Abstract
OBJECTIVE
To evaluate the association between cognitive dysfunction and other barriers and glycemic control in older adults with diabetes.
RESEARCH DESIGN AND METHODS
Patients over the age of 70 years presenting to a geriatric diabetes clinic were evaluated for barriers to successful diabetes management. Patients were screened for cognitive dysfunction with the Mini Mental State Examination (MMSE) and a clock-drawing test (CDT) scored by 1) a method validated by Mendez et al. and 2) a modified CDT (clock in a box [CIB]). Depression was evaluated with the Geriatric Depression Scale. Interview questionnaires surveyed activities of daily living (ADLs) and instrumental ADLs (IADLs), as well as other functional disabilities.
RESULTS
Sixty patients (age 79 ± 5 years, diabetes duration 14 ± 13 years) were evaluated. Thirty-four percent of patients had low CIB (≤5), and 38% of patients had low CDT (≤13). Both CIB as well as CDT were inversely correlated with HbA1c, suggesting that cognitive dysfunction is associated with poor glycemic control (r = −0.37, P < 0.004 and r = −0.38, P < 0.004, respectively). Thirty-three percent of patients had depressive symptoms with greater difficulty completing the tasks of the IADL survey (5.7 ± 1.7 vs. 4.6 ± 2.0; P < 0.03). These older adults with diabetes had a high incidence of functional disabilities, including hearing impairment (48%), vision impairment (53%), history of recent falls (33%), fear of falls (44%), and difficulty performing IADLs (39%).
CONCLUSIONS
Older adults with diabetes have a high risk of undiagnosed cognitive dysfunction, depression, and functional disabilities. Cognitive dysfunction in this population is associated with poor diabetes control.
Diabetes in older adults has become a major public health problem affecting an increasing number of individuals worldwide. Both older age and diabetes are independently associated with an increased risk of cognitive dys-function; the risk is even greater for older adults with diabetes (1-6). Neuropsychological tests have shown deficits in various aspects of cognitive function in both young and older patients with diabetes. Deficits have been seen in areas of psychomotor efficiency, global cognition, episodic memory, semantic memory, and working memory (7,8). Abnormalities in cognitive functions mediated by frontal lobe (executive functions), including a number of complex behaviors such as problem solving, planning, organization, insight, reasoning, and attention, are noted in patients with diabetes (9-12). Considering the importance of self-management behaviors in diabetes treatment and the high complexity of diabetes treatment regimens (e.g., blood glucose testing, meal planning, medication compliance), diabetic patients with cognitive dysfunction may experience significant difficulty managing their disease. They may also have difficulty treating acute conditions associated with diabetes treatment such as hypoglycemia. Cognitive dysfunction, especially executive dys-function, can affect insight into one's behavior (13,14) and may, therefore, contribute to the patient minimizing the difficulties that he/she is experiencing. Such patients are unlikely to self-report either cognitive problems or difficulty managing their diabetes. As a result, many healthcare providers may be unaware that their patients have cognitive dysfunction.
Diabetes and cognitive dysfunction have also been associated with depression and functional impairment in elderly patients (15-21). Therefore, we hypothesize that cognitive dysfunction along with declining overall functional status and co-morbid conditions such as depression may form a barrier to achieving or maintaining good glycemic control among older adults with diabetes. While the majority of elderly patients, especially those with diabetes, are screened for cardiovascular risk factors, few of these patients are screened or evaluated for impairments in cognitive functions. We assessed unrecognized barriers to successful management of diabetes at a geriatric diabetes clinic by screening older adults over the age of 70 years for the presence of depression and functional disabilities, as well as cognitive dysfunction
RESEARCH DESIGN AND METHODS
We analyzed data collected from consecutive patients age 70 or older who were evaluated at a geriatric diabetes clinic and who underwent screening by a diabetes educator. Patients with an established diagnosis of dementia or a memory disorder, those needing an interpreter, or those with severe visual impairment (unable to complete the tests) were excluded. The study was reviewed and found to be exempt by the institutional review board. The cognitive measures, questionnaires, and tests included in this study are described in detail below.
