Abstract
A more complete understanding of the psychosocial and clinical predictors of response to pharmacotherapy would be of great value to both patients and physicians. Most demographic and clinical factors have not been found to be useful predictors of response. Although comorbid illness affects quality of life, there is confounding evidence about its importance when predicting response to antidepressant therapy. Some social support factors appear to be positive predictors of outcome in most trials. There is evidence to suggest that comorbid anxiety disorders and panic–agoraphobic spectrum symptoms are negative predictors of response to treatment. Substance abuse has been associated with a poorer response to antidepressant therapy, and recovery from substance abuse problems has been shown to be poorer among patients with comorbid depression. Assessment of personality dimensions may be a useful predictor of clinical course and outcome, but personality disorders present a complicated picture, with significant interaction among variables. A number of variables are significantly related to clinical course, but few factors have been clearly linked to treatment response. The challenge is to determine if any of these factors are indeed independent predictors of response and whether it is possible to match choice of antidepressant therapy and patient type.
Medical subject headings: antidepressive agents; behavioral symptoms; comorbidity; depressive disorder; drug therapy; psychiatric status rating scales; risk factors; psychology, social; recurrence; remission induction; treatment outcome.
Abstract
Il serait très utile tant pour les patients que pour les médecins de comprendre entièrement les prédicteurs psychosociaux et cliniques de la réponse à la pharmacothérapie. La plupart des facteurs démographiques et cliniques ne sont pas des prédicteurs utiles de réponse. Même si une comorbidité a des répercussions sur la qualité de vie, il existe des données confusionnelles sur son importance lorsque l'on prédit la réponse à une thérapie aux antidépresseurs. On a constaté que certains facteurs d'appui social sont des prédicteurs positifs des résultats dans le cadre de la plupart des études. Tout semple indiquer que les troubles comorbides de l'anxiété ou les symptômes de la gamme panique-agoraphobie sont des prédicteurs négatifs de réponse au traitement. On a établi un lien entre la toxicomanie et une moins bonne réponse à la thérapie aux antidépresseurs, et l'on a démontré que le rétablissement à la suite d'une toxicomanie est moins bon chez les patients atteints d'une dépression comorbide. L'évaluation des aspects de la personnalité peut constituer un prédicteur utile de l'évolution et du résultat clinique, mais les troubles de la personnalité présentent un tableau compliqué où l'interaction entre les variables est importante. De nombreuses variables ont un lien important avec les résultats, mais les facteurs reliés clairement à la réponse au traitement sont peu nombreux. Le défi consiste à déterminer si certains de ces facteurs sont vraiment des prédicteurs indépendants de réponse et s'il est possible de jumeler le choix de la thérapie aux antidépresseurs et le type de patient.
Introduction
Despite the introduction of a variety of antidepressant medications over the past 10–15 years, an unfavourable response to pharmacological intervention in the treatment of depression is not uncommon. As a result, there have been many attempts to determine the characteristics of depressed patients who will or will not respond to treatment. Both sociodemographic and clinical factors have been examined, but the potential predictors of nonresponse are most often inconsistent or not strong enough to be useful clinically. More often, antidepressants are chosen on the basis of side-effect profile an not the predicted efficacy for individual patients or patient groups.1 The ability to select the most successful treatment and to predict the outcome of therapy for a patient would be of great value to both patients and physicians.2 The purpose of this paper is to systematically review the association between treatment outcome and a number of psychosocial variables as identified in the published literature. Articles were retrieved using MEDLINE searches, and further key references were then identified from the initial review papers.
