Abstract
Background
Severe acute respiratory syndrome (SARS) has only recently been described. We provide individual patient data on the clinical course, treatment and complications experienced by 14 front-line health care workers and hospital support staff in Toronto who were diagnosed with SARS, and we provide follow-up information for up to 3 weeks after their discharge from hospital.
Methods
As part of the initial response to the SARS outbreak in Toronto, our health care centre was asked to establish a SARS unit for health care workers who were infected. Patients were admitted to this unit and were closely monitored and treated until they were well enough to be discharged. We prospectively compiled information on their clinical course, management and complications and followed them for 3 weeks after discharge.
Results
The 11 women and 3 men described here (mean age 42 [standard deviation {SD} 9] years) were all involved in providing medical or ancillary hospital services to patients who were later found to have SARS. Onset of symptoms in 4 of our patients who could clearly identify only a single contact with a patient with SARS occurred on average 4 (SD 3) days after exposure. For the remaining 10 patients with multiple patient contacts, symptom onset followed exposure by a mean of 3.5 (SD 3) days after their exposure. All patients were treated with ribavirin, and all patients received levofloxacin. Many experienced major complications. Dyspnea was present in 12 patients during their stay in hospital, and all developed abnormalities on chest radiograph; 3 patients developed severe hypoxemia (PaO2 < 50 mm Hg). All patients experienced a drop in hemoglobin. Nine patients had hemolytic anemia. Three patients experienced numbness and tingling in their hands and feet, and 2 developed frank tetany. All 3 had magnesium levels that were less than 0.1 mmol/L. All patients recovered and were discharged home. At a follow-up examination 3 weeks after discharge (5 weeks after onset of illness), all patients were no longer weak but continued to become fatigued easily and had dyspnea on minimal exertion. For 5 patients, chest radiographs still showed residual disease.
Interpretation
SARS is a very serious illness even in healthy, relatively young people. The clinical course in our patients, all of whom met the case definition for SARS (which requires pulmonary involvement), resulted in dyspnea and, in some individuals, severe hypoxemia. Severe hemolytic anemia may be a feature of SARS or may be a complication of therapy, possibly with ribavirin.
The early phases of the Toronto outbreak of severe acute respiratory syndrome (SARS) have been described elsewhere.1 A summary report of 144 cases of SARS,2 which includes the 14 cases reported here and another 15 that were reported earlier in CMAJ,3 has been published. In this report, we provide additional details about the main clinical features, management, and severity and frequency of complications of SARS. We also include information about our patients' clinical status 1 week and 3 weeks post discharge from our SARS unit.
Methods
As the number of patients with SARS increased in Toronto in March 2003, West Park Healthcare Centre, a 478-bed facility providing rehabilitation, complex continuing care and long-term care, was asked to establish an operational SARS unit to provide medical care to health care workers affected with SARS. Staff assigned to the new unit included a manager, nurse practitioner, advanced practice nurse, unit clerk, clinical pharmacist, registered dietitian, respiratory therapists, x-ray and laboratory technicians, and a chaplain. Nursing care was provided by nurses at our centre supplemented by additional nurses hired from the community. Because our centre did not usually provide critical care, nurses with experience in critical care were temporarily transferred from other regional hospitals. Our hospital infection control nurse was on site several times a day to monitor infection control measures and precautions. Medical coverage was provided by 2 staff physicians: a family practitioner (who is also the Chief of Staff) and a respirologist (who is the physician in charge of the Tuberculosis Service).
Diagnosis of probable SARS was based on the case definition of the World Health Organization.4 This diagnosis requires that the patient have radiographic features of pneumonia, respiratory distress syndrome, or an unexplained respiratory illness resulting in death with autopsy results demonstrating pathology of respiratory distress syndrome without an identifiable cause.
Data collection
We prospectively documented daily changes in the physical examination, laboratory tests and clinical course for all patients. For this report, all 3 authors reviewed all the patients' records using a standard data collection form. The information retrieved included the following: age, sex, occupation, medical history, time and nature of exposure, symptoms and physical findings on admission, chest radiograph, ECGs, complete blood count with a differential, platelet and reticulocyte count, liver function tests, and measurement of urea and creatinine, albumin, electrolytes, magnesium, phosphate, calcium (ionized), lactate dehydrogenase (LD), creatine kinase (CK) and blood sugar.
Chest radiographs were performed on admission and thereafter as clinically indicated. Hematological and biochemical tests were done every 2 days or daily depending on the patient's clinical status. When clinically indicated, sputum, urine and blood specimens were sent for serology and for bacteriological testing. We interviewed all the patients to determine the number and health status of their household contacts. Microbiology investigations of specimens received from all of the SARS cases were conducted at local, national and international laboratories.
Our study was approved by the West Park Healthcare Centre research ethics board for the data collection and reporting. All patients gave approval for publication of details of their case histories.
Results
Initial assessment
Our 14 patients were initially assessed as outpatients at their place of employment 2–3 days after the start of their symptoms. None of the patients were suspected of having SARS at the time, and all were sent home with instructions to continue to measure their temperature and monitor for the appearance of respiratory symptoms. They were also instructed to return for further assessment if their symptoms worsened. All patients were home for a period of 4.6 (standard deviation [SD] 2.0, range 1–8) days before admission to our SARS unit (Table 1). On the day of admission of the first patients to our unit (Mar. 23, 2003), some of them had returned to the emergency department because of worsening of their symptoms; others still at home were contacted and instructed to go directly to West Park Healthcare Centre for admission. We did not see these patients before their admission to the SARS unit.
