As of December 2002, an estimated 19.2 million women worldwide were living with HIV infection.1 It is clear that HIV-positive women are living longer and are choosing to become pregnant, and a substantial proportion of infected women give birth each year.2,3 The perinatal transmission of HIV both in Canada4,5,6 and around the world1,2,3,7 is a source of concern. In fact, the vast majority of all HIV infections in children are acquired perinatally.1,2,3,7 Thus, care of the mother and her offspring in the setting of HIV infection has become an important health care issue.
Canadian consensus guidelines for the treatment of HIV infection in adults have been published previously,8,9,10 but they contained only minimal information about the complexities of caring for HIV-positive pregnant women. In October 1998 a representative group of HIV and infectious disease specialists, obstetricians with interest and expertise in the care of HIV-positive pregnant women, family physicians, pediatric HIV specialists and community members convened to review recently published guidelines and their supporting scientific literature and to make recommendations. Information that became available after the 1998 workshop, either in published form or through presentation at conferences, was also considered before the guidelines were finalized. The guidelines therefore represent the current Canadian consensus on the care of HIV-positive pregnant women and their infants.
These consensus recommendations are summarized as a commentary on page 1671 of this issue.11 The full-length guidelines and the evidence supporting them can be accessed online at www.cmaj.ca. In this article we present 7 scenarios demonstrating how the recommendations are intended to be applied in practice.
Scenario 1
An HIV-infected pregnant woman who is not receiving antiretroviral therapy when pregnancy is confirmed
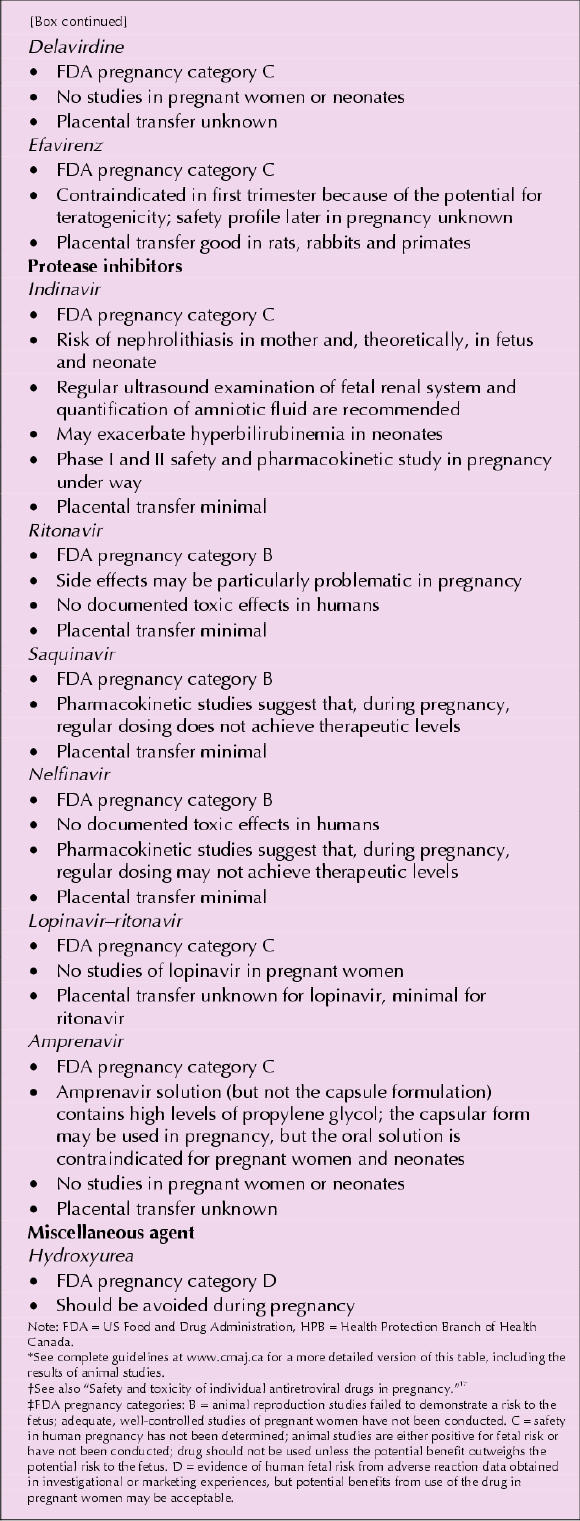
The woman's clinical, virologic and immunologic status should be assessed. Antiretroviral therapy should be offered, the regimen being carefully chosen on the basis of the principles outlined in the consensus guidelines.11 If the woman has never received antiretroviral therapy, then the regimen selected should include a protease inhibitor or a non-nucleoside reverse transcriptase inhibitor; trials comparing these 2 types of regimens are currently being planned and initiated. Most experts still recommend including zidovudine whenever possible, as it remains the best-studied perinatal prophylactic agent.12 If the woman has previously received antiretroviral therapy, resistance testing should be performed on viral isolates obtained during the prior antiretroviral therapy, if possible, and the results used to aid in the choice of regimen. Experts should be consulted in determining the best regimen. The available information regarding potential toxicities of individual antiretroviral agents in pregnancy is outlined in Box 1.
