Abstract
C1-inhibitor (C1-INH) is a major regulator of the complement classical pathway. Besides this action, it may also inhibit other related inflammatory systems. We have studied the effect of C1-INH in C57BL/6 mice with focal transient brain ischemia induced by 30 minutes of occlusion of the middle cerebral artery. C1-INH induced a dose-dependent reduction of ischemic volume that, with the dose of 15 U/mouse, reached 10.8% of the volume of saline-treated mice. Four days after ischemia the treated mice had significantly lower general and focal neurological deficit scores. Fluoro-Jade staining, a marker for neuronal degeneration, showed that C1-INH-treated mice had a lower number of degenerating cells. Leukocyte infiltration, as assessed by CD45 immunostaining, was also markedly decreased. We then investigated the response to ischemia in C1q−/− mice. There was a slight, nonsignificant decrease in infarct volume in C1q−/− mice (reduction to 72.3%) compared to wild types. Administration of C1-INH to these mice was still able to reduce the ischemic volume to 31.4%. The study shows that C1-INH has a strong neuroprotective effect on brain ischemia/reperfusion injury and that its action is independent from C1q-mediated activation of classical pathway.
C1-inhibitor (C1-INH) is an acute phase protein belonging to the superfamily of serine protease inhibitors called serpins. It is the only known physiological inhibitor of C1s and C1r, the activated homologous serin proteases of the first component of the complement, thus playing an essential role as a regulator of complement classical pathway in blood and tissue.1 C1-INH is also one of the major inhibitors of plasma kallikrein and activated factor XII of the contact-kinin system.2,3 Beside this essential role as regulator of the activation of complement classical pathway and of contact-kinin systems, there is evidence that C1-INH can also inhibit the complement lectin pathway proteases (MASP-1 and MASP-2), and the complement alternative pathway (C3b), plasmin, activated factor XI, plasminogen activator, and glandular kallikrein thus acting as a multifunctional regulator of the various kinin-generating cascade systems.2–5
Observations in patients receiving C1-INH as a replacement therapy for C1-INH deficiency, and studies in animal experimental models suggest that this molecule may be beneficial in clinical conditions in which activation of the complement and contact systems occurs.2,6–9 A common feature to these systems is that on activation they give rise to biologically active peptides, including bradykinin (contact system) and anaphylatoxins (complement system) endowed with proinflammatory effects. Ischemia-reperfusion brain injury is accompanied by a marked inflammatory reaction that contributes to the evolution of tissue injury by several possible mechanisms including production of toxic mediators by activated glial and inflammatory cells and microvascular obstruction by neutrophils.10,11 Complement is known to be activated in human stroke12 as well as in experimental models of cerebral ischemia.13–15 However studies aimed at evaluating the effects of complement inhibition in cerebral ischemia and ischemia-reperfusion injury have not reached definite conclusions.13,16–21 Reports that selective blockade of bradykinin B2 receptors reduce selected aspects of brain injury after cerebral ischemia22–25 suggest a role for the contact-kinin system in ischemia-reperfusion injury. Moreover the activation of the contact-kinin system in stroke patients has been recently proved.26
We have previously shown that C1-INH significantly decreases the ischemic lesion in CD1 mice.19 We have now verified the protective effect of C1-INH in C57BL/6 mice because the genetic background of different mouse strains may affect the sensitivity to ischemia27–29 and we further analyzed the characteristics of the protection by exploring the dose-response and the time-window of its effect. We have also studied the effect of C1-INH on the neurodegeneration and on the inflammatory responses of ischemic mice. We have then specifically addressed the involvement of classical complement pathway activation in the protective effect of C1-INH using mice carrying a targeted deletion of the gene encoding C1q (C57BL/6.C1qa−/−, classical pathway deficiency).27,30 These mice have no overt phenotype with no evidence of autoimmunity. On intraperitoneal exposure to prions they show partial or full protection against spongiform encephalopathy.31,32
Materials and Methods
Animals
Male C57BL/6 mice (26 to 28 g; Charles River, Calco, Italy) and mice carrying a targeted deletion of the gene encoding C1q on C57BL/6 genetic background27 (C1q−/−, kindly provided by Marina Botto, Imperial College School of Medicine), were housed five per cage and kept at constant temperature (21 ± 1°C) and relative humidity (60%) with regular light/dark schedule (7 a.m. to 7 p.m.). Food (Altromin pellets for mice) and water were available ad libitum. Procedures involving animals and their care were conducted in conformity with institutional guidelines that are in compliance with national (D.L. n.116, G.U. suppl. 40, 18 February 1992) and international laws and policies (EEC Council Directive 86/609, OJ L 358,1; Dec.12, 1987; National Institutes of Health Guide for the Care and Use of Laboratory Animals, United States National Research Council, 1996).
