Abstract
Background
Hip fractures are an important cause of morbidity and mortality among older adults. Little is known regarding older adults' treatment preferences for osteoporosis. Individual patient preferences are particularly important to consider in this context given that adherence with osteoporosis treatment is low.
Methods
Subjects at high risk for an osteoporotic hip fracture completed a discrete choice questionnaire to determine preferences for hip protectors versus oral weekly bisphosphonates. Simulations, based on respondents' values for type of treatment and absolute reduction in risk of hip fractures over five years, were performed to predict treatment choices.
Results
Seventy-six patients participated in this study (92% participation rate). At the time of the study 57% of the participants were currently using bisphosphonates; none had ever heard of a hip protector. In the base case scenario, in which both options were described as being equally effective, 9% preferred hip protectors, 88% weekly oral bisphosphonates, and 3% refused all options. When hip protectors were described as being more effective than bisphosphonates, 26% preferred hip protectors, 71% weekly oral bisphosphonates, and 3% continued to refuse all options. Preference for hip protectors was stronger among participants not currently using bisphosphonates (36% versus 19%, p=0.08), as well as among subjects preferring to avoid taking prescription drugs for most health problems (44% vs 12%, p=0.002).
Conclusion
When presented with tradeoffs between hip protectors and bisphosphonates, the majority of community-dwelling older adults at high risk for fracture prefer the latter. Of note, however, many of the participants in this study were current bisphosphonate users. Future trials and education programs should consider targeting respondents preferring to manage health problems using nonpharmacologic treatment approaches since, based on the results of this study, adherence and proper use of hip protectors is expected to be higher amongst these patients.
Hip fractures are an important cause of morbidity and mortality among older adults (1). Mortality rates exceed 20% in elderly patients and more than 25% require long-term care or assistance with activities of daily living for at least one year following fracture (1, 2). External hip protectors have been shown to decrease the risk of hip fractures among frail older adults in several controlled trials (3-5). Studies have also found these devices to be a potentially cost-effective or cost-saving strategy among high risk persons (6,7). In a recent trial, Cameron et al (8) found that hip protector users had significantly greater improvement in fall self-efficacy compared to non-users indicating that hip protectors may increase older adults' confidence and allow them to complete tasks more safely. In contrast, other trials have failed to demonstrate any protective effect associated with these devices, and a recent updated review concluded that these devices are not effective at preventing hip fractures (3). However, the quality of many of these trials was limited by poor adherence and improper use of the study device (3,9,10). Moreover, effectiveness of such interventions is difficult to demonstrate, especially in community settings, because of the low rate of hip fractures.
Significant efforts have been directed towards developing newer, more comfortable, hip protectors. Researchers have also focused on improving educational programs to increase adherence and proper use of these devices. Yet despite the fact that treatment preferences for osteoporosis and the prevention of fractures depend on personal values, there have been no studies quantifying older adults' treatment preferences for hip protectors when presented with choices involving explicit tradeoffs between non-pharmacologic and pharmacologic options. Individual patient preferences are particularly important to consider in this context given that adherence with osteoporosis treatment options is low (11-13). Future efforts towards modifying/promoting hip protectors for osteoporosis should, therefore, ideally be guided by patient preferences. The objective of this study was to quantify treatment preferences for hip protectors versus bisphosphonates among older adults at high risk for osteoporotic fractures. We used Choice Based Conjoint Analysis (Sawtooth Software Inc.®) to elicit preferences. Choice Based Conjoint Analysis (CBCA) is a computerized questionnaire which predicts preferences based on how respondents make tradeoffs between the risks and benefits related to the specific options under consideration (14).
METHODS
Participants
We recruited women (postmenopausal) and men (over the age of 65) who had recently (within 2 weeks) undergone bone densitometry. Participants were drawn from six centers performing bone densitometry in the greater New Haven area.
All English-speaking patients undergoing bone densitometry were asked whether they agreed to be contacted by a research assistant to learn more about, and potentially participate in, a study examining patients' opinions about medications for osteoporosis. Patients were asked to fill out a form indicating whether or not they wished to be contacted.
Subjects at high risk for an osteoporotic hip fracture (Fracture Index Score > 7 (15)) were eligible to participate in this study. Only persons with known secondary causes of osteoporosis or contraindications to bisphosphonates (esophagitis, severe heartburn, the inability to sit upright for at least 30 minutes, or previous allergic reactions to bisphosphonates) were excluded. All eligibility criteria were ascertained by self-report. The research protocol was approved by the Human Investigations Committee at our institution.
