Abstract
There is a growing recognition that relapse and recurrence after the successful treatment of major depression is a common and debilitating outcome that has massive social costs. Although many patients achieve a sustained recovery with maintenance pharmacotherapy, the long-term outcome for a significant proportion of patients is still poor. The purpose of this review is to evaluate the role of combined psychological and pharmacological therapies in minimizing relapse and recurrence in the treatment of depression. Three approaches have been investigated: concurrent treatment, sequential treatment and crossover treatment. Concurrent therapy is as effective as monotherapy for the treatment of mild-to-moderate depressive disorder and shows evidence of a potential treatment advantage in cases where depression is more severe. Consecutive sequencing of pharmacotherapy and psychotherapy has demonstrated some benefit for both the conversion of partial to full response and the prevention of relapse and recurrence, especially in more severely depressed patients. Crossover treatments during the maintenance phase (i.e., switching patients from one treatment to a second after an adequate response to the first) show evidence of being beneficial in preventing relapse and recurrence. Variants of cognitive therapy that have been modified to specifically address residual symptoms in patients who have recovered from depression appear to be the most effective. A review of the studies to date indicates that cognitive therapy may play a role in improving remission rates and decreasing relapse and recurrence rates. Although most studies are small, there is a consistent suggestion of superior prophylaxis for patients receiving some type of sequenced or crossover treatment in which the delivery of antidepressant medication and structured antidepressant psychotherapy is combined. These approaches warrant greater attention; they may present another route for enhancing long-term recovery from major depression.
Medical subject headings: antidepressive agents, behavioral symptoms, cognitive therapy, combined modality therapy, depressive disorder, drug therapy, psychiatric status rating scales, psychotherapy, recurrence, remission induction, treatment outcome
Abstract
On reconnaÎt de plus en plus que la rechute et la récidive après le traitement réussi d'une dépression majeure constituent un résultat courant et invalidant qui entraÎne des coûts énormes pour la société. Même si beaucoup de patients parviennent à se rétablir grâce à une pharmacothérapie d'entretien, le résultat à long terme demeure médiocre pour un pourcentage important des patients. Cette étude vise à évaluer dans quelle mesure les thérapies psychologique et pharmacologique combinées réussissent à minimiser les rechutes et les récidives dans le traitement de la dépression. On a étudié trois démarches : traitement combiné simultané, traitement séquentiel et traitement croisé. La thérapie combinée simultanée est aussi efficace que la monothérapie pour traiter un trouble dépressif de bénin à moyen et montre un avantage possible dans les cas de dépression plus graves. Le séquençage de la pharmacothérapie et de la psychothérapie a montré des avantages en ce qui concerne à la fois la conversion de la réponse partielle en réponse complète et la prévention des rechutes et des récidives, surtout chez les patients dont la dépression est plus grave. Les traitements croisés pendant la phase d'entretien (c.-à-d. faire passer les patients d'un traitement à un deuxième après une réaction adéquate au premier) aident à prévenir les rechutes et les récidives. Des variantes de la thérapie cognitive modifiée pour tenir compte spécifiquement des symptômes résiduels chez les patients qui se sont rétablis d'une dépression semblent les plus efficaces. Une recension des études réalisées jusqu'à maintenant indique que la thérapie cognitive peut jouer un rôle en améliorant les taux de rémission et réduisant les taux de rechute et de récidive. Même si la plupart des études sont d'envergure limitée, elles indiquent constamment une prophylaxie supérieure dans le cas des patients soumis à un traitement séquencé ou croisé dans le cadre duquel on combine l'administration d'un antidépresseur et une psychothérapie structurée contre la dépression. Il convient d'accorder plus d'attention à ces démarches qui peuvent offrir un autre moyen d'améliorer le rétablissement à long terme à la suite d'une dépression majeure.