Surgery
Transient focal cerebral ischemia was achieved by middle cerebral artery occlusion as previously described.19 Anesthesia was induced by 5% isoflurane in N2O/O2 (70/30%) mixture and maintained by 1.5 to 2% isoflurane in the same mixture. To confirm the adequacy of the vascular occlusion in each animal, blood flow was measured by laser Doppler flowmetry (Transonic BLF-21) using a flexible 0.5-mm fiberoptic probe (type M, 0.5 mm diameter; Transonic) positioned on the brain surface and secured with impression material on the skull at the following coordinates: AP = −1 mm; L = −3.5 mm.33 Briefly, the left common carotid artery was exposed and the external carotid artery and its branches, including the occipital artery and the superior thyroid artery were isolated and cauterized. The pterytopalatine artery was ligated and the external carotid artery cauterized. A 5-0 monofilament nylon suture, blunted at the tip by heat and coated in poly-l-lysine, was introduced into the internal carotid artery through the external carotid artery stump and advanced to the anterior cerebral artery so as to block its bifurcation into the anterior cerebral artery and the middle cerebral artery. The filament was advanced until a >70% reduction of blood flow, compared to preischemic baseline, was observed. At the end of the 30-minute ischemic period, blood flow was restored by carefully removing the nylon filament.
Drug Treatment
Mice received an intravenous injection of C1-INH (C1 esterase inhibitor, 1 U corresponding to the activity of 1 ml of normal plasma; Baxter-Immuno, Pisa, Italy) or the same volume (150 μl) of saline at different doses and at different times from ischemia.
Quantification of Infarct Size and Volume
Mice were deeply anesthetized with Equitensin (120 μl/mice i.p.) and brains were rapidly frozen by immersion in isopentane at −45°C for 3 minutes before being sealed into vials and stored at −70°C until use. For lesion size determination, 40-μm coronal brain sections were cut serially at 320-μm intervals and stained with neutral red (Neutral Red Gurr Certistain; BDH, UK).19 On each slice, infarcted areas were assessed blindly and delineated by the relative paleness of histological staining. The infarcted area was determined by subtracting the area of the healthy tissue in the ipsilateral hemisphere from the area of the contralateral hemisphere on each section. Infarct volumes were calculated by the integration of infarcted areas on each brain slice as quantified with computer-assisted image analyzer and calculated by the Analytical Image System (Imaging Research Inc., Brock University, St. Catharines, Ontario, Canada).
Neurological Deficits
Four days after ischemia, each mouse was rated on two neurological function scales unique to the mouse.19,34 For both scales mice were scored from 0 (healthy mouse) to 28. The score given represents the sum of the results of all categories for each scale. General deficit scale evaluates the hair, ears, eyes, posture, spontaneous activity, and epileptic behavior. Focal deficit scale evaluates the body symmetry, gait, climbing on a surface held at 45°, circling behavior, front limb symmetry, compulsory circling, whisker response to a light touch. All of the experiments were run by a trained investigator blinded to the experimental conditions. Data were expressed as median and 25th to 75th percentiles because intervals between scores are not equal.
Brain Transcardial Perfusion
Mice were deeply anesthetized with Equitensin (120 μl/mouse i.p.) and transcardially perfused with 20 ml of phosphate-buffered saline (PBS) 0.1 mol/L, pH 7.4, followed by 50 ml of chilled paraformaldehyde (4%) in PBS. After carefully removing the brains from the skull, they were transferred to 30% sucrose in PBS at 4°C overnight for cryoprotection. The brains were then rapidly frozen by immersion in isopentane at −45°C for 3 minutes before being sealed into vials and stored at −70°C until use.
Fluoro-Jade Labeling
Fluoro-Jade labeling was performed on perfused brains.35 Briefly, 20-μm mounted sections were dried and rehydrated in ethanol (100 to 75%) and distilled water, then they were incubated in 0.06% potassium permanganate, washed in distilled water, and transferred to 0.001% Fluoro-Jade staining solution. After staining, the sections were rinsed in distilled water, dried, immersed in xylene, and coverslipped.
Immunocytochemistry
Forty-μm-thick coronal sections, prepared from perfused brains as described above, were used for assessment of leukocyte immunostaining. Briefly, free-floating sections were rinsed for 30 minutes in 0.4% Triton X-100 in PBS, 0.1 mol/L, pH 7.4, followed by 15 minutes in 0.1% Triton X-100 and 3% fetal calf serum in PBS. The primary antibody was diluted in 0.1% Triton X-100 in PBS containing 3% fetal calf serum and slices were incubated at 4°C overnight with the biotinylated primary monoclonal antibody (rat anti-mouse CD45, 1:1500; BD Biosciences Pharmingen, San Diego, CA). After three 5-minute washes in PBS, immunoreactivity was tested by the avidin-biotin-peroxidase technique (Vectastain ABC kit; Vector Laboratories, Burlingame, CA). The sections were then reacted by incubation with 3′-3-diaminobenzidine (Sigma, Munich, Germany) in Tris-HCl-buffered saline, pH 7.4, and 0.01% H2O2, and the signal amplified using nickel ammonium. After 3′-3-diaminobenzidine incubation, three 5-minute washes were done with Tris-HCl-buffered saline, then the slices were mounted onto gelatin-coated slides, dried, dehydrated through graded alcohol, fixed in xylene, and coverslipped using DPX mountant (BDH, Poole, UK) before light microscopy analysis.
