Abstract
Objective
Negative emotions have been linked to increases in blood pressure, but relations between positive emotion and blood pressure have not been investigated. Our aim was to test the hypothesis that high positive emotion would be associated with lower blood pressure in older adults.
Methods
A cross-sectional study that included 2564 Mexican Americans aged 65 or older living in one of 5 southwestern states. Primary measures included blood pressure and positive emotion score. Data analyses included descriptive and categorical statistics and regression and cumulative logit analysis.
Results
The average age was 72.5 years, 52.8% were women and 32.8% were on anti-hypertensive medication. For individuals not on anti-hypertensive medication, increasing positive emotion score was significantly associated with lower systolic (b= −0.35, SE .10) and diastolic (b= −0.56, SE .07) blood pressure after adjusting for relevant risk factors; for those on anti-hypertensive medication, increasing positive emotion score was significantly associated with lower diastolic (b= −0.46, SE .11) blood pressure, but not systolic blood pressure. Positive emotion was significantly associated with a 4-level joint blood pressure variable. Each 1-point increase in positive emotion score was associated with a 3% and 9% decreased odds of being in a higher blood pressure category for those on (OR 0.97; 95% CI 0.93–1.00) and not on (OR 0.91; 95% CI 0.89–0.93) anti-hypertensive medication, respectively.
Conclusions
Findings indicate an association between high positive emotion and lower blood pressure among older Mexican Americans. Targeting the emotional health of older adults might be considered as part of non-pharmacologic hypertension treatment programs or as part of adjunctive therapy for those on anti-hypertensive medication.
Keywords: Hypertension, blood pressure, aging, positive emotion, Mexican Americans
Hypertension affects about 50 million individuals in the US and about 1 billion worldwide (1). Though progress in prevention, treatment, and control of high blood pressure has been made, hypertension remains a major public health challenge. A large minority of the US population – estimated at 30% – are unaware of their high blood pressure (1). Even more worrying, however, is the apparent lack of awareness that high blood pressure can increase the risk for myocardial infarction, heart failure, stroke and kidney disease. Each 20 mmHg increase in systolic blood pressure doubles the risk for cardiovascular related diseases (2).
Identifiable factors associated with high blood pressure are well-established and include older age, increased weight, physical inactivity, excessive alcohol consumption, smoking, poor diet control, diabetes and genetic predisposition (3, 4). The role of negative emotions such as depression or anxiety in the etiology of hypertension is also supported by research (5, 6). For example, a population-based study of 3310 normotensive and chronic disease-free individuals showed negative emotion as a significant predictor of incident hypertension among whites and African Americans (7).
In the last decade an emerging literature has begun to identify the health benefits of positive emotions (8-10). In older populations, studies show that high positive emotion can reduce the risk of incident disability and mobility limitations, stroke, cardiovascular and all-cause mortality, and can aid in recovery from Coronary Artery Bypass Graft surgery (11-14). Knowing an older person's emotional well-being prior to heart attack, stroke or hip fracture is also a good predictor of functional recovery 1-year post event (15).
Given the strong association between blood pressure and cardiovascular health, an important question is whether high positive emotion is associated with lower blood pressure. A basic element of health is homeostasis (the physiological responses that maintain internal balance) and initial studies suggest that positive emotion may play an important role in keeping the body in balance via chemical and neural responses (16-18). Steptoe et al (19) recently showed an independent association between positive emotion and lower cortisol levels and heart rate, and reduced fibrinogen stress responsivity. There is also some indication that under stressful conditions positive emotions may help promote skills necessary to adapt to and cope with changing life events (20, 21). Taken together, these studies provide theoretical support for an association between positive emotion and blood pressure and may provide insight into why some individuals who belong to underserved or disadvantaged groups appear resilient to poor health outcomes.
Mexican Americans, the largest minority group in the US, are typically disadvantaged in relation to socioeconomic position (with about 20 percent living in households with poverty-level incomes) (22), access to health care and social services compared with their non-Hispanic whites counterparts, and report higher rates of diabetes and obesity (23). Despite these disadvantages, research indicates Mexican Americans to have similar or better health profiles than non-Hispanic whites (24-26). For example, Mexican Americans display lower mortality rates from several of the leading causes of death including cardiovascular diseases and cancer (27). One possible explanation is that lower rates of affective disorders in Mexican Americans compared with non-Hispanic whites create a health advantage (28-30). In the present study, we use data from the Hispanic Established Population for the Epidemiologic Study of the Elderly to examine the role of positive emotion and its association with blood pressure in older Mexican Americans. We hypothesized that high positive emotion would be associated with lower blood pressure.