Demographic and clinical factors
Demographics
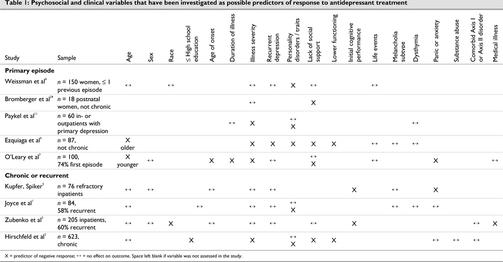
Most demographic factors have not been found to be useful predictors of response to antidepressant therapy. With few exceptions, age and sex do not affect response rates (Table 1).1,2,3,4,5 In the 2 studies that did show an age–response relation, one reported a poorer response in older subjects6 and the other, a poorer response in younger subjects.7 It has also been suggested that antidepressants are less effective in children and adolescents.8,9 This idea is based mainly on earlier small studies using tricyclic antidepressants (TCAs). More recent placebo-controlled trials with selective serotonin reuptake inhibitors (SSRIs), fluoxetine and paroxetine have demonstrated significant efficacy in this patient population.9,10 Race or ethnicity does not appear to be associated with treatment response either.4 In one study, a better than average treatment response reported for a subgroup of African–Americans was determined to be associated with less aggressive pretreatment of the index episode, which resulted in fewer treatment-resistant cases in this patient population.3
Table 1
Clinical factors
Duration of illness, number of prior episodes and age of onset do not appear to be predictors of response.1,3,4,5,7,11
Severity of illness may predict response in patients with primary depressive episodes,6,7,11 but not in patients with recurrent depression.1,3,5,12 However, in a study by Hirschfeld and colleagues,2 of 623 patients with chronic major or double depression, those who responded to antidepressant therapy had significantly lower baseline depression severity scores as measured by the Montgomery–Asberg Depression Rating Scale (MADRS) than nonresponders; however, the Hamilton Rating Scale for Depression (HAM-D) scores did not differ between responders and nonresponders.2
Age of onset of depression may be an important source of heterogeneity in both chronic and nonchronic mood disorders. In a study examining this variable as a potential predictor of response in 289 outpatients, early-onset chronic major depression had a more malignant course and was associated with more comorbid disorders than late-onset chronic major depression.13 However, the early–late onset distinction was not associated with differences in symptom severity, functional impairment or treatment response. This supports several other studies that also reported no impact of age of onset on response to therapy.1,3,5,12
Greater degree of cognitive impairment (as measured by the KDS Self-rating Scale or the Mini-Mental State Examination) at admission was an independent predictor of nonresponse to therapy in middle-aged and elderly inpatients with major depression.3,5
Results indicate that an early nonresponse to medication (i.e., 1–2 wk) may predict a poor outcome overall.14 No response to fluoxetine as early as week 2 of therapy predicted a negative outcome at 8 weeks.15 Moreover, the opposite was found to be true — of those patients who experienced a robust improvement by weeks 2 or 4, 80%–90% went on respond well, suggesting that responsiveness can at least be determined relatively quickly. Similar results have been also been demonstrated with TCAs.16
Comorbid physical illness
In elderly patients in community, outpatient and inpatient samples, physical illness emerges consistently as the most common clinical feature associated with depressive symptoms and diagnosis.17,18,19 In addition, some studies indicate that physical illness is associated with a poor prognosis for depression.20,21 However, in a study assessing the impact of comorbid illness on functional status and treatment outcome in 671 older depressed outpatients, Small et al22 found those with chronic physical illness responded to antidepressants as well as those without such illness. Interestingly though, the burden of prior (historical) physical illness was associated with a greater fluoxetine response and a lower placebo response. In contrast, another study of 205 consecutively admitted elderly inpatients with major depression demonstrated that the number of medical problems and length of hospital stay independently contributed to the prediction of response to treatment.3
Social support
Some researchers have suggested that social support has an important impact on recovery from depression.2,6,23 For example, elderly patients who were impaired in social interaction and subjective social support at baseline were less likely to recover from their depressive episode.23 Living with a spouse or partner, longer duration of personal relationships, higher educational level and higher quality of life have been found to be significant predictors of positive response.2 Other studies have also found that lack of everyday psychological support provided by a spouse was associated with incomplete recovery.6 In a sample of 18 married mothers who underwent 12-week antidepressant treatment for major depressive disorder, high disaffection toward their husband was a predictor of incomplete recovery, independent of symptom severity.24
A naturalistic study of 100 inpatients found that a longer time to remission was associated with not owning a house, residing in an urban residence and single marital status.7 None of these variables were significant predictors in the multivariate analysis, however. Several other studies have failed to find a relation between response to antidepressant therapy and social factors such as social class, marital status, widowhood or prior residential setting.3,4
Religion
There has been increasing interest in the effects of religious belief and activity on mental health and depression.25 Despite evidence suggesting its potential importance, the effects of religion on recovery from depression have been largely ignored.26 Studies show a significant inverse relation between religiosity and depression.27,28,29 In a study of 87 depressed elderly patients, which controlled for many potential predictors of outcome, greater intrinsic religiosity independently predicted shorter time to remission.30 This was not attributable to the social aspects of organized religious functions and church going, as these activities were not associated with time to remission. Less than half of the patients in this study received antidepressants or psychotherapy.