Results
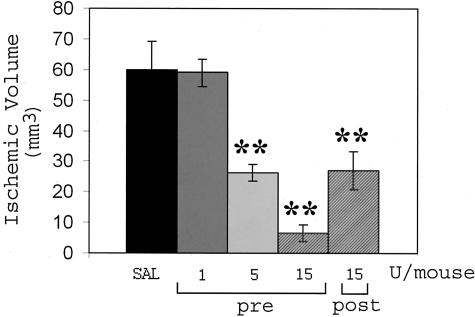
C1-INH-treated C57BL/6 mice had a dose-dependent reduction of ischemic volume that reached 10.8% of the volume of saline-treated mice (60.01 ± 9.32 mm3 and 6.5 ± 2.81 mm3, saline and C1-INH-treated mice, respectively) with the dose of 15 U/mouse (Figure 1). Also 5 U/mouse was able to significantly reduce the ischemic lesion (26.28 ± 4.61 mm3, reduction to 43.8%), whereas 1 U/mouse was ineffective (Figure 1). In all these experiments the inhibitor was given at the beginning of the ischemic period (pre). When given at reperfusion, ie, 30 minutes after the beginning of ischemia, C1-INH was still able to significantly reduce the ischemic volume (27.12 ± 6.22 mm3, reduction to 45.2%, Figure 1), but its efficacy was completely lost when the inhibitor was given after 30 minutes of reperfusion (ie, 60 minutes after the beginning of ischemia).
Figure 1.
Infarct volume assessed 24 hours after ischemia in mice receiving saline (SAL), different doses of C1-INH at the beginning of ischemia (pre), or 15 U at reperfusion (post). Data are expressed as mean ± SEM (n = 6 to 9 mice per group). **, P < 0.01 versus saline, Dunnett test.
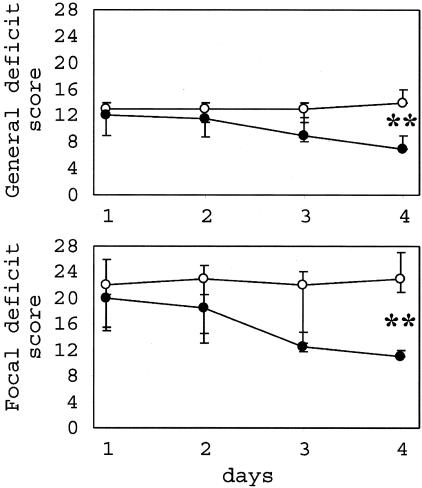
To evaluate if the marked reduction of the ischemic lesion observed 24 hours after ischemia resulted in a reduced functional impairment, neurological deficits were evaluated daily, starting from day 1 for 4 days, in mice receiving saline or 15 U/mouse of C1-INH pre (Figure 2). At day 4, although saline-treated mice showed stable scores, those who received CI-INH had significantly reduced general (14 and 7, medians of saline- and C1-INH-treated mice, respectively; Figure 2, top) and focal (23 and 11, medians of saline- and C1-INH-treated mice, respectively; Figure 2, bottom) deficit scores.
Figure 2.
General and focal neurological deficit score evaluation (0 to 28) assessed daily in ischemic mice treated with 15 U of C1-INH at the beginning of ischemia (black dots, n = 8) or with saline (white dots, n = 9). Data are expressed as median and 25th to 75th percentiles. Differences between curves were evaluated by two-way analysis of variance for repeated measures. Differences between scores at a given time were evaluated by Fisher’s exact test. **, P < 0.01.