Method
Sample
The Hispanic Established Population for the Epidemiologic Study of the Elderly (HEPESE) is a population-based study of non-institutionalized Mexican Americans aged 65 years or older. Details of the study design are published elsewhere (31). Briefly, individuals were selected from the five southwestern states of Texas, California, Arizona, Colorado, and New Mexico. The sample design was for a multistage area probability cluster sample that involved selection of counties, census tracts, and households. In the first stage, counties (a small census-based geographical area) were selected if at least 6.6% of the county population was of Mexican American ethnicity. In the second stage, census tracts were selected with a probability proportional to the size of their older (age 65+) Mexican American population, using counts from the 1990 U.S. census. In the third stage, census blocks (small area units within census tracts) were selected at random to obtain at least 400 households within each census tract. These households were screened to identify persons who were older Mexican Americans. The sampling procedure assures a sample that is generalizable to the more than 500,000 older Mexican Americans living in the southwest. The five states in the H-EPESE sampling frame contain 85% of the 65 and older Mexican American population living in the United States. The response rate at baseline interview (1993/1994) was 83% (31). In-home interviews were conducted in Spanish or English and participants gave informed consent. The study was approved by the University of Texas Medical Branch Institutional Review Board.
Exclusion criteria
A total of 486 older Mexican Americans were excluded from the current sample. This included 170 individuals with missing data on blood pressure (n = 88) and anthropometric measures (n = 82) and those who were interviewed by proxy (n = 316). The current sample contained a total of 2564 older individuals.
Measures
Anti-Hypertensive Medication
The use of prescription medications for blood pressure control was assessed by in-person interview, using previously established protocols (32). Individuals were first asked about use of any prescription medications within 2 weeks of the interview, and then asked to show the interviewer all current prescription medications. The interviewers documented the drug name, its dosage form, and strength. A panel of three geriatricians compiled a list of all the medications including brand and fixed-dose combination medications. The generic equivalents were established and the medications were classified into major therapeutic classes and subclasses. Of the 2564 individuals included in the current sample, 841 (32.8 %) were on anti-hypertensive medication.
Systolic and Diastolic Blood Pressure
Systolic and diastolic blood pressures were used as continuous variables and as a 4-level joint categorical variable according to the criteria of the Joint National Committee (JNC) 7 classification system on prevention, detection, evaluation and treatment of hypertension (2). Normotensive was defined as a systolic blood pressure of < 120 mmHg and a diastolic blood pressure of < 80 mmHg, prehypertension as a systolic pressure of 120-139 or a diastolic pressure of 80-89, stage 1 hypertension as a systolic blood pressure of 140-159 mmHg or diastolic blood pressure as 90-99 mmHg and stage 2 hypertension as a systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 100 mm Hg. In the current study, blood pressure was measured using a standard mercury sphygmomanometer with appropriate cuff size after the individual had remained seated for at least 5 minutes, according to the standard protocol used in the Hypertension Detection and Follow-up Program (33). An average of two blood pressure readings was calculated. If the individual had only one blood pressure reading, it was used. Ninety-eight percent of individuals had two blood pressure readings.
Positive emotion
A four-item positive emotion summary scale was created from the 20 item Center for Epidemiologic Studies - Depression (CES-D) scale. Factor analysis has shown the 4 CES-D items to load onto a single positive emotion factor (34-37). The four positive emotion items included: “I felt that I was just as good as other people”, “I felt hopeful about the future”, “I was happy”, and “I enjoyed life” (35). Responses were scored on a four-point scale (0 to 3) ranging from: rarely or none of the time (<1 day per week) to most of the time (5-7 days per week). Summing the responses, the positive emotion scale had a potential range of 0 to 12, where higher scores indicated higher positive emotion. The four items from the positive emotion scale have shown high internal consistency (alpha = .80) and a weak correlation (r = −.25) with the remaining 16 negative emotion items (12).
Covariates
Covariates included sociodemographic characteristics (age, sex, marital status, and years of schooling), health behaviors (current alcohol use and smoking status), and clinical measures (body mass index, depressive symptoms, and self-reported diabetes). Alcohol use was based on the number of drinks (beer, wine or liquor) per week. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Depressive symptoms were calculated by summing the 16 remaining items from the CES-D scale (range of 0 to 48), where higher scores indicate increased depressive symptoms.
Statistical Analysis
Sociodemographic, health behaviors and clinical variables were examined using descriptive and univariate statistics for continuous variables and contingency tables for categorical variables, with significance tests by χ2 analysis. Generalized linear regression models were used to describe associations between positive emotion and systolic and diastolic blood pressure with and without adjustment for relevant risk factors. Risk factors included sociodemographic characteristics, health behaviors, and clinical variables. For general linear models, unstandardized parameter estimates were presented along with corresponding standard errors (SE), p < 0.05 was considered significant. Interactions were tested between positive emotion and covariates including age, gender, marital status, BMI and diabetes on blood pressure using general linear regression models. No significant interactions were identified and these models were not reported.
Cumulative logit models (i.e., ordered logit models) were used to assess associations between the continuous positive emotion score and the 4-level joint systolic and diastolic blood pressure variable using criteria established by the Joint National Committee 7. Each reported odds ratio (and 95% CIs) for the cumulative logit models is interpreted as the effect of the independent variable on the odds of being in a higher blood pressure level rather than in a lower level. The first model examined the univariate association between positive emotion and the 4-level blood pressure measure. The second model added sociodemographic characteristics and health behaviors. The third model included sociodemographic characteristics, health behaviors and clinical measures. Model assumptions for the regression and logit analysis were tested and met. All analyses were performed using SAS statistical software version 9.1 (SAS Institute, Inc. Cary, North Carolina).