Table 1
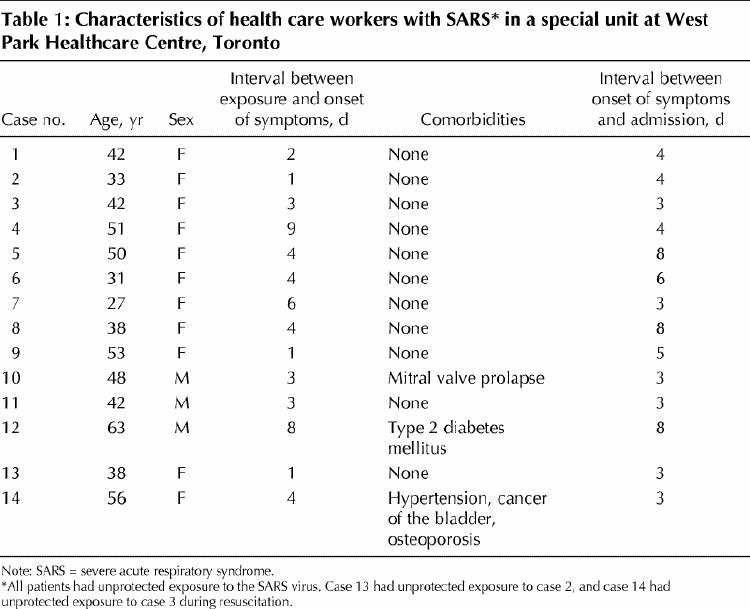
Clinical presentation
The patients, 11 women and 3 men aged between 27 and 63 (mean 42 [SD 9]) years, were health care workers or support staff who had been involved in the care of patients who were later found to have SARS (Table 1). Contact with SARS patients had occurred before full infection control measures for personal protection were instituted. Almost all our patients were healthy, young adults. None were smokers. Most had multiple potential exposures. Twelve were able to indicate the date of the exposure that they believed had resulted in infection with SARS. On admission, 12 patients were considered to have probable SARS and 2 were thought to have suspect SARS.
Of the 4 patients (cases 1, 3, 8 and 9) who could identify a single contact with a patient with SARS, the interval between putative exposure and onset of symptoms (headache, fever, malaise, myalgias) was 4 (SD 3) days. For the 10 patients with multiple contacts with patients with SARS, the interval between the last unprotected contact and development of symptoms was 3.5 (SD 3) days. Among our patients, fever, headache, myalgias and malaise were present from the beginning.
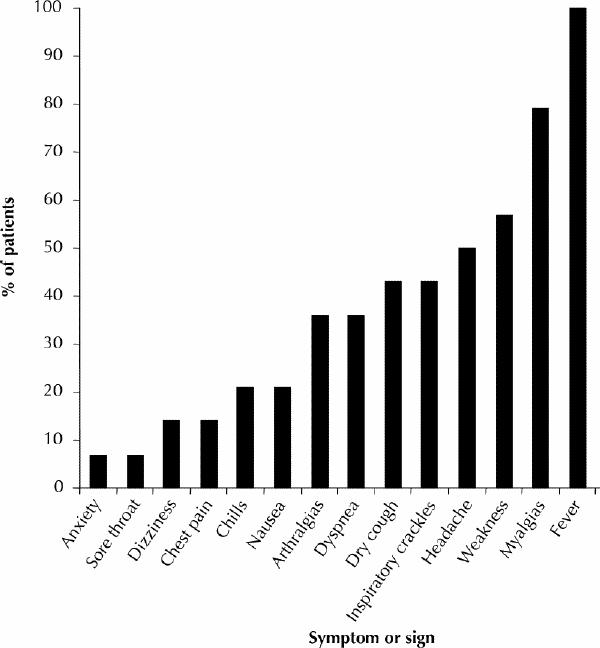
The symptoms and signs on admission are illustrated in Fig. 1. All patients had a temperature that was higher than 38°C once antipyretic drugs were stopped. Eleven (79%) had generalized severe myalgias that involved the extremities and, in some, the pelvic girdle and the chest wall. Eight (57%) experienced profound generalized weakness. Mild nonspecific headache was present in 7 patients (50%), and 6 (42%) presented with a history of dry cough. None reported a productive cough. Nausea was present in 3 patients; none had diarrhea.
Anorexia was experienced by all patients during their first week in hospital; their diets were modified and limited to fluids and soft foods. Nausea and vomiting developed in 7 patients 2–3 days after admission. It was controlled in all but 1 patient with antiemetic drugs. Mild diarrhea, although not present on admission, did develop on day 4 in 3 patients. Six patients required intravenous rehydration.
The initial treatment consisted of a loading dose of 2 g of intravenous ribavirin, followed by 1 g every 6 hours for 4 days and then 0.5 g every 8 hours for 3 days for all suspect and probable cases. In addition, levofloxacin, 500 mg daily for 6 days, was added for all probable cases (those who had abnormal chest radiographs).
Initially, none of the patients received steroids. During their hospital course, 5 patients were given intravenous methylprednisolone at a high dose (125 mg intravenously every 6 hours) for 1 to 2 days, followed by a tapering dose of prednisone (initial dose 40 mg daily). Two patients received oral prednisone alone. In 3 patients, steroids were prescribed due to severe respiratory failure (PaO2 < 50 mm Hg). In the remaining 4, steroids were prescribed because of severe hemolysis.