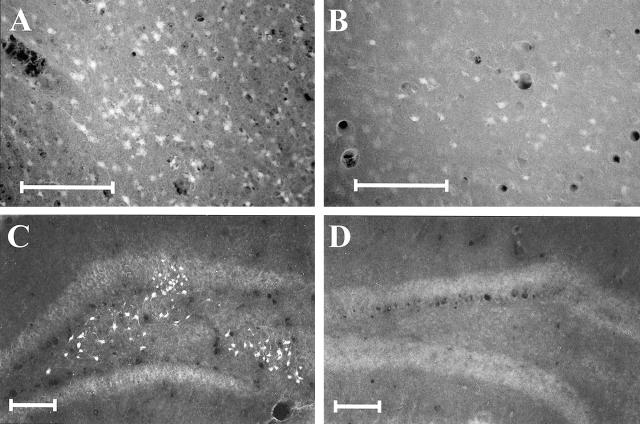
In the same mice we then analyzed the effect of ischemia and C1-INH treatment on neurodegeneration to assess if neurons were actually spared by the inhibitor treatment. The staining with Fluoro-Jade, a marker for neuronal degeneration,35 evaluated 4 days after ischemia, showed the presence of degenerating neurons in selected brain areas. In saline-treated mice, positive cells were consistently observed in temporal cortex where they appeared as extended clusters of fluorescent cells (four of four) often amid necrotic tissue (Figure 3A). Few and sparse positive cells could also be detected in hippocampus [dentate gyrus hilus, three mice (Figure 3C) and CA1 pyramidal cells, one mouse], striatum (two mice), and thalamus (two mice). In mice treated with C1-INH the number of degenerating cells was greatly reduced and the general structure of the brain tissue, well preserved compared to saline-treated mice. Three mice of four showed small groups of Fluoro-Jade-positive cells in temporal cortex (Figure 3B). Positive cells could not be found in the other brain regions in these mice.
Figure 3.
Fluoro-Jade labeling of degenerating neurons in different brain areas of representative ischemic mice 4 days after ischemia. Clusters of Fluoro-Jade-positive neurons amid a necrotic tissue can be observed in the cortex of saline-treated mice (A), whereas only a few scattered fluorescent cells can be found in the same brain area of mice treated with C1-INH (B). Several groups of positive cells can be observed in dentate gyrus of saline-treated (C), but not C1-INH-treated mice (D). Scale bars, 100 μm.
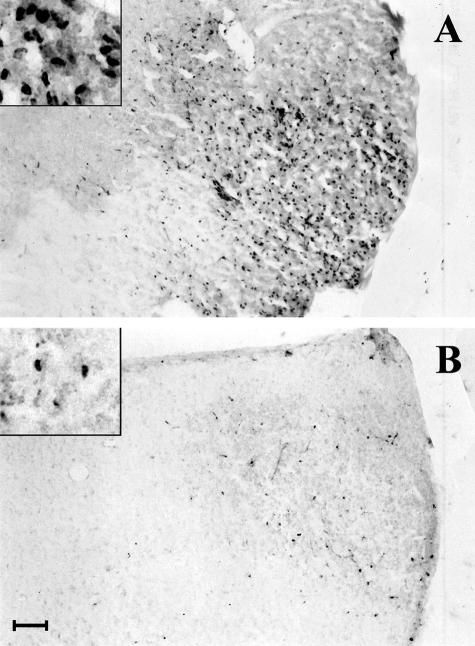
Leukocyte infiltration was then evaluated by CD45 immunostaining. Twenty-four hours after ischemia, infiltrating leukocytes were clearly detectable in hypothalamus (Figure 4A) and few, sparse cells were present in cortex, hippocampus and striatum (not shown). C1-INH administration (15 U/mouse, pre) strongly reduced leukocyte infiltration and only few cells could be observed in the hypothalamic area (Figure 4B).
Figure 4.
Leukocyte infiltrating the hypothalamic area in ischemic mice treated with saline (A) or C1-INH (B) as in Figure 2, 24 hours after ischemia. Scale bar, 100 μm. Insets show CD45-positive cells at higher magnification.
Because C1-INH, besides being a potent inhibitor of the complement classical pathway, may also act on lectin and alternative pathways and on other related inflammatory systems, we set to investigate the response to ischemia in C1q−/− mice. There was a slight, nonsignificant decrease in infarct volume in C1q−/− mice (43.42 ± 6.73 mm3, reduction to 72.3%) compared to wild types (C57BL/6, see above). Administration of C1-INH (15 U/mouse, pre) to C1q−/− mice was still able to exert its neuroprotective effects as shown by the significant reduction of the ischemic volume to 33% (18.2 ± 5.05 mm3) (Figure 5).
Figure 5.
Infarct volume assessed 24 hours after ischemia in C1q−/− mice receiving saline (SAL) or 15 U of C1-INH at the beginning of ischemia. For comparison the ischemic volume of wild types (C57BL/6 mice) is also reported (black column, see Figure 1). Data are expressed as mean ± SEM (n = 7 to 10 mice per group). **, P < 0.01 versus wild types (black column); ○, P < 0.05 versus C1q−/− (gray column), Tukey-Kramer test.