Results
The average age of the sample was 72.5 (SD 6.3) years, 52.8% were women and the mean years of schooling was 4.9 (SD 3.8). The mean positive emotion score was 8.2 (SD 3.5). Of those currently on anti-hypertensive medication (n = 841) the mean systolic and diastolic blood pressure was 138.5 mmHg (SD 17.1) and 82.1 mmHg (SD 10.8), respectively. This compared with a mean systolic and diastolic blood pressure of 132.5 mmHg (SD 14.8) and 79.9 mmHg (SD 10.4), respectively, for those not on anti-hypertensive medications (n = 1723).
Table 1 shows the sample population stratified by use of anti-hypertensive medication. There were no statistically significant differences between the two groups in relation to positive emotion score, age, and years of schooling. Individuals on anti-hypertensive medication were significantly more likely to have higher BMI and depressive symptom scores and to report being diabetic. Conversely, individuals not on anti-hypertensive medication were significantly more likely to be men, married, a current smoker, and use alcohol, though the average number of drinks per week in both groups was less than one.
Table 1.
Sociodemographic, health behaviors and clinical measures stratified by use of anti-hypertensive medication (n = 2564).
| Blood Pressure Medication |
|||
|---|---|---|---|
| Explanatory Variable | Yes (n = 841) | No (n = 1723) | p-value |
| Positive emotion, Mean (SD) | 8.3 (3.3) | 8.7 (3.7) | .14 |
| Age, Mean (SD) | 72.7 (6.2) | 72.4 (6.3) | .18 |
| Men, n (%) | 280 (32.3) | 829 (46.4) | .0001 |
| Married, n (%) | 456 (52.7) | 1036 (58.0) | .001 |
| Years of Education, Mean (SD) | 5.0 (3.9) | 4.9 (3.9) | .50 |
| Current smoker, n (%) | 74 (8.5%) | 266 (14.9) | .0001 |
| Alcohol consumption (drinks per week), Mean (SD) | 0.28 (1.54) | 0.45 (1.98) | .03 |
| Body Mass Index, Mean (SD) | 28.9 (5.7) | 27.3 (5.0) | .0001 |
| Diabetes, n (%) | 287 (33.1) | 311 (17.4) | .0001 |
| Depressive symptoms, Mean (SD) | 7.1 (7.8) | 6.0 (7.1) | .0007 |
Figures 1 and 2 show unadjusted associations between positive emotion score and percent with high systolic (BP ≥ 140 mm Hg) and diastolic (BP ≥ 90 mm Hg) blood pressure, respectively, stratified by use of anti-hypertensive medication. For individuals not on anti-hypertensive medication, Figures 1 and 2 show a general trend of association between increasing positive emotion score and lower risk of high systolic (p < .0001) and diastolic (p < .0001) blood pressure. Similarly, for those on anti-hypertensive medication, increasing positive emotion score was significantly associated with lower risk of high diastolic blood pressure (p = .0007); whereas a non-significant association was observed between positive emotion score and high systolic blood pressure (p = .09).
Figure 1.
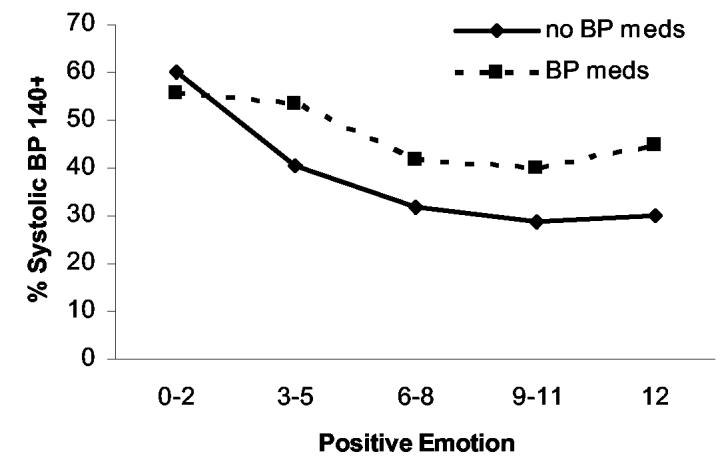
Percentage of older Mexican Americans with high systolic blood pressure by positive emotion score stratified by use of anti-hypertensive medication (p=.0001 no meds; p= .09 meds).
Figure 2.
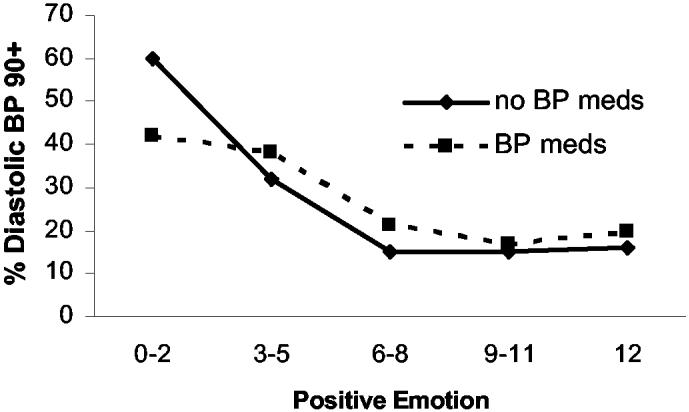
Percentage of older Mexican Americans with high diastolic blood pressure by positive emotion score stratified by use of anti-hypertensive medication (p=.0001 no meds; p= .0007 meds).