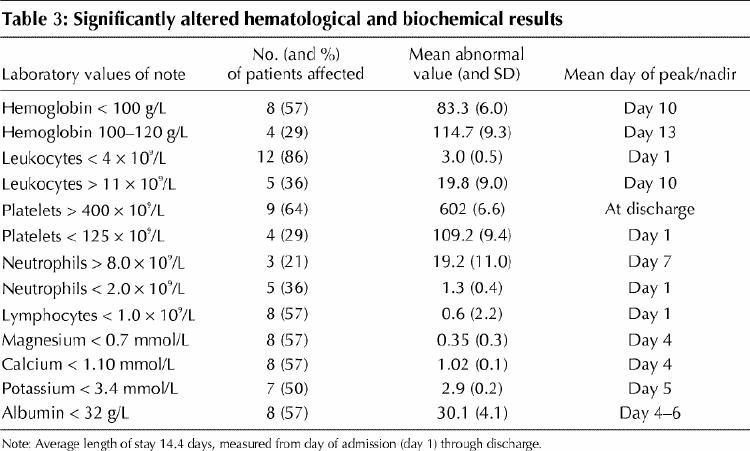
The clinical course, treatment and laboratory test results are shown in Figs. 2, 3 and 4 and summary measures of the various laboratory tests (admission, peak and nadir values) in Tables 2 and 3. Here we emphasize some of the major symptoms and complications that developed during the course of the patients' illness.
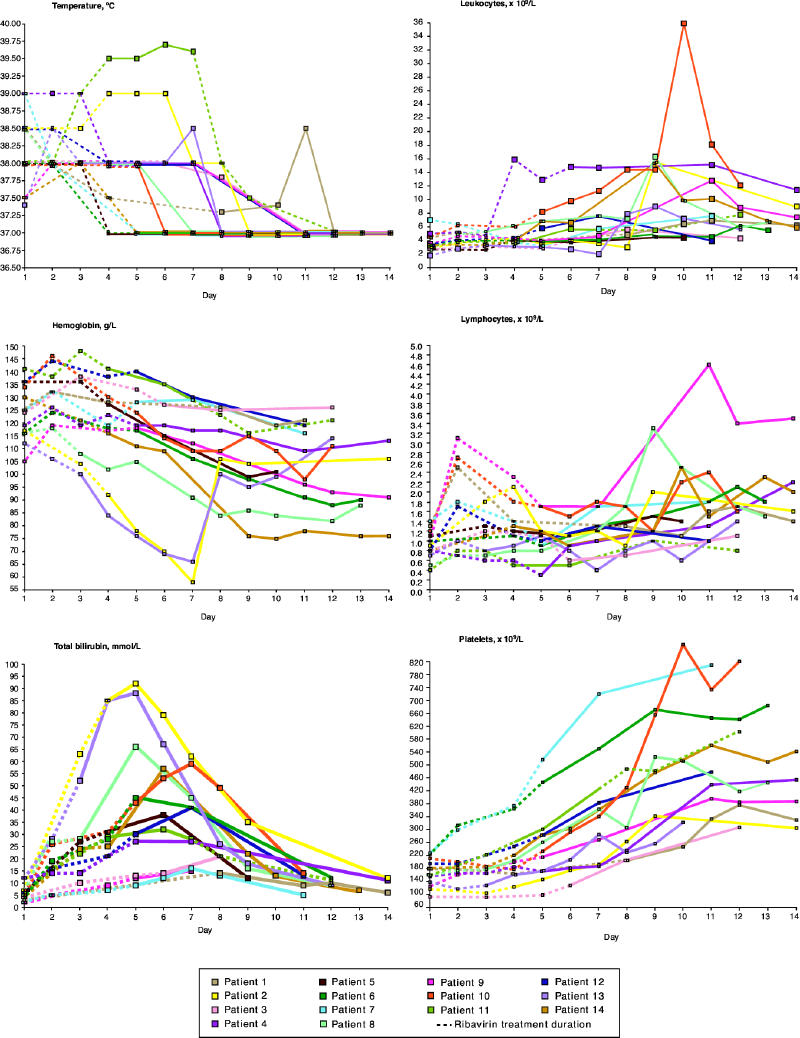
Fig. 2: Temperature and hematological measurements in 14 patients treated for SARS at the West Park Healthcare Centre, Toronto. SARS = severe acute respiratory syndrome. Photo: Myra Rudakewich
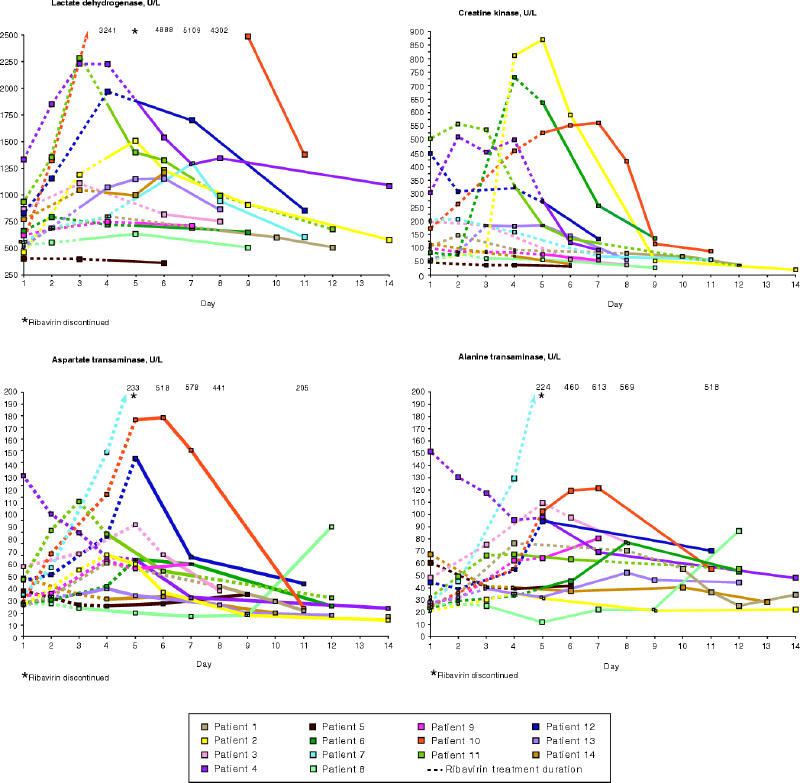
Fig. 3: Lactate dehydrogenase, creatine kinase, aspartate transaminase and alanine transaminase measurements in 14 patients treated for SARS at the West Park Healthcare Centre, Toronto. Photo: Myra Rudakewich
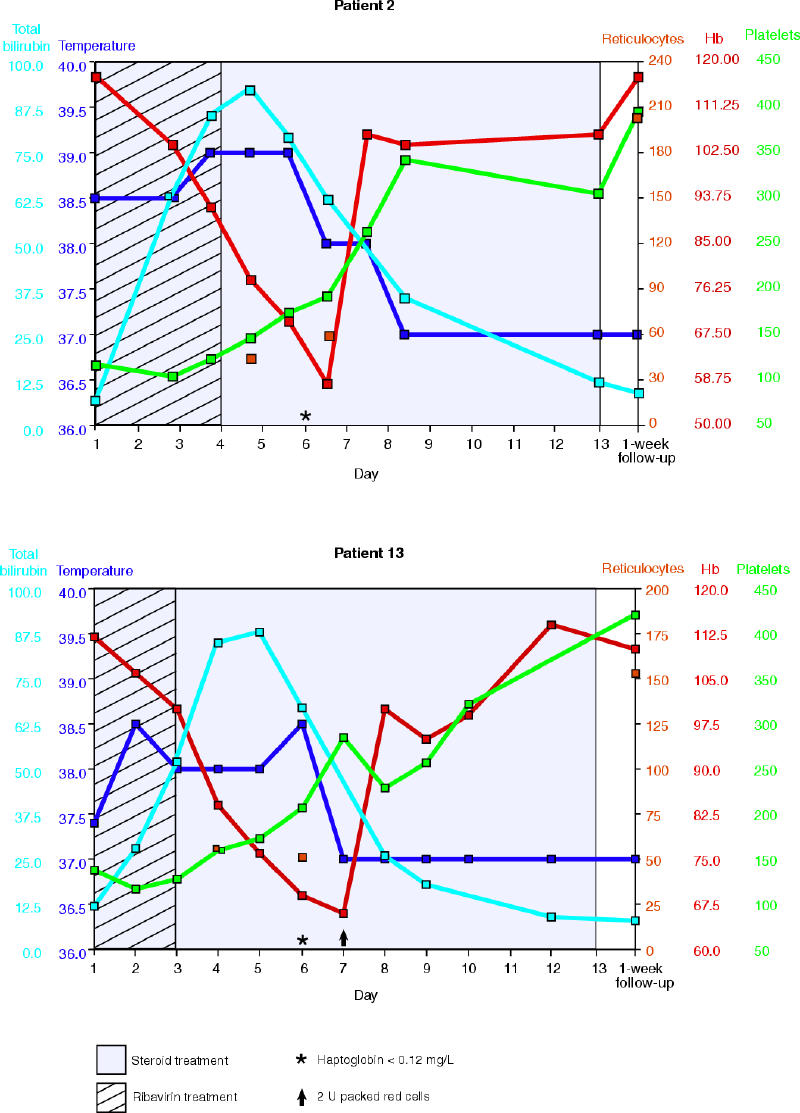
Fig. 4: Temperature measurements and selected laboratory data for 2 of the 14 patients treated for SARS at the West Park Healthcare Centre, Toronto. Photo: Myra Rudakewich
Table 2
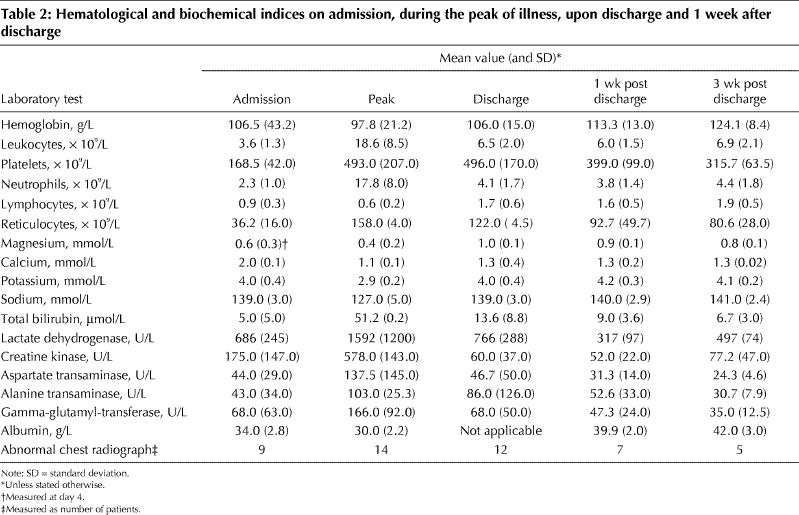
Table 3
Laboratory diagnosis of SARS
Direct microscopic examination for bacteria and fungi including Pneumocystis jiroveci on all respiratory specimens was negative. Routine bacterial and fungal cultures were negative for all blood, respiratory and urine specimens. Cultures for Legionella spp., direct fluorescent antibody testing against Legionella spp. on all respiratory specimens, and testing for the presence of Legionella pneumophila serogroup 1 antigen in urine specimens yielded negative results.
DNA was extracted from all respiratory specimens. Polymerase chain reaction (PCR) detection for targets specific for atypical pneumonia agents including L. pneumophila, Mycoplasma pneumoniae, Chlamydia pneumoniae, C. psittaci and Chlamydophila at the genus level was found to be negative. PCR testing targeting Yersinia pestis and Bacillus anthracis was also found to be negative. No product was obtained using universal primers targeting the 16S rRNA gene sequence. Virological examination of SARS specimens was initiated immediately upon receipt. Direct fluorescent antibody testing against influenza A/B, parainfluenza 1/2/3, adenovirus and respiratory syncytial virus was completed on all nasopharyngeal swabs and was negative.