Discussion
This study shows the powerful neuroprotective action of C1-INH and establishes that this action does not require the presence of C1q. C1-INH dose dependently reduced the ischemic volume. The highest dose used, 15 U/mouse, was able to reduce the ischemic volume to 10.8%, a remarkably high degree of protection, and 5 U/mouse reduced it to 43.8%, still a highly significant effect. Data obtained measuring C1-INH activity in mouse plasma showed that the inhibitor is cleared within 1 hour (data not shown), whereas in humans the C1-INH half-life is ∼35 hours,36 indicating that C1-INH doses used in this study cannot be directly compared to those used in humans. Notably the minimal effective dose (5 U) is only 1.8 times the safe loading dose used in humans.36 The present finding confirms and extends our previous data and all together show the marked protective action of this inhibitor that is effective on both inbred and outbred mouse strains.19 Its efficacy in brain ischemia-reperfusion injury has recently been described also in rats.37
Administration of C1-INH at the beginning of ischemia or at the beginning of reperfusion markedly reduced the ischemic volume, whereas the effect was lost when it was administered after 30 minutes of reperfusion. The early and narrow time window of the protection shows the critical role of the systems inhibited by C1-INH in the very first phase of reperfusion of the ischemic brain. We have previously shown a marked C1-INH immunostaining in the brain capillary endothelium and in the tissue around them, indicating that the inhibitor can reach the brain compartment where it could possibly act.19 However our data do not allow to draw conclusions on which is the compartment relevant to C1-INH neuroprotection, plasma, brain tissue, or both.
The use of Fluoro-Jade staining to evidence degenerating neuronal cells, allowed us to investigate whether C1-INH action resulted in sparing of these cells. Preliminary experiments showed that 24 hours after ischemia, Fluoro-Jade-positive cells were less in C1-INH-treated mice compared to mice receiving saline (data not shown). To assess if this effect was because of a delay in degenerating processes or to a real neuroprotection induced by the treatment, we then analyzed Fluoro-Jade-positive cells 4 days after ischemia and fully confirmed the observation that neurodegeneration was actually inhibited by C1-INH treatment.
We then investigated whether C1-INH, being a major inhibitor of inflammatory systems, could affect given aspects of the inflammatory response. C1-INH induced a marked reduction of leukocyte infiltration in the brain tissue. As documented in experimental animal models as well as in patients, after ischemia leukocytes accumulate in brain parenchyma as a consequence of a cascade of events including margination, adhesion, and transmigration through the vessel wall.38–40 This represents an important aspect of the inflammatory response triggered by the ischemic event. These cells contribute to the evolution of tissue injury by several possible mechanisms including microvascular obstruction by neutrophils and production of cytokines and other toxic mediators.10,11 An additional important aspect when assessing the protective effect of a compound on ischemia-reperfusion injury is the evaluation of functional deficits. C1-INH induces a progressive recovery in both general and focal neurological deficits indicating an amelioration of the appearance of the mice, their motor performance, their reactivity, and response to stimuli. All these data show that C1-INH is a powerful neuroprotective agent.
The experiments performed using C1q−/− mice show only a slight decrease in ischemic volume compared to wild types, indicating that ischemia-reperfusion brain injury is not dependent on C1q. Interestingly, recent data on gastrointestinal ischemia-reperfusion injury report a similar observation.41 In view of the several substrates on which C1-INH may act (see Introduction), the finding that this inhibitor is still able to markedly reduce the reperfusion injury in C1q−/− mice, opens the question of which is the action that results in neuroprotection. Recent data from studies in different organs now support the view that inhibition of classical, lectin, or alternative complement pathway, is beneficial to reduce ischemia reperfusion injury.2,3,5,42 Furthermore, the presence of tissue kallikrein in the brain tissue43 and the identification of bradykinin B2 receptors on brain cells44,45 are in line with a role also for this system in nervous system pathophysiology. Specifically, the involvement of the contact-kinin system in ischemia-reperfusion injury is supported by data showing the effectiveness of bradykinin B2 receptor antagonists in reducing ischemic brain damage.22–25 Accumulating evidence suggests that these pathways may be not as independent as originally thought, and their complex cross-talk and interplay has not allowed dissection of each other specific role yet.4
In conclusion the present study shows that: 1) C1-INH has a strong neuroprotective effect; 2) it acts on a system that is crucial in the early phases of the ischemic injury development; 3) its action is independent from C1q-mediated activation of classical pathway; 4) other complement pathways or inflammatory systems, possibly the contact-kinin system, may be involved in ischemia-reperfusion injury. Blockade of such systems can reduce the numerous inflammatory reactions that in turn condition the postischemic brain function.
Footnotes
Address reprint requests to Maria Grazia De Simoni, Laboratory of Inflammation and Nervous System Diseases, Mario Negri Institute, via Eritrea, 62, 20157 Milano, Italy. E-mail: desimoni@marionegri.it.