Box 1.
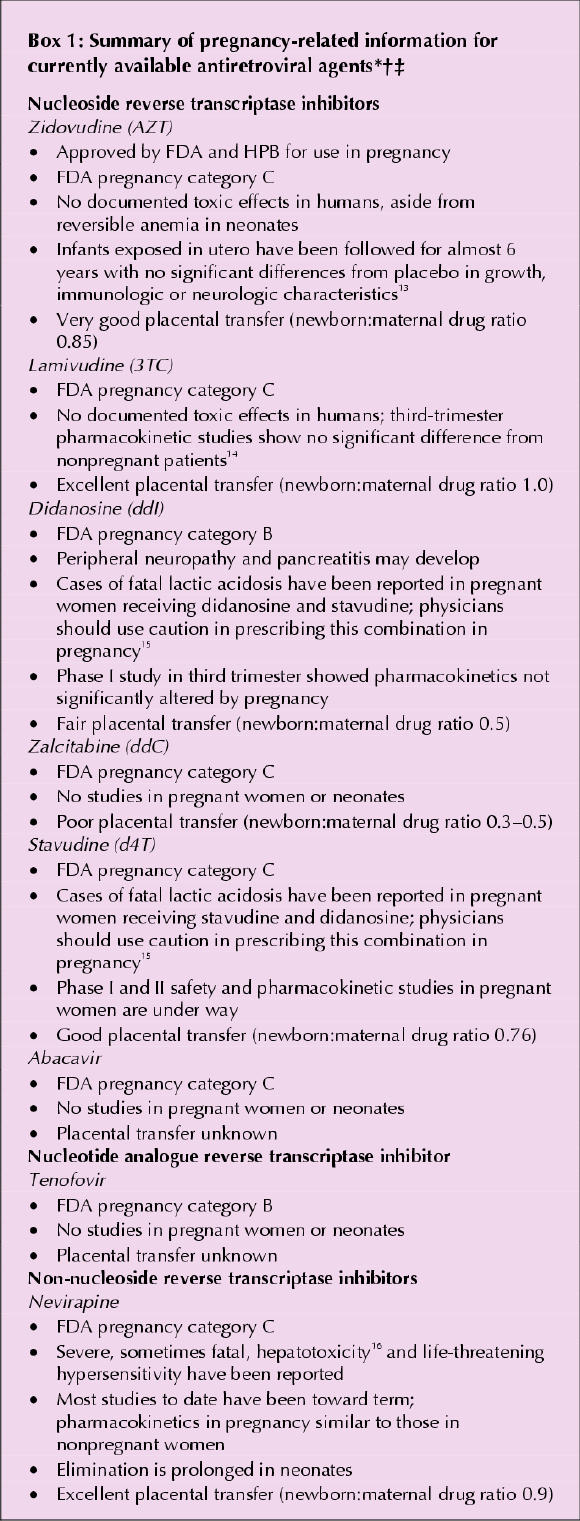
Box 1.
In most circumstances, initiation of antiretroviral therapy should be delayed until after the first trimester (and consideration should be given to awaiting the results of a detailed ultrasound assessment at 18 weeks' gestation), unless early initiation of therapy is judged important for maternal health. Delaying the initiation of antiretroviral therapy until after the first trimester minimizes the risk of drug-related teratogenicity and usually results in better adherence, as the nausea associated with pregnancy has usually diminished by this time. Adherence to antiretroviral therapy during pregnancy may be difficult, even in the second and third trimesters, and close monitoring for and management of side effects is important to maximize adherence.
