Abstract
Objective
To determine the prevalence of the side effects of lithium therapy and possible predictors of hypothyroidism in women and men with bipolar disorder.
Method
Twenty-two men and 38 women with bipolar disorder and taking lithium for at least 1 year, were interviewed about lithium side effects using a list of the most commonly reported symptoms.
Results
The complaint most frequently reported was polyuria–polydipsia syndrome, which affected 36 (60%) of 60 patients. More men than women reported tremor (54% v. 26%, p < 0.05), but weight gain during the first year of treatment was more frequent in women than men (47% v. 18%, p < 0.05), as was the development of clinical hypothyroidism (37% v. 9%, p < 0.05). Weight gain during the first year of treatment (and not sex) was the only significant predictor of hypothyroidism.
Conclusion
Weight gain during the first year of lithium treatment, in the absence of biological evidence of subclinical hypothyroidism, was the most predictive and, possibly, the first sign of hypothyroidism.
Medical subject headings: bipolar disorder, drug toxicity, hypothyroidism, lithium carbonate, sex factors, weight gain
Abstract
Objectif
Déterminer la prévalence des effets secondaires de la thérapie au lithium et les prédicteurs possibles d'hypothyroïdie chez les femmes et les hommes atteints de trouble bipolaire.
Méthode
On a interviewé 22 hommes et 38 femmes atteints de trouble bipolaire et prenant du lithium depuis au moins un an au sujet des effets secondaires du lithium, en utilisant une liste des symptômes les plus couramment déclarés.
Résultats
Le syndrome de polyurie–polydipsie, qui a atteint 36 (60 %) des 60 patients, a constitué la plainte la plus courante. Plus d'hommes que de femmes ont signalé des tremblements (54 % c. 26 %, p < 0,05), mais la prise de poids au cours de la première année du traitement a été plus fréquente chez les femmes que chez les hommes (47 % c. 18 %, p < 0,05), tout comme l'apparition de l'hypothyroïdie clinique (37 % c. 9 %, p < 0,05). La prise de poids au cours de la première année du traitement (et non le sexe) a été la seule variable significative pour la prédiction de l'hypothyroïdie.
Conclusion
La prise de poids au cours de la première année de traitement au lithium, en l'absence de preuves biologiques d'hypothyroïdie sous-clinique, a été le signe le plus prédicteur d'hypothyroïdie et, possiblement, le premier signe d'hypothyroïdie.
Introduction
Lithium, a mainstay in the treatment of bipolar disorder, has been reported to induce adverse effects in 35%–93% of patients who take it,1 and these adverse events often lead to noncompliance.2 To optimize lithium treatment, it is therefore important to be aware of these effects. The “antithyroid” effect of lithium is one of the most common side effects,3,4 but little is known of the factors that predispose patients to develop hypothyroidism during treatment. A recent study showed that the main risk factor was being female (prevalence of 14% in women v. 4.5% in men).5 Women also seemed to be at highest risk during the first 2 years of lithium treatment, and the prevalence was highest for women starting treatment over the age of 50 years.6 Another study showed that patients with first-degree relatives affected by thyroid disease experienced an earlier onset of lithium-induced hypothyroidism.7 It has been suggested that even mild thyroid dysfunction may be associated with impaired cognition, mood and response to psychotropic medication; it is therefore important to define subjects at high risk for developing hypothyroidism so that they can be followed with particular attention.8,9,10
With the exception of hypothyroidism, differences between the sexes in lithium side effects have not been systematically studied. Thus, the purpose of this study was to assess the side effects of lithium treatment as a function of sex and to identify factors that are predictive of developing hypothyroidism.