Predicting remission versus predicting response
Many studies chose either remission or response as endpoints. The few that have examined both have found that, in general, the predictors of remission and those of response are similar. In a study assessing the factors associated with full remission (defined as HAM-D < 8), response and nonresponse, the univariate analysis indicated that greater age was a significant predictor of remission but not of response, and initial higher HAM-D score was a negative predictor of response but not of recovery.6 In the multivariate analysis, initial functioning and partner social support were predictors of remission, initial HAM-D was predictive of response and personality disorders were associated with both response and remission. In another study, significantly lower levels of self-rated cognitive disorganization, depression and anxiety were seen in the complete responders (HAM-D ≤ 12) than in the partial (HAM-D 13–19) or nonresponders.5 In elderly patients, predictors of remission were found to be the same when the HAM-D cutoff was 10 or less and when it was below 7.3 Although there appear to be some variations, insufficient data are available to draw conclusions about whether various factors have different predictive value for remission or response.
Comorbid DSM-IV Axis I conditions
Anxiety disorders
Converging evidence indicates that patients with major depression and comorbid anxiety disorders experience less favourable treatment outcomes than patients who have major depression alone.31,32,33,34,35,36,37,38,39 There are relatively few studies in which the existence of a comorbid anxiety disorder was not predictive of nonresponse.1,2
In a recent study, a lifetime burden of panic–agoraphobic spectrum symptoms (including core and severe symptoms and more subtle features related to the core condition) predicted a poorer response to interpersonal psychotherapy (IPT) and an 8-week delay in response to sequential treatment (adding an SSRI to IPT) among 61 women with recurrent depression.40 Even after controlling for lifetime panic history, patients with high panic scores differed significantly in treatment outcome for depressive symptoms than those with low scores. In another study of 312 patients fulfilling criteria for treatment-resistant depression, response to treatment with venlafaxine was significantly higher in patients with an absence (58%) compared with the presence (31%) of any comorbid psychiatric disorder (p < 0.001).41
Substance abuse
An estimated 14% of the general population in the United States have a history of alcohol abuse or dependence, and alcoholism exists as a comorbid diagnosis in 20% of depressed men and 10% of depressed women.42,43 The prevalence of smoking is also higher among patients with depression than it is in normal control groups (49% v. 30%).44 “Self-medication,” both with legal and illegal drugs of various kinds, is common among depressed patients.44,45,46
Consumption of alcohol has been shown to be a predictor of poorer response to antidepressant therapy even in those who are not considered to be abusers (i.e., avg. intake < 30 mL [1 oz] per day).47 The degree of alcohol consumption at baseline was a significant predictor of poorer response in 94 patients treated with fluoxetine, even after adjusting for severity of depression at baseline. Patients with depression secondary to anxiety and substance abuse were less improved after treatment and more likely to have suicidal thoughts and relapses than patients with comorbid medical but not psychiatric conditions.48 Other studies, however, have found that a comorbid Axis I diagnoses, including substance abuse, does not influence antidepressant response rates.2,3
The alternative — recovery from comorbid conditions in patients with depression — has also been shown to be poorer. For example, recovery from substance abuse was poorer when patients had comorbid anxiety or depressive disorders.49 Comorbid patients had comparable substance abuse outcomes but fared worse on psychological symptoms and employment outcomes. Similarly, recovery from bulimia nervosa was poorer when there was comorbidity with depression.50
Comorbid DSM-IV Axis II disorders and personality dimensions
There has long been interest in the connection between personality and depression. The presence of a DSM-IV Axis II personality disorder has been linked to increased severity of depression and a poorer response to pharmacotherapy.6,11,51,52 Nevertheless, studies in which Axis II personality disorders have been specifically recorded do not consistently show a link.51,53,54 Personality traits, or specific dimensions of personality, appear to be more important predictors of outcome in patients with major depressive disorder.1,54,55
In a study designed to examine predictors of short-term response, Joyce and colleagues1 reported that personality traits, rather than clinical variables or Axis II personality disorder diagnoses, were the main predictors of response to TCAs. Eighty-four patients with a current major depressive episode completed a 6-week double-blind trial of either clomipramine or desipramine. No specific personality disorder diagnosis was predictive, but borderline personality did show a trend toward poorer treatment outcome (p = 0.09). The personality dimensions neuroticism, psychoticism and extraversion also did not predict outcome. Three temperament types in Cloninger's biosocial model of personality — novelty seeking, harm avoidance and reward dependence — accounted for 35% of the variance in treatment outcome, compared with less than 5% predicted by clinical variables. In the more severely depressed patients, these temperaments predicted nearly 50% of the variance in treatment outcome. Schizoid, passive–aggressive and passive–dependent personalities were associated with better outcomes, whereas antisocial and cyclothymic personalities fared poorly.