The woman should be encouraged to continue oral antiretroviral therapy until as close to delivery as possible, and intravenous administration of zidovudine should be offered during labour, as outlined in the perinatal prophylaxis protocol (Box 2). In the postpartum period, the physician or another health care provider should discuss with the woman her need for ongoing antiretroviral therapy. If her immunologic characteristics are favourable, complete discontinuation of the therapy in the postpartum period and ongoing monitoring is a reasonable option. However, if it is considered appropriate for the woman's health, then antiretroviral therapy should be continued postpartum, and the woman should be followed and monitored according to usual adult HIV treatment guidelines.8,9,10
Box 2.
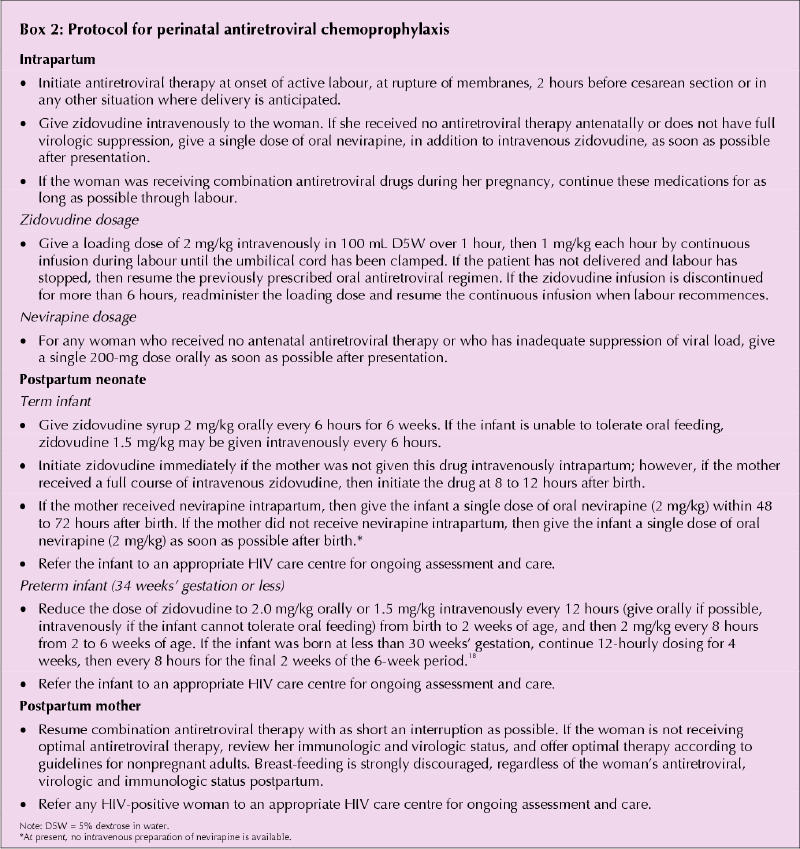
Any woman who declines combination antiretroviral therapy after appropriate counselling and education should be offered modified antiretroviral treatment for perinatal prophylaxis (see Box 2). A woman who chooses to take only prophylactic therapy to minimize exposure of her fetus to these drugs should be informed of the potential risk of resistance developing in the course of suboptimal antiretroviral therapy (e.g., zidovudine monotherapy), and she should be reassessed postpartum to determine the need for combination antiretroviral therapy. Discussion of treatment options and recommendations must be noncoercive, and the final decision regarding the use of these drugs is the woman's responsibility.
Scenario 2
An HIV-infected pregnant woman receiving combination antiretroviral therapy when pregnancy is confirmed
The woman's antiretroviral regimen should be reviewed in light of the pregnancy, both from the perspective of safety and toxicity and from the perspective of efficacy. Dosages should be reviewed to account for the increased volume of distribution in pregnancy. The potential need for antiemetics should be addressed, and doxylamine-pyridoxine with or without dimenhydrinate should be prescribed as required. If nausea and vomiting are significant problems, consideration should be given to discontinuing all antiretrovirals until the symptoms are controlled. If the existing combination therapy regimen is judged to be safe in pregnancy and is providing adequate viral suppression, the regimen should be continued. Antiretroviral combinations should be discontinued or changed if the regimen is thought to be potentially teratogenic or fetotoxic (e.g., if it contains efavirenz, delavirdine or hydroxyurea).
If the current regimen is not controlling viral replication, the physician should review the history of antiretroviral use and, if possible, perform resistance testing to aid in the choice of a new regimen. Drugs should be chosen on the basis of the principles outlined in the recommendations.11 Experts in the field should be consulted.
