Abstract
The normal gut flora has been implicated in the pathophysiology of inflammatory bowel disease and there is increased interest in the role that stress can play in gut disease. The chemical stressor dinitrophenol (DNP, uncouples oxidative phosphorylation) was injected into the ileum of laparotomized rats and mitochondria structure, epithelial permeability, and inflammatory cell infiltrate were examined 6 and 24 hours later. Monolayers of human colonic epithelial cells (T84, HT-29) were treated with DNP ± commensal Escherichia coli, followed by assessment of epithelial permeability, bacterial translocation, and chemokine (ie, interleukin-8) synthesis. Delivery of DNP into rat distal ileum resulted in disruption of epithelial mitochondria; similar changes were noted in mildly inflamed ileal resections from patients with Crohn’s disease. Also, DNP-treated ileum displayed increased gut permeability and immune cell recruitment. Subsequent studies revealed deceased barrier function, increased bacterial translocation, increased production of interleukin-8, and enhanced mobilization of the transcription factor AP-1 in the model epithelial cell lines exposed to commensal bacteria (E. coli strains HB101 or C25), but only when the monolayers were pretreated with DNP (0.1 mmol/L). These data suggest that enteric epithelia under metabolic stress perceive a normally innocuous bacterium as threatening, resulting in loss of barrier function, increased penetration of bacteria into the mucosa, and increased chemokine synthesis. Such responses could precipitate an inflammatory episode and contribute to existing enteric inflammatory disorders.
The burden of human chronic gastrointestinal illnesses is immense.1 For example, the inflammatory bowel diseases (IBD, Crohn’s disease and ulcerative colitis) are insidious, debilitating disorders, the incidence of which is increasing.1 The cause of IBD is unknown and there is as yet no cure. Current therapies often rely heavily on corticosteroids—an unacceptable solution given their spectrum of side-effects. Substantial experimental data exist implicating a component(s) of the gut flora as crucial for the development of enteric inflammation. Indeed, the hypothesis has been advanced that IBD is the consequence of an inappropriate immune response against the normal gut microflora.2–4 Furthermore, IBD is characterized by periods of quiescence interspersed with active disease, with disease relapse often coincident with stressful life events.5,6 Moreover, exposure to various stressors can result in increased enteric epithelial permeability7–9 that would allow luminal antigens access to the mucosa, and evoke inflammatory reactions; increased epithelial permeability accompanies many enteropathies and it has been postulated that Crohn’s disease is a permeability disorder.10 Maintenance of the epithelial barrier, in terms of the paracellular flux of material, is dependent on regulation of the intercellular tight junctions, which is an energy-dependent process.11,12 Accordingly, it is noteworthy that reduced ATP levels have been observed in inflamed tissues excised from some patients with IBD.13 Also noninflamed tissues obtained from patients with Crohn’s disease are more sensitive to uncouplers of oxidative phosphorylation.14 Integrating these data, we formulated a research strategy to test the hypothesis that exposure to commensal, nonpathogenic Escherichia coli would result in increased permeability in epithelia concurrently under metabolic stress.
Materials and Methods
Analysis of Human Tissues
Consent was obtained from patients with colon cancer (as controls) or Crohn’s disease and sections of mildly inflamed ileum were processed for transmission electron microscopy (EM).15 Sections on coded slides were examined for evidence of epithelial structural abnormalities and the average mitochondrial area was calculated from 60 mitochondria in two to four sections from each tissue.16
Rodent Studies
A 2-cm mid-abdominal incision was made in anesthetized male Sprague-Dawley rats (Charles River Laboratories, St. Constant, Quebec, Canada) and dinitrophenol [DNP: 0.5 ml of 3 mmol/L in 5% dimethyl sulfoxide/phosphate-buffered saline (PBS)17 (Sigma Chemical Co., St. Louis, MO)] was injected into the ileal lumen, 10 cm proximal to the ileal-cecal junction. The incision was closed and a 10-cm segment of terminal ileum was removed 6 hours or 24 hours later. Portions of tissue were fixed for EM or formalin-fixed for the enumeration of immune cells on hematoxylin and eosin (H&E)-stained sections (cells in 10 microscopic fields were counted from each well-oriented section).16 Two-cm portions were mounted in Ussing chambers and, under voltage clamped conditions, ion conductance was calculated (indicative of barrier to passive ion flux) and the mucosal-to-serosal flux of horseradish peroxidase (HRP) (type IV, Sigma Chemical Co.) determined following a published protocol.15 Age- and time-matched control rats were injected with 0.5 ml of 5% dimethyl sulfoxide/PBS only. Additional ileal pieces were excised, rinsed in PBS (three times), treated with gentamicin (200 μg/ml), extensively washed, and then homogenized. Homogenates were grown on blood agar for 24 hours and colony-forming units (cfu) enumerated by serial dilution counts and normalized against the original tissue weight. These studies were performed in compliance with institutional and governmental regulations relating to the use of animals in research.
In Vitro Cell Culture Studies
Cell Lines, Bacteria, and Reagents
The human colon-derived crypt-like T84 and HT-29 epithelial cell lines were maintained and cultured as previously described.18 E. coli strains HB10119 and C2520 were cultured in Luria Bertani (LB) broth. Pharmacological inhibitors were purchased from Calbiochem (San Diego, CA): U0126 (25 μmol/L) and PD98059 (50 μmol/L) block the ERK 1/2 mitogen-activated protein kinase (MAPK) pathway; SB203580 (10 μmol/L) inhibits p38 MAPK activity;21 pyrrolidinedithiocarbamate (50 μmol/L) inhibits nuclear factor (NF)-κΒ activation; and SN50 (20 μmol/L) blocks nuclear import and inhibits NF-κΒ activation. Indomethacin (general cyclooxygenase inhibitor and can disrupt electron transfer) and the inhibitors of myosin light chain kinase (MLCK) (ie, ML-7, 20 μmol/L)22 and phosphatidylinositol 3′-kinase (PI-3K) (ie, LY294002, 20 μmol/L)23 activity were purchased from Sigma Chemical Co.
Epithelial cells were grown to confluence (ie, T84 cells, TER ≥1000 Ω · cm2; HT-29 cells, TER >250 Ω · cm2) on 0.4- or 3-μm pore-size filter supports (Costar Inc., Cambridge, MA) or until ∼80% confluence (determined by phase contrast microscopy) on 12-well culture plates. DNP (1.0 or 0.1 mmol/L) and E. coli strains (106 cfu unless stated otherwise) were added simultaneously to the apical side of filter-grown monolayers. Controls: 1) time-matched naïve monolayers, 2) DNP only, and 3) E. coli HB101 (or C25) only. In some experiments 10 μmol/L indomethacin was used instead of DNP.24 In some experiments an 18-hour incubation with enteropathogenic E. coli (EPEC, 106 cfu) was used as a positive control for bacterial disruption of epithelial barrier function.19
Epithelial Cell Mitochondrial Structure and Function
Epithelial monolayers were fixed on filter supports and processed for transmission EM.15,19 Epithelial mitochondrial activity was assessed by the MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazoliumbromide salt] assay after a 24-hour exposure to DNP (0.1 mmol/L).25
Barrier Function
Transepithelial resistance (TER in Ω · cm2; indicates barrier to passive ion flux) across filter-grown monolayers was monitored using a voltmeter and matched electrodes (Millicell-ERS; Millipore, Bedford, MA) and expressed as the percentage of pretreatment TER.23 HRP flux assays were conducted as described.26 Twenty-four hours after DNP ± E. coli HB101 treatment, HRP (10 μmol/L) was added to the apical side of filter-grown T84 cell monolayers. Two hours later samples were retrieved from the basal compartment of the culture well and HRP amounts determined by enzymatic assay and presented as percent recovery of the amount added.