PCR testing for the coronavirus was positive on nasopharyngeal swabs from 4 patients. In addition, serum was positive by immunofluorescent assay (IFA) in one of them. Negative results for coronavirus were present in the remaining 10 patients.The results of serum enzyme-linked immunosorbent assay (ELISA) were negative in all patients.
Complications of SARS in our patients
Pulmonary disease
Cough and dyspnea were common on admission. Dyspnea was present in 5 of our patients on admission and developed in a further 7. Thus, overall, 12 patients developed shortness of breath. In 7 patients, the dsypnea prevented them from walking more than 5 metres.
On admission, 12 of the 14 patients had abnormal chest radiographs. The remaining 2 patients developed abnormalities on chest radiographs within 3 days of admission. Focal air space disease was seen in all patients. Bilateral abnormalities were present in 7 patients. One patient had minimal unilateral involvement.
Figs. 5 and 6 show the chest radiographs of 2 of our patients. Case 10 had an initial abnormal chest radiograph showing perihilar air space disease that continued to deteriorate. Case 4 had a relatively unremarkable admission film that showed deterioration by day 3. At discharge, between 12 and 15 days after admission, 2 patients had normal chest radiographs and 12 patients showed improvement in their radiographs.
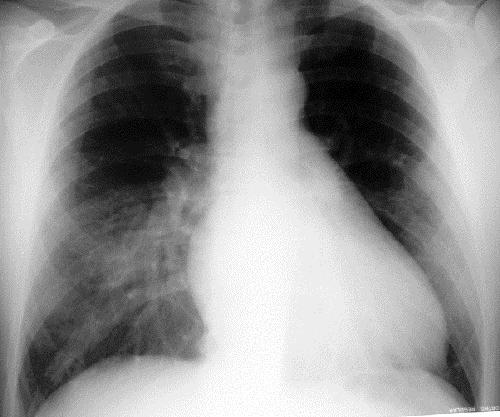
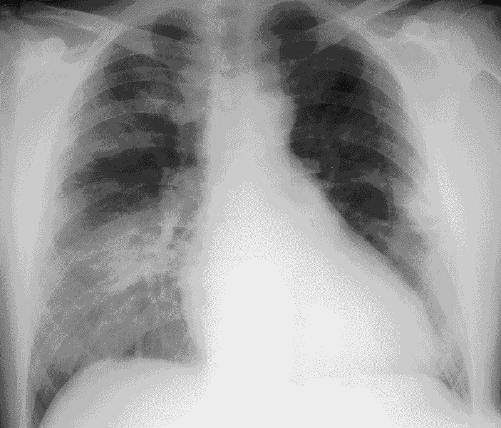
Figure 5. Continued.
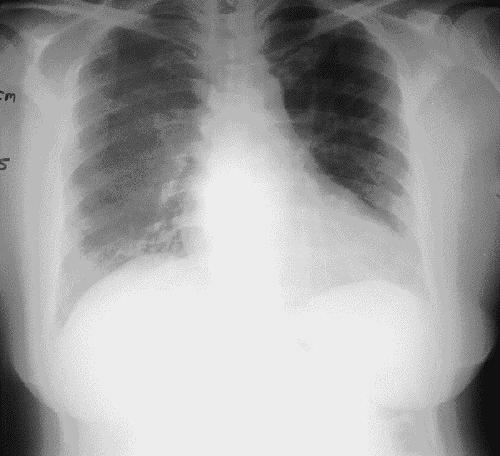
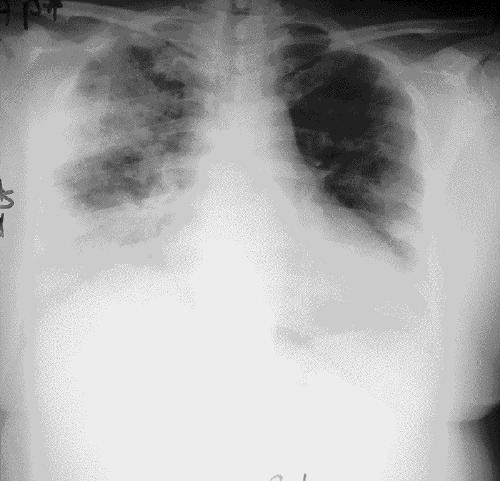
Figure 6. Continued.
Mild hypoxemia (SaO2 < 95% breathing room air) was present on admission in 3 patients, but by the fourth day in hospital an additional 4 patients had mild hypoxemia (SaO2 < 95% on room air) and required supplemental oxygen. Three patients (cases 4, 6 and 12) developed severe hypoxia (PaO2 ≤50 mm Hg). The management of these patients with more severe respiratory impairment consisted of supplemental oxygen (high FiO2 [50%]) and high doses of intravenous steroids. We were unable to transfer these patients to an acute care facility for the following reasons: we were involved in caring for patients with SARS early in the outbreak and it was felt that we could manage them, short of intensive care unit care; the transfer procedure between hospitals for patients with SARS was not yet clear; and the local hospitals had not yet established intensive care units with isolation capacity. At West Park Healthcare Centre, there is a ventilatory care unit with staff familiar with the care of ventilator-dependent patients. The attending respirologist, the nursing staff and the respiratory therapists monitored these patients at the bedside and, if mechanical ventilation had been required, we were prepared to initiate it. These patients perhaps could have benefited from intubation and mechanical ventilation, but they were successfully managed conservatively.
There was a good correlation between the severity of dyspnea and findings on chest radiographs and blood gas determinations; as dyspnea worsened, so did the chest radiographs. For example, a 51-year-old woman with mild dyspnea on admission and an unremarkable chest radiograph developed shortness of breath on day 3. This increased to the point where she could not walk. Her blood gases on room air showed a pH of 7.51, PaCO2 32 mm Hg, PaO2 47 mm Hg and HCO3 25 mEq/L. The chest radiograph demonstrated extensive air space disease predominantly involving the right lung without associated pleural effusion or hilar or mediastinal adenopathy. However, there were exceptions. Two patients (cases 1 and 11) had no shortness of breath even though their chest radiographs were similar to those of the patients with dyspnea.