Mini Mental State Examination
The Mini Mental State Examination (MMSE) is one of the most commonly used cognitive screening measures because it is quick and easy to administer (22,23). The MMSE includes specific questions related to attention, orientation, memory, calculation, and language. The measure's scoring is based on 30 total points, and impairment is indicated by a score of 24 or lower. While this measure is often used to screen for memory function, it has a number of psychometric limitations, such as few executive function items. While the MMSE has good specificity (96%), the sensitivity is poor (64%), suggesting that cognitive changes remain undetected in a number of individuals (24).
Clock drawing test
The clock-drawing test (CDT) is a well-known and validated measure of cognitive function that is used commonly in clinical practice due to its ease of administration (25,26). Several scoring systems have been used and standardized by investigators as a screen for cognitive dysfunction (27-30). In this test, participants are presented with two sheets of paper: one provides written instructions, the other serves as a response sheet. The instructions direct participants to draw a clock and set the time to ten minutes after eleven.
CDT Scored by Mendez method
We have used the scoring system validated by Mendez et al. (29), which uses a 20-point scale as reported. This system of scoring has been shown to be most accurate in predicting deficit in cognitive function and correlates with MMSE (31,32).
Clock-in-a-box test
The clock-in-a-box (CIB) test is a modified CDT aimed at screening cognitive dysfunction in the medical setting (10). This test was developed specifically to be a fast and reliable index of executive function. In this test, as an added step participants are asked to draw a clock in the blue box. The response sheet includes four 9.5 × 12.5-cm boxes, each of a different color (yellow, red, green, and blue). Each CIB clock is scored using an eight-point scale that consists of four-point working memory and four-point executive function subscores. The four features that contribute to the working memory subscore include completing the drawing in the correct square, resemblance to a clock, writing all numbers, and setting the correct time. The four features that contribute to the executive function subscore include drawing an appropriately sized clock with hands of different lengths and writing the numbers in numerical order and also evenly spaced. The total score is the sum of the memory and executive function subscores. Total score in CIB is used to assess overall cognitive function.
Geriatric depression scale
The 15-item Geriatric Depression Scale (GDS) is a well-validated tool often used to screen for depressive symptoms in older individuals (33,34). This measure is scored based on a 15-point scale, and impairment is indicated by a score of 5 or higher.
Questionnaires
Questionnaires were administered via interview by a nurse educator in a geriatric diabetes clinic to evaluate self-reported functional disabilities. These questionnaires addressed difficulty with vision, hearing, falls and fear of falls, activities of daily living (ADLs), and instrumental ADLs (IADLs). The ADL and IADL questionnaires are informant-based assessments of functional abilities. The ADL questionnaire measures functionality in five areas: bathing, toileting, grooming, dressing, and eating. The IADL questionnaire measures functionality in traveling, shopping, housework, managing finances, using the telephone, and taking medications. ADL and IADL scales are scored inversely relative to disability, such that lower scores indicate higher levels of disability.
Demographics and clinical information on diabetes
Demographic information and information pertaining to diabetes and its control was collected from the data gathered during the clinic visit. These data included age, sex, type and duration of diabetes, HbA1c (A1C), self-reported history of hypoglycemia, and the type of treatment for diabetes (insulin, oral, medications, and/or lifestyle modification).
Statistical methods
Data are presented as means ± SD for continuous data and as n (%) for frequency data. The CDT is scored with two methods. One is the scoring method validated by Mendez (CDT) and the second one is the modified version (CIB). We estimated odds ratios (ORs) for continuous data using simple logistic regression and evaluated difference in frequency data using Fisher's exact test. We estimated Pearson or Spearman correlation coefficients depending on the bivariate distributions of continuous variables. We then estimated simple linear regression models predicting A1C with variables of interest. Finally, we estimated multivariate models predicting A1C controlling for variables of interest.