Table 2 shows both standardized and unstandardized generalized regression analyses for the association between continuous positive emotion score and continuous systolic and diastolic blood pressure. Model analysis was stratified by use of anti-hypertensive medication and was adjusted for sociodemographic characteristics (Model 1) and sociodemographic characteristics, health behaviors and clinical variables (Model 2). For individuals not on anti-hypertensive medication, increasing positive emotion score was significantly associated with lower systolic blood pressure after adjustment for covariates in Models 1 and 2. Conversely, for those on anti-hypertensive medication, the association between increasing positive emotion score and lower systolic blood pressure did not reach significance for either Model 1 or 2.
Table 2.
Generalized Linear Models assessing the association between systolic and diastolic blood pressure and positive emotion score stratified by use of anti-hypertensive medication.
| Systolic Blood Pressure |
Diastolic Blood Pressure |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anti-hypertensive | Model 1 | Model 2 | Model 1 | Model 2 | ||||||||||||
| Medication | b | β | (SE) | p | b | β | (SE) | p | b | β | (SE) | p | b | β | (SE) | p |
| Yes (n = 841) | ||||||||||||||||
| Positive emotion | −0.18 | − 0.04 | (.16) | .36 | −0.18 | −0.04 | (.16) | .30 | −0.30 | −0.09 | (.10) | .003 | −0.46 | −0.14 | (11) | .0001 |
| No (n = 1723) | ||||||||||||||||
| Positive emotion | −0.31 | −0.09 | (.09) | .001 | −0.35 | −0.09 | (.10) | .001 | −0.52 | −0.19 | (.06) | .0001 | −0.56 | −0.12 | (.07) | .0001 |
Model 1, under systolic and diastolic blood pressure, respectively adjusted for: sociodemographic characteristics (age, gender, marital status, and years of education)
Model 2, under systolic and diastolic blood pressure, respectively adjusted for: Model 1 and + health behaviors (current smoking status, drinks per week) and clinical measures (diabetes, depressive symptoms and BMI).
Other factors significantly associated with higher systolic blood pressure in the anti-hypertensive medication group included men (b = 2.59, β = 0.07; SE 1.27, p = .04) and increasing BMI (b = 0.23, β = 0.08; SE .11, p = .02). For those not on anti-hypertension medication being married (b = −1.99, β = −0.07; SE 0.79, p = .01) and increasing years of schooling (b = −0.21, β−0.06; SE .09, p = .03) were associated with lower systolic blood pressure, whereas increasing negative emotion score (b = 0.14, β = 0.07; SE .0.06, p = .007) and men (b = 2.13, β = 0.07; SE .78, p = .007) were associated with higher systolic blood pressure.
Table 2 (Models 1 and 2) also shows that increasing positive emotion score was significantly associated with lower diastolic blood pressure for all individuals, those on and not on anti-hypertensive medication; though, the strength of association between positive emotion score and diastolic blood pressure was stronger for those not on anti-hypertensive medication. Other factors significantly associated with diastolic blood pressure were similar for both anti-hypertensive groups. Increasing BMI and negative emotion score, being diabetic and men were associated with higher diastolic blood pressure, while younger age and non-smokers were associated with lower diastolic blood pressure.
Table 3 shows the association between continuous positive emotion score and the 4-level joint blood pressure variable for individuals not on anti-hypertensive medication. Results were presented using cumulative logit models, where sociodemographic characteristics, health behaviors and clinical variables were sequentially added to the analysis. Model 1 shows the univariate association between positive emotion score and blood pressure. Each 1-point increase in positive emotion score decreased the odds of being in a higher blood pressure category by 9% (OR 0.91; 95% CI 0.89 – 0.94). The associated odds remained similar in Model 2 with the addition of sociodemographic characteristics (age, sex, marital status, and years of education) and health behaviors (current alcohol consumption and smoking status). In Model 3, with clinical measures added (BMI, self-rated diabetes and depressive symptoms), each 1-point increase in positive emotion score was associated with a 9% decreased odds of being in a higher blood pressure category (OR 0.91; 95% CI 0.89 – 0.93).
Table 3.