Hemolytic anemia
In 9 patients, the hemoglobin level fell 38 (SD 13) g/L. Blood smears for all 9 patients showed polychromasia and nonspecific erythrocyte changes (but not schistocytes). Some smears showed hypersegmented neutrophils. The fall in hemoglobin was accompanied by an increase in total bilirubin of 51 (SD 20) μmol/L, increased indirect bilirubin (49.4 [SD 18.3] μmol/L) and very low haptoglobin values (< 0.12 g/L). In all cases, the fall in hemoglobin was presumed to be a result of hemolysis. Although 3 patients (cases 2, 13 and 14) required transfusion of erythrocytes, only 2 received it because the other patient (case 14) refused. Patients who did not show evidence of hemolysis (5/14) did have slight reductions in hemoglobin (8.4 [SD 5.6] g/L).
In all cases, hemolytic anemia became evident between 4 and 6 days after the patient started receiving ribavirin and levofloxacin. Ribavirin was started on the day of admission. In 8 patients, we discontinued the ribavirin and the levofloxacin at the same time. In 7 patients who showed evidence of hemolytic anemia and who did not receive transfusion, reticulocyte counts measured at 1 week after discharge were elevated (130 [SD 50] х 109/L). The initial hemoglobin level and the severity of the pneumonia were similar for those patients who developed hemolysis and for those who did not.
Two patients who had not demonstrated adverse affects attributed to the ribavirin did develop a relapse of fever and worsening of the abnormalities on their chest radiographs after discontinuing the drug. Oral ribavirin was restarted in both and the fever subsided 3 days after its reintroduction. The evolution of the abnormalities on chest radiograph was similar to that of the remaining 12 patients.
Leukopenia and leukocytosis were noted at different stages of the disease. Four patients initially presented with leukocyte counts of less than 4 х 109 L. Five developed significant elevations in their leukocytes, to a mean of 19.8 х 109 L by day 10. Similarly neutrophil counts in 5 of the patients were below normal, with a mean of 1.3 х 109 L at the time of admission. Four patients eventually experienced elevated neutrophils (mean 19.2 х 109 L) by day 7. Lymphopenia (0.7 [0.2] х 109 L) was present on admission in 8 of our patients but had returned to normal by discharge.
Elevated LD and CK
High LD (mean 900 [SD 230] U/L) was present in 6 patients on admission. It increased to a mean 1608 (SD 1576) U/L in an additional 7 patients during the course of their illness. Of those patients with the highest values of LD, 1 patient (case 3) had minimal changes on chest radiograph and no hemolysis, 3 (case 4, 7 and 12) had extensive changes on chest radiograph and no hemolysis, and 5 had both hemolysis and extensive abnormalities on their chest radiograph.
High CK (peak 613.5 [SD 157] U/L) was seen in 6 patients. In 5 of these, there was also an increase in LD. In the 1 patient with elevated CK and normal LD, the transaminases were very high (case 7).
Hypomagnesemia and tetany
Values were within normal ranges in 6 patients and below normal in the remaining 8 patients, reaching a nadir, 0.35 (SD 0.3) mmol/L, on day 4. Three patients (cases 2, 8 and 13) experienced numbness and tingling in their hands and feet, and 2 of them developed tetany (stiffness and frank spasm of the hands and feet). In all 3 patients, the magnesium level was less than 0.1 mmol/L, and corrected calcium levels were 0.92 (SD 0.13) mmol/L. All 3 had a significant drop in their hemoglobin, and 2 (cases 2 and 13) received transfusion. Noninvasive measurement of PaCO2 revealed normal values. All 3 responded to magnesium and calcium replacement. Serum magnesium was not initially measured. However, following the development of tetany and hypomagnesemia in the 3 patients described above, we began to measure magnesium in the other patients.
Hypocalcemia and hypokalemia
Hypocalcemia was present in most patients (mean nadir 1.02 [SD 0.14] mmol/L) within 3 days of admission. Half of the patients developed hypokalemia with a mean nadir of 2.9 (SD 0.2) mmol/L by day 5. It had become normal by discharge.
ECG changes
ECG abnormalities, mainly minor atrial arrhythmias such as atrial extrasystoles, were noted in all patients. Mild T-wave inversion was noted in 2 patients, and 1 patient showed QT prolongation (0.49 seconds). One patient developed atrial fibrillation with rapid ventricular response (rate 179 beats per minute). This patient responded to medical cardioversion.
Psychological effects of SARS on health care workers
Most patients expressed feelings of fear, depression and anxiety at the time of the acute illness (see appendices containing patients' accounts of their illness at www.cmaj.ca). In addition, many expressed nonspecific anger and frustration at being in isolation and without contact with family and loved ones. This was particularly the case for those patients with young children, and especially the 2 patients whose children developed SARS. The fact that all the patients were health care workers or hospital support staff posed a special challenge for our team. They were compliant but, at times, challenging with regard to their status and treatment. As most of these patients were either critical care nurses or physicians, they wanted daily reports on their test results and wanted to discuss the abnormalities. These findings were similar to those reported by Maunder and colleagues.5
After one of our nurses was diagnosed with SARS, 24 members of the SARS unit team were quarantined, some at home and others on working quarantine. This was a source of considerable stress for our team.
Outcome
Patients remained in hospital for a mean of 14 (range 12–15) days. All improved clinically. Chest radiographs had completely cleared in 2 of the patients and had improved in the remaining 12 by the end of their stay in hospital. At the time of discharge, they had been afebrile for at least 72 hours. The hematological and biochemical values had also improved (Table 2).