Introduction
The existence of effective treatment modalities for individuals in a depressive episode has been well documented. Therapies to treat depression have advanced considerably over the past 20 years. However, typical “intent to treat” response rates for both antidepressant pharmacotherapy and short-term psychosocial treatments range from 50% to 60%.1 The fact that episodes of major depression and dysthymia respond well to acute-phase treatments has been used to bolster traditional views of this disorder as a condition that is self-limited in nature and associated with a favourable prognostic picture. There is a growing recognition, however, that relapse and recurrence after successful treatment are common and debilitating outcomes that have massive social costs.2 At present, the best validated and most widely used approach for achieving sustained recovery is maintenance pharmacotherapy. However, the protection afforded lasts only as long as patients continue to take their antidepressant medication. There is also evidence that structured short-term psychotherapies such as cognitive behaviour therapy (CBT) and interpersonal therapy (IPT) administered in the acute phase may reduce relapse risk for patients in recovery.3,4 This may present another route for enhancing long-term recovery from major depression.
Limits of monotherapy in supporting sustained recovery
Relying on either maintenance pharmacotherapy or acute-phase structured psychotherapies alone to ensure sustained recovery from major depressive disorder (MDD) has its drawbacks. An operative assumption behind the use of maintenance pharmacotherapy is that patients will continue to take their medication for extended periods. However, in practice, the rate of noncompliance may be as high as 40%.5 In a study of 155 depressed patients in primary care, 28% of patients stopped taking antidepressants during the first month of treatment, and 44% had stopped taking their medicine by the third month.6 The alternative, providing acute-phase structured psychotherapy on a large scale may also be unrealistic. These treatments depend on scarce, expensive, professionally trained personnel and, as such, it may not be possible to administer these interventions in their traditional format, to make an impact on an illness as prevalent as depression.
If the use of pharmacotherapy or psychotherapy alone has its limits, then would combining them be one way to capitalize on their respective benefits? In this paper, we review the evidence for combining pharmacotherapy and psychotherapy in the treatment of depression.