Methods
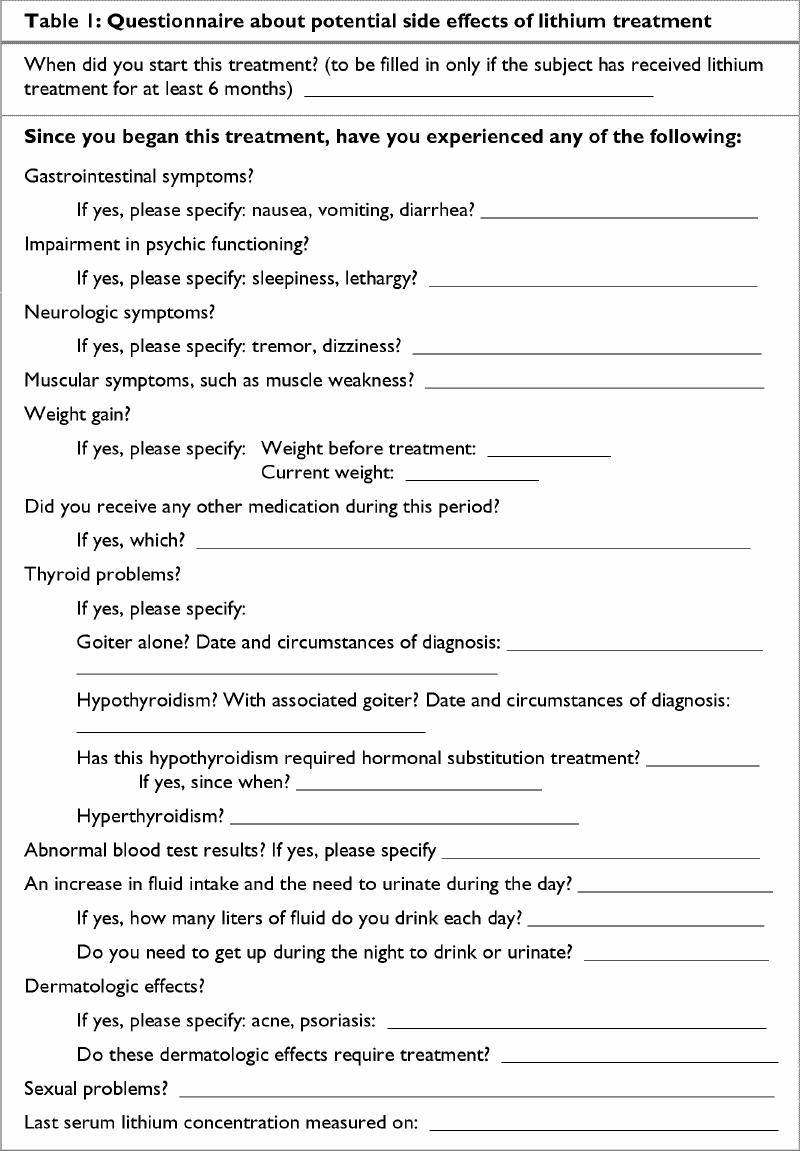
The study population consisted of 22 men and 38 women outpatients with bipolar disorder, type I. All patients provided informed written consent for participation. Patients were screened for diagnosis using the French version of the “Diagnosis Interview for Genetic Studies,” a clinical interview constructed for the assessment of major mood and psychotic disorders and their spectrum conditions.11 We then used a list of the 15 symptoms most frequently reported in the literature2,12 and the Vidal dictionary13 (used by most practitioners in France) to interview patients who had been taking lithium for at least 1 year about side effects they had experienced (Table 1).
Table 1
The clinical severity and biochemical abnormalities associated with hypothyroidism vary greatly. We therefore took into account only overt hypothyroidism for which patients were taking thyroid supplementation.
Chi-square tests were used to assess differences between men and women in terms of side effects. If the sample size was too small to perform the chi-square test, a p value for Fisher's exact test was calculated. However, only those groups of a size appropriate for statistical analysis were compared. To investigate the relation between hypothyroidism and risk factors, a linear regression was performed with age, sex, duration of treatment and weight gain as putative predictive factors.
Results
The mean age of the 22 men (36.7%) and 38 women (63.3%) with bipolar disorder, type I, was 41.3 (standard deviation [SD] 12.8, range 19–75) years. At the time of the interview, the mean duration of lithium treatment was 6.9 (SD 6.5, range 1–26) years, and mean blood lithium concentration was 0.74 (SD 0.11, range 0.6–1) mmol/L. Lithium treatment improved the symptoms in all patients; only 8 received other concomitant medication.
The complaint most frequently reported in the side-effects interview was polyuria–polydipsia syndrome, which affected 36 (60%) of 60 patients (Table 2). It is difficult to assess increases in fluid intake accurately without a 24-hour urine volume measurement, but we asked patients if they needed to get up during the night to drink, urinate or both, and 36 (60%) of the 60 patients said they had to since beginning lithium treatment. However, creatinine levels of these patients were in the normal range.