Internalization of Bacteria and Bacterial Translocation
Semiconfluent monolayers of T84 cells were grown in six-well plates and inoculated with E. coli HB101 (106 cfu/ml) ± DNP and incubated for 24 hours at 37°C. A sample of bacterial culture was collected and the number of bacteria determined using the Miles and Misra method. Epithelia were washed extensively and treated with gentamicin (300 μg/ml, Sigma Chemical Co.) for 1 hour, at which point the epithelia were rinsed with sterile PBS (three times), lysed with 1.0 ml of cold 1% Triton X-100/PBS (10 minutes at 4°C) and plated onto LB agar. The number of internalized, viable bacteria was determined and presented as a percentage of the number of extracellular bacteria after the 24-hour growth period.
For translocation assays, T84 cells were grown to confluence on 3-μm pore-size filters, transferred to antibiotic-free medium, and inoculated apically with E. coli HB101 ± DNP. Aliquots were collected from the basolateral compartment 16 hours later and the number of bacteria determined.
F-Actin and α-Actinin Visualization
Epithelial preparations were rinsed in PBS, fixed with ∼4οC methanol or formalin for 10 to 20 minutes, and incubated with mouse anti-human α-actinin antibodies (1:100 dilution, Sigma Chemical Co.) for 1 hour at 37°C. Epithelia were rinsed in cold PBS and incubated with fluorescein isothiocyanate-labeled donkey anti-mouse IgM μ-chain-specific antibodies (1 hour at 37°C, 1:100 dilution; Jackson ImmunoResearch Lab Inc., West Grove, PA).27 After three PBS rinses, the cells were stained with propidium iodide to identify the nucleus. Additional monolayers were treated with Texas Red-conjugated phalloidin (0.1 μmol/L; Molecular Probes, Eugene, OR) to identify filamentous (F) actin.28 Coded preparations were observed on a Zeiss 510 confocal scanning laser microscope.
Interleukin (IL)-8 Enzyme-Linked Immunosorbent Assay
Epithelial cells were grown to ∼80% confluence, exposed to E. coli HB101 ± DNP for 24 hours and 1) RNA extracted and reverse transcriptase-polymerase chain reaction performed for IL-8 followed by densitometric analysis of the electrophoretic gel as previous described29 and 2) culture medium samples collected 24 hours later for IL-8 determination by commercial enzyme-linked immunosorbent assay (R&D Systems, Minneapolis, MN). Epithelia treated with tumor necrosis factor (TNF)-α (10 ng/ml) or exposed to EPEC (106 cfu) for 24 hours served as positive controls for induction of IL-8. The assay detection limit was 16 pg/ml. Pharmacological inhibitors were added, at the doses indicated, 30 minutes before E. coli HB101 ± DNP treatment.
Electrophoretic Mobility Shift Assay
Epithelial nuclear protein extracts were obtained and electrophoretic mobility shift assay conducted using a published protocol23 with end-labeled double-stranded oligonucleotides bearing the AP-1 consensus binding sequence: 5′-CGC TTG ATG ACT CAG CCG GAA-3′ (Santa Cruz Biotechnology, Santa Cruz, CA). Specificity controls consisted of non-32P-labeled double-stranded DNA oligonucleotide as a cold competitor and supershifts with a pan-anti-Fos antibody (K-25, Santa Cruz Biotechnology). Nuclear extracts from TNF-α (10 ng/ml, R&D Systems)-treated epithelia served as positive controls.
Statistical Analyses
Data are presented as mean ± SEM and n values are the number of individual epithelial preparations. Data were analyzed with Student’s t-test or a one-way analysis of variance followed by posthoc comparisons with the Neuman-Keuls test. A statistically significant difference was accepted at P < 0.05.
Results
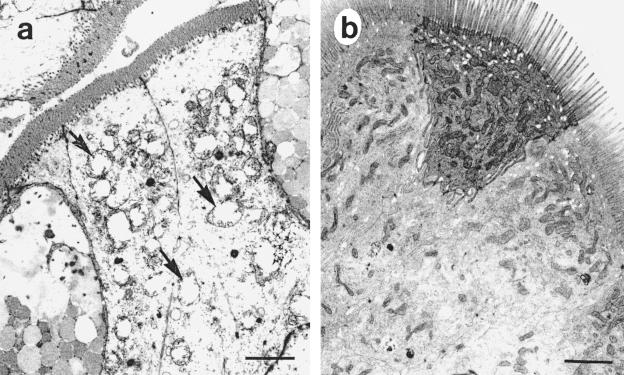
Transmission electron photomicrographs of mildly inflamed ileal specimens obtained from patients with Crohn’s disease revealed swollen epithelial cell mitochondria with disrupted cristae (Figure 1). Morphometric analysis confirmed a significant increase in average mitochondrial area (0.57 ± 0.11 μm2) in tissues from patients with Crohn’s disease compared to resections from patients with cancer (0.19 ± 0.06 μm2; P < 0.05; n = 60 mitochondria from three patient samples). These findings support previous literature indicative of altered energy metabolism in gut tissues from patients with IBD,14 and provided the impetus to proceed to complementary animal and in vitro studies.
Figure 1.
Mildly inflamed ileum from patients with Crohn’s disease has abnormal mitochondria. Transmission EM reveals swollen mitochondria with irregular cristae in enterocytes from patients with Crohn’s disease (arrows) (a) that were not apparent in ileal resections from patients with cancer (b) (n = 3). Scale bars, 2 μm.