Subjects then were divided into two groups based on performance of CDT and CIB separated at the mean value of the total test scores. Those participants with a CIB total score of ≤5 were assigned to the CIB low group, whereas those with a CIB total score of ≥6 were assigned to the CIB high group. Similarly, participants with a CDT score of ≤13 were assigned to the CDT low group, whereas those with a CDT score of ≥14 were assigned to the CDT high group. Data were analyzed using SAS, version 8.02 (SAS Institute, Cary, NC). A1C provides an estimate of glycemic control for the previous 2–3 months. A1C was measured at the Joslin Diabetes Center using the high-performance liquid chromatography ion capture method (reference range 4.0–6.0%; Tosoh Medics, San Francisco, CA).
RESULT
Sixty consecutive patients over the age of 70 years with type 2 diabetes seen at a geriatric diabetes clinic were evaluated. The mean age of the population was 79 ± 5 years (range 70–93); the mean duration of diabetes was 14 ± 13 years (1-55), and the mean A1C was 7.9±1.4%. The higher proportion of the study population was female (female-to-male ratio 58:42), Caucasian (82%), and college educated (53%), with 92% having at least some high school education. Sixty-eight percent of patients lived with their spouse or other family members, representing a relatively well-supported population seen at this tertiary care specialized institution. The characteristics of the study population and the treatment modalities utilized for glycemic control are listed in Table 1.
Table 1.
Demographic and health characteristics of study population and variables separated by low versus high CIB score
| All patients | CIB high | CIB low | |
|---|---|---|---|
| n | 58 | 38 | 20 |
| Age (years) | 79 ± 5 | 77.73 ± 5.3 | 80.3 ± 4.5 |
| Duration of diabetes (years) | 14 ± 13 | 13.07 ± 11.6 | 17.45 ± 16.2 |
| Average A1C (%) | 7.9 ± 1.4 | 7.5 ± 1.17 | 8.725 ± 1.43 |
| BMI (kg/m2)* | 28 ± 6 | 29.70 ± 5.09 | 26.45 ± 5.54 |
| Ethnicity (%) | |||
| Caucasians | 82 | 94.7 | 60 |
| African Americans | 13 | 2.6 | 30 |
| Hispanics | 5 | 2.6 | 10 |
| Education (%) | |||
| Elementary | 5 | 66 | 32 |
| Middle | 3 | 0 | 11 |
| High school | 39 | 34 | 47 |
| College | 53 | 0 | 11 |
| Living status (%) | |||
| Alone | 30 | 26 | 35 |
| With spouse | 50 | 55 | 40 |
| With others | 20 | 18 | 25 |
| Smoking (%) | |||
| Current | 5 | 5 | 5 |
| Previous history | 45 | 53 | 30 |
| Treatment modality (%) | |||
| Lifestyle modification | 3 | 5 | 0 |
| Oral medications only | 58 | 66 | 45 |
| Insulin only | 15 | 11 | 20 |
| Oral medications + insulin | 23 | 18 | 35 |
| Comorbidities (%) | |||
| Hypertension | 93 | 92 | 95 |
| Hypercholesteremia | 77 | 84 | 65 |
| Coronary artery disease | 37 | 45 | 20 |
| Cardiovascular disease | 17 | 18 | 15 |
| Functional barriers (%) | |||
| Hearing impairment | 48 | 55 | 35 |
| Vision impairment | 53 | 38 | 65 |
| History of recent falls | 33 | 37 | 30 |
| Fear of falling | 44 | 39 | 55 |
| Difficulty performing IADLs | 39 | 47 | 25 |
| Weight loss | 18 | 11 | 30 |
| Hypoglycemic episodes | 48 | 39 | 60 |
Statistically significant.
We observed significant functional disability in our patient sample. Forty-eight percent of the patients had hearing impairments, 53% had vision impairments, 33% had a history of recent falls, and 44% were afraid of falling. Although a majority (95%) of the patients were able to perform ADLs independently, only 39% could carry out IADLs independently, suggesting the need for significant support from caregivers.