Hirschfeld et al2 reported that, in patients with chronic or double depression, the presence of a concurrent personality disorder did not predict response to medication. When specific diagnoses were examined, an Axis II passive–aggressive personality disorder was found to be significantly associated with a favorable response to 12 weeks of acute-phase treatment. Although the measurement of overall “depressive temperament” (as determined by the Diagnostic Interview for Depressive Personality) was not predictive of nonresponse to pharmacotherapy, certain characteristics of depressive personality, specifically low self-esteem, introversion and quietness, were.
In Paykel's landmark paper on residual symptoms after partial remission of depression, patients with residual symptoms had higher rates of personality abnormalities.11 Passive–dependent, but not schizoid, sociopathic or anankastic personality traits were associated with a poorer response.
Similarly, in a study in 83 depressed outpatients treated with fluoxetine for 8 weeks, there were no differences in outcome between patients who had and did not have a comorbid personality disorder diagnosis at baseline (as assessed with a self-rating score on the Personality Diagnostic Questionnaire-Revised).52 However, when diagnoses were grouped into clusters, the presence of a pretreatment cluster B diagnosis (i.e., histrionic, narcissistic, borderline and antisocial diagnosis) was predictive of a better response to antidepressant treatment than the absence of pretreatment cluster B diagnosis. No differences in response were apparent in patients with or without Cluster A (i.e., paranoid, schizoid, schizotypal) or Cluster C (i.e., avoidant, dependent, obsessive–compulsive, passive–aggressive) diagnoses.
In another prospective study specifically designed to identify predictors of recovery, the presence of Axis II personality disorder was the strongest predictor of poor outcome.6 Having suffered a previous episode, lower level of functioning and some aspects of social support were also associated with not achieving full remission. Only personality disorder and high initial HAM-D score were related to nonresponse. This study also examined self-esteem; a poorer response was observed in patients with a high negative evaluation of self.
Two other studies have also looked at the personality dimensions neuroticism and extraversion. In one study,4 neuroticism but not extraversion was an important predictor of chronic poor outcome with both psychotherapy and drug treatment. In contrast, the other study reported that neuroticism may be a predisposing factor for major depression but was not a predictor of response when severity of illness was considered.56 Moreover, extraversion was the best predictor of treatment outcome, with the gregariousness facet accounting for the reduction in depressive symptoms.
Several other studies have reported on the effects of specific personality traits on response to treatment. A better response has been shown in low angry-hostile, than in high angry-hostile depressive patients.57 In addition, distraction but not rumination was demonstrated to predict response.58 Rector et al59 reported that neither pretreatment self-criticism nor dependency scores were predictors of response to pharmacotherapy, but self-criticism scores were predictive of response to cognitive therapy.59
These findings demonstrate that personality assessment may be useful to help predict the clinical course and outcome of treatment for depressed patients. Dimensions of personality may prove to be more helpful than formal personality disorder diagnoses, but, at present, this idea requires further study.
