Abstract
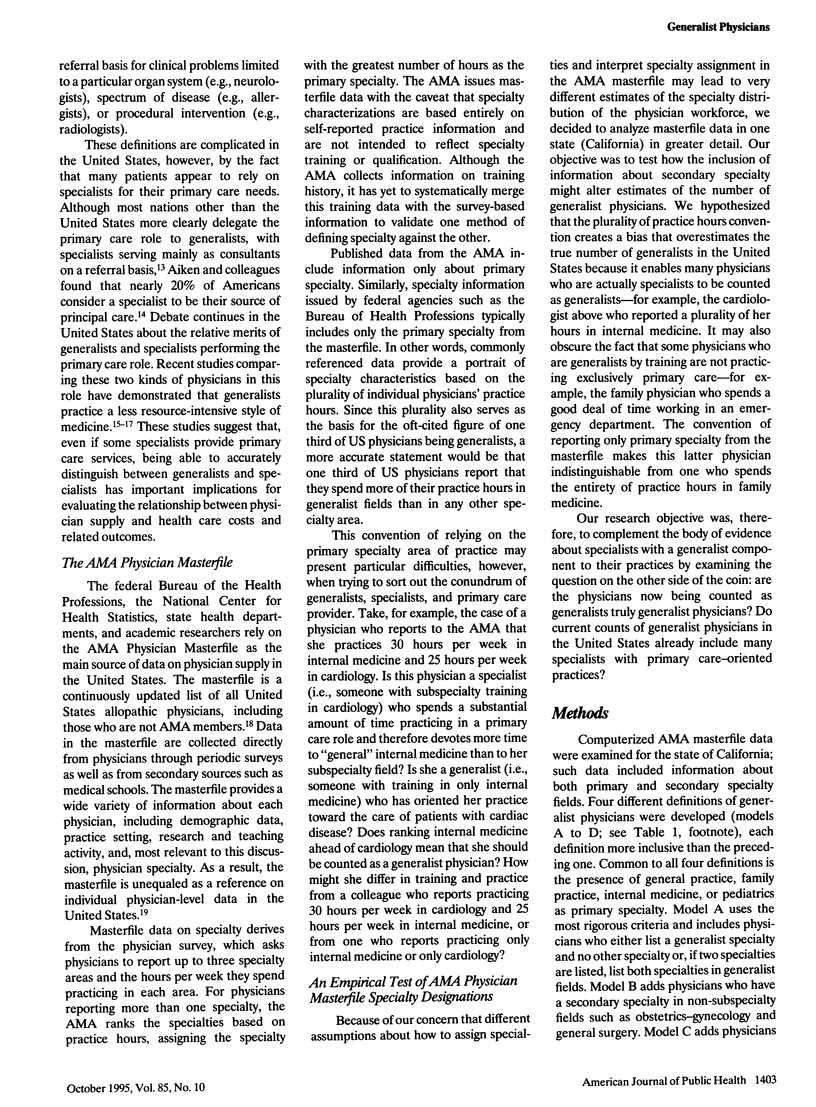
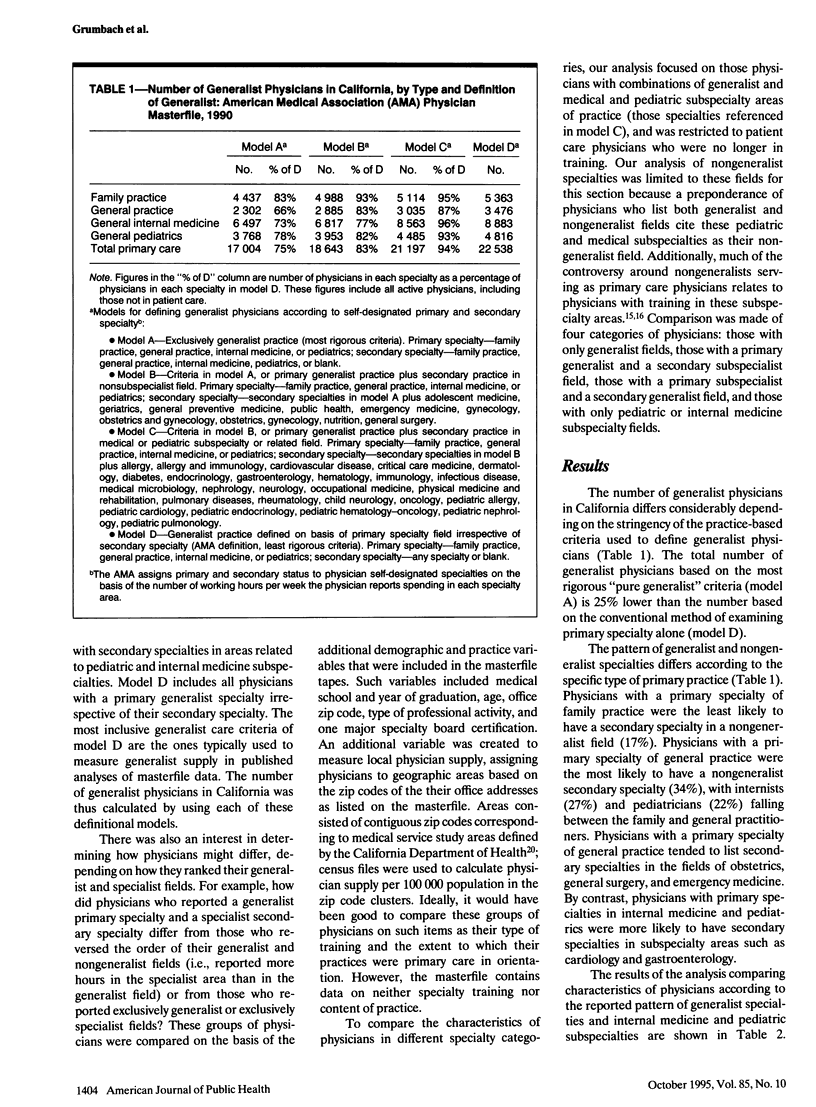
OBJECTIVES. The study reviewed methods for measuring the specialty distribution of the US physician workforce. It was hypothesized that current databases and measurement conventions overestimate the number of generalist physicians. METHODS. A descriptive analysis of the American Medical Association (AMA) Physician Masterfile for California was done with different assumptions about the definition of generalists based on primary and secondary specialty information. RESULTS. A rigorous definition of generalist physician that excludes physicians with secondary practices in specialist fields resulted in an estimate of generalist physicians 25% lower than the number estimated by conventional workforce evaluation methods. Physicians who reported practicing in both generalist and specialist fields were more likely to be older, to be international medical school graduates, and to be in solo or duo practice compared with physicians who listed only generalist or specialist fields. CONCLUSIONS. The actual number of generalist physicians in the United States may be less than previously believed. Although the exact magnitude of the "hidden system" of specialists providing primary care is difficult to measure, at least a portion appear to already be counted as generalist physicians by current conventions.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aiken L. H., Lewis C. E., Craig J., Mendenhall R. C., Blendon R. J., Rogers D. E. The contribution of specialists to the delivery of primary care. N Engl J Med. 1979 Jun 14;300(24):1363–1370. doi: 10.1056/NEJM197906143002404. [DOI] [PubMed] [Google Scholar]
- Franks P., Nutting P. A., Clancy C. M. Health care reform, primary care, and the need for research. JAMA. 1993 Sep 22;270(12):1449–1453. [PubMed] [Google Scholar]
- Greenfield S., Nelson E. C., Zubkoff M., Manning W., Rogers W., Kravitz R. L., Keller A., Tarlov A. R., Ware J. E., Jr Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992 Mar 25;267(12):1624–1630. [PubMed] [Google Scholar]
- Grumbach K., Fry J. Managing primary care in the United States and in the United Kingdom. N Engl J Med. 1993 Apr 1;328(13):940–945. doi: 10.1056/NEJM199304013281308. [DOI] [PubMed] [Google Scholar]
- Grumbach K., Lee P. R. How many physicians can we afford? JAMA. 1991 May 8;265(18):2369–2372. [PubMed] [Google Scholar]