Partially supported by the “Ministero dell’Istruzione, dell’Universita’ e della Ricerca, FIRB” (project code RBAU01RXS2).
References
- Cai S, Davis AE., III Complement regulatory protein C1 inhibitor binds to selectins and interferes with endothelial-leukocyte adhesion. J Immunol. 2003;171:4786–4791. doi: 10.4049/jimmunol.171.9.4786. [DOI] [PubMed] [Google Scholar]
- Caliezi C, Wuillenin WA, Zeerleder S, Redondo M, Eisele B, Hack CE. C1 esterase inhibitor: an anti-inflammatory agent and its potential use in the treatment of diseases other than hereditary angioedema. Pharmacol Rev. 2000;52:91–112. [PubMed] [Google Scholar]
- Kirschfink M, Mollnes TE. C1-inhibitor: an anti-inflammatory reagent with therapeutic potential. Expert Opin Pharmacother. 2001;2:1073–1083. doi: 10.1517/14656566.2.7.1073. [DOI] [PubMed] [Google Scholar]
- Riedemann NC, Ward PA. Complement in ischemia reperfusion injury. Am J Pathol. 2003;162:363–367. doi: 10.1016/S0002-9440(10)63830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H, Wagner E, Zhang H, Frank MM. Complement 1 inhibitor is a regulator of the alternative complement pathway. J Exp Med. 2001;194:1609–1616. doi: 10.1084/jem.194.11.1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agostoni A, Cicardi M. Hereditary and acquired C1-inhibitor deficiency: biological and clinical characteristics in 235 patients. Medicine (Baltimore) 1992;71:206–215. doi: 10.1097/00005792-199207000-00003. [DOI] [PubMed] [Google Scholar]
- Bork K, Barnstedt SE. Treatment of 193 episodes of laryngeal edema with C1 inhibitor concentrate in patients with hereditary angioedema. Arch Intern Med. 2001;161:714–718. doi: 10.1001/archinte.161.5.714. [DOI] [PubMed] [Google Scholar]
- Nussberger J, Cugno M, Amstutz C, Cicardi M, Pellacani A, Agostoni A. Plasma bradykinin in angio-oedema. Lancet. 1998;351:1693–1697. doi: 10.1016/S0140-6736(97)09137-X. [DOI] [PubMed] [Google Scholar]
- Han ED, MacFarlane RC, Mulligan AN, Scafidi J, Davis AE., III Increased vascular permeability in C1 inhibitor-deficient mice mediated by the bradykinin type 2 receptor. J Clin Invest. 2002;109:1057–1063. doi: 10.1172/JCI14211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–397. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- Iadecola C, Alexander M. Cerebral ischemia and inflammation. Curr Opin Neurol. 2001;14:89–94. doi: 10.1097/00019052-200102000-00014. [DOI] [PubMed] [Google Scholar]
- Di Napoli M. Systemic complement activation in ischemic stroke. Stroke. 2001;32:1443–1448. doi: 10.1161/01.str.32.6.1443-a. [DOI] [PubMed] [Google Scholar]
- Huang J, Kim LJ, Mealey R, Marsh HC, Jr, Zhang Y, Tenner AJ, Connolly ES, Jr, Pinsky DJ. Neuronal protection in stroke by an sLex-glycosylated complement inhibitory protein. Science. 1999;285:595–599. doi: 10.1126/science.285.5427.595. [DOI] [PubMed] [Google Scholar]
- Schafer MK, Schwaeble WJ, Post C, Salvati P, Calabresi M, Sim RB, Petry F, Loos M, Weihe E. Complement C1q is dramatically up-regulated in brain microglia in response to transient global cerebral ischemia. J Immunol. 2000;164:5446–5452. doi: 10.4049/jimmunol.164.10.5446. [DOI] [PubMed] [Google Scholar]
- van Beek J, Elward K, Gasque P. Activation of complement in the central nervous system: roles in neurodegeneration and neuroprotection. Ann NY Acad Sci. 2003;992:56–71. doi: 10.1111/j.1749-6632.2003.tb03138.x. [DOI] [PubMed] [Google Scholar]
- Vasthare US, Barone FC, Sarau HM, Rosenwasser RH, Di Martino M, Young WF, Tuma RF. Complement depletion improves neurological function in cerebral ischemia. Brain Res Bull. 1998;45:413–419. doi: 10.1016/s0361-9230(97)00408-5. [DOI] [PubMed] [Google Scholar]