DNP Instilled into Rat Ileum Causes Increased Permeability, Bacterial Attachment, and an Inflammatory Cell Infiltrate
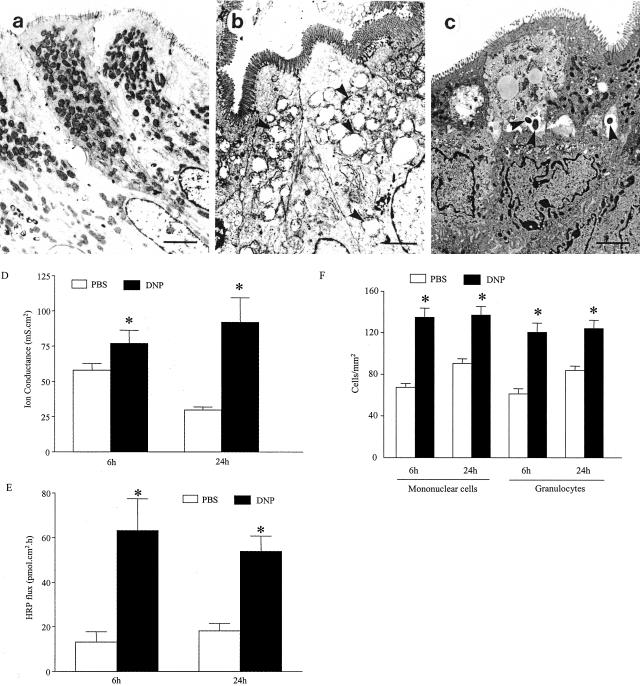
To mimic the conditions observed in human tissue, DNP was used to uncouple oxidative phosphorylation.17 Instillation of DNP into the distal ileum of rats resulted in damaged epithelial mitochondria (mitochondria size, PBS = 0.51 ± 0.02 μm2 versus DNP = 0.79 ± 0.05 μm2; P < 0.05; n = 60 mitochondria from four rats) and an apparent increase in bacteria attached to, and inside, the enterocytes of treated intestine. These changes were most apparent at 6 hours after DNP treatment (Figure 2; A to C). The increased occurrence of bacteria in tissues from DNP-treated rats was confirmed by culturing tissue homogenates that had been treated with antibiotics to kill attached bacteria: control = 7.5 × 104 versus DNP-treated = 6.8 × 105 cfu/g tissue (average of two rats).
Figure 2.
DNP treatment results in mitochondrial abnormalities, increased permeability, and an inflammatory infiltrate in the rat ileum. Tissues from controls show numerous electron-dense mitochondria (A), whereas those in tissues from ileum exposed to DNP 6 hours previously have swollen disrupted mitochondria (arrowheads) (B). C: Bacteria (arrowheads) were commonly observed within enterocytes of tissue from DNP-treated rats. Tissue ion conductance (D) and flux of HRP (E) were increased in ileal segments from DNP-treated rats at 6 hours and 24 hours after treatment. F: Concomitantly these tissues showed evidence of an inflammatory infiltrate as assessed by mononuclear cell and granulocyte (neutrophil, eosinophil, and mast cells) counts on H&E-stained sections (n = 4; *, P < 0.05 compared to PBS/dimethyl sulfoxide control; mean ± SEM). Scale bars, 2 μm.
Concomitantly, DNP treatment evoked increases in epithelial permeability as gauged by ion conductance and the transepithelial flux of HRP (Figure 2, D and E). Histological assessment of ileal sections from the DNP-treated rats revealed increased numbers of mononuclear and polymorphonuclear immune cells in the mucosa by 6 hours after treatment that remained elevated until 24 hours after treatment (Figure 2F). There were no differences between the magnitude of the increase in immune cells at 6 and 24 hours after DNP. This suggests that either the maximum response has occurred by 6 hours, or that there is increased immune cell traffic to the gut in the 6- to 24-hour period that is balanced by exit from the tissue perhaps as cells move to the local draining lymph nodes.
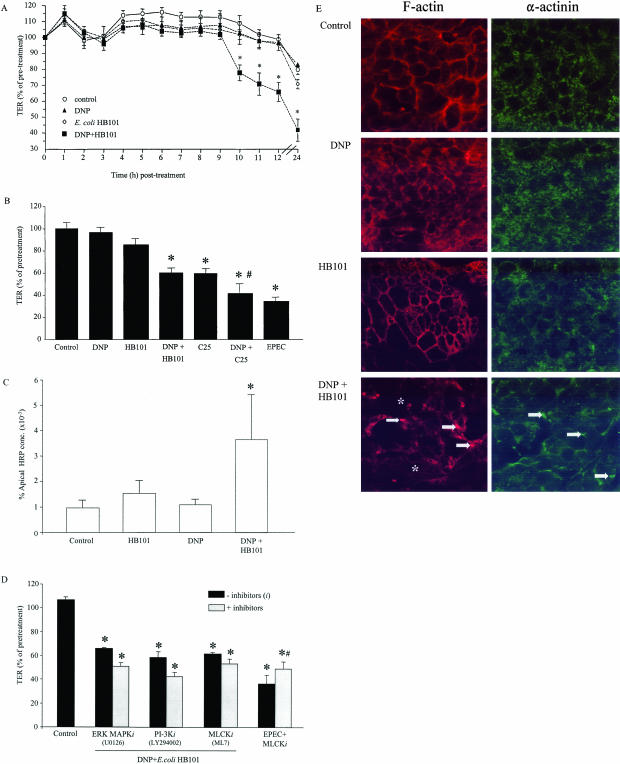
Commensal E. coli Strains in the Presence of DNP Disrupt Epithelial Barrier Function
A cell culture model was used to delineate the mechanism of the altered epithelial function after exposure to DNP + nonpathogenic E. coli. Initial experiments revealed that low-dose DNP (0.1 mmol/L) did not affect the growth of E. coli HB101 (n = 2) (1.0 mmol/L blocked bacteria growth), but did result in swollen, irregular epithelial mitochondria and reduced mitochondrial activity by 30 to 40% as indicated by the MTT assay (n = 3); these effects of DNP have been reported previously.17 Exposure of polarized T84 epithelial cell monolayers to DNP (0.1 mmol/L) or E. coli HB101 (106 cfu) alone did not affect TER (a marker of paracellular permeability). In contrast, DNP + E. coli HB101 treatment resulted in significant increases in epithelial permeability that were apparent by 10 hours after infection and maximal at 24 hours after infection (end of experiment) (Figure 3, A and B). A 24-hour exposure to DNP + E. coli HB101 also resulted in increased transepithelial flux of the 44-kd protein, HRP that traverses the epithelium via transcellular and paracellular (albeit to a less extent) routes (Figure 3C).
Figure 3.
Loss of barrier function occurs in metabolically stressed polarized T84 epithelia exposed to nonpathogenic E. coli strains. A: Monolayers treated with DNP + E. coli HB101 display a drop in TER 10 hours later (n = 3; mean ± SD; *, P < 0.05 compared to other treatments). B: Bar chart showing that 24 hours of exposure to DNP (0.1 mmol/L) + E. coli HB101 (HB101; 106 cfu) reduces TER (presented as percent of pretreatment values of the same monolayer) and that while E. coli C25 (C25) alone reduces TER, this is enhanced in the presence of DNP. The effect of EPEC is included as a positive control (n = 9; *, P < 0.05 compared to control; #, P < 0.05 compared to C25 only). C: Under the same conditions, DNP + HB101 exposure evoked increases in transepithelial flux of HRP (n = 6; *, P < 0.05 compared to control). D: A 30- to 60-minute pretreatment with an ERK MAPK inhibitor (i) (U0126; 25 μmol/L; n = 4), or inhibitors of PI-3K (LY294002; 20 μmol/L; n = 4) or MLCK (ML-7; 20 μmol/L; n = 4) did not prevent the DNP + E. coli HB101-induced drop in TER observed after a 24-hour culture. As a control, the MCLKi partially reduced the EPEC-induced drop in TER (*, P < 0.05 compared to control; #, P < 0.05 compared to EPEC only; n = 4; mean ± SEM). In these experiments pretreatment TER ranged from 1000 to 2500 Ω · cm2. E: En face confocal scanning laser microscope images of epithelial F-actin (left) and α-actinin (right) showing that 24 hours of DNP + E. coli HB101 co-treatment resulted in disruption of the normal enterocytic cytoskeleton as shown by focal condensation of F-actin (arrows) and dissociation from the cell periphery/perijunctional region (*), and redistribution and focal hot spots of α-actinin (arrows) (images are representative of six monolayers/condition).