- Kassebaum D. G., Szenas P. L. Specialty preferences of 1993 medical school graduates. Acad Med. 1993 Nov;68(11):866–869. [PubMed] [Google Scholar]
- Kindig D. A. Counting generalist physicians. JAMA. 1994 May 18;271(19):1505–1507. [PubMed] [Google Scholar]
- Kindig D. A., Cultice J. M., Mullan F. The elusive generalist physician. Can we reach a 50% goal? JAMA. 1993 Sep 1;270(9):1069–1073. [PubMed] [Google Scholar]
- Manu P., Schwartz S. E. Patterns of diagnostic testing in the academic setting: the influence of medical attendings' subspecialty training. Soc Sci Med. 1983;17(18):1339–1342. doi: 10.1016/0277-9536(83)90193-4. [DOI] [PubMed] [Google Scholar]
- Martini C. J., Grenholm G. Institutional responsibility in graduate medical education and highlights of historical data. JAMA. 1993 Sep 1;270(9):1053–1060. [PubMed] [Google Scholar]
- Moore F. D., Priebe C. Board-certified physicians in the United States, 1971-1986. N Engl J Med. 1991 Feb 21;324(8):536–543. doi: 10.1056/NEJM199102213240806. [DOI] [PubMed] [Google Scholar]
- Petersdorf R. G. The doctor is in. Acad Med. 1993 Feb;68(2):113–117. doi: 10.1097/00001888-199302000-00001. [DOI] [PubMed] [Google Scholar]
- Rivo M. L., Jackson D. M., Clare F. L. Comparing physician workforce reform recommendations. JAMA. 1993 Sep 1;270(9):1083–1084. [PubMed] [Google Scholar]
- Schroeder S. A., Sandy L. G. Specialty distribution of U.S. physicians--the invisible driver of health care costs. N Engl J Med. 1993 Apr 1;328(13):961–963. doi: 10.1056/NEJM199304013281312. [DOI] [PubMed] [Google Scholar]
- Schroeder S. A. The making of a medical generalist. Health Aff (Millwood) 1985 Summer;4(2):22–46. doi: 10.1377/hlthaff.4.2.22. [DOI] [PubMed] [Google Scholar]
- Schwartz A., Ginsburg P. B., LeRoy L. B. Reforming graduate medical education. Summary report of the Physician Payment Review Commission. JAMA. 1993 Sep 1;270(9):1079–1082. doi: 10.1001/jama.270.9.1079. [DOI] [PubMed] [Google Scholar]
- Smeloff E. A., Burnett W. H., Kelzer P. J. A geographic framework for coordination of needs assessment for primary medical care in California. Public Health Rep. 1981 Jul-Aug;96(4):310–314. [PMC free article] [PubMed] [Google Scholar]
- Weiner J. P. Forecasting the effects of health reform on US physician workforce requirement. Evidence from HMO staffing patterns. JAMA. 1994 Jul 20;272(3):222–230. [PubMed] [Google Scholar]