Antidepressant therapy and personality
Some of the variability in the results of studies assessing personality may be related to the specific medication patients were taking. In women, temperament type predicted a variable response to different tricyclic antidepressants, with high reward dependence associated with a good response to clomipramine, and high harm avoidance associated with a good response to desipramine.1 This phenomenon was not observed in the men.
Some researchers have suggested that different antidepressant agents may have different effects on particular personality disorders or traits. One trial showed a reduction in anger attacks with fluoxetine treatment and suggested that patients with depression and anger attacks may respond better to SSRIs.60 In a study testing this hypothesis, in which 2 SSRIs, sertraline and paroxetine, as well as a tricyclic and a serotonin and norepinephrine reuptake inhibitor were used, there was no likelihood that high angry-hostile patients would respond better to SSRIs than to the other classes of medications.57 A comparison of the effectiveness of sertraline and citalopram in depressed patients with comorbid personality disorders showed equal reductions in paranoid, borderline, avoidant and dependent personality disorder diagnoses.61 Note, however, that both of these medications are SSRIs.
Conclusion
Despite finding a number of variables that were significantly related to outcome, few have been clearly linked to treatment response at this time.2 Clinical and sociodemographic variables are not particularly helpful, with age, sex, age of onset, duration of illness and number of recurrences having no effect on response to treatment. Severity of illness may predict response in patients with first-onset depression. Social support has been shown to be a predictor, particularly living with a spouse or partner, as has religiosity. Concurrent medical illness, although it appears to negatively affect quality of life, does not appear to be associated with treatment response.
Comorbid anxiety disorders as well as substance abuse appear to be negative predictors of response. Comorbid personality disorder diagnoses may not be predictive, as such, but personality dimensions or traits may be. Passive–aggressive personality, extraversion and lower hostility levels contribute to a positive response to therapy. Personality disorders present a complicated picture, with significant interaction between variables. A patient with more comorbid personality problems may have more severe illness and less social support. It is difficult to determine whether any of these variables are truly independent predictors of response or if they all are intertwined, combining to create a situation where the patient is unlikely to achieve a positive response. There is also the additional confound that many Axis II traits appear as symptoms for many Axis I conditions.62 This calls into question whether one can use Axis II traits as a stable independent predictor of changes in Axis I conditions.
Finally, it is important to reiterate that none of the reviewed variables are particularly powerful or consistent predictors of response. Moreover, most, if not all, of the studies reviewed fail to make inference regarding the causal relation between the predictor and outcome variables. For example, it was unclear if the predictor variables were moderators of outcome (i.e., when or under what conditions effects will occur) or mediators of outcome (i.e., how or why effects occur). Future studies might benefit by clarifying the nature of their predictors.
Footnotes
Competing interests: None declared for Dr. Ryder. Dr. Bagby received an honorarium for his contributions to this article, research support to develop the 7-item Hamilton Rating Scale for Depression and to derive cut-off scores, and travel assistance to attend a conference where the data were discussed from CMED. Dr. Bagby also received research support and financial assistance for his work on the conceptual and statistical procedures used to develop the HAM-D7 from Eli Lilly Canada. Dr. Cristi received travel assistance from CMED to attend a conference where she presented data related to this paper.