- Heimann A, Takeshima T, Horstick G, Kempski O. C1-esterase inhibitor reduces infarct volume after cortical vein occlusion. Brain Res. 1999;838:210–213. doi: 10.1016/s0006-8993(99)01740-0. [DOI] [PubMed] [Google Scholar]
- Liu XH, Kwon D, Schiele GP, Yang GY, Silverstein FS, Barks JDE. Mice deficient interleukin-1 converting enzyme are resistant to neonatal hypoxic/ischemic brain damage. J Cereb Blood Flow Metab. 1999;19:1099–1108. doi: 10.1097/00004647-199910000-00006. [DOI] [PubMed] [Google Scholar]
- De Simoni MG, Storini C, Barba M, Catapano L, Arabia AM, Rossi E, Bergamaschini L. Neuroprotection by complement (C1) inhibitor in mouse transient brain ischemia. J Cereb Blood Flow Metab. 2003;23:232–239. doi: 10.1097/01.WCB.0000046146.31247.A1. [DOI] [PubMed] [Google Scholar]
- Lew SM, Gross CE, Bednar MM, Russel SJ, Fuller SP, Ellenberger CL, Howard D. Complement depletion does not reduce brain injury in a rabbit model of thromboembolic stroke. Brain Res Bull. 1999;48:325–331. doi: 10.1016/s0361-9230(99)00004-0. [DOI] [PubMed] [Google Scholar]
- Lassiter HA, Feldhoff RC, Dabhia N, Parker JC, Jr, Feldhoff PW. Complement inhibition does not reduce post-hypoxic-ischemic cerebral injury in 21-day-old rats. Neurosci Lett. 2001;302:37–40. doi: 10.1016/s0304-3940(01)01653-6. [DOI] [PubMed] [Google Scholar]
- Relton JK, Beckey VE, Hanson WL, Whalley ET. CP-0597, a selective bradykinin B2 receptor antagonist, inhibits brain injury in a rat model of reversible middle cerebral artery occlusion. Stroke. 1997;28:1430–1436. doi: 10.1161/01.str.28.7.1430. [DOI] [PubMed] [Google Scholar]
- Zausinger S, Lumenta DB, Pruneau D, Schmid-Elsaesser R, Plesnila N, Baethmann A. Effects of LF 16–0687 Ms, a bradykinin B(2) receptor antagonist, on brain edema formation and tissue damage in a rat model of temporary focal cerebral ischemia. Brain Res. 2002;950:268–278. doi: 10.1016/s0006-8993(02)03053-6. [DOI] [PubMed] [Google Scholar]
- Lehmberg J, Beck J, Baethmann A, Uhl E. Bradykinin antagonists reduce leukocyte-endothelium interactions after global cerebral ischemia. J Cereb Blood Flow Metab. 2003;23:441–448. doi: 10.1097/01.WCB.0000052280.23292.35. [DOI] [PubMed] [Google Scholar]
- Ding-Zhou L, Margaill I, Palmier B, Pruneau D, Plotkine M, Marchand-Verrecchia C. LF 16–0687 Ms, a bradykinin B2 receptor antagonist, reduces ischemic brain injury in a murine model of transient focal cerebral ischemia. Br J Pharmacol. 2003;139:1539–1547. doi: 10.1038/sj.bjp.0705385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner S, Kalb P, Lukosava M, Hilgenfeldt U, Schwaninger M. Activation of the tissue kallikrein-kinin system in stroke. J Neurol Sci. 2002;202:75–76. doi: 10.1016/s0022-510x(02)00208-3. [DOI] [PubMed] [Google Scholar]
- Mitchell DA, Pickering MC, Warren J, Fossati-Jimack L, Cortes-Hernandez J, Cook HT, Botto M, Walport MJ. C1q deficiency and autoimmunity: the effects of genetic background on disease expression. J Immunol. 2002;168:2538–2543. doi: 10.4049/jimmunol.168.5.2538. [DOI] [PubMed] [Google Scholar]
- Lambertsen KL, Gregersen R, Finsen B. Microglial-macrophage synthesis of tumor necrosis factor after focal cerebral ischemia in mice is strain dependent. J Cereb Blood Flow Metab. 2002;22:785–797. doi: 10.1097/00004647-200207000-00004. [DOI] [PubMed] [Google Scholar]
- Fujii M, Hara H, Meng W, Vonsattel JP, Huang Z, Moskowitz MA. Strain-related differences in susceptibility to transient forebrain ischemia in SV-129 and C57black/6 mice. Stroke. 1997;28:1805–1811. doi: 10.1161/01.str.28.9.1805. [DOI] [PubMed] [Google Scholar]
- Botto M, Dell’Angola C, Bygrave AE, Thompson EM, Cook HT, Petry F, Loos M, Pandolfi PP, Walport MJ. Homozygous C1q deficiency causes glomerulonephritis associated with multiple apoptotic bodies. Nat Genet. 1998;19:56–59. doi: 10.1038/ng0598-56. [DOI] [PubMed] [Google Scholar]