Exposure to E. coli strain C25 alone reduced T84 TER and this was further reduced by simultaneous DNP treatment (n = 9) (Figure 3B). Also, a 24-hour exposure to E. coli C25 alone increased the transepithelial flux of HRP (control = 1.1 ± 0.5 × 10−3 versus C25 = 11.2 ± 4.5 × 10−3% of apical HRP dose) and this was increased approximately threefold by co-treatment with DNP (30.5 ± 6.8 × 10−3% of apical HRP; n = 6; *, P < 0.05 compared to E. coli C25 only). These data are consistent with E. coli C25 designation as a putative low-grade pathogen20 and show that metabolically stressed epithelia are more sensitive to this organism.
DNP may have elicited effects by affecting the bacteria, the enterocytes, or both. Exposure of T84 cells to 1) DNP-treated E. coli HB101, 2) heat-killed E. coli HB101 + DNP, 3) a 0.22-μm culture medium filtrate from naïve bacterial cultures, 4) medium from DNP-treated bacterial cultures, or 5) medium from E. coli HB101 24-hour cultures spiked with DNP (0.1 mmol/L) each failed to significantly affect TER (n = 6 monolayers/condition; data not shown). Thus, the increase in epithelial permeability evoked by DNP + E. coli HB101 required the presence of viable organisms, was not dependent on a bacteria-derived product, and was because of the impact of DNP on the epithelium.
Pharmacological studies have implicated the intracellular signaling molecules, ERK 1/2 MAPK, PI-3K, and MLCK in the control of epithelial paracellular permeability.23,30,31 Indeed, MLCK activation is important in the drop in TER that occurs after EPEC infection.19,31 Use of U0126, LY294002, and ML-7 to inhibit the activity of ERK 1/2 MAPK, PI-3K, and MLCK, respectively, failed to ameliorate the drop in TER evoked by DNP + E. coli HB101 (Figure 3D). We have used these drugs to successfully block cytokine signaling in T84 and HT-29 epithelia21–23 and ML-7 partially prevented the reduced TER caused by exposure to EPEC (Figure 3D).
However, there were discernable effects on the enterocytic cytoskeleton that were reminiscent of infection with EPEC or parasitic protozoa19,32—DNP + E. coli HB101 treatment resulted in dissociation of F-actin from the perijunctional actinomyosin ring, and focal condensations of F-actin and the actin-associated protein, α-actinin (Figure 3E).
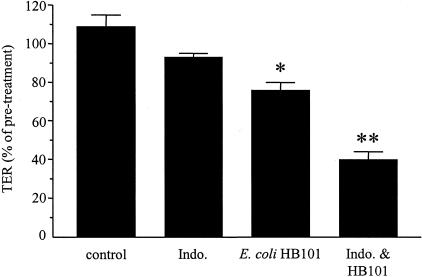
Like DNP, the nonsteroid anti-inflammatory drug indomethacin can interfere with oxidative phosphorylation. Indomethacin (10 μmol/L) alone did not alter T84 monolayer TER nor did it affect E. coli HB101 growth. Figure 4 shows that monolayers exposed for 24 hours to the combination of indomethacin + E. coli HB101 displayed a significant drop in TER (n = 11).
Figure 4.
Bar chart showing the significant drop in TER across T84 epithelial monolayers 24 hours after treatment with indomethacin (indo.; 10 μmol/L) + E. coli HB101 (n = 11 monolayers; * and **, P < 0.05 compared to other treatments; note in these experiments HB101 alone resulted in a small but significant drop in TER; pretreatment TER ranged from 1380 to 3760 Ω · cm2).
DNP + E. coli Increase Bacterial Translocation Across Polarized Epithelia
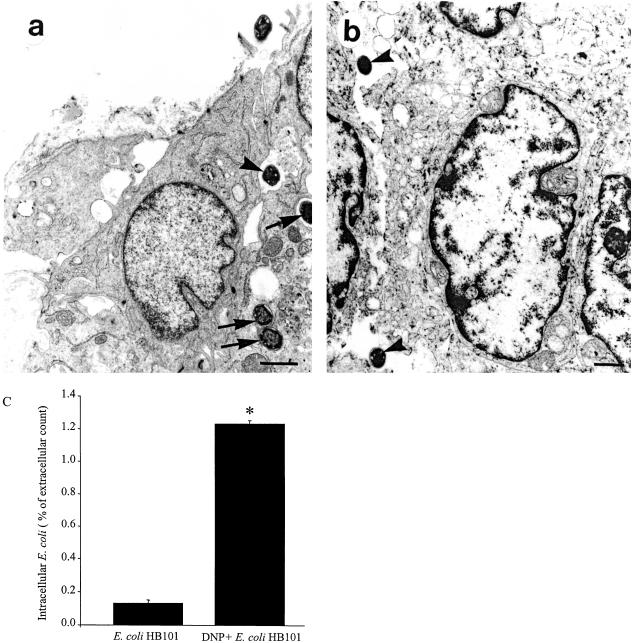
Transmission EM photomicrographs revealed increased numbers of bacteria inside T84 cells exposed to DNP + E. coli HB101 for 24 hours, with occasional bacteria being noted in the paracellular space (Figure 5, a and b). Bacteria were not observed in sections of control monolayers, which could be because of sampling and the small area examined. However, a modified bacterial invasion assay confirmed the presence of ∼10-fold increase in intracellular bacteria compared to E. coli-only treated cells (Figure 5c). Coupling DNP + E. coli HB101 also resulted in significant bacteria translocation across the filter-grown epithelial monolayers: bacteria were found in the basal compartment of every (n = 18) monolayer treated 16 hours previously with DNP + E. coli HB101, whereas bacterial translocation was not apparent during the same time frame in T84 monolayers treated with E. coli HB101 only (n = 18).
Figure 5.
Exposure to DNP + E. coli HB101 results in increased bacterial entry and translocation across polarized epithelial monolayers. a and b: Representative EM photomicrographs showing bacteria within T84 cells (arrows) and in the paracellular spaces (arrowheads) between adjacent DNP + E. coli HB101-treated filter-grown T84 epithelial monolayers. c: Using a modified invasion assay, ∼10-fold more bacteria were obtained from cell lysates of DNP + E. coli HB101-treated cells compared to those exposed to E. coli only (data are expressed as the percentage of the number of extracellular bacteria 24 hours after culture; n = 18; *, P < 0.05 compared to control). Scale bars, 1 μm.