Correspondence to: Dr. R. Michael Bagby, Centre for Addiction and Mental Health, 250 College St., Toronto ON M5T 1R8; fax 416 979-6821; Michael_Bagby@camh.net
Submitted Jun. 11, 2001 Revised Jun. 13, 2002 Accepted Jun. 13, 2002
References
- 1.Joyce PR, Mulder RT, Cloninger CR. Temperament predicts clomipramine and desipramine response in major depression. J Affect Disord 1994;30:35-46. [DOI] [PubMed]
- 2.Hirschfeld RM, Russell JM, Delgado PL, Fawcett J, Friedman RA, Harrison WM, et al. Predictors of response to acute treatment of chronic and double depression with sertraline or imipramine. J Clin Psychiatry 1998;59:669-75. [DOI] [PubMed]
- 3.Zubenko GS, Mulsant BH, Rifai AH, Sweet RA, Pasternak RE, Marino LJ Jr, et al. Impact of acute psychiatric inpatient treatment on major depression in late life and prediction of response. Am J Psychiatry 1994;151:987-94. [DOI] [PubMed]
- 4.Weissman MM, Prusoff BA, Klerman GL. Personality and the prediction of long-term outcome of depression. Am J Psychiatry 1978;7:797-800. [DOI] [PubMed]
- 5.Kupfer DJ, Spiker DG. Refractory depression: prediction of non-response by clinical indicators. J Clin Psychiatry 1981; 42: 307-12. [PubMed]
- 6.Ezquiaga E, Garcia A, Bravo F, Pallares T. Factors associated with outcome in major depression: a 6-month prospective study. Soc Psychiatry Psychiatr Epidemiol 1998;33(11):552-7. [DOI] [PubMed]
- 7.O'Leary D, Costello F, Gormley N, Webb M. Remission onset and relapse in depression. An 18-month prospective study of course for 100 first admission patients. J Affect Disord 2000; 57: 159-71. [DOI] [PubMed]
- 8.Hazell P, O'Connell D, Heathcote D, Robertson J, Henry D. Efficacy of tricyclic drugs in treating child and adolescent depression: a meta-analysis. Br Med J 1995;310:897-901. [DOI] [PMC free article] [PubMed]
- 9.Ryan ND, Varma D. Child and adolescent mood disorders — experience with serotonin-based therapies. Biol Psychiatry 1998; 44: 336-40. [DOI] [PubMed]
- 10.Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in child and adolescent with depression. Arch Gen Psychiatry 1997;54:1031-7. [DOI] [PubMed]
- 11.Paykel ES, Ramana R, Cooper Z, Hayhurst H, Kerr J, Barocka A. Residual symptoms after partial remission: an important outcome in depression. Psychol Med 1995;25:1171-80. [DOI] [PubMed]
- 12.Kocsis JH, Mason BJ, Frances AJ, Sweeney J, Mann JJ, Marin D. Prediction of response of chronic depression to imipramine. J Affect Disord 1989;17:225-60. [DOI] [PubMed]
- 13.Klein DN, Schatzberg AF, McCullough JP, Dowling F, Goodman D, Howland RH, et al. Age of onset in chronic major depression: relation to demographic and clinical variables, family history, and treatment response. J Affect Disord 1999;55: 149-57. [DOI] [PubMed]
- 14.Kennedy SH, Eisfeld BS, Meyer JH, Bagby RM. Antidepressants in clinical practice: limitations of assessment methods and drug response. Hum Psychopharmacol Clin Exp 2001;16:105-14. [DOI] [PubMed]
- 15.Nierenberg A, McLean NE, Alpert JE, Worthington JJ, Rosenbaum JF, Fava M. Early nonresponse to fluoxetine as a predictor of poor 8-week outcome. Am J Psychiatry 1995:152:1500-3. [DOI] [PubMed]
- 16.Stassen HH, Angst J, Delina-Stula A. Severity at baseline and onset of improvement in depression: meta analysis of imipramine and moclobemide versus placebo. Eur Psychiatry 1994; 9: 129-36.