Cumulative logit models assessing associations between positive emotion and blood pressure for individuals not on anti-hypertensive medication (n = 1723).
| Blood Pressure* | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Positive emotion (continuous) | 0.91 | (0.89 – 0.94) | 0.91 | (0.89 – 0.94) | 0.91 | (0.89 – 0.93) |
| Age (continuous) | 0.98 | (0.97 – 1.00) | 0.98 | (0.97 – 1.00) | ||
| Men (vs. women) | 1.27 | (1.05 – 1.55) | 1.25 | (1.02 – 1.52) | ||
| Married (vs. unmarried) | 0.78 | (0.64 – 0.95) | 0.77 | (0.63 – 0.94) | ||
| Years of Schooling (continuous) | 0.99 | (0.96 – 1.01) | 0.99 | (0.96 – 1.01) | ||
| Non-Smoker | 0.77 | (0.60 – 1.00) | 0.80 | (0.62 – 1.03) | ||
| Alcohol Consumption (yes) | 1.01 | (0.96 – 1.06) | 1.08 | (0.98 – 1.19) | ||
| Body Mass Index | 1.02 | (1.00 – 1.04) | ||||
| Negative emotion | 1.00 | (0.98 – 1.01) | ||||
| Diabetes (yes) | 1.06 | (0.84 – 1.34) | ||||
Blood pressure was categorized according to the Joint National Committee: Normotensive (SBP < 120 mmHg and DBP < 80 mmHg); prehypertension (SBP 120-139 and DBP 80-89); stage 1 hypertension (SBP 140-159 mmHg and DBP 90-99 mmHg) and stage 2 hypertension (SBP ≥ 160 mmHg or DBP ≥ 100 mm Hg).
Model 3 was re-analyzed for individuals on anti-hypertensive medication. Two variables – positive emotion score and BMI – were significantly associated with blood pressure. Each 1-point increase in positive emotion score was associated with a 3% decreased odds of being in a higher blood pressure category (OR 0.97; 95% CI 0.93 – 1.00), while each 1 unit increase in BMI was associated with a 5% increased odds of being in a higher blood pressure category (OR 1.05; 95% CI 1.02 – 1.07).
Conclusion
The present study tested the hypothesis of an association between high positive emotion and lower blood pressure in Mexican Americans aged 65 or older. To increase the clinical applicability of our findings, blood pressure was measured using standard protocol from the Hypertension Detection and Follow-up Program and individuals on anti-hypertensive medication were identified and included in separate analyses. As well, systolic and diastolic blood pressure were assessed as independent continuous variables and as a joint categorical variable according to the Joint National Committee (JNC) 7 classification system on prevention, detection, evaluation and treatment of hypertension (2).
Our main findings can be summarized as follows. Increasing positive emotion score was significantly associated with lower continuous systolic and diastolic blood pressure for older Mexican Americans not on anti-hypertensive medication and was significantly associated with continuous diastolic blood pressure for those on anti-hypertensive medication. Associations were independent of sociodemographic characteristics, health behaviors and clinical variables known to affect blood pressure. As well, the positive emotion–blood pressure association remained significant after adjustment for depressive symptoms, so was not a reflection of the relationship between negative emotion and elevated blood pressure (38). We further showed that when blood pressure was categorized according to the JNC 7 recommended guidelines positive emotion was significantly associated with lower odds of being in higher blood pressure category. The analysis also showed a non-significant association between positive emotion score and continuous systolic blood pressure, for those on anti-hypertensive medication. Lack of a significant association for this group was not entirely clear. If anti-hypertensive medication reduced the association between positive emotion score and systolic blood pressure to non-significance then a similar non-significant association, for those on anti-hypertensive medication, would have been expected between positive emotion score and diastolic blood pressure. As part of the analysis, we also tested possible moderating effects of selected sociodemographic characteristics, health behaviors and clinical variables on the association between positive emotion score and systolic and diastolic blood pressure. All tested interactions were all non-significant. Therefore, it is possible that some unmeasured third variable may have affected the positive emotion – systolic blood pressure association for those on anti-hypertensive medication.
In general, the findings indicate a linkage between an individual's level of emotional well-being and blood pressure and suggest efforts to reduce or normalize blood pressure through psychological or cognitive-behavioral programs such as relaxation therapy or stress management may prove clinically beneficial. Sobel (39) has reported on the value of using psychosocial techniques to improve health outcomes including hypertension, while reducing the need for more expensive medical treatments. In a meta-analysis of 23 randomized controlled trials, Linden et al (40) showed with the addition of psychosocial treatments to standard cardiac rehabilitation regimens systolic blood pressure and heart rate were significantly reduced in patients with coronary artery disease compared with those who received usual care over a two year period. Though more research is needed to clarify relations between positive emotion and blood pressure, behavioral treatments might be considered as part of non-pharmacologic treatment programs among individuals not currently on anti-hypertensive medication with mild to moderate hypertension or as part of adjunctive therapy for those on anti-hypertensive medication.
Our results linking high positive emotion with lower blood pressure are consistent with an emerging literature on psychological well-being and cardiovascular-related health outcomes (41). A study of 1306 male war veterans from the Normative Aging Study showed optimists were less likely to suffer from angina and heart attacks than pessimists (42). Ostir et al (43) showed that 6-year stroke incidence in a sample of 2478 older whites and African Americans was significantly reduced among those with high positive emotion. Others have also shown that psychological well-being can predict recovery from cardiovascular related diseases (44-47).