Table 2
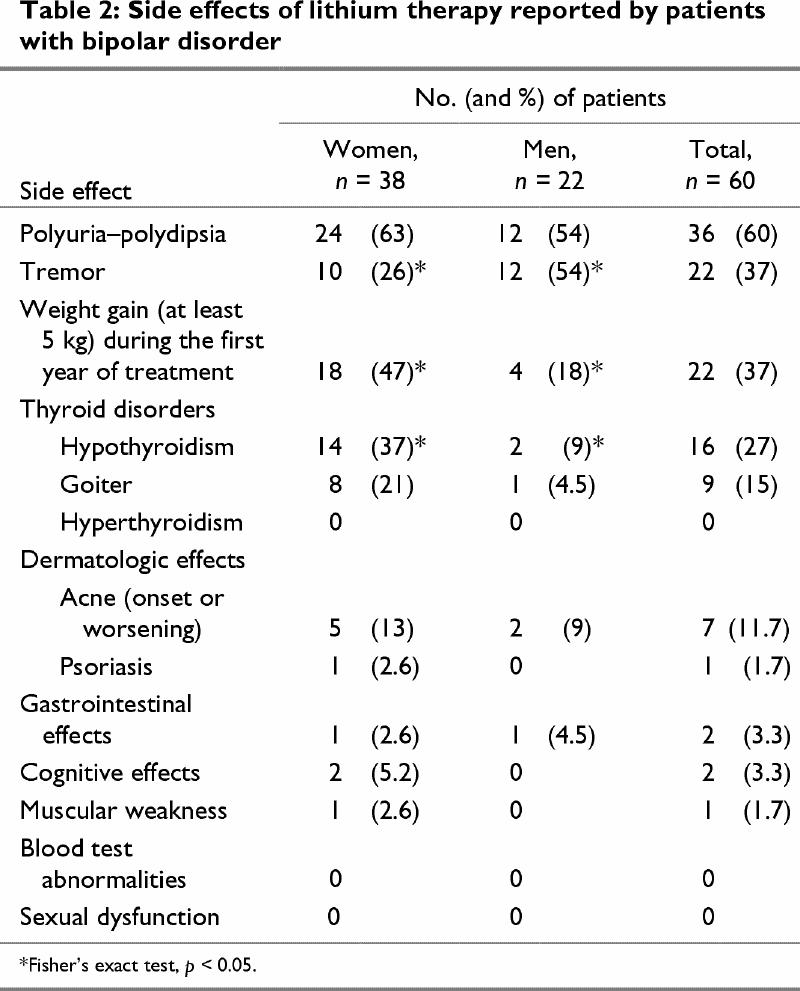
Hypothyroidism (for which thyroid supplementation was required) was observed in 16 (27%) of the 60 patients, and 9 of these had a goiter. The mean time between the start of lithium treatment and diagnosis of thyroid dysfunction was 7 (SD 4.53, range 1–14) years.
Men presented tremor more frequently than did women (54% v. 26%, p < 0.05), but weight gain was more frequent in women than in men (47% v. 18%, p < 0.05) as was hypothyroidism (37% v. 9%, p < 0.05). Dermatological effects also were more frequent in women (16% v. 9%), but this difference was not statistically significant.
We carried out a linear regression with hypothyroidism as the dependent variable and age, sex, duration of treatment and weight gain as independent variables. The only independent variable that was significant for predicting hypothyroidism was weight gain (> 5 kg) in the first year of treatment (β = 0.38, t = 2.7, p < 0.01), and there was a trend for age (β = 0.008, t = 1.7, p < 0.09).
Discussion
In this study, the side effects of lithium differed between men and women; men were more likely to experience tremor, whereas women were more likely to gain weight and develop clinical hypothyroidism. Moreover, the factor most predictive of hypothyroidism was weight gain during the first year of treatment (weight gain was not due to subclinical hypothyroidism).
As reported by others,14 our patients frequently experienced polyuria–polydipsia syndrome. In addition, there were more dermatological effects reported by women than men; although not statistically significant, this result is consistent with the findings of Sarantidis and Waters.15
We observed overt hypothyroidism in 27% of the patients in our sample. This is higher than the 8% to 20% reported in other studies.12,16 There may be several reasons for this. First, definitions of clinical and subclinical hypothyroidism may differ between studies. Indeed, hypothyroidism is a graded phenomenon with various degrees of clinical severity and biochemical abnormalities. Patients with overt hypothyroidism have abnormally low free thyroxin levels and high concentrations of thyroid stimulating hormone. In addition, overt hypothyroidism is usually, but not always, associated with symptoms.12 In our sample, we considered only those patients who required thyroid supplementation as having overt hypothyroidism. The hormone substitute was prescribed by another physician, independent of the psychiatrist.
Another possible explanation for the high incidence of hypothyroidism in our group, is the well-established observation that the rate of thyroid dysfunction is high in the southwest of France, particularly in the Pyrenees area where some of our patients lived.
Transbol et al17 suggested that the risk of developing lithium-induced hypothyroidism increases with the duration of treatment. The mean duration of lithium treatment for our sample was relatively long, at 6.9 years. However, in this study, the duration of treatment was not associated with an increase in the risk of developing hypothyroidism.