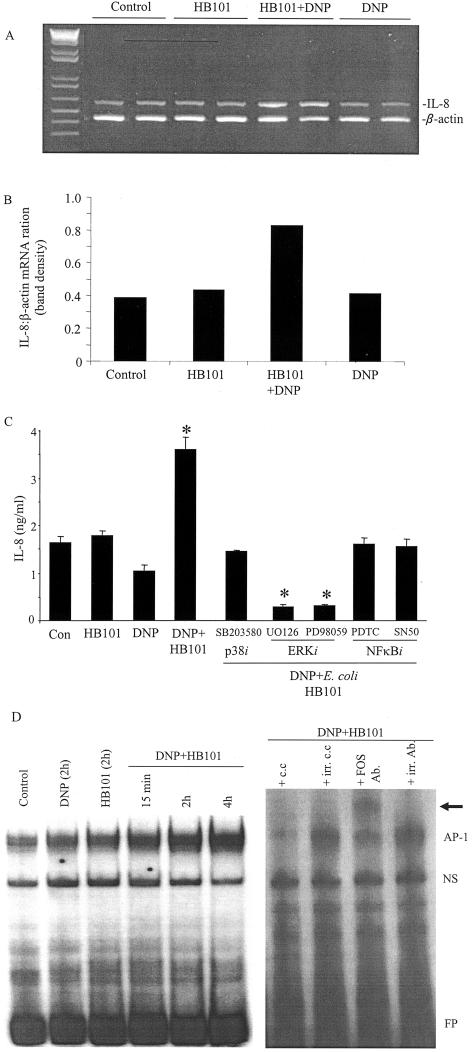
DNP + E. coli Evokes Epithelial IL-8 Synthesis and Activation of the Transcription Factor, Activated Protein (AP)-1
Entry of bacteria into the mucosa represents a serious threat to the host that could result in sepsis and multiorgan failure. The DNP + E. coli HB101-induced drop in TER and concomitant increases in bacterial translocation could be accompanied by induction of an alarm response from the enterocyte to mobilize an anti-bacterial response. Reverse transcriptase-polymerase chain reaction analysis revealed a small increase in IL-8 mRNA in DNP + E. coli HB101-treated epithelia (Figure 6, A and B) and this was translated into increased IL-8 protein: T84 cells displayed a 29 ± 7% (P < 0.05, n = 8) increase in IL-8 protein 24 hours after co-treatment, whereas DNP + E. coli HB101 evoked approximately twofold increase in IL-8 production in the human HT-29 colonic epithelial cell line (HB101 only = 2.21 ± 0.12 versus DNP + HB101 = 4.67 ± 0.36 ng/ml, P < 0.05; n = 5). The increase in IL-8 secretion from HT-29 cells was prevented by use of pharmacological inhibitors of the ERK and p38 MAPK pathways, and NF-κB signaling (Figure 6C). It should be noted that EPEC-infected HT-29 cells produced more IL-8 that those treated DNP + HB101 (P = 0.04) and, consistent with earlier findings,29 TNF-α exposure led to a massive increase in IL-8 (61.5 ± 7.3 ng/ml; n = 5; P < 0.001 compared to control and DNP + HB101).
Figure 6.
Metabolic stress and exposure to nonpathogenic E. coli evokes increased IL-8 production and AP-1 activation. A: Image representative of three separate experiments showing increased IL-8 mRNA reverse transcriptase-polymerase chain reaction product in epithelia treated with DNP + E. coli, which is semiquantified by densitometry (average of the two separate epithelial preparations shown in A). B and C: Bar chart showing that increased HT-29 IL-8 production is blocked by use of pharmacological inhibitors of ERK and p38 MAPKs, and NF-κB (n = 5; *, P < 0.05 compared to control, E. coli HB101 or DNP only). D: Representative electrophoretic mobility shift assay gel showing time-dependent induction in AP-1 activation in DNP + E. coli HB101-treated epithelia (left). Specificity of the AP-1 band was confirmed by ablation of the band by inclusion of a cold competitor (c.c.) double-stranded oligonucleotide but not an irrelevant cold competitor (irr. c.c.) and supershifting by a pan-anti-Fos antibody (Ab), but not an irrelevant isotype-matched antibody (irr. Ab.) (right; extracts from cells 2 hours after DNP + E. coli HB101 treatment; NS, nonspecific band; FP, free probe). Extracts from TNF-α (10 ng/ml)-treated epithelia were used as a positive control (not shown).
A variety of signaling pathways regulate IL-8 synthesis at both the transcription and posttranscriptional levels;21 AP-1 is one such signal and, indeed, AP-1 can be activated by ERK MAPK.33 Electrophoretic mobility shift assay revealed a time-dependent activation of AP-1 in epithelia exposed to DNP + E. coli HB101 (Figure 6D), but not to either agent alone.
Discussion
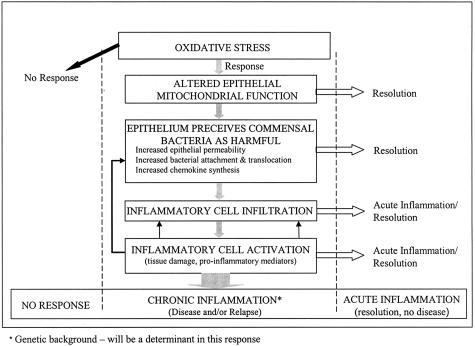
A current hypothesis in IBD research is that the disease is because of an inappropriate immune response to a component of the normal microflora, and may be precipitated by altered epithelial function, including increased permeability. Evidence in support of this postulate comes from a variety of sources: 1) diversion of the fecal stream can ameliorate colitis and analysis of patient tissue resections reveals increased numbers of bacteria attached to the gut epithelium;34,35 2) immunodeficient mice that develop spontaneous colitis have less severe disease when maintained in a germ-free environment;36 3) stress can evoke IBD relapse and elicits increases in human and rodent epithelial permeability—in the latter case this can be associated with deranged epithelial mitochondrial appearance and increased bacterial attachment;7,8,16,37,38 4) regulation of epithelial barrier function is an energy-dependent process that can be directly affected by bacterial pathogens such as enteropathogenic and enterohemorrhagic E. coli (EHEC).11,13,14,19,22 The current study integrates these observations into a unifying paradigm (Figure 7).
Figure 7.
Hypothetical model for the interplay of metabolically perturbed gut epithelia and the normal gut flora in the induction of intestinal inflammatory disease and/or disease relapse.
Initial findings with human tissues confirmed previous studies, showing swollen and irregular mitochondria indicative of perturbed function and predictive of lower cellular ATP levels.13,14 Importantly, these abnormalities occurred in slightly inflamed tissue, which may have implications for disease progression and the induction of relapses. Such speculation is supported by the increased sensitivity of IBD tissue to sodium caprate,14 and the facts that nonsteroidal anti-inflammatory drugs (NSAIDs) can increase gut permeability39 (possibly via effects on epithelial mitochondria24) and that NSAID use can elicit relapse in patients with Crohn’s disease.40,41
Recently we reported that exposure of rats to mild chronic stress resulted in disrupted epithelial mitochondrial structure, increased bacterial attachment to the epithelium, and a low-grade ileal and colonic mucosal inflammation.16 The abnormalities were a consequence of the stress—supporting the hypothesis of stress-induced gut dysfunction.9 However, it remained unclear if the mitochondrial dysfunction resulted in bacterial attachment and if the inflammatory infiltrate was a consequence of epithelial cell activation or vice versa. Thus experiments were initiated with DNP, which by virtue of its ability to uncouple oxidative phosphorylation would be expected to elicit any gut effects by affecting energy metabolism/mitochondria activity.