Because a key hypothesis of the current study and other psychological well-being studies is the relation between high positive emotion and optimal health, it becomes important to understand pathways through which positive emotion may work to influence health. Some evidence suggests that positive emotion promotes adaptive coping abilities and builds resilience to stressful life events (20, 48). Folkman (20) has identified three coping mechanisms related to positive emotions – positive reappraisal, problem focused coping and recalling positive events. All three coping mechanisms involve the need to create or reinforce purpose and meaning in life. Ryff (49) has presented evidence showing positive relations between an older individual's ability to adapt and change with life circumstances and psychological well-being.
Positive emotions may also help promote strong and lasting social relationships, (50) which are vital to health and well-being. Over the past several decades, a large body of research has shown that absence of social ties is a major risk factor for increased morbidity and mortality (51-55). Uchino et al (56), in a review of 81 studies, found linkages between social networks and beneficial effects on the cardiovascular, endocrine, and immune systems. Population-based studies have also reported that an increasing number of social ties are associated with better physiologic profiles, including lower heart rate and systolic blood pressure (57, 58).
An emerging literature also indicates the likelihood that positive emotion can affect biochemical pathways, which in turn may affect change in blood pressure. Cortisol, a key stress hormone and related to hypertension (59) was found to be lower in persons with high levels of positive emotion compared with low positive emotion (19). Epel et al (60) showed individuals who were able to find positive meaning in a traumatic event had more adaptive hormonal responses to subsequent stressors. These and other studies (16, 17, 61) are preliminary but they provide an interesting and promising psycho-biological approach to better understand why some older adults, especially those from minority populations, appear resilient to adverse life events and present with good physical health profiles despite being disadvantaged.
The current study has some limitations. First, our measure of positive emotion was relatively crude. Because the positive emotion summary scale encompasses such overlapping concepts as happiness, autonomy, and being hopeful about future events, one could argue that it would not be well represented by a four-item scale. Second, the current findings may not generalize to other populations where cultural or age differences may exist. Therefore, it would be important to replicate our findings in other populations. Our study has several strengths including its large community-based sample, its design, and use of objective measures including blood pressure and anti-hypertensive medications. The current study was also the first, to our knowledge, to examine blood pressure and the protective role of positive emotion in the largest minority population in the United States (62).
In summary, our findings indicate that positive emotion is related to lower blood pressure and are suggestive of a protective role against cardiovascular-related diseases. Further investigations are warranted, as well, there is a need to understand how to cultivate the positive in a person's life and to understand why some individuals, especially those belonging to disadvantaged minority groups, are able to maintain high levels of emotional well-being. Broadening current health outcome models to include measures of well-being including positive emotion may help provide answers to these questions and may subsequently challenge the way we think about disease prevention and recovery.
Abbreviations used
- BMI
Body mass index
- CES-D
Center for Epidemiologic Studies - Depression
- CI
Confidence interval
- H-EPESE
Hispanic Established Population for the Epidemiologic Study of the Elderly
- JNC
Joint National Committee
- SD
Standard deviation
- SE
Standard error
Footnotes
References
- 1.American Heart Association . Heart Disease and Stroke Statistics -- 2005 Update. American Heart Association; Dallas, Tex: 2004. [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.He J, Whelton PK. Epidemiology and prevention of hypertension. Med Clin North Am. 1997;81:1077–1097. doi: 10.1016/s0025-7125(05)70568-x. [DOI] [PubMed] [Google Scholar]
- 4.Kornitzer M, Dramaix M, De Backer G. Epidemiology of risk factors for hypertension: implications for prevention and therapy. Drugs. 1999;57:695–712. doi: 10.2165/00003495-199957050-00003. [DOI] [PubMed] [Google Scholar]
- 5.Jonas BS, Franks P, Ingram DD. Are symptoms of anxiety and depression risk factors for hypertension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Fam Med. 1997;6:43–49. doi: 10.1001/archfami.6.1.43. [DOI] [PubMed] [Google Scholar]
- 6.Marshall GN, Sherbourne CD, Meredith LS, Camp P, Hays RD. The tripartite model of anxiety and depression: symptom structure in depressive and hypertensive patient groups. Journal of Personality Assessment. 2003;80(2):139–53. doi: 10.1207/S15327752JPA8002_03. [DOI] [PubMed] [Google Scholar]