Data Collection
Participants first underwent a standardized educational session with the research assistant regarding the pathophysiology of osteoporosis and its complications. The information presented to participants was based on patient information materials published by the National Osteoporosis Foundation. The educational session was performed to ensure that all participants had the same information available to them before performing the preference task. All participants were shown, and given the opportunity to handle, an actual hip protector purchased from HIProtector® to ensure that they were familiar with the device. Details on this device are available at www.HIProtector.com.
Participants completed a CBCA questionnaire (Sawtooth Software Inc.®, SSI Web Version 3.5, Sequim, WA) to determine preferences for hip protectors versus oral weekly bisphosphonates (14). Monthly oral bisphosphonates were not included because this option was not available at the time of the study. CBCA assesses preferences by asking respondents to choose a preferred option from a set of alternatives. Each option is defined using a limited number of characteristics. This feature allows respondents to choose the real option of refusing or deferring treatment. Respondents do not evaluate treatment alternatives directly. Rather, each participant considers the tradeoffs between conflicting characteristics. Answers to respondent-specific questions allow the investigator to infer values for specific treatment characteristics. These values are then used to predict which option most closely suits each participant's individual preferences.
Conjoint analysis assumes that each option is a composite of different characteristics, and that each characteristic represents one of a number of levels. Levels refer to the range of estimates for each characteristic. The characteristics and levels of the prevention measures included in the questionnaire are described in Appendix 1. Brand names were not included to avoid potential bias. We did not include cost as an attribute in this study because, depending on individual insurance plans, the out-of-pocket costs for both treatment options were exceedingly variable.
We designed the questionnaire to present respondents with 12 choice sets. Each set was composed of three treatment alternatives and a “None” option, which allowed respondents to refuse all treatments. An example is provided in Appendix 2. We used the software's complete enumeration strategy to construct the choice sets. This strategy constructs options by randomly assigning levels to each option.
Sociodemographic and clinical data were collected by self-report. Attitude towards medications was measured using a question from the Medical Care Preference Scale (16). “I prefer to treat most health problems without help from doctors or prescription drugs” coded on a five item response scale ranging from “Strongly disagree” to “Strongly agree”. Participants stating that they “Agreed” or “Strongly agreed” with this statement were classified as preferring to treat health problems without doctors or prescription drugs.
Analyses
Relative importance of the characteristics studied was calculated by dividing the range of utilities for each characteristic by the sum of ranges, and multiplying by 100. In this context “utility” is a number that represents the value a respondent associates with a particular characteristic, with higher utilities indicating increased value. The relative importance reflects the extent to which the difference between the best and worst levels of each characteristic influenced respondents' decisions to choose a particular option.
We performed simulations based on respondents' values for type of treatment and absolute reduction in risk of hip fractures over five years to predict treatment choices. In conjoint analysis, options are defined based on the levels of each characteristic. CBCA generates a predicted overall score for each option in a simulation based on individual respondent's estimated values for specific treatment characteristics (14). The option with the highest estimated utility, i.e. the option that is most consistent with each individual respondent's values, is regarded as that respondent's predicted choice. Utilities were calculated based on a Hierarchical Bayes model using Monte Carlo Markov Chain algorithms (17). In the base-case scenario, medications and hip protectors were described as being equally effective. We subsequently conducted sensitivity analyses to examine whether increasing the benfit associated with hip protectors affected participants' preferences. Because respondents' preferences are predicted based on how they made trade-offs between treatment characteristics they are less biased by familiarity with specific options.
Associations between treatment preferences and participants' characteristics were examined using chi-square and t-tests as appropriate.
RESULTS
Of the 233 patients agreeing to be contacted, 81 were eligible. Seventy-two women and four men participated in this study, mean age (± SD) = 78 ± 5 years. Participant characteristics are further described in Table 1. At the time of the study 57% of the participants were currently using bisphosphonates, and none were using a hip protector. Furthermore, none of the participants had ever heard of a hip protector prior to the study, none had talked to their physicians about using one, and none were aware of this option as a potential therapeutic device.
Table 1.