- 17.Kinzie JD, Lewinsohn P, Maricle R, Teri L. The relationship of depression to medical illness in an older community population. Comp Psychiatry 1986;27:241-6. [DOI] [PubMed]
- 18.Koenig HG, Meador KG, Cohen HJ, Blazer D. Depression in elderly hospitalized patients with mental illness. Arch Intern Med 1988;148:1929-36. [PubMed]
- 19.Murrell SA, Himmelfarb S, Wright K. Prevalence of depression and its correlates in older adults. Am J Epidemiol 1983;117: 173-85. [DOI] [PubMed]
- 20.Cole MG. The prognosis of depression in the elderly. CMAJ 1990;143:633-9. [PMC free article] [PubMed]
- 21.Henrichsen GA, Hernandez NA. Factors associated with recovery from and relapse into major depressive disorder in the elderly. Am J Psychiatry 1993;150:1820-5. [DOI] [PubMed]
- 22.Small GW, Birkett M, Meyers BS, Koran LM, Bystritsky A, Nemeroff CB. Impact of physical illness on quality of life and antidepressant response in geriatric major depression. Fluoxetine Collaborative Study Group. J Am Geriatr Soc 1996;44:1220-5. [DOI] [PubMed]
- 23.George L, Blazer D, Hughes D, Fowler N. Social support and the outcome of major depression. Br J Psychiatry 1989;154:478-85. [DOI] [PubMed]
- 24.Bromberger JT, Wisner KL, Hanusa BH. Marital support and remission of treated depression. A prospective pilot study of mothers of infants and toddlers. J Nerv Ment Dis 1994;182:40-4. [DOI] [PubMed]
- 25.Marwick C. Should physicians prescribe prayer for health? Spiritual aspects of well being considered. JAMA 1995; 273:1561-2. [PubMed]
- 26.Koenig HG, Cohen HJ, Blazer DG, Pieper C, Meador KG, Shelp F, et al. Religious coping and depression among elderly, hospitalized medically ill men. Am J Psychiatry 1992;149:1693-1700. [DOI] [PubMed]
- 27.Nelson PB. Ethnic differences in intrinsic/extrinsic religious orientation and depression in the elderly. Arch Psychiatr Nurs 1989; 3:199-204. [PubMed]
- 28.O'Connor BP, Vallerand RJ. Religious motivation in the elderly: a French-Canadian replication and extension. J Soc Psychol 1990;130:55-9. [DOI] [PubMed]
- 29.Koenig HC. Religion and older men in prison. Int J Geriatr Psychiatry 1994;10:219-30.
- 30.Koenig HG George LK Peterson BL. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry 1998; 155:536-42. [DOI] [PubMed]
- 31.Brown C, Schulber HC, Madonia JH, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry 1996; 153: 1293-1300. [DOI] [PubMed]
- 32.Joffe RT, Bagby RM, Levitt A. Anxious and nonanxious depression. Am J Psychiatry 1993;150:1257-8. [DOI] [PubMed]
- 33.Clayton P. The co-morbidity factor: establishing the primary diagnosis in patients with mixed symptoms of anxiety and depression. J Clin Psychiatry 1990;51:35-9. [PubMed]
- 34.Clayton PJ, Grove WM, Coryell W, Keller M, Hirschfeld R, Fawcett J. Follow-up and family study of anxious depression. Am J Psychiatry 1991;148:1512-7. [DOI] [PubMed]
- 35.Zung W, Magruder-Habib K, Velez R, Alling W. The comorbidity of anxiety and depression in general medical patients: a longitudinal study. J Clin Psychiatry 1990;51:77-80. [PubMed]
- 36.Coryell W, Endicott J, Winokur G. Anxiety syndromes as epiphenomena of primary major depression: outcome and familial psychopathology. Am J Psychiatry 1992;149:100-7. [DOI] [PubMed]
- 37.VanValkenburg C, Akiskal HS, Puzantian V, Rosethal T. Anxious depression: clinical, family history, and naturalistic outcome comparison with panic and major depressive disorder. J Affect Disord 1984;6:67-82. [DOI] [PubMed]
- 38.Feske U, Frank E, Kupfer DJ, Shear MK, Weaver E. Anxiety as a current major depression: an exploratory investigation. Depress Anxiety 1998;8:135-41. [PubMed]
- 39.Grunhaus L, Rabin D, Greden JF. Simultaneous panic and depressive disorders: response to antidepressant treatments. J Clin Psychiatry 1986;47:4-7. [PubMed]
- 40.Frank E, Shear MK, Rucci P, Cyranowski JM, Endicott J, Fagiolini A, et al. Influence of panic-agoraphobic spectrum symptoms on treatment response in patients with recurrent major depression. Am J Psychiatry 2000;157:1101-7. [DOI] [PubMed]