All patients were evaluated for cognitive dysfunction with the MMSE, CDT, and CIB tests and for depression with the GDS test described in the research design and methods section. Two patients were unable to perform CDT/CIB due to language barrier, although they were able to complete tasks on other measures. The mean CIB score for the population was 6 and mean CDT score was 14. Of all the patients, 35% were below the mean CIB score, and 38% were below the mean CDT score. Twelve percent of patients had a MMSE score below 24. MMSE score correlated with CIB as well as CDT scores (r = 0.45, P < 0.0004 and r = 0.33, P < 0.01, respectively). Next, we evaluated the relationship between cognitive dysfunction and glycemic control as measured by A1C levels. An inverse correlation was observed between CIB and A1C (r =−0.37, P < 0.004), as well as CDT and A1C (r = −0.38, P < 0.003); however, MMSE, demographic, depression, and other variables did not correlate with A1C. Simple linear regression models confirmed both CIB (R2 = 0.139, P = 0.004) and CDT (R2 = 0.144, P = 0.003) to be predictive for glycemic control. In a multivariate analyses, controlling for variables of interest including age, sex, living status, BMI, duration of diabetes, depression, MMSE, education, and other comorbidities, cognitive dysfunction measured by either CIB or CDT was the only predictor of poor glycemic control. Patients with high or low MMSE scores did not differ in diabetes control as seen by A1C level (8.44 ± 1.66 vs. 7.81 ± 1.32%; OR 1.36 [95% CI 0.82–2.254]). However, patients with cognitive dysfunction had a higher A1C compared with patients without cognitive dysfunction; A1C in high versus low CIB was 8.7 ± 1.4 vs. 7.5 ± 1.2%, respectively (2.016 [1.258–3.229]; P < 0.003), and A1C in high versus low CDT was 8.4 ± 1.6 vs. 7.6 ± 1.1% (P < 0.05) (Fig. 1).
Figure 1.
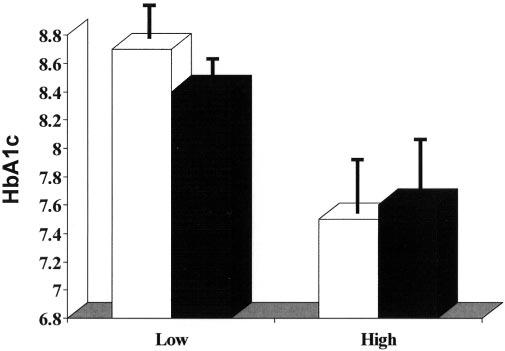
Patients with cognitive dysfunction (CIB ≤5 or CDT ≤13) had a higher A1C, indicating poorer glycemic control compared with patients without cognitive dysfunction (P < 0.003 with CIB and P < 0.05 with CDT).□, CIB; ■, CDT.
Thirty-three percent of patients had depressive symptoms as suggested by GDS scores ≥5. No correlation was observed between CIB, CDT, or MMSE scores and depression; however, patients with depression had greater difficulty completing the tasks of the IADLs (5.7 vs. 4.6; P < 0.03; 0.720 ([0.531–0.976]). Glycemic control was not associated with the presence of depression as assessed by the GDS.
We next evaluated the group of patients with low versus high CIB scores (Table 1). We did not observe significant differences in age, sex, and duration of diabetes in patients with or without cognitive dysfunction (low versus high CIB). However, patients with a low CIB score had a lower BMI (26 vs. 30; 0.883 [0.786–0.992]; P < 0.03) and were more likely to be on insulin treatment (P = 0.05). There was a higher incidence of weight loss, hypoglycemic episodes, and difficulty performing IADLs independently in patients with cognitive dysfunction; however, the differences did not reach statistical significance. More than a third (35%) of patients with a low CIB score were living alone, which puts this vulnerable population at higher risk of complications due to the multiple barriers they face.
CONCLUSIONS
Elderly patients with diabetes have an increased risk of developing cognitive problems. Our study is the first to evaluate cognitive dysfunction in older adults with diabetes and to correlate it with diabetes control. One-third of the study population had cognitive dysfunction as described by the CIB, and its presence was associated with poor diabetes control.