If the woman chooses to discontinue antiretroviral therapy during the first trimester, all drugs should be discontinued at the same time and then resumed at the same time, at 14 weeks' gestation (or as soon as possible after the detailed ultrasound examination at 18 weeks' gestation) to minimize the risk of viral resistance developing. Any woman who chooses to discontinue her combination antiretroviral therapy should be warned about the possibility of viral load rebound and the theoretical increased risk of perinatal transmission.
The woman should be encouraged to continue her combination antiretroviral regimen until as close to delivery as possible; in addition, she should be offered intrapartum zidovudine, administered intravenously, according to the perinatal prophylaxis protocol (Box 2). After the birth, the infant should be referred to a specialized centre for ongoing assessment and care.
The woman should be assessed in the postpartum period to determine the need for continuing antiretroviral therapy, contraceptive therapy, and other health care needs and issues, according to adult HIV care guidelines.8,9,10
Scenario 3
A woman diagnosed with HIV infection, who presents or is referred for care within 1 month of term
In this situation, it may not be possible to reliably suppress the plasma viral load before delivery (because of time constraints), and the following steps are recommended:
· The woman should be treated with combination antiretroviral therapy according to the principles outlined in the recommendations.11
· Elective cesarean section should be offered at 38 completed weeks of gestation.
· Oral antiretroviral therapy should be continued until 2 hours before the cesarean section (in consultation with anesthesia colleagues).
· Zidovudine should be administered intravenously starting 2 hours before the cesarean section, as outlined in the perinatal prophylaxis protocol (see Box 2). In addition, if the antepartum regimen did not contain nevirapine, a single oral dose of this drug should be considered.
· The infant should be given zidovudine (see Box 2).
Scenario 4
A woman who probably has detectable plasma viral load at term (because of suboptimal antiretroviral therapy during the pregnancy, problems with adherence or other drug-related issues, or lack of pregnancy care)
If labour has not commenced, the woman should be offered a cesarean section.
Several antiretroviral options are available, including intrapartum intravenous administration of zidovudine, followed by 6 weeks of zidovudine for the infant, combined with a single oral dose of nevirapine for the woman and a single oral dose of nevirapine for the infant. Although this approach has not been formally studied in a controlled clinical trial, it is currently favoured by the majority of Canadian experts.
Scenario 5
An infant born to a known HIV-positive mother who received no antiretroviral therapy during pregnancy or intrapartum
Oral administration of zidovudine and a single oral dose of nevirapine for the infant should be discussed with the mother; such therapy should start as soon as possible, preferably within 6 hours of birth, as efficacy after 96 hours is considered low.12 Details of antiretroviral prophylaxis for the infant are given in Box 2. The infant should be referred to a centre with specialized expertise for ongoing assessment and care.
The woman should be assessed postpartum (for viral load, CD4 count and other HIV markers), referred for ongoing HIV care and offered combination antiretroviral therapy according to the guidelines for adult HIV care.8,9,10
Scenario 6
A woman who experiences primary HIV infection (seroconversion) during pregnancy
Documented primary infection during pregnancy is an indication for combination antiretroviral therapy. Initiating such therapy is important not only for long-term maternal well-being but also for the prevention of perinatal transmission, since the risk of maternal-infant transmission in this situation is probably higher than among women who experience seroconversion before pregnancy. In the setting of documented seroconversion during pregnancy, the woman should be carefully counselled, in a noncoercive manner, regarding her reproductive choices, and she should be supported in her decisions. If the woman chooses to initiate combination antiretroviral therapy, it should be started as soon as possible, regardless of gestational age. If a woman with primary infection chooses to continue the pregnancy and refuses combination therapy, perinatal antiretroviral chemoprophylaxis should be offered, as outlined in Box 2.
Scenario 7
Use of perinatal prophylactic antiretroviral therapy in pregnant women presenting at delivery with significant risk factors but unknown HIV status
Many women who are at risk for HIV infection do not receive antenatal care and present late in their pregnancy or in early labour with unknown HIV status. Women at particular risk of HIV infection include those who use injection drugs and have shared needles, those who have had a recent illness suggestive of a seroconversion illness, and those who have had regular unprotected sex with a known HIV-infected partner or a partner with significant risk factors for HIV infection.