- 7.Jonas BS, Lando JF. Negative affect as a prospective risk factor for hypertension. Psychosom Med. 2000;62:188–196. doi: 10.1097/00006842-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Fredrickson BL. The value of positive emotions - The emerging science of positive psychology in coming to understand why it's good to feel good. Am Sci. 2003;91:330–335. [Google Scholar]
- 9.Ryff CD, Singer B. The contours of positive human health. Psychol Inquiry. 1998;9:1–28. [Google Scholar]
- 10.Richman LS, Kubzansky L, Maselko J, Kawachi I, Choo P, Bauer M. Positive emotion and health: going beyond the negative. Health Psychology. 2005;24(4):422–9. doi: 10.1037/0278-6133.24.4.422. [DOI] [PubMed] [Google Scholar]
- 11.Danner DD, Snowdon DA, Friesen WV. Positive emotions in early life and longevity: findings from the nun study. J Pers Soc Psychol. 2001;80:804–813. [PubMed] [Google Scholar]
- 12.Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. J Am Geriatr Soc. 2000;48:473–478. doi: 10.1111/j.1532-5415.2000.tb04991.x. [DOI] [PubMed] [Google Scholar]
- 13.Scheier MF, Matthews KA, Owens JF, Schulz R, Bridges MW, Magovern GJ, et al. Optimism and rehospitalization after coronary artery bypass graft surgery. Archives of Internal Medicine. 1999;159(8):829–35. doi: 10.1001/archinte.159.8.829. [DOI] [PubMed] [Google Scholar]
- 14.Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly dutch men and women. Archives of General Psychiatry. 2004;61(11):1126–35. doi: 10.1001/archpsyc.61.11.1126. [DOI] [PubMed] [Google Scholar]
- 15.Ostir GV, Goodwin JS, Markides KS, Ottenbacher KJ, Balfour J, Guralnik JM. Differential effects of premorbid physical and emotional health on recovery from acute events. J Am Geriatr Soc. 2002;50:713–718. doi: 10.1046/j.1532-5415.2002.50167.x. [DOI] [PubMed] [Google Scholar]
- 16.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annu Rev Psychol. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- 17.Ryff CD, Singer BH, Love GD. Positive health: connecting well-being with biology. Philos Trans R Soc Lond B Biol Sci. 2004;359:1383–1394. doi: 10.1098/rstb.2004.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiol Aging. 2005;26(Suppl 1):108–112. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc Natl Acad Sci U S A. 2005;102:6508–6512. doi: 10.1073/pnas.0409174102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. 2000;55:647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- 21.Lazarus RS. Emotion and Adaptation. Cambridge University Press; Cambridge, UK: 1991. [Google Scholar]
- 22.US Census Bureau . U.S. Bureau of the Census; Washington D.C: 2002. Census 2000 supplementary survey.Public-use microdata file. Machine-readable file. [Google Scholar]
- 23.Markides KS, Stroup-Benham CA, Black SA, Satish S, Perkowski LC, Ostir GV. The health of Mexican American Elderly: selected findings from the Hispanic EPESE. In: Wykle ML, Ford AB, editors. Serving Minority Elders in the Twenty-first Century. Springer Publishing; New York, NY: 1999. pp. 72–90. [Google Scholar]
- 24.Hayes-Bautista DE, Baezconde-Garbanati L, Hayes-Bautista M. Latino health in Los Angeles: family medicine in a changing minority context. Fam Pract. 1994;11:318–324. doi: 10.1093/fampra/11.3.318. [DOI] [PubMed] [Google Scholar]
- 25.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- 26.Vega WA, Amaro H. Latino outlook: good health, uncertain prognosis. Annu Rev Public Health. 1994;15:39–67. doi: 10.1146/annurev.pu.15.050194.000351. [DOI] [PubMed] [Google Scholar]
- 27.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 28.Burnam MA, Hough RL, Escobar JI, Karno M, Timbers DM, Telles CA, et al. Six-month prevalence of specific psychiatric disorders among Mexican Americans and non-Hispanic whites in Los Angeles. Arch Gen Psychiatry. 1987;44:687–694. doi: 10.1001/archpsyc.1987.01800200013003. [DOI] [PubMed] [Google Scholar]
- 29.Moscicki EK, Locke BZ, Rae DS, Boyd JH. Depressive symptoms among Mexican Americans: the Hispanic Health and Nutrition Examination Survey. Am J Epidemiol. 1989;130:348–360. doi: 10.1093/oxfordjournals.aje.a115341. [DOI] [PubMed] [Google Scholar]
- 30.Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry. 1998;55:771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- 31.Markides KS, Rudkin L, Angel RJ, Espino DV. Health status of Hispanic elderly in the United States. In: Martin LJ, Soldo B, editors. Racial and Ethnic Differences in the Health of Older Americans. National Academy Press; Washington, DC: 1997. pp. 285–300. [PubMed] [Google Scholar]
- 32.Cornoni-Huntley JC, Blazer D, Lafferty ME, Everett DF. Established Populations for the Epidemiologic Studies of the Elderly, II. Resource Data Book. National Institute on Aging; Washington, DC: 1990. (NIA Publication 90-495). [Google Scholar]
- 33.Hypertension Detection and Follow-up Program Cooperative Group Variability of blood pressure and the results of screening in the hypertension detection and follow-up program. J Chronic Dis. 1978;31:651–657. doi: 10.1016/0021-9681(78)90069-3. [DOI] [PubMed] [Google Scholar]