Cognitive functions that enable complex behaviors are particularly important for patients with diabetes. Ever since landmark trials demonstrated a decline in diabetes-related complications following tight glycemic control (35,36), diabetes treatment regimens have become more complex in an effort to achieve this goal. However, older patients with diabetes and concomitant cognitive dysfunction may be unable to follow complicated regimens (e.g., multiple daily insulin injections with or without a sliding scale, multiple oral medications, complex dietary regimen). These patients may be at increased risk of treatment complications (e.g., omission of meals leading to hypoglycemia or incorrect dose or timing of insulin injections and/or oral medications). Thus cognitive dysfunction is an important comorbidity that needs to be identified in older adults with diabetes for goal adjustment and/or individualization and simplification of treatment plans. To that end, the fact that 35% of our study patients with cognitive dysfunction were living alone is worrisome. Patients living alone typically do not have the benefit of interacting with, or being closely observed by, family members or friends over an extended period of time. As a result, health care providers must rely on self-report of complications such as hypoglycemia and other health problems with these patients, which may be underreported.
In our study, we have utilized easily administered tools to assess cognitive function. The CIB was designed specifically to assess working memory and executive function components of cognitive function. As this test has not been fully validated yet, we have further confirmed our results using a validated CDT. CIB and CDT were superior at identifying patients with cognitive dysfunction, compared with MMSE, a more widely used tool to evaluate cognitive dysfunction. MMSE has been reported to have low sensitivity in detecting subtle cognitive dysfunction. In an analysis of multiple longitudinal studies in patients with diabetes who were at higher risk of cognitive dysfunction, MMSE proved less sensitive than other psychometric tests (37). However, with only seven patients with low MMSE score in this study, there is a higher risk of sampling error. Performance on the CIB is related to performance on standardized measures of memory and executive functions such as Trail Making B, Hopkins Verbal Learning, and verbal fluency tests (10). CIB was more sensitive in predicting poor glycemic control than CDT. Subtle changes in cognition, especially executive functions, are difficult to detect during a short office visit, and tools such as CIB or CDT can be used to identify vulnerable individuals with cognitive dysfunction quickly.
Patients with diabetes are twice as likely to experience depression when compared with individuals without diabetes (38). In our study of older patients with diabetes, 32% of men and 34% of women reported depressive symptoms. Depression in patients with diabetes is independently associated with increased healthcare use and expenditures (39). Although diabetes self-management could be affected by depression, we did not find an association between the presence of depression and glycemic control. However, depression was associated with decreased ability to perform IADLs, which may add to the functional disability and dependence observed in older patients with diabetes.
The high prevalence of functional disabilities observed in our study population is consistent with prior reports. Diabetes has been associated with increased incidence of functional disabilities (11,18) and increased risk of falls and fractures (40). Cognitive functions, especially executive dysfunction, has been reported to correlate with inability to perform lower-extremity tasks (21). These data offer insight into why older adults with diabetes are at higher risk of falls (42). Thirty-three percent of the study patients had a history of falls compared with a general population of older adults without diabetes (42). Falls and fear of falls, possibly indicating balance and gait disturbance or muscle deconditioning, can increase the risk of injuries in this vulnerable population. Forty-eight percent of the study population had hearing impairments compared with 38% in the general population age >65 years, and 53% had vision impairments compared with 17% in the national population of older adults (43). Hearing and vision impairments can also add to functional decline and increased morbidity. While some of these disabilities can be improved (e.g., physical therapy for deconditioning and gait training), it is imperative that clinicians screen for these barriers in older patients with diabetes.
Our study was conducted at a tertiary care specialty setting. Patients in this setting tend to be highly motivated, educated, and have excellent support systems. We presume that the prevalence of barriers to diabetes control will be even higher in community settings, and these barriers may remain undiagnosed. Adverse outcomes due to unrecognized barriers would also be more prevalent in these settings.