HIV testing should be offered to any woman who has not been tested during her pregnancy, and particularly to those recognized to be at risk for HIV infection. The test should be performed as rapidly as possible; with point-of-care test kits, the screening result should be available within 1 hour. Positive results must be verified by formal serologic testing, including HIV enzyme-linked immunosorbent assay and Western blot test. Rational decisions can then be made regarding the need for ongoing chemoprophylaxis for the infant, and appropriate care can be offered to the woman. Testing should always be done with the woman's knowledge and consent, and the woman must give her consent for any antiretroviral therapy.
A woman at high risk may be offered perinatal prophylaxis as outlined in scenario 4. The infant's zidovudine therapy should be continued until the HIV status of the mother is known. If the woman proves to be HIV negative and seroconversion is unlikely, the chemoprophylaxis for the infant can be discontinued. If the woman proves to be HIV positive, then a full course of zidovudine chemoprophylaxis should be offered to the infant, as outlined in Box 2. Both the infant and the woman should be referred to the nearest appropriate HIV care centre for ongoing assessment and care.
Conclusions
The care of HIV-positive pregnant women and their infants is complex. Ideally, such care should involve the woman herself, her HIV specialist, an HIV-experienced obstetrician and a pediatric HIV specialist. The assistance of a pharmacist and dietitian with HIV expertise is also invaluable. A wide variety of issues must be addressed, and close monitoring of the patient is essential. This area of medicine and science is evolving, and we anticipate that these guidelines will also evolve. Further clinical research is needed to ensure that the health outcomes of HIV-positive women and their infants will improve in the future.
β See related article page 1671
Footnotes
This article has been peer reviewed.
Contributors: David Burdge was chair of the working group; he wrote the first draft of the guidelines, edited and circulated subsequent drafts, and coordinated input from all other authors. Deborah Money provided extensive input into the guidelines from an obstetrician's perspective, did extensive editing and provided many valuable suggestions. She is a member of the Infectious Diseases Committee of the Society of Obstetricians and Gynecologists of Canada (SOGC) and facilitated that committee's review of the guidelines. John Forbes and Lindy Samson provided extensive input into the guidelines from a pediatric perspective, did extensive editing and provided many valuable suggestions. They are both members of the Canadian Pediatric AIDS Research Group and facilitated review of the guidelines by that group. Lindy Samson also critically reviewed the levels of evidence. Sharon Walmsley provided extensive input into the guidelines from an adult HIV perspective, did extensive editing and provided many valuable suggestions. Fiona Smaill provided extensive input into the guidelines, did extensive editing and provided many valuable suggestions, especially with respect to the levels of evidence. Marc Boucher provided extensive input into the guidelines. He chairs the Infectious Diseases Committee of the SOGC and facilitated the SOGC's review of the guidelines. Marc Steben was a member of the original Working Group and provided extensive editorial suggestions.
Acknowledgments: The guidelines on which this article is based were developed with support from the Canadian HIV Trials Network, which received unrestricted educational grants from Abbott Laboratories Limited, BioChem Pharma Inc., Boehringer Ingelheim (Canada) Ltd., Bristol-Myers Squibb, Glaxo Wellcome Inc., Hoffmann-La Roche Limited, Merck Frosst Canada Inc., and Pharmacia & Upjohn Inc., as well as funding from the National AIDS Strategy of Health Canada.
Competing interests: David Burdge, Deborah Money, John Forbes, Sharon Walmsley, Fiona Smaill and Marc Steben have all received speaker fees and/or educational grants from various pharmaceutical companies manufacturing drugs mentioned in this article. David Burdge, John Forbes, Sharon Walmsley, Fiona Smaill and Marc Steben have received travel assistance from various pharmaceutical companies to attend meetings within the past 2 years. Fiona Smaill has had ongoing paid consultancies with 3 pharmaceutical companies within the past 2 years. No competing interests declared for Marc Boucher or Lindy M. Samson.
Correspondence to: Dr. David R. Burdge, Oak Tree Clinic, B4 West Old Shaughnessy Building, Children's and Women's Health Centre of British Columbia, 4500 Oak St., Vancouver BC V6H 3N1; fax 604 875-3063; dburdge@cw.bc.ca
References
- 1.AIDS epidemic update—December 2002. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization; 2002. Report no.: UNAIDS/02.46E.
- 2.Panel members, International AIDS Society. IAS position paper on prevention of HIV 1 mother-to-child transmission. Int AIDS Soc Newsl 1999:(13):5-9. [PubMed]
- 3.Mother to child transmission of HIV: UNAIDS technical update. Revised. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 1998 Oct. UNAIDS Best Practice Collection Technical Update. Report no.: WC 503.71.