Participant Characteristics
| Characteristic | Total Number = 76 |
|---|---|
| Age, years (mean ± SD, range) | 78 ± 5 (65-90) |
| Female | 95% |
| Caucasian | 82% |
| Married | 41% |
| At least some college education | 65% |
| Annual household income at least $40,000 | 24% |
| Medical Insurance | |
| Medicare + Private | 85% |
| Medicare alone | 9% |
| Medicaid | 3% |
| Other | 3% |
| Having a prescription drug plan | 62% |
| Currently using bisphosphonates | 57% |
| Currently using hip protectors | 0 |
| Health status very good or excellent | 40% |
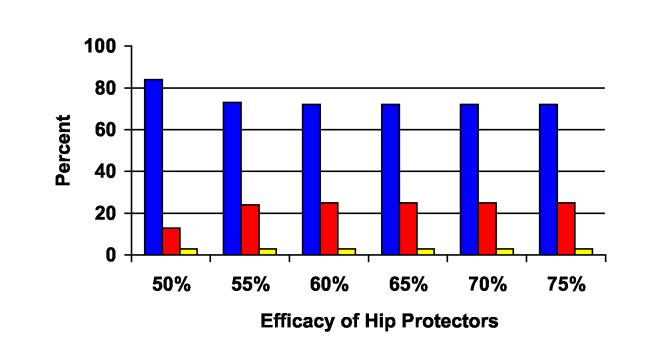
The relative importance of the characteristics studied is demonstrated in Figure 1. Participants' preferences were more strongly influenced by the type of treatment (i.e. medication versus device) (60%) than the expected benefits (40%).
Figure 1.
Relative influence* of type of treatment versus efficacy on participants' treatment choices.
Legend:
Blue = Relative influence of efficacy (decrease in risk of fractures over five years)
Red = Relative influence of type of treatment
* Relative influences sum to 100.
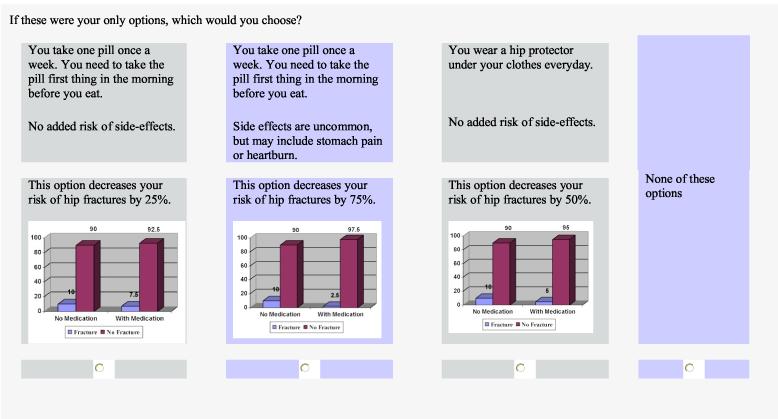
In the base case scenario, in which both options were described as being equally effective, 9% of the subjects surveyed preferred hip protectors, 88% preferred weekly oral bisphosphonates, and 3% refused all options. When hip protectors were described as resulting in a 55% decrease in risk of fracture and bisphosphonates a 50% reduction in future fracture, 26% of the subjects surveyed preferred hip protectors, 71% preferred weekly oral bisphosphonates, and 3% continued to refuse all options (Figure 2). Additional increases in the efficacy of hip protectors over bisphosphonates (as demonstrated in Figure 2) did not further increase the proportion of participants willing to use this option.
Figure 2.
Preferences for hip protectors versus bisphosphonate* as the efficacy of hip protectors is increased.
Legend:
Blue = Proportion of respondents preferring bisphosphonates
Red = Proportion of respondents preferring hip protectors
Yellow = Proportion of respondents preferring neither option
*Efficacy of bisphosphonates held constant at 50% risk reduction.
Hip protectors were more strongly preferred among participants not currently using bisphosphonates compared to current users (36% versus 19%, p=0.08). Age, education, income, insurance, and health status were not related to treatment preferences. However, older adults preferring to avoid taking prescription drugs for most health problems were more likely to prefer hip protectors compared to their counterparts (44% vs 12%, p=0.002). This association remained significant after controlling for current use of bisphosphonates [Adjusted Odds Ratio (95% Confidence Interval) = 5.6 (1.7 - 18.0)].
DISCUSSION
In this study we found that, when presented with tradeoffs between hip protectors and bisphosphonates, the majority of community-dwelling older adults at high risk for fracture prefer the latter. Of note, many of the participants in this study were current bisphosphonate users, and preferences for hip protectors would be expected to be higher among a population in which a greater proportion of subjects were current hip protector users. Participants were more strongly influenced by the type of treatment than expected benefits, and when given a choice most preferred taking a pill over wearing a hip protector. Nevertheless, some of those surveyed did prefer hip protectors over bisphosphonates. This was especially evident among participants not currently using bisphosphonates as well as those preferring nonpharmacologic treatment approaches as measured by a question from the validated Medical Care Preference scale (16).