In summary, this study identifies the high prevalence of cognitive dysfunction, depression, and functional disabilities among the elderly with diabetes and draws attention to various challenges in their management. First, all older patients with diabetes need to be evaluated for barriers to safe and effective diabetes control. Screening for subtle cognitive dysfunction is important when complicated treatment regimens are used. Second, goals for glycemic control may need to be adjusted and diabetes treatment regimens simplified. Third, older patients with diabetes and executive dysfunction may need special education and skills to manage their disease. Family members who live with patients or who are caregivers from a distance may benefit from education and support to enable them to effectively help these older patients. Lastly, it is essential to formulate diabetes treatment regimens, which are least likely to cause hypoglycemia. The risk versus benefit ratio of glycemic control needs to be frequently assessed among elderly with cognitive dysfunction to achieve the tightest possible control with the lowest possible risk of hypoglycemia.
Acknowledgments
Funding was provided by a grant from the Diabetes and Endocrinology Research Center National Institutes of Health 5P30 DK36836-19 (to M.M.) and the National Institute of Health DK60115 (to K.W.).
An earlier version of the article was presented in abstract form at the 65th annual meeting of the American Diabetes Association, San Diego, California, 10–14 June 2005.
Abbreviations
- ADL
activity of daily living
- CDT
clock-drawing test
- CIB
clock in a box
- GDS
Geriatric Depression Scale
- IADL
instrumental ADL
- MMSE
Mini Mental State Examination
Footnotes
A table elsewhere in this issue shows conventional and Système International (SI) units and conversion factors for many substances.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Yaffe K, Blackwell T, Kanaya AM, Davidowitz N, Barrett-Connor E, Krueger K. Diabetes, impaired fasting glucose, and development of cognitive impairment in older women. Neurology. 2004;63:658–663. doi: 10.1212/01.wnl.0000134666.64593.ba. [DOI] [PubMed] [Google Scholar]
- 2.Crooks VC, Buckwalter JG, Petitti DB. Diabetes mellitus and cognitive performance in older women. Ann Epidemiol. 2003;13:613–619. doi: 10.1016/S1047-2797(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 3.Ryan CM. Diabetes, aging, and cognitive decline. Neurobiol Aging. 2005;26(Suppl 1):21–25. doi: 10.1016/j.neurobiolaging.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Ryan CM. Effects of diabetes mellitus on neuropsychological functioning: a lifespan perspective. Semin Clin Neuropsychiatry. 1997;2:4–14. doi: 10.1053/SCNP00200004. [DOI] [PubMed] [Google Scholar]
- 5.Hassing LB, Grant MD, Hofer SM, Pedersen NL, Nilsson SE, Berg S, McClearn G, Johansson B. Type 2 diabetes mellitus contributes to cognitive decline in old age: a longitudinal population-based study. J Int Neuropsychol Soc. 2004;10:599–607. doi: 10.1017/S1355617704104165. [DOI] [PubMed] [Google Scholar]
- 6.Messier C. Impact of impaired glucose tolerance and type 2 diabetes on cognitive aging. Neurobiol Aging. 2005;26(Suppl 1):26–30. doi: 10.1016/j.neurobiolaging.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Arvanitakis Z, Wilson RS, Bienias JL, Evans DA, Bennett DA. Diabetes mellitus and risk of Alzheimer disease and decline in cognitive function. Arch Neurol. 2004;61:661–666. doi: 10.1001/archneur.61.5.661. [DOI] [PubMed] [Google Scholar]
- 8.Ryan CM, Williams TM. Effects of insulin-dependent diabetes on learning and memory efficiency in adults. J Clin Exp Neuropsychol. 1993;15:685–700. doi: 10.1080/01688639308402589. [DOI] [PubMed] [Google Scholar]