- 41.Mitchell PB, Schweitzer I, Burrows G, Johnson G, Polonowita A. Efficacy of venlafaxine and predictors of response in a prospective open-label study of patients with treatment-resistant major depression. J Clin Psychopharmacol 2000;20:483-7. [DOI] [PubMed]
- 42.Group for the Advancement of Psychiatry and the Committee on Alcoholism and the Addictions. Substance abuse disorders: a psychiatric priority. Am J Psychiatry 1991;148:1291-1300. [DOI] [PubMed]
- 43.Coryell W, Winokur G, Keller M, Scheftner W, Endicott J. Alcoholism and primary major depression: a family study approach to co-existing disorders. J Affect Disord 1992;24:93-9. [DOI] [PubMed]
- 44.Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry 1986;143:993-7. [DOI] [PubMed]
- 45.Khantzian EJ. The self medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am J Psychiatry 1985;142:1259-64. [DOI] [PubMed]
- 46.Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. J Stud Alcohol 1988;49:219-24. [DOI] [PubMed]
- 47.Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, et al. Consumption of alcohol, nicotine, and caffeine among depressed outpatients. Relationship with response to treatment. Psychosomatics 1996;37:518-22. [DOI] [PubMed]
- 48.Winokur G, Black DW, Nasrallah A. Depressions secondary to other psychiatric disorders and medical illnesses. Am J Psychiatry 1988;145:233-7. [DOI] [PubMed]
- 49.Ouimette PC, Gima K, Moos RH, Finney JW. A comparative evaluation of substance abuse treatment IV. The effect of co-morbid psychiatric diagnoses on amount of treatment, continuing care, and 1-year outcomes. Alcohol Clin Exp Res 1999;23: 552-7. [PubMed]
- 50.Fahy TA, Eisler I, Russell GF. Personality disorders and treatment response in bulimia nervosa. Br J Psychiatry 1993;162:765-70. [DOI] [PubMed]
- 51.Pfohl B, Strangl D, Zimmerman M. The implications of DSM-III personality disorders for patients with major depression. J Affect Disord 1984;7:309-18. [DOI] [PubMed]
- 52.Fava M, Bouffides E, Pava JA, McCarthy MK, Steingard RJ, Rosenbaum JF. Personality disorder co-morbidity with major depression and response to fluoxetine treatment. Psychother Psychosom 1994;62:160-7. [DOI] [PubMed]
- 53.Downs NS, Swerdlow NR, Zisook S. The relationship of affective illness and personality disorders in psychiatric outpatients. Ann Clin Psychiatry 1992;4:87-94.
- 54.Joffe RT, Regan JJ. Personality and response to tricyclic antidepressants in depressed patients. J Nerv Ment Dis 1989;177:745-9. [DOI] [PubMed]
- 55.Peselow ED, Fieve RR, Di Figlia C. Personality traits and response to desipramine. J Affect Disord 1992;24:209-16. [DOI] [PubMed]
- 56.Bagby RM, Joffe RT, Parker JDA, Kalembra V, Harkness KL. Major depression and the five-factor model of personality. J Personal Disord 1995;9:224-34.
- 57.Bagby RM, Kennedy SH, Schuller DR, Dickens SE, Minifie CE, Levitt A, et al. Differential pharmacological treatment response in high angry and low angry hostile depressed patients: a retrospective analysis. J Affect Disord 1997;45:161-6. [DOI] [PubMed]
- 58.Bagby RM, Rector NA, Zindel V, Joffe RT, Levitt AJ, Kennedy SH, et al. Rumination and distraction in major depression: assessing response to pharmacological treatment. J Affect Disord 1999; 55:225-9. [DOI] [PubMed]
- 59.Rector NA, Bagby RM, Segal ZV, Joffe RT, Levitt A. Self-criticism and dependency in depressed patients treated with cognitive therapy or pharmacotherapy. Cog Ther Res 2000;24:571-84.
- 60.Fava M, Rosebaum JF, Pava JA, McCarthy MK, Steingard RJ, Bouffides E. Anger attacks in unipolar depression. Part 1: Clinical correlates and response to fluoxetine treatment. Am J Psychiatry 1993;150:1158-63. [DOI] [PubMed]
- 61.Ekselius L, von Knorring L. Personality disorder co-morbidity with major depression and response to treatment with sertraline or citalopram. Int Clin Psychopharmacol 1998;13:205-11. [DOI] [PubMed]
- 62.Ryder AG, Bagby RM. Diagnostic viability of the depressive personality disorder. J Personal Disord 1999;13:99-117. [DOI] [PubMed]