The strengths of this study include the methods used to elicit preferences and the clinical context in which choices were ascertained. Regarding the former, we chose to use CBCA to derive participants' predicted choices because this approach requires respondents to make choices based on tradeoffs between specific treatment characteristics. Construction of preferences based on explicit tradeoffs minimizes biases associated with the context in which choices are presented and decreases the influence of individual provider preferences. Most importantly, CBCA has a strong theoretical basis, obtains high levels of internal consistency and, by using Hierarchical Bayes analysis, is able to derive preferences at the individual respondent level (17). In addition, we tried to maximize understanding of risk magnitude using several strategies (22, 23). We provided both numerical estimates (natural frequencies) as well as graphical representations of absolute risk data for fracture risk for patients with and without treatment. Regarding the context in which choices were ascertained, preferences were elicited soon after bone densitometry, thereby ensuring that the task was meaningful for the respondents.
Our results must be interpreted in view of the limitations of this study. Although we used robust methods to ascertain preferences, ideally acceptance and adherence to these therapies would be measured as baseline and outcomes measures in a head to head randomized controlled trial. In addition, many of the participants interviewed were taking bisphosphonates, because we could not recruit sufficient numbers of treatment naïve, high risk participants at a relevant point in decision-making. This limits the generalizability of our results. Moreover, preferences for hip protectors would be expected to be higher in a population with including current hip protector users. In addition, because of the wide range of costs available for both bisphosphonates and hip protectors, we did not evaluate the influence of cost on patient preferences in this study. We would expect cost to be an important factor in decision-making among older adults on fixed incomes depending on the constraints of their insurance plans. Lastly, most participants were Caucasian, female, and well-educated, which also limits the generalizability of the results.
In summary, we found that the majority of participants (many of whom were currently using bisphosphonates) preferred oral weekly bisphosphonates over hip protectors. Most patients preferred bisphosphonates over hip protectors even when the latter was associated with a much greater benefit in terms of hip fracture prevention and no adverse effects. These results suggest, that hip protectors, as currently manufactured, are unlikely to be a widely accepted treatment option amongst community dwelling older adults. Future trials and education programs should consider targeting respondents preferring to manage health problems using nonpharmacologic treatment approaches since, based on the results of this study, adherence and proper use of hip protectors would be expected to be highest amongst these patients.
ACKNOWLEDGEMENTS
We would like to thank all participants for their time and effort. Dr. Fraenkel had full access to all the data and takes full responsibility for the integrity of the data and the accuracy of the analysis. There are no potential conflicts or overlap with other publications to the best of our knowledge. The authors do not have any financial interests that would be considered a conflict of interest.
Appendix 1
Description of characteristics included in the CBCA questionnaire
| Characteristic | Level |
|---|---|
| Type of treatment | • You take one pill once a week. You need to take the pill first thing in the morning before you eat. Side effects are uncommon, but may include stomach pain or heartburn. |
| • You wear a hip protector under your clothes everyday. No added risk of side-effects. | |
| Efficacy | • This option decreases your risk of hip fractures by 75 |
| • This option decreases your risk of hip fractures by 50%. | |
| • This option decreases your risk of hip fractures by 25%. | |
| Absolute risk information for reduction in hip fracture risk was provided using frequency data and bar graphs (see Appendix 2). |
Appendix 2
Example of a CBCA choice tas
Footnotes
This study was funded by the Arthritis Foundation Clinical Science Grant. Dr. Fraenkel is also supported by the K23 Award AR048826-01 A1.