- 9.Gold AE, Deary IJ, Frier BM. Hypoglycemia and cognitive function. Diabetes Care. 1993;16:958–959. doi: 10.2337/diacare.16.6.958. [DOI] [PubMed] [Google Scholar]
- 10.Grande L, Milberg W, Rodolph J, Gaziano M, McGlinchey R. A timely screening for executive functions and memory. J Int Neuropsychol Soc. 2005;11(Suppl 1):9–10. [Google Scholar]
- 11.Kuo HK, Jones RN, Milberg WP, Tennstedt S, Talbot L, Morris JN, Lipsitz LA. Effect of blood pressure and diabetes mellitus on cognitive and physical functions in older adults: a longitudinal analysis of the advanced cognitive training for independent and vital elderly cohort. J Am Geriatr Soc. 2005;53:1154–1161. doi: 10.1111/j.1532-5415.2005.53368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abbatecola AM, Paolisso G, Lamponi M, Bandinelli S, Lauretani F, Launer L, Ferrucci L. Insulin resistance and executive dysfunction in older persons. J Am Geriatr Soc. 2004;52:1713–1718. doi: 10.1111/j.1532-5415.2004.52466.x. [DOI] [PubMed] [Google Scholar]
- 13.Seltzer B, Vasterling JJ, Mathias CW, Brennan A. Clinical and neuropsychological correlates of impaired awareness of deficits in Alzheimer disease and Parkinson disease: a comparative study. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14:122–129. [PubMed] [Google Scholar]
- 14.McKhann GM, Albert MS, Grossman M, Miller B, Dickson D, Trojanowski JQ. Clinical and pathological diagnosis of frontotemporal dementia: report of the Work Group on Frontotemporal Dementia and Pick's Disease. Arch Neurol. 2001;58:1803–1809. doi: 10.1001/archneur.58.11.1803. [DOI] [PubMed] [Google Scholar]
- 15.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 16.Egede LE. Diabetes, major depression, and functional disability among U.S. adults. Diabetes Care. 2004;27:421–428. doi: 10.2337/diacare.27.2.421. [DOI] [PubMed] [Google Scholar]
- 17.Egede LE. Effect of comorbid chronic diseases on prevalence and odds of depression in adults with diabetes. Psychosom Med. 2005;67:46–51. doi: 10.1097/01.psy.0000149260.82006.fb. [DOI] [PubMed] [Google Scholar]
- 18.Gregg EW, Beckles GL, Williamson DF, Leveille SG, Langlois JA, Engelgau MM, Narayan KM. Diabetes and physical disability among older U.S. adults. Diabetes Care. 2000;23:1272–1277. doi: 10.2337/diacare.23.9.1272. [DOI] [PubMed] [Google Scholar]
- 19.Sinclair AJ, Girling AJ, Bayer AJ. Cognitive dysfunction in older subjects with diabetes mellitus: impact on diabetes self-management and use of care services: All Wales Research into Elderly (AWARE) Study. Diabetes Res Clin Pract. 2000;50:203–212. doi: 10.1016/s0168-8227(00)00195-9. [DOI] [PubMed] [Google Scholar]
- 20.Grigsby JKK, Baxter J, Shetterly SM, Hamman RF. Executive cognitive abilities and functional status among community-dwelling older persons in the San Luis Valley Health and Aging Study. J Am Geriatr Soc. 1998;46:590–596. doi: 10.1111/j.1532-5415.1998.tb01075.x. [DOI] [PubMed] [Google Scholar]
- 21.Ble A, Volpato S, Zuliani G, Guralnik JM, Bandinelli S, Lauretani F, Bartali B, Maraldi C, Fellin R, Ferrucci L. Executive function correlates with walking speed in older persons: the InCHIANTI study. J Am Geriatr Soc. 2005;53:410–415. doi: 10.1111/j.1532-5415.2005.53157.x. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state:” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Malloy PF, Cummings JL, Coffey CE, Duffy J, Fink M, Lauterbach EC, Lovell M, Royall D, Salloway S. Cognitive screening instruments in neuropsychiatry: a report of the Committee on Research of the American Neuropsychiatric Association. J Neuropsychiatry Clin Neurosci. 1997;9:189–197. doi: 10.1176/jnp.9.2.189. [DOI] [PubMed] [Google Scholar]
- 24.Lomholt RK, Jurgensen KS. The minimental state examination in screening of cognitive dysfunction and dementia. Ugeskr Laeger. 1998;160:7251–7254. article in Danish. [PubMed] [Google Scholar]