We investigated weight gain during the first year of treatment only because weight generally increases with age and because rapid weight gain is a symptom of hypothyroidism. People who rapidly gained weight at the beginning of lithium treatment seemed to have a higher risk of developing hypothyroidism.
Although more women than men developed hypothyroidism in our sample , the factor most predictive of hypothyroidism was not sex, but weight gain. This is the first study to consider this parameter as a predictor of hypothyroidism and suggests that psychiatrists should monitor body weight changes during treatment and consider thyroid dysfunction as a possible side effect of lithium if a patient starts to gain weight during treatment.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. Chantal Henry, Service Universitaire de Psychiatrie, CH Charles Perrens, 121 rue de la Béchade, 33076 Bordeaux, France; fax: 33 5 56 56 35 41; chantal.henry@bordeaux.inserm.fr
Submitted Jan. 18, 2001 Revised Jun. 6, 2001, Nov. 9, 2001 Accepted Nov. 21, 2001
References
- 1.Lenox RH, Manji H. Lithium. In: Schatzberg AF, Nemerff CB, editors. American psychiatric press textbook of psychopharmacology. 2nd ed. Washington: American Psychiatric Press; 1998. p. 379-429.
- 2.Dunner DL. Optimizing lithium treatment. J Clin Psychiatry 2000;61(9):76-81. [PubMed]
- 3.Amisden A, Jensen SE, Glsen, Schou M. Development of goiter during lithium treatment [in Danish]. Ugeskr Laeger 1968;130: 1515-8. [PubMed]
- 4.Amdisen A, Andersen CJ. Lithium treatment and thyroid function. A survey of 237 patients with long-term lithium treatment. Pharmacopsychiatria 1982;15(5):149-55. [DOI] [PubMed]
- 5.Johnston AM, Eagles JM. Lithium-associated clinical hypothyroidism. Prevalence and risk factors. Br J Psychiatry 1999;113:336-9. [DOI] [PubMed]
- 6.Kirov G. Thyroid disorders in lithium-treated patients. J Affect Disord 1998;50(1):33-40. [DOI] [PubMed]
- 7.Kusalic M, Engelsmann F. Effect of lithium maintenance therapy on thyroid and parathyroid function. J Psychiatry Neurosci 1999;24(3):227-33. [PMC free article] [PubMed]
- 8.Cowdry R, Wehr T, Zis A, Goodwin FK. Thyroid abnormalities associated with rapid cycling bipolar illness. Arch Gen Psychiatry 1983;40:414-20. [DOI] [PubMed]
- 9.Joffe R, Kutcheer S, MacDonald C. Thyroid function and bipolar affective disorder. Psychiatry Res 1988;21:117-21. [DOI] [PubMed]
- 10.Haggerty JJ, Stern RA, Masson GA, Beckwith J, Morey CE, Prange AJ Jr. Subclinical hypothyroidism: a modifiable risk factor for depression? Am J Psychiatry 1993;150:508-10. [DOI] [PubMed]
- 11.Nurnberger JI, Blehar MC, Kaufman CA, York-Cooler C, Simpson SG, Harkavy-Freedman J, et al. Diagnostic interview for genetic studies. Arch Gen Psychiatry 1994;51:849-64. [DOI] [PubMed]
- 12.Kleiner J, Altshuler L, Hendrick V, Hershman JM. Lithium-induced subclinical hypothyroidism: review of the literature and guidelines for treatment. J Clin Psychiatry 1999;60(4):249-55. [PubMed]
- 13.Vidal le Dictionnaire. Paris: Ed. du Vidal; 2000.
- 14.Vestergaard P, Thomsen K. Renal side effects of lithium: the importance of the serum lithium level. Psychopharmacalogy (Berl) 1981;72(2):203-4. [DOI] [PubMed]
- 15.Sarantidis D, Waters B. A review and controlled study of cutaneous conditions associated with lithium carbonate. Br J Psychiatry 1983;143:42-50. [DOI] [PubMed]
- 16.Lindstedt G, Nilsson LA, Walinder J, Skott A, Ohman R. On the prevalence, diagnosis and management of lithium-induced hypothyroidism in psychiatric patients. Br J Psychiatry 1977; 130: 452-8. [DOI] [PubMed]
- 17.Transbol I, Christiansen C, Baastrup PC. Endocrine effects of lithium: hypothyroidism, its prevalence in long-term treated patients. Acta Endocrinol 1978;87:759-67. [PubMed]


