphic disorder and comorbid axis II diagnoses. Behav Ther. 1996;27:67–77. [Google Scholar]
- 13.Cohen L, Kingston P, Bell A, Kwon J, Aronowitz B, Hollander E. Comorbid personality impairment in body dysmorphic disorder. Compr Psychiatry. 2000;41:4–12. doi: 10.1016/s0010-440x(00)90124-x. [DOI] [PubMed] [Google Scholar]
- 14.Phillips KA, McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases. Psychopharmacol Bull. 1994;30:179–186. [PubMed] [Google Scholar]
- 15.Lecrubier Y. The influence of comorbidity on the prevalence of suicidal behavior. Eur Psychiatry. 2001;16:395–399. doi: 10.1016/s0924-9338(01)00596-x. [DOI] [PubMed] [Google Scholar]
- 16.Haw C, Houston K, Tonsend E, Hawton K. Deliberate self-harm in patients with alcohol disorders: characteristics, treatment, and outcome. Crisis. 2001;22:93–101. doi: 10.1027//0227-5910.22.3.93. [DOI] [PubMed] [Google Scholar]
- 17.Wittchen HU, Fuetsch M, Sonntag H, Muller N, Liebowitz M. Disability and quality of life in pure and comorbid social phobia: findings from a controlled study. Eur Psychiatry. 2000;15:46–58. doi: 10.1016/s0924-9338(00)00211-x. [DOI] [PubMed] [Google Scholar]
- 18.Welkowitz LA, Struening EL, Pittman J, Guardino M, Welkowitz J. Obsessive-compulsive disorder and comorbid anxiety problems in a national anxiety screening sample. J Anxiety Disord. 2000;14:471–482. doi: 10.1016/s0887-6185(00)00034-7. [DOI] [PubMed] [Google Scholar]
- 19.Ballenger J, Davidson J, Lecrubier Y, Nutt D, Borkovec T, Rickels K. Consensus statement on generalized anxiety disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. 2001;62:53–58. [PubMed] [Google Scholar]
- 20.Phillips KA, Dwight M, McElroy S. Efficacy and safety of fluvoxamine in body dysmorphic disorder. J Clin Psychiatry. 1998;59:165–171. doi: 10.4088/jcp.v59n0404. [DOI] [PubMed] [Google Scholar]
- 21.Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry. 2002;59:381–388. doi: 10.1001/archpsyc.59.4.381. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Williams JBW, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID): I. History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 23.Williams J, Gibbon M, First M, Spitzer R, Davies M, Borus J. The Structured Clinical Interview for DSM-III-R (SCID): II. Multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 24.Phillips KA, Atala KD, Pope HG. New Research Program and Abstracts, American Psychiatric Association 148th Annual Meeting. Miami, FL: APA; 1995. Diagnostic instruments for body dysmorphic disorder; p. 157. [Google Scholar]
- 25.Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: challenges to the current system and future directions. Ann Rev Psychol. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- 26.Du Fort GG, Newman SC, Bland RC. Psychiatric comorbidity and treatment seeking. Sources of selection bias in the study of clinical populations. J Nerv Ment Dis. 1993;181:467–474. [PubMed] [Google Scholar]
- 27.Krueger R. Psychometric perspectives on comorbidity. Defining Psychopathology in the 21st Century. In: Helzer J, Hudziak J, editors. Washington, DC: American Psychiatric Press; 2002. pp. 41–54. [Google Scholar]
- 28.Lyons M, Tyrer P, Gunderson J, Tohen M. Heuristic models of comorbidity of axis I and axis II disorders. J Personal Disord. 1997;11:260–269. doi: 10.1521/pedi.1997.11.3.260. [DOI] [PubMed] [Google Scholar]
- 29.Hollander E. Introduction. In: Hollander E, editor. Obsessive-Compulsive Related Disorders. Washington, DC: American Psychiatric Press Inc; 1993. pp. 1–16. [Google Scholar]
- 30.Phillips KA, Gunderson CG, Mallya G, McElroy SL, Carter W. A comparison study of body dysmorphic disorder and obsessive compulsive disorder. J Clin Psychiatry. 1998;59:568–575. doi: 10.4088/jcp.v59n1102. [DOI] [PubMed] [Google Scholar]
- 31.Attiullah N, Eisen JL, Rasmussen SA. Clinical features of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:469–491. doi: 10.1016/s0193-953x(05)70175-1. [DOI] [PubMed] [Google Scholar]
- 32.Phillips KA, McElroy SL, Hudson JI, Pope HG. Body dysmorphic disorder: an obsessive-compulsive spectrum disorder, a form of affective spectrum disorder, or both? J Clin Psychiatry. 1995;56:41–51. [PubMed] [Google Scholar]
- 33.Wittchen H. Critical issues in the evaluation of comorbidity of psychiatric disorders. Br J Psychiatry. 1996;168(30 Suppl):9–16. [PubMed] [Google Scholar]
- 34.Phillips KA, Price LH, Greenberg BD, Rasmussen SA. Should DSM’s diagnostic groupings be changed? In: Phillips KA, First MB, Pincus H, editors. Advancing DSM: Dilemmas in Psychiatric Diagnosis. Washington DC: American Psychiatric Publishing; 2003. [Google Scholar]
- 35.Claussen B. Alcohol disorders and re-employment in a 5-year follow-up of long-term unemployed. Addiction. 1999;94:133–138. doi: 10.1046/j.1360-0443.1999.94113310.x. [DOI] [PubMed] [Google Scholar]
- 36.Substance Abuse and Mental Health Services Administration. Statistics Source Book, 1998: Online Version ( www.samhsa.gov/oas/analytic.htm). [Google Scholar]
- 37.Zimmerman M, Mattia J, Posternak M. Are subjects in pharmacological treatment trials of depression representative of patients in routine clinical practice? Am J Psychiatry. 2002;159:469–473. doi: 10.1176/appi.ajp.159.3.469. [DOI] [PubMed] [Google Scholar]
- 38.Clarkin J, Kendall P. Comorbidity and treatment planning: summary and future directions. J Consult Clin Psychol. 1992;60:904–908. [PubMed] [Google Scholar]
- 39.Merikangas KR. Comorbidity and social phobia: evidence from clinical, epidemiologic, and genetic studies. Eur Arch Psychiatry Clin Neurosci. 1995;244:297–303. doi: 10.1007/BF02190407. [DOI] [PubMed] [Google Scholar]