- 25.Nishiwaki Y, Breeze E, Smeeth L, Bulpitt CJ, Peters R, Fletcher AE. Validity of the Clock-Drawing Test as a screening tool for cognitive impairment in the elderly. Am J Epidemiol. 2004;160:797–807. doi: 10.1093/aje/kwh288. [DOI] [PubMed] [Google Scholar]
- 26.Yamamoto S, Mogi N, Umegaki H, Suzuki Y, Ando F, Shimokata H, Iguchi A. The clock drawing test as a valid screening method for mild cognitive impairment. Dement Geriatr Cogn Disord. 2004;18:172–179. doi: 10.1159/000079198. [DOI] [PubMed] [Google Scholar]
- 27.Rouleau I, Salmon DP, Butters N, Kennedy C, McGuire K. Quantitative and qualitative analyses of clock drawings in Alzheimer's and Huntington's disease. Brain Cogn. 1992;18:70–87. doi: 10.1016/0278-2626(92)90112-y. [DOI] [PubMed] [Google Scholar]
- 28.Ferrucci L, Cecchi F, Guralnik JM, Giampaoli S, Lo Noce C, Salani B, Bandinelli S, Baroni A. Does the clock drawing test predict cognitive decline in older persons independent of the Mini-Mental State Examination? The FINE Study Group: Finland, Italy, The Netherlands Elderly. J Am Geriatr Soc. 1996;44:1326–1331. doi: 10.1111/j.1532-5415.1996.tb01403.x. [DOI] [PubMed] [Google Scholar]
- 29.Mendez MF, Ala T, Underwood KL. Development of scoring criteria for the clock drawing task in Alzheimer's disease. J Am Geriatr Soc. 1992;40:1095–1099. doi: 10.1111/j.1532-5415.1992.tb01796.x. [DOI] [PubMed] [Google Scholar]
- 30.Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000;15:548–561. doi: 10.1002/1099-1166(200006)15:6<548::aid-gps242>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 31.Scanlan JM, Brush M, Quijano C, Borson S. Comparing clock tests for dementia screening: naive judgments vs formal systems: what is optimal? Int J Geriatr Psychiatry. 2002;17:14–21. doi: 10.1002/gps.516. [DOI] [PubMed] [Google Scholar]
- 32.Storey JE, Rowland JT, Basic D, Conforti DA. Accuracy of the clock drawing test for detecting dementia in a multicultural sample of elderly Australian patients. Int Psychogeriatr. 2002;14:259–271. doi: 10.1017/s1041610202008463. [DOI] [PubMed] [Google Scholar]
- 33.D'Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract. 1994;11:260–266. doi: 10.1093/fampra/11.3.260. [DOI] [PubMed] [Google Scholar]
- 34.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 35.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 36.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 37.Allen KV, Frier BM, Strachan MW. The relationship between type 2 diabetes and cognitive dysfunction: longitudinal studies and their methodological limitations. Eur J Pharmacol. 2004;490:169–175. doi: 10.1016/j.ejphar.2004.02.054. [DOI] [PubMed] [Google Scholar]
- 38.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 39.Finkelstein EA, Bray JW, Chen H, Larson MJ, Miller K, Tompkins C, Keme A, Manderscheid R. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care. 2003;26:415–420. doi: 10.2337/diacare.26.2.415. [DOI] [PubMed] [Google Scholar]
- 40.Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR. Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab. 2001;86:32–38. doi: 10.1210/jcem.86.1.7139. [DOI] [PubMed] [Google Scholar]
- 41.Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51:S265–280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
- 42.Blaum CS, Ofstedal MB, Langa KM, Wray LA. Functional status and health outcomes in older americans with diabetes mellitus. J Am Geriatr Soc. 2003;51:745–753. doi: 10.1046/j.1365-2389.2003.51256.x. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention National Center for Health Statistics, Trends in Health and Aging [article online] Available at http://www.cdc.gov/nchs/agingact.htm. Accessed 21 April 2006.