- Klein MA, Kaeser PS, Schwarz P, Weyd H, Xenarios I, Zinkernagel RM, Carroll MC, Verbeek JS, Botto M, Walport MJ, Molina H, Kalinke U, Acha-Orbea H, Aguzzi A. Complement facilitates early prion pathogenesis. Nat Med. 2001;7:488–492. doi: 10.1038/86567. [DOI] [PubMed] [Google Scholar]
- Mabbott NA, Bruce ME, Botto M, Walport MJ, Pepys MB. Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nat Med. 2001;7:485–487. doi: 10.1038/86562. [DOI] [PubMed] [Google Scholar]
- Yang GY, Mao Y, Zhou LF, Ye W, Liu XH, Gong C, Lorris Betz A. Attenuation of temporary focal cerebral ischemic injury in the mouse following transfection with interleukin-1 receptor antagonist. Brain Res Mol Brain Res. 1999;72:129–137. doi: 10.1016/s0169-328x(99)00205-3. [DOI] [PubMed] [Google Scholar]
- Clark WM, Lessov NK, Dixon MP, Eckenstein F. Monofilament intraluminal middle cerebral artery occlusion in the mouse. Neurol Res. 1997;19:641–648. doi: 10.1080/01616412.1997.11740874. [DOI] [PubMed] [Google Scholar]
- Schmued LC, Albertson C, Sikker W. Fluoro-Jade: a novel fluorochrome for the sensitive and reliable histochemical localization of neuronal degeneration. Brain Res. 1997;751:37–46. doi: 10.1016/s0006-8993(96)01387-x. [DOI] [PubMed] [Google Scholar]
- de Zwaan C, Kleine AH, Diris JH, Glatz JF, Wellens HJ, Strengers PF, Tissing M, Hack CE, van Dieijen-Visser MP, Hermens WT. Continuous 48-h C1-inhibitor treatment, following reperfusion therapy, in patients with acute myocardial infarction. Eur Heart J. 2002;23:1670–1677. doi: 10.1053/euhj.2002.3191. [DOI] [PubMed] [Google Scholar]
- Akita N, Nakase H, Kaido T, Kanemoto Y, Sakaki T. Protective effect of C1 esterase inhibitor on reperfusion injury in the rat middle cerebral artery occlusion model. Neurosurgery. 2003;52:391–400. doi: 10.1227/01.neu.0000043710.61233.b4. [DOI] [PubMed] [Google Scholar]
- Kato H, Kogure K, Liu XH, Araki T, Itoyama Y. Progressive expression of immunomolecules on activated microglia and invading leukocytes following focal cerebral ischemia in the rat. Brain Res. 1996;734:203–212. [PubMed] [Google Scholar]
- Pozzilli C, Lenzi GL, Argentino C, Carolei A, Rasura M, Signore A, Bozzao L, Pozzilli P. Imaging of leukocytic infiltration in human cerebral infarcts. Stroke. 1985;16:251–255. doi: 10.1161/01.str.16.2.251. [DOI] [PubMed] [Google Scholar]
- Barone FC, Hillegass LM, Price WJ, White RF, Lee EV, Feuerstein GZ, Sarau HM, Clark RK, Griswold DE. Polymorphonuclear leukocyte infiltration into cerebral focal ischemic tissue: myeloperoxidase activity assay and histologic verification. J Neurosci Res. 1991;29:336–345. doi: 10.1002/jnr.490290309. [DOI] [PubMed] [Google Scholar]
- Hart ML, Ceonzo KA, Buras JA, Stahl JL. Gastrointestinal ischemia-reperfusion injury is complement-dependent but not dependent on C1q. Mol Immunol. 2003;40:187. [Google Scholar]
- De Vries B, Matthijsen RA, Wolfs TG, Van Bijnen AA, Heeringa P, Buurman WA. Inhibition of complement factor C5 protects against renal ischemia-reperfusion injury: inhibition of late apoptosis and inflammation. Transplantation. 2003;75:375–382. doi: 10.1097/01.TP.0000044455.05584.2A. [DOI] [PubMed] [Google Scholar]
- Raidoo DM, Bhoola KD. Pathophysiology of the kallikrein-kinin system in mammalian nervous tissue. Pharmacol Ther. 1998;79:105–127. doi: 10.1016/s0163-7258(98)00011-4. [DOI] [PubMed] [Google Scholar]
- Raidoo DM, Ramchurren N, Naidoo Y, Naidoo S, Muller-Esterl W, Bhoola KD. Visualisation of bradykinin B2 receptors on human brain neurons. Immunopharmacology. 1996;33:104–107. doi: 10.1016/0162-3109(96)00021-5. [DOI] [PubMed] [Google Scholar]
- Chen EY, Emerich DF, Bartus RT, Kordower JH. B2 bradykinin receptor immunoreactivity in rat brain. J Comp Neurol. 2000;427:1–18. [PubMed] [Google Scholar]