Follow-up
All patients were seen in a special SARS clinic 1 week and 3 weeks after discharge. At the first follow-up visit, all the patients were feeling better, however, they still felt weak and complained of dyspnea on exertion. They all reported significant weight loss during their acute illness (mean 7 [SD 2] kg). As their appetite was improving, they were regaining some of their weight. Two patients had low grade fever (up 37.5°C) for 2–3 days following discharge. Only 2 patients had persistence of a slight dry cough. The chest radiograph was clear for 7 patients and, although improved, abnormalities on chest radiograph persisted for the remaining 7.
Three weeks after discharge, the patients were no longer as weak but still complained of easy fatiguability and dyspnea on climbing stairs. They had continued to regain weight, and the cough was no longer present. The chest radiograph had cleared for an additional 2 patients. For 5 patients the chest radiograph was still abnormal, but improvement was noted.
In those patients who experienced hemolysis, the reticulocyte count was well above normal (130 [SD 50] х 109/L) 1 week after discharge, and it remained slightly elevated at the 3-week follow-up visit. Hemoglobin had increased by a mean of 124 (SD 8) g/L.
Since the appointment at week 3 post discharge, we have seen 4 of the patients (case 1 because of severe insomnia; case 3 because of a recurrent cough and wheezing that developed after being well for over 1 week; case 14 because of severe insomnia, dyspnea and depression; and case 5 because she was out of town at the time of the 3-week follow-up clinic). We have kept in contact by telephone with all of the patients at least twice a week. One patient (case 10) has returned to work part-time but is extremely tired at the end of the day. The remaining patients are much better, but they are still experiencing insomnia, easy fatiguability and dyspnea following activities that did not cause it before their illness. One patient continued to have mild pyrexia on and off up to 37.6°C, mostly in the evenings 2 or 3 times a week.
We plan further follow-up of these patients with particular emphasis on pulmonary function. We are also planning chest CT scans and graduated exercise tests. Case 1 had a sleep study that showed severe periodic limb movements. We are therefore planning to do sleep studies in all or most of this cohort.
Household contacts
Our patients had a total of 33 household contacts. In 2 cases, one family member (a daughter aged 14 years and a daughter aged 17 years) was diagnosed with SARS 1 week and 12 days respectively after the parent had been removed from the household. Both children recovered uneventfully.
Interpretation
We report the main clinical features and the outcome of 14 SARS patients, all health care workers and hospital support staff, who had contracted the disease upon unprotected exposure at the hospital where case 2 of the Toronto outbreak had been admitted.1 Our findings are similar to those reported in larger numbers of patients both in Toronto and in Hong Kong.2,6,7,8 A report by Dwosh and colleagues3 describes the containment procedures taken in a community hospital. The situation in our hospital was different, because at the time of admission the patients were considered either to have suspect or probable SARS. Therefore, appropriate measures were taken to protect the staff from the beginning.
Our cases met the WHO case definition for SARS.4 Coronavirus was detected by PCR in only 4 of our patients. This probably indicates that, although recent data indicate that a coronavirus could be the causative agent,9,10,11 we do not yet have a reliable diagnostic test and the diagnosis is mainly based on the clinical, biochemical, radiological and epidemiological features.2,7,8,12
None of our patients required mechanical ventilation, despite 3 having had significant hypoxemia. They responded to close monitoring and aggressive treatment with supplemental oxygen and intravenous steroids.
There have been no designed controlled studies using ribavirin in the treatment of SARS. Empiric treatment with ribavirin, a ribonucleoside analogue, is based on its proposed mechanism of action as causing mutagenesis of RNA viral genomes. Apparently it has a broad spectrum of activity on RNA viruses and has been approved for the treatment of respiratory syncytial virus and hepatitis C in conjunction with interferon.13
All our patients were treated empirically with intravenous ribavirin. Because of the adverse effects observed in 12 patients, the drug was discontinued in all. In 2 patients, we observed a recurrence of the fever and worsening of the abnormalities seen on chest radiograph. We did not observe any deterioration in the remaining 12 patients.
It is our impression that the hemolytic anemia present in 9 of our patients had a deleterious effect and increased their morbidity. These adverse effects of ribavirin were not mentioned in some of the Hong Kong SARS reports,7,8 however, other sources have reported an association between ribavirin use and hemolysis.13 Examination of the clinical course of our patients and the frequencies of complications suggests that ribavirin may not have been effective and may actually have caused some of the complications. Only a randomized controlled clinical trial will resolve this question.
The initial level of LD was marginally elevated in all the patients. During the course of their illness, the peak value was over 1000 U/L in 4 patients, and over 1500 U/L in an additional 5 patients (peak 5109 U/L in one). High levels of LD are usually associated with tissue damage. In our patients these high levels may have reflected muscle tissue damage, hepatic injury and/or hemolysis. Although CK was elevated on admission in only 1 patient, it became elevated in another 5. In 3 patients, myalgias were predominant (cases 4, 6 and 11).
An elevated neutrophil count has been reported to be associated with an adverse outcome.11 In 4 of our patients neutrophil counts were extremely high (17.8 [9.3] х109/L). All of them had extensive radiographic abnormalities and a worsening of their clinical course consistent with the elevation in neutrophils. Lymphopenia was a consistent finding that was in agreement with previous reports.1,2,7,8 The initial low reticulocyte counts might reflect bone marrow suppression caused by ribavirin, as reported by Koren and colleagues.13
Another association with a poor outcome is the presence of diabetes,1,2 however, in our cohort only 1 patient had type 2 diabetes mellitus. Even though the initial course was complicated by respiratory insufficiency, there was an improvement and the patient's stay in hospital was not significantly prolonged. Hypomagnesemia was described in the report on the Toronto cases.2 We cannot explain this finding, because the usual causes14 were not present in our patients. We wonder if ribavirin excreted renally has an adverse effect on tubular reabsorption of magnesium.