Direct instillation of DNP into the lumen of rat ileum caused the predicted perturbation of epithelial mitochondrial structure, and resulted in increased epithelial permeability, bacterial penetration, and an immune cell infiltrate: gut events reminiscent of those observed in the stress model.16 However, the inflammatory infiltrate was subtle (ie, approximately twofold increase) and was quantifiably similar at 6 and 24 hours after treatment, suggesting either an equilibrium had been reached between cell influx and exit or that the effect of this acute DNP treatment peaked at 6 hours after treatment. The lack of obvious tissue damage and sustained immune cell accumulation may indicate a generalized gut response to low-grade insults (eg, limited periods of ischemia); moreover, it suggests that the DNP exposure has primed the intestine to respond more aggressively to otherwise nonnoxious stimuli. Together, the data strongly support the concept that the epithelial abnormality was the catalyst for the enteric changes. However, the possibility that the effects of DNP were mediated by dendritic cells or intraepithelial lymphocytes that can be exposed to the luminal contents, or other mucosal cells could not be unequivocally dismissed.42,43 A cell culture approach was adopted to address this issue.
Low-dose DNP added to epithelial monolayers resulted in disrupted mitochondrial structure and function but did not affect TER, suggesting negligible cytotoxic effects of DNP at this dose and the importance of maintaining an intact epithelial barrier. Consistent with previous findings, E. coli HB101 had no, or negligible, effects on T84 TER.19 Strikingly, DNP + E. coli HB101 treatment resulted in dramatic changes in epithelial paracellular and transcellular permeability as gauged by the transepithelial movement of ions (ie, TER) and the larger, potentially antigenic protein HRP, respectively. The findings were reproduced with two human colonic epithelial cell lines and two E. coli strains: the nonpathogenic HB101 control stain and C25, a clinical isolate and potential low-grade pathogen. Thus, the metabolically stressed epithelia have become sensitive or hyperresponsive to both nonnoxious and mild pathogens. It is important, and clinically relevant given the association between NSAID use and relapse in IBD, to highlight that the combination of indomethacin and E. coli HB101 also evoked a significant drop in TER. However, because indomethacin inhibits both arachidonic acid metabolism and affects mitochondria we focused the subsequent mechanistic studies on DNP, which selectively interferes with mitochondrial function.
Analysis of a variety of control experiments supports the view that the increased epithelial permeability requires contact with live bacteria and is not because of the release of a soluble product from E. coli. Also, the possibility that the DNP was converting the nonpathogenic E. coli HB101 into a pathogen was dismissed by experiments with DNP-treated E. coli HB101. Furthermore, use of pharmacological inhibitors that block intracellular signals known to be involved in control of epithelial tight junctions, and hence paracellular permeability (ie, ERK MAPK, PI-3K, and MLCK), all failed to prevent the barrier defect evoked by DNP + E. coli HB101. The lack of involvement of MLCK is particularly intriguing because this enzyme has been implicated in EPEC- and EHEC-induced increases in epithelial permeability.22,31 Moreover, although focal modifications in the distribution of F-actin and α-actinin were associated with DNP + E. coli HB101 treatment, and these were somewhat reminiscent of the enterocytic cytoskeletal response to EPEC infection,19 attaching-effacing lesions typical of EPEC infection44 were not observed. Thus, although the data indicate that epithelia under metabolic stress can perceive nonpathogenic commensal bacteria as threatening, this response is distinct from that elicited by known bacterial pathogens such as EPEC and EHEC. Moreover, should these findings extrapolate to human disease then precise definition of the mechanisms responsible for the DNP + E. coli HB101-induced disruption of epithelial barrier function has the potential to provide insight into how commensal bacteria may evoke IBD or stress-induced relapses in IBD.
EM revealed increased numbers of bacteria within the enterocyte and in the paracellular spaces and this was confirmed by invasion assays that revealed an ∼10-fold increase in intracellular bacteria in DNP + E. coli HB101-treated epithelia compared to E. coli HB101-only treatedcells. The increase in intracellular bacteria was accompanied by a marked increase in bacterial translocation across the filter-grown polarized monolayers. This was an unexpected finding because E. coli HB101 is noninvasive and was, to us, particularly intriguing in light of reports describing increases in adherent bacteria on tissue resections from patients with IBD.45,46 Further use of this model to explore the mechanism of the enhanced bacterial translocation may present means to block similar in vivo events.
Reduced barrier function in vivo and bacterial penetration across the epithelium would be expected to elicit an immune response, which could either effectively neutralize the pathogen/antigen or if inappropriately controlled result in inflammatory disease. In this context we found that exposure to DNP + E. coli HB101 evoked a significant increase in epithelial IL-8 production, an event not observed with DNP or E. coli HB101 alone. This up-regulation of IL-8 synthesis by model epithelia in vitro complements the in vivo observation of an inflammatory cell infiltrate in the DNP-treated rat ileum. However, this enhanced IL-8 production was significantly less than that evoked by TNF-α or EPEC exposure, which is again consistent with the postulate that metabolic stress in the face of a normally nonnoxious commensal flora triggers events that could predispose an individual to more vigorous subsequent immune responses.
The ERK and p38 MAPKs, and NF-κB are important controls of IL-8 production and all have been implicated in the regulation of enteric epithelial IL-8 synthesis.21 In accordance with this the DNP + E. coli HB101 induced IL-8 was abrogated by pharmacological inhibitors of all three signal transduction pathways. Additionally, AP-1 activation (ie, DNA binding activity), a downstream signal from ERK MAPK that is involved in the regulation of IL-8 production,33 was only increased in DNP + E. coli HB101-treated epithelial. Thus, the findings that the epithelial IL-8 synthesis was ERK-, p38-, and NF-κB-dependent are in agreement with the current understanding of the control of IL-8 production and this contrasts with the DNP + E. coli HB101-induced perturbation of epithelial barrier function, the mechanism of which remains to be elucidated. Finally, and perhaps most importantly, the data indicate that the stressed (ie, DNP-treated) enterocyte responds differently to nonpathogenic bacteria, mobilizing a panel of signals and subsequent gene activation events that may cause inflammation and supports a central role for the epithelium in the modulation of mucosal immunity.
In conclusion, based on initial observations with human tissues this study presents data from in vivo and in vitro investigations as proof-of-principal evidence in support of our hypothesis (Figure 7), in which perturbations of epithelial cell energy metabolism results in normally innocuous bacteria being perceived as a threat that could lead to inflammatory disease should the altered epithelial response (eg, increased permeability, bacterial translocation, chemokine synthesis) be prolonged.
Footnotes
Address reprint requests to Derek M. McKay, Ph.D., Intestinal Disease Research Programme, HSC-3N5C, McMaster University, 1200 Main St. West, Hamilton, Ontario, Canada L8N 3Z5. E-mail: mckayd@mcmaster.ca.
Supported by a group grant from the Crohn’s and Colitis Foundation of Canada.
P.M.S. is the recipient of a Canada Research Chair in Gastrointestinal Disease.