- 34.Miller TQ, Markides KS, Black SA. The factor structure of the CES-D in two surveys of elderly Mexican Americans. J Gerontol B Psychol Sci Soc Sci. 1997;52B:S259–S269. doi: 10.1093/geronb/52b.5.s259. [DOI] [PubMed] [Google Scholar]
- 35.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 36.Roberts RE. Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 37.Sheehan TJ, Fifield J, Reisine S, Tennen H. The measurement structure of the Center for Epidemiologic Studies Depression Scale. J Pers Assess. 1995;64:507–521. doi: 10.1207/s15327752jpa6403_9. [DOI] [PubMed] [Google Scholar]
- 38.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290:2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 39.Sobel DS. Rethinking medicine: improving health outcomes with cost-effective psychosocial interventions. Psychosom Med. 1995;57:234–244. doi: 10.1097/00006842-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease: a meta-analysis. Arch Intern Med. 1996;156:745–752. [PubMed] [Google Scholar]
- 41.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 42.Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosom Med. 2001;63:910–916. doi: 10.1097/00006842-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Ostir GV, Markides KS, Peek MK, Goodwin JS. The association between emotional well-being and the incidence of stroke in older adults. Psychosom Med. 2001;63:210–215. doi: 10.1097/00006842-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Agarwal M, Dalal AK, Agarwal DK, Agarwal RK. Positive life orientation and recovery from myocardial infarction. Soc Sci Med. 1995;40:125–130. doi: 10.1016/0277-9536(94)e0058-z. [DOI] [PubMed] [Google Scholar]
- 45.Fitzgerald TE, Tennen H, Affleck G, Pransky GS. The relative importance of dispositional optimism and control appraisals in quality of life after coronary artery bypass surgery. J Behav Med. 1993;16:25–43. doi: 10.1007/BF00844753. [DOI] [PubMed] [Google Scholar]
- 46.Middleton RA, Byrd EK. Psychosocial factors and hospital readmission status of older persons with cardiovascular disease. Journal of Applied Rehabilitation Counseling. 1996;27:3–10. [Google Scholar]
- 47.Ostir GV, Peek MK, Markides KP, Goodwin JS. The association of emotional well-being on future risk of myocardial infarction in older adults. Primary Psychiatry. 2001;8:34–38. [Google Scholar]
- 48.Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. J Pers Soc Psychol. 1996;70:349–361. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 49.Kwan CM, Love GD, Ryff CD, Essex MJ. The role of self-enhancing evaluations in a successful life transition. Psychol Aging. 2003;18:3–12. doi: 10.1037/0882-7974.18.1.3. [DOI] [PubMed] [Google Scholar]
- 50.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. 2003;84:365–376. doi: 10.1037//0022-3514.84.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Glass TA, Maddox GL. The quality and quantity of social support: stroke recovery as psycho-social transition. Soc Sci Med. 1992;34:1249–1261. doi: 10.1016/0277-9536(92)90317-j. [DOI] [PubMed] [Google Scholar]
- 52.House JS, Landis KR, Umberson D. Social Relationships and Health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 53.Berkman LF, Oxman TE, Seeman TE. Social networks and social support among the elderly: assessment issues. In: Wallace RB, Woolson RF, editors. The Epidemiologic Study of the Elderly. Oxford University Press; New York: 1992. pp. 196–212. [Google Scholar]
- 54.Due P, Holstein B, Lund R, Modvig J, Avlund K. Social relations: network, support and relational strain. Soc Sci Med. 1999;48:661–673. doi: 10.1016/s0277-9536(98)00381-5. [DOI] [PubMed] [Google Scholar]
- 55.Unger JB, McAvay G, Bruce ML, Berkman L, Seeman T. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 1999;54:S245–S251. doi: 10.1093/geronb/54b.5.s245. [DOI] [PubMed] [Google Scholar]
- 56.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 57.Linden W, Chambers L, Maurice J, Lenz JW. Sex differences in social support, self-deception, hostility, and ambulatory cardiovascular activity. Health Psychol. 1993;12:376–380. doi: 10.1037//0278-6133.12.5.376. [DOI] [PubMed] [Google Scholar]
- 58.Unden AL, Orth-Gomer K, Elofsson S. Cardiovascular effects of social support in the work place: twenty-four-hour ECG monitoring of men and women. Psychosom Med. 1991;53:50–60. doi: 10.1097/00006842-199101000-00005. [DOI] [PubMed] [Google Scholar]
- 59.McEwen BS, Biron CA, Brunson KW, Bulloch K, Chambers WH, Dhabhar FS, et al. The role of adrenocorticoids as modulators of immune function in health and disease: neural, endocrine and immune interactions. Brain Res Brain Res Rev. 1997;23:79–133. doi: 10.1016/s0165-0173(96)00012-4. [DOI] [PubMed] [Google Scholar]
- 60.Epel ES, McEwen BS, Ickovics JR. Embodying psychological thriving: Physical thriving in response to stress. J Soc Issues. 1998;54:301–322. [Google Scholar]
- 61.Damasio A. Fundamental feelings. Nature. 2001;413:781. doi: 10.1038/35101669. [DOI] [PubMed] [Google Scholar]
- 62.Day JC. Population projections of the United States, by age, sex, race, and Hispanic origin : 1995 to 2050. US Dept. of Commerce, Bureau of the Census; Washington, DC: 1996. (Publication P25-1130). Current population reports. [Google Scholar]