REFERENCES
- 1.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–7. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 2.Wehren LE, Magaziner J. Hip fracture: risk factors and outcomes. Curr Osteoporos Rep. 2003;1:78–85. doi: 10.1007/s11914-003-0013-8. [DOI] [PubMed] [Google Scholar]
- 3.Parker MJ, Gillespie WJ, Gillespie LD. Effectiveness of hip protectors for preventing hip fractures in elderly people: systematic review. BMJ. 2006;332:571–4. doi: 10.1136/bmj.38753.375324.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kannus P, Parkkari J, Niemi S, et al. Prevention of hip fracture in elderly people with use of a hip protector. N Engl J Med. 2000;343:1506–13. doi: 10.1056/NEJM200011233432101. [DOI] [PubMed] [Google Scholar]
- 5.Heikinheimo R, Jalonen-Mannikko A, Asumaniemi H, Lehtomaki E. External hip protectors in home-dwelling older persons. Aging Clin Exp Res. 2004;16:41–3. doi: 10.1007/BF03324530. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Sun H, Anis AH. Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol. 2004;31:1607–13. [PubMed] [Google Scholar]
- 7.Segui-Gomez M, Keuffel E, Frick KD. Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess Health Care. 2002;18:55–66. [PubMed] [Google Scholar]
- 8.Cameron ID, Stafford B, Cumming RG, Birks C, Kurrle SE, Lockwood K, Quine S, Finnegan T, Salkeld G. Hip protectors improve falls self-efficacy. Age Ageing. 2000;29:57–62. doi: 10.1093/ageing/29.1.57. [DOI] [PubMed] [Google Scholar]
- 9.Sawka AM, Boulos P, Beattie K, et al. Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2005;16:1461–74. doi: 10.1007/s00198-005-1932-2. [DOI] [PubMed] [Google Scholar]
- 10.van Schoor NM, Asma G, Smit JH, Bouter LM, Lips P. The Amsterdam hip protector study: compliance and determinants of compliance. Osteoporos Int. 2003;14:353–9. doi: 10.1007/s00198-003-1382-7. [DOI] [PubMed] [Google Scholar]
- 11.Cramer JA, Amonkar MM, Hebborn A, Suppapanya N. Assessing the relationship between bisphosphonate dosing regimen and treatment adherence among postmenopausal osteoporotic women. Arthritis Rheum. 2004;50(suppl):S294. Abstract 677. [Google Scholar]
- 12.Bocuzzi SJ, Foltz SH, Omar MA, Kahler KH, Gutierrez B. Adherence and persistence associated with the pharmacologic treatment of osteoporosis. Osteoporos Int. 2005;16(suppl 3):S24. doi: 10.1097/01.smj.0000221637.90495.66. 2005. Abstract P129. [DOI] [PubMed] [Google Scholar]
- 13.Solomon DH, Avorn J, Katz JN, et al. Compliance with osteoporosis medication. Arch Intern Med. 2005;165:2414–19. doi: 10.1001/archinte.165.20.2414. [DOI] [PubMed] [Google Scholar]
- 14.Orme B. CBC/web analysis module and market simulator. Sawtooth Software Inc; Sequim: 2001. [Google Scholar]
- 15.Black DM, Steinbuch M, Palermo L, et al. An assessment tool for predicting fracture risk in postmenopausal women. Osteoporosis Int. 2001;12:519–28. doi: 10.1007/s001980170072. [DOI] [PubMed] [Google Scholar]
- 16.Ganther JM, Wiederholt JB, Kreling DH. Measuring patients' medical care preferences: care seeking versus self-treating. Med Decis Making. 2001;21:133–40. doi: 10.1177/0272989X0102100206. [DOI] [PubMed] [Google Scholar]
- 17.Orme B. Hierarchical Bayes regression analysis: technical paper. Sawtooth Software; Sequim: 2003. (Technical Paper Series). [Google Scholar]
- 18.Kurrle SE, Cameron ID, Quine S, Cumming RG. Adherence with hip protectors: a proposal for standardised definitions. Osteoporos Int. 2004;15:1–4. doi: 10.1007/s00198-003-1503-3. [DOI] [PubMed] [Google Scholar]
- 19.Kurrle SE, Cameron ID, Quine S. Predictors of adherence with the recommended use of hip protectors. J Gerontol A Biol Sci Med Sci. 2004;59:958–61. doi: 10.1093/gerona/59.9.m958. [DOI] [PubMed] [Google Scholar]
- 20.McAughey JM, McAdoo M. Hip protectors. Acceptability of hip protectors was 35% at six months in the community. BMJ. 2002;324:1454. [PubMed] [Google Scholar]
- 21.Patel S, Ogunremi L, Chinappen U. Acceptability and compliance with hip protectors in community-dwelling women at high risk of hip fracture. Rheumatology. 2003;42:769–72. doi: 10.1093/rheumatology/keg215. [DOI] [PubMed] [Google Scholar]
- 22.Braddock CH, 3rd,, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999;282:2313–20. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 23.Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. Monogr Natl Cancer Inst. 1999;25:44–51. doi: 10.1093/oxfordjournals.jncimonographs.a024207. [DOI] [PubMed] [Google Scholar]