References
- Beck IT. Disproportion of economic impact, research achievements and research support in digestive diseases in Canada. Clin Invest Med. 2001;24:12–36. [PubMed] [Google Scholar]
- McKay DM. Intestinal inflammation and the gut microflora. Can J Gastroenterol. 1999;13:509–516. doi: 10.1155/1999/680206. [DOI] [PubMed] [Google Scholar]
- Farrell RJ, LaMont JT. Microbial factors in inflammatory bowel disease. Gastroenterol Clin N Am. 2002;31:41–62. doi: 10.1016/s0889-8553(01)00004-8. [DOI] [PubMed] [Google Scholar]
- Shanahan F. Inflammatory bowel disease: immunodiagnostics, immunotherapeutics, and ecotherapies. Gastroenterology. 2001;120(Suppl. 1):S622–S635. doi: 10.1053/gast.2001.22122. [DOI] [PubMed] [Google Scholar]
- Collins SM. Stress in the gastrointestinal tract IV. Modulation of intestinal inflammation by stress: basic mechanisms and clinical relevance. Am J Physiol. 2001;280:G315–G318. doi: 10.1152/ajpgi.2001.280.3.G315. [DOI] [PubMed] [Google Scholar]
- Collins SM. Similarities and dissimilarities between asthma and inflammatory bowel diseases. Aliment Pharmacol Ther. 1996;10 (Suppl. 2):S25–S31. doi: 10.1046/j.1365-2036.1996.22164017.x. [DOI] [PubMed] [Google Scholar]
- Saunders PR, Kosecka U, McKay DM, Perdue MH. Acute stressors stimulate ion secretion and increase epithelial permeability in rat intestine. Am J Physiol. 1994;267:G794–G799. doi: 10.1152/ajpgi.1994.267.5.G794. [DOI] [PubMed] [Google Scholar]
- Santos J, Saperas E, Nogueiras C, Mourelle M, Antolin M, Cadahia A, Malagelada JR. Release of mast cell mediators into the jejunum by cold pain stress in humans. Gastroenterology. 1998;114:640–848. doi: 10.1016/s0016-5085(98)70577-3. [DOI] [PubMed] [Google Scholar]
- Soderholm JD, Perdue MH. Stress and the gastrointestinal tract. II. Stress and intestinal barrier function. Am J Physiol. 2001;280:G7–G13. doi: 10.1152/ajpgi.2001.280.1.G7. [DOI] [PubMed] [Google Scholar]
- Hollander D. Crohn’s disease—a permeability disorder of the tight junction? Gut. 1998;29:1621–1624. doi: 10.1136/gut.29.12.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickman KG, Hempson SJ, Anderson J, Lippe S, Zhao L, Burakoff R, Shaw RD. Rotavirus alters paracellular permeability and energy metabolism in caco-2 cells. Am J Physiol. 2000;279:G757–G766. doi: 10.1152/ajpgi.2000.279.4.G757. [DOI] [PubMed] [Google Scholar]
- Gabe SM, Bjarnason I, Tolou-Ghamari Z, Tredger JM, Johnson PG, Barclay GR, Williams R, Silk DB. The effect of tacrolimus (FK506) on intestinal barrier function and cellular energy production in humans. Gastroenterology. 1998;115:67–74. doi: 10.1016/s0016-5085(98)70366-x. [DOI] [PubMed] [Google Scholar]
- Schurmann G, Bruwer M, Klotz A, Schmid KW, Senninger N, Zimmer KP. Transepithelial transport processes at the intestinal mucosa in inflammatory bowel disease. Int J Colorectal Dis. 1999;14:41–46. doi: 10.1007/s003840050181. [DOI] [PubMed] [Google Scholar]
- Soderholm JD, Olaison G, Peterson KH, Franzen LE, Lindmark T, Wiren M, Tagesson C, Sjodahl R. Augmented increase in tight junction permeability by luminal stimuli in the non-inflamed ileum of Crohn’s disease. Gut. 2002;50:307–313. doi: 10.1136/gut.50.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berin MC, Kiliaan AJ, Yang PC, Groot JA, Taminiau JA, Perdue MH. Rapid transepithelial antigen transport in rat jejunum: impact of sensitization and hypersensitivity reaction. Gastroenterology. 1997;113:856–864. doi: 10.1016/s0016-5085(97)70180-x. [DOI] [PubMed] [Google Scholar]
- Soderholm JD, Yang PC, Ceponis P, Vohra A, Riddell R, Sherman PM, Perdue MH. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- Somasundaram S, Sigthorsson G, Simpson RJ, Watts J, Jacob M, Tavares IA, Rafi S, Roseth A, Foster R, Price A, Wrigglesworth JM, Bjarnason I. Uncoupling of intestinal mitochondrial oxidative phosphorylation and inhibition of cyclooxygenase are required for the development of NSAID-enteropathy in the rat. Aliment Pharmacol Ther. 2000;14:639–650. doi: 10.1046/j.1365-2036.2000.00723.x. [DOI] [PubMed] [Google Scholar]
- McKay DM, Singh PK. Superantigen-activation of immune cells evokes epithelial (T84) transport and barrier abnormalities via interferon-γ and tumour necrosis factor-α. Inhibition of increased permeability, but not diminished secretory responses by transforming growth factor β2. J Immunol. 1997;159:2382–2390. [PubMed] [Google Scholar]
- Philpott DJ, McKay DM, Sherman PM, Perdue MH. Infection of T84 cells with enteropathogenic Escherichia coli alters barrier and transport functions. Am J Physiol. 1996;270:G634–G645. doi: 10.1152/ajpgi.1996.270.4.G634. [DOI] [PubMed] [Google Scholar]
- Mattar AF, Drongowski RA, Coran AG, Harmon CM. Effect of probiotics on enterocyte bacterial translocation in vitro. Pediatr Surg Int. 2001;17:265–268. doi: 10.1007/s003830100591. [DOI] [PubMed] [Google Scholar]
- Jijon HB, Panenka WJ, Madsen KL, Parsons HG. MAP kinases contribute to IL-8 secretion by intestinal epithelial cells via a post-transcriptional mechanism. Am J Physiol. 2002;283:C31–C41. doi: 10.1152/ajpcell.00113.2001. [DOI] [PubMed] [Google Scholar]
- Philpott DJ, McKay DM, Mak W, Perdue MH, Sherman PM. Signal transduction pathways involved in enterohemorrhagic Escherichia coli-induced alterations in T84 epithelial permeability. Infect Immunity. 1998;66:1680–1687. doi: 10.1128/iai.66.4.1680-1687.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceponis PJM, Botelho F, Richards CD, McKay DM. Interleukins 4 and 13 increase intestinal epithelial permeability via a phosphatidylinositol-3′ kinase dependent pathway: lack of evidence for stat-6 involvement. J Biol Chem. 2000;275:29132–29137. doi: 10.1074/jbc.M003516200. [DOI] [PubMed] [Google Scholar]