The electrocardiographic abnormalities were most likely the result of electrolyte imbalances. QT prolongation and atrial disturbances can be seen in patients with low calcium, low potassium and/or low magnesium levels. The abnormalities resolved when the imbalances were corrected. The results of troponin assays were negative.
We had difficulties deciding on the appropriate timing for discharge. Without clear discharge criteria, Toronto hospitals have generally followed the World Health Organization (WHO) recommendations.15 We discharged patients after they had been afebrile for at least 72 hours and their biochemical, hematological and radiographic abnormalities were improving along with their clinical status. Only 2 patients had complete resolution of the abnormalities on chest radiograph at the time of discharge. All patients were discharged on home quarantine for an additional 14 days. This was in contrast to current recommendations that they remain quarantined for 7–10 days. We chose a longer period of time out of concern for relapse and the danger of transmission to contacts, partly because one of our patients' children developed SARS 12 days after the parent was removed from the household.
The follow-up of our patients has allowed us to appreciate that although the acute phase of the illness appears to have resolved, there are lingering nonspecific after-effects of this disease that perhaps may continue for an unknown period of time. None of our patients have reported secondary cases in their household following their discharge home.
As Maunder and colleagues found in their hospital,5 most patients voiced some complaints consistent with depression and anxiety regarding various facets of their disease, stay in hospital, personal and family impact, and the nature of their occupational exposure. Some reported insomnia and nightmares. This was compounded by their post-discharge home quarantine. The psychosocial aspects associated with this illness should not be underestimated and warrant further investigation. In addition to the effect on the patients, the psychological impact on staff and their families was also noted to be significant.
The transmission of SARS is believed to be the result of droplet exposure. Our observation suggests that this is indeed the case. The total number of household contacts of our patients was 33. It is remarkable that only 2 patients infected a family member (2 previously healthy teenagers). This in spite of unprotected contact in the home environment for a mean of 4.5 days and the presence of very young children in 2 of the households. We can only hypothesize that not all patients with SARS are as infectious as has been reported previously. This fact gives us some hope that this disease will not spread in a totally uncontrolled manner in the community.
Supplementary Material
Acknowledgments
We wish to thank Dr. Donald Low for his support and guidance and Dr. Richard Mah who worked tirelessly when the unit was first opened. We also want to thank all the dedicated staff who made this unit possible.
Footnotes
Fast-tracked article. Published at www.cmaj.ca on May 28, 2003. Revised on June 6, 2003.
This article has been peer reviewed.
Contributors: Drs. Avendano and Derkach were the only attending physicians at the SARS unit. Ms. Swan was seconded from the Tuberculosis Service to act as nurse practitioner, working in conjunction with the 2 physicians. All 3 authors collected the data and contributed to the writing of the paper.
Competing interests: None declared.
Correspondence to: Dr. Monica Avendano, Department of Respiratory Medicine, West Park Healthcare Centre, 82 Buttonwood Ave., Toronto ON M6M 2J5; fax 416 243-8947; monica.avendano@westpark.org
References
- 1.Poutanen SM, Low DE, Henry B, Finkelstein S, Rose D, Green K, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med 2003;348(20):1995-2005. [DOI] [PubMed]
- 2.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2003;289: [early online release 2003 May 6]. Available: http://jama.ama-assn.org/cgi/content/full/289.21.JOC30885v1 (accessed 2003 May 27). [DOI] [PubMed]
- 3.Dwosh HA, Hong HL, Austgarden D, Herman S, Schabas R. Identification and containment of an outbreak of SARS in a community hospital CMAJ 2003;168(11):1415-20. [PMC free article] [PubMed]
- 4.World Health Organization. Case definitions for surveillance of severe acute respiratory syndrome (SARS). Revised 2003 May 1. Available: www.who.int/csr/sars/casedefinition/en (accessed 2003 May 26).
- 5.Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168(10):1245-51. [PMC free article] [PubMed]
- 6.World Health Organization. Global surveillance for severe acute respiratory syndrome (SARS). Wkly Epidemiol Rec 2003;78(14):100-5. [PubMed]
- 7.Tsang KW, Ho PK, Ooi GC, Yee WK, Wang T, Chan-Yeung M, et al. A cluster of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003;348(20):1977-85. [DOI] [PubMed]
- 8.Lee N, Hui D, Alan W, Chan P, Cameron P, Joynt GM, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003;348(20):1986-94. [DOI] [PubMed]
- 9.Drosten C, Gunther S, Preiser W, van der Werf S, Brodt HR, Becker S, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 2003;348(20):1967-76. [DOI] [PubMed]
- 10.Ksiazek TG, Erdman D, Goldsmith C, Zaki SR, Peret T, Emery S, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003;348(20):1953-66. [DOI] [PubMed]
- 11.Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003;361(9366):1319-25. [DOI] [PMC free article] [PubMed]
- 12.Chan-Yeung M, Yu WC. Outbreak of severe acute respiratory syndrome in Hong Kong Special Administrative Region: case report. BMJ 2003;326(7394):850-2. [DOI] [PMC free article] [PubMed]
- 13.Koren G, King S, Knowles S, Phillips E. Ribavirin in the treatment of SARS: a new trick for an old drug. CMAJ 2003;168(10):1289-92. [PMC free article] [PubMed]
- 14.Dacey MJ. Endocrine and metabolic dysfunction syndromes in the critically ill. Crit Care Clin 2001;17(1):155-73.11219227
- 15.World Health Organization. Hospital discharge and follow-up policy for patients who have been diagnosed with severe acute respiratory syndrome (SARS). Geneva: The Organization; 2003. Available: www.who.int/csr/discharge/en (accessed 2003 May 27).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