- 4.Birnun A, King SM, Arneson C, Read SE. Failure to prevent perinatal HIV infection. CMAJ 2002;166(7):904-5. [PMC free article] [PubMed]
- 5.Robinson JL, Lee BE. Prevention of perinatal transmission of HIV infection. CMAJ 2000;163(7);831-2. [PMC free article] [PubMed]
- 6.O'Connor KS, MacDonald SE. Aiming for zero: preventing mother-to-child transmission of HIV [editorial]. CMAJ 2002;166(7):909-10. [PMC free article] [PubMed]
- 7.Mother-to-child transmission (MTCT) of HIV. Questions and answers. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 1999 Aug 5. Background Briefs. Report no.: UNAIDS/99.40E.
- 8.Rachlis AR, Zarowny DP, for the Canadian HIV Trials Network Antiretroviral Working Group. Guidelines for antiretroviral therapy for HIV infection. CMAJ 1998;158(4):496-505. [PMC free article] [PubMed]
- 9.Carpenter CCJ, Cooper DA, Fischl MA, Gatell JM, Gazzard BG, Hammer SM, et al. Antiretroviral therapy in adults. Updated recommendations of the International AIDS Society—USA panel. JAMA 2000;283:381-90. [DOI] [PubMed]
- 10.US Department of Health and Human Services Panel on Clinical Practices for Treatment of HIV Infection. Guidelines for the use of antiretroviral agents in HIV-1 infected adults and adolescents. MMWR Morb Mortal Wkly Rep 1998;47(RR-5):42-82. [PubMed]
- 11.Burdge DR, Money DM, Forbes JC, Walmsley SL, Smaill FM, Boucher M, et al. Canadian consensus guidelines for the management of pregnancy, labour and delivery and for postpartum care in HIV-positive pregnant women and their offspring (summary of 2002 guidelines) [editorial]. CMAJ 2003;168(13):1671-74. [PMC free article] [PubMed]
- 12.Public Health Service Task Force recommendations for use of antiretroviral drugs in pregnant women infected with HIV-1 for maternal health and for reducing perinatal HIV-1 transmission in the United States. Rockville (MD): US Department of Health and Human Services; 2002 Feb 4. Available: www.hivatis.org/trtgdlas.html#perinatal (accessed 2002 Feb 22).
- 13.Sperling RS, Shapiro DE, McSherry GD, Britto P, Cunningham BE, Culnane M, et al. Safety of the maternal–infant zidovudine regimen utilized in the Pediatric AIDS Clinical Trial Group 076 Study. AIDS 1998;12:1805-13. [DOI] [PubMed]
- 14.Moodley J, Moodley D, Pillay K, Coovadia H, Saba J, van Leeuwen R, et al. Pharmacokinetics and antiretroviral activity of lamivudine alone or when coadministered with zidovudine in human immunodeficiency virus type 1-Infected pregnant women and their off-spring. J Infect Dis 1998;178:1327-33. [DOI] [PubMed]
- 15.Smyth AC. Important drug warning [letter]. [place unknown]: Bristol-Myers Squibb Company; 2001 Jan 05. Available: www.fda.gov/medwatch/SAFETY/2001/Zerit&Videx_letter.htm (accessed 2003 May 28). Report of fatal lactic acidosis in 3 pregnant women treated with stavudine and didanosine.
- 16.Martinez E, Blanco JL, Arnaiz JA, Perez-Cuevas JB, Mocroft A, Cruceta A, et al. Hepatotoxicity in HIV-1-infected patients receiving nevirapine-containing antiretroviral therapy. AIDS 2001;15:1261-8 [DOI] [PubMed]
- 17.Safety and toxicity of individual antiretroviral agents in pregnancy: nucleoside and nucleotide analogue reverse transcriptase inhibitors. Supplement to: Public Health Service Task Force recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV-1 transmission in the United States. Rockville (MD): US Department of Health and Human Services; 2003 May 23. Available: www.aidsinfo.nih.gov/guidelines/perinatal/ST_052303.pdf (accessed 2003 May 28).
- 18.Capparelli EV, Mirochnick M, Dankner WM, Blanchard S, Mofenson L, McSherry GD, et al. Pharmacokinetics and tolerance of zidovudine in preterm infants. J Pediatr 2003;142:47-52. [DOI] [PubMed]