- Somasundaram S, Rafi S, Sigthorsson G, Jacob M, Price AB, Macpherson A, Mahmod T, Scott D, Wigglesworth JM, Bjarnason I. Mitochondrial damage: a possible mechanisms of the “topical” phase of NSAID induced injury in the rat intestine. Gut. 1997;41:344–353. doi: 10.1136/gut.41.3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Granados N, Howe K, Lu J, McKay DM. Dextran sulphate sodium-induced colonic histopathology, but not altered epithelial ion transport, is reduced by inhibition of phosphodiesterase activity. Am J Pathol. 2000;156:2169–2177. doi: 10.1016/S0002-9440(10)65087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berin MC, Yang PC, Ciok L, Waserman S, Perdue MH. Role of IL-4 in macromolecular transport across intestinal epithelium. Am J Physiol. 1999;276:C1046–C1052. doi: 10.1152/ajpcell.1999.276.5.C1046. [DOI] [PubMed] [Google Scholar]
- Ismaili A, Philpott DJ, Dytoc MT, Soni R, Ratnam S, Sherman PM. Alpha-actinin accumulation in epithelial cells infected with attaching and effacing gastrointestinal pathogens. J Infect Dis. 1995;172:1393–1396. doi: 10.1093/infdis/172.5.1393. [DOI] [PubMed] [Google Scholar]
- McKay DM, Croitoru K, Perdue MH. T cell monocyte interactions regulate epithelial physiology in a coculture model of inflammation. Am J Physiol. 1996;270:C418–C428. doi: 10.1152/ajpcell.1996.270.2.C418. [DOI] [PubMed] [Google Scholar]
- Akhtar M, Watson JL, Nazli A, McKay DM. Bacterial DNA evokes epithelial IL-8 production by a MAPK-dependent, NF-κΒ-independent pathway. FASEB J. 2003;17:1319–1321. doi: 10.1096/fj.03-0950fje. [DOI] [PubMed] [Google Scholar]
- Kinugasa T, Sakaguchi T, Gu X, Reinecker H-C. Claudins regulate the intestinal barrier in response to immune mediators. Gastroenterology. 2000;118:1001–1011. doi: 10.1016/s0016-5085(00)70351-9. [DOI] [PubMed] [Google Scholar]
- Zolotarevsky Y, Hecht G, Koutsouris A, Gonzalez DE, Quan C, Tom J, Mrsny RJ, Turner JR. A membrane-permeant peptide that inhibits MLC kinase restores barrier function in in vitro models of intestinal disease. Gastroenterology. 2002;123:163–172. doi: 10.1053/gast.2002.34235. [DOI] [PubMed] [Google Scholar]
- Scott KG, Meddings JB, Kirk DR, Lees-Miller SP, Buret AG. Intestinal infection with Giardia spp. reduces epithelial barrier function in a myosin light chain kinase-dependent fashion. Gastroenterology. 2002;123:1179–1190. doi: 10.1053/gast.2002.36002. [DOI] [PubMed] [Google Scholar]
- Wisdom R. AP-1: one switch for many signals. Exp Cell Res. 1999;253:180–185. doi: 10.1006/excr.1999.4685. [DOI] [PubMed] [Google Scholar]
- Landers CJ, Cohavy O, Misra R, Yang H, Lin YC, Braun J, Targan SR. Selected loss of tolerance evidenced by Crohn’s disease-associated immune responses to auto- and microbial antigens. Gastroenterology. 2002;123:689–699. doi: 10.1053/gast.2002.35379. [DOI] [PubMed] [Google Scholar]
- D’Haens GR, Geboes K, Peeters M, Baert F, Penninckx F, Rutgeerts P. Early lesions of recurrent Crohn’s disease caused by infusion of intestinal contents in excluded ileum. Gastroenterology. 1998;114:262–267. doi: 10.1016/s0016-5085(98)70476-7. [DOI] [PubMed] [Google Scholar]
- Sadlack B, Lohler J, Schorle H, Klebb G, Haber H, Sickel E, Noelle RJ, Horak I. Ulcerative colitis like disease in mice with a disrupted interleukin-2 gene. Cell. 1992;5:253–261. doi: 10.1016/0092-8674(93)80067-o. [DOI] [PubMed] [Google Scholar]
- Rocha F, Laughlin R, Musch MW, Hendrickson BA, Chang EB, Alverdy J. Surgical stress shifts the intestinal Escherichia coli population to that of a more adherent phenotype: role in barrier regulation. Surgery. 2001;130:65–73. doi: 10.1067/msy.2001.115360. [DOI] [PubMed] [Google Scholar]
- Levenstein S, Prantera C, Varvo V, Scribano ML, Andreoli A, Luzi C, Arca M, Berto E, Milite G, Marcheggiano A. Stress and exacerbation in ulcerative colitis: a prospective study of patients enrolled in remission. Am J Gastroenterol. 2000;95:1213–1220. doi: 10.1111/j.1572-0241.2000.02012.x. [DOI] [PubMed] [Google Scholar]
- Smecuol E, Bai JC, Sugai E, Vazquez H, Niveloni S, Pedreira S, Maurino E, Meddings J. Acute gastrointestinal permeability responses to different non-steroidal anti-inflammatory drugs. Gut. 2001;49:650–655. doi: 10.1136/gut.49.5.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderholm JD, Olaison G, Lindberg E, Hannestad U, Vindels A, Tysk C, Jarnerot G, Sjodahl R. Different intestinal permeability patterns in relatives and spouses of patients with Crohn’s disease: an inherited defect in mucosal defence? Gut. 1999;44:96–100. doi: 10.1136/gut.44.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamora SA, Hilsden RJ, Meddings JB, Butzner JD, Scott RB, Sutherland LR. Intestinal permeability before and after ibufrofen in families of children with Crohn’s disease. Can J Gastroenterol. 1999;13:31–36. doi: 10.1155/1999/457315. [DOI] [PubMed] [Google Scholar]
- Maric I, Holt PG, Perdue MH, Bienenstock J. Class II MHC antigen (Ia)-bearing dendritic cells in the epithelium of the rat intestine. J Immunol. 1996;156:1408–1414. [PubMed] [Google Scholar]
- Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, Granucci F, Kraehenbuhl J-P, Ricciardi-Castagnoli P. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–367. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- Goosney DL, de Grado M, Finlay BB. Putting E. coli on a pedestal: a unique system to study signal transduction and the actin cytoskeleton. Trends Cell Biol. 1999;9:11–14. doi: 10.1016/s0962-8924(98)01418-4. [DOI] [PubMed] [Google Scholar]
- Swidsinski A, Ladhoff A, Pernthaler A, Swidsinski S, Loening-Baucke V, Ortner M, Weber J, Hoffmann U, Schriber S, Dietel M, Lochs H. Mucosal flora in inflammatory bowel disease. Gastroenterology. 2002;122:44–54. doi: 10.1053/gast.2002.30294. [DOI] [PubMed] [Google Scholar]
- Michaud-Darfeuille A, Neut C, Barnich N, Lederman E, Di Martino P, Desreumaux P, Gambiez L, Joly B, Cortot A, Colombel JF. Presence of adherent Escherichia coli strains on ileal mucosa of patients with Crohn’s disease. Gastroenterology. 1998;115:1405–1413. doi: 10.1016/s0016-5085(98)70019-8. [DOI] [PubMed] [Google Scholar]