Treatments reviewed
CBT is a structured approach to the treatment of depression in which patients are trained to identify and modify negative beliefs and negative interpretations of the past, present and future. The elements of treatment in CBT include education, symptom management strategies, stress management, exposure to symptoms or situations to facilitate desensitization to feared stimuli and cognitive challenges to change negative beliefs.7,8
IPT uses a medical model to focus on 4 types of interpersonal problem categories that are viewed as causes of depression. This therapy specifically focuses on grief, interpersonal disputes, role transitions and social deficits.9,10
The cognitive behavioural-analysis system of psychotherapy (CBASP) was developed specifically for the treatment of chronic forms of major depression. The approach draws on many behavioural, cognitive and interpersonal techniques used in other forms of psychotherapy. It teaches patients to focus on the consequences of their behaviour and to use a social problem-solving algorithm to address interpersonal difficulties. CBASP is more structured and directive than IPT and differs from cognitive therapy in that it focuses primarily on interpersonal interactions.11
A number of variants of cognitive therapy (CT) approaches have also been described including mindfulness-based CT (MBCT), which focuses on changing the awareness of thoughts rather than their content.12 Other variants have been designed to specifically target symptoms that remain after antidepressant therapy.8
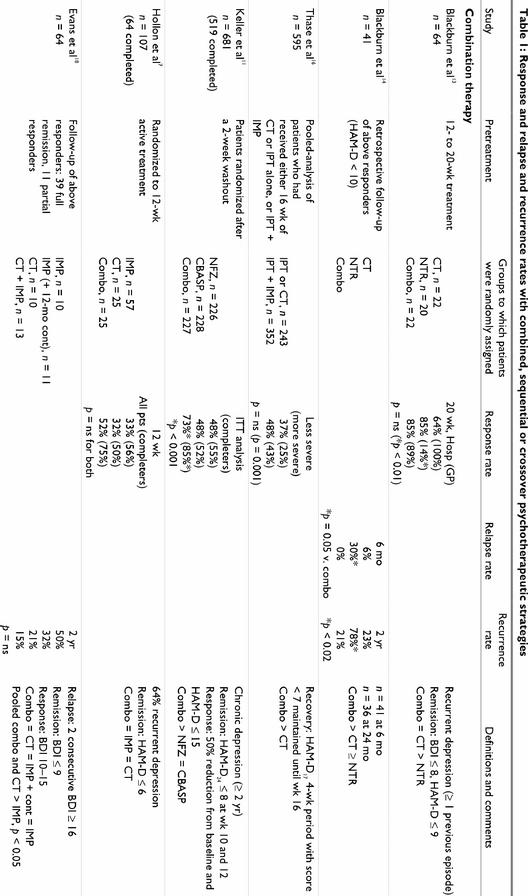
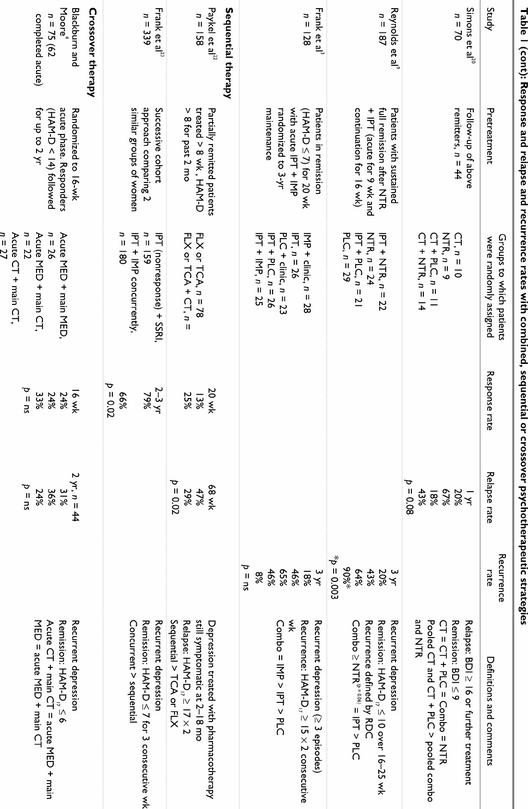
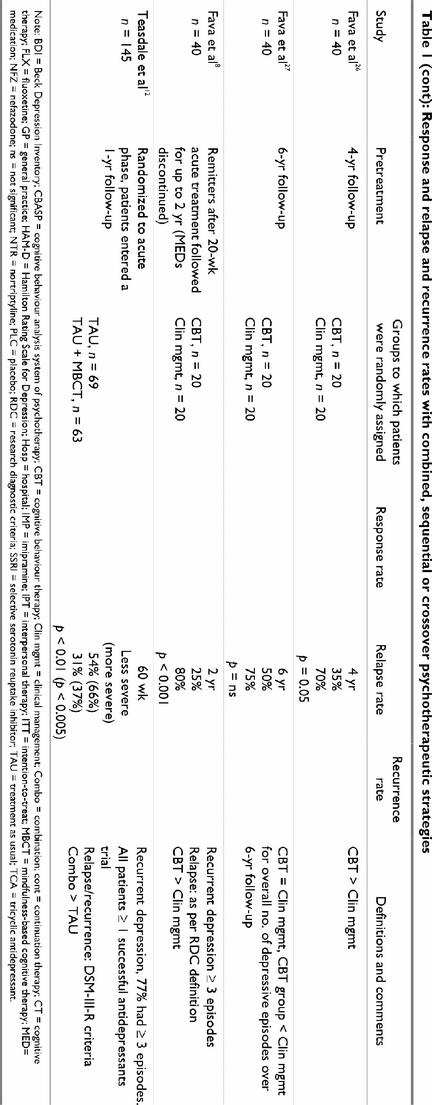
Three approaches have been used to combine pharmacological and psychological treatments in the treatment of depression: (1) concurrent treatment, (2) sequential treatment, in which one treatment is added to the other, and (3) crossover treatment, in which one treatment is discontinued and a second is initiated (Table 1).
Table 1
Table 1 continued
Table 1 continued
Concurrent treatment
One of the first studies to evaluate the concurrent use of pharmacotherapy and psychotherapy was conducted by Blackburn and colleagues in Scotland in 1981.13 They studied hospital outpatients and general practice patients with recurrent depression (i.e., at least 1 previous episode) who were allocated to 1 of 3 treatment groups: CT, tricyclic antidepressant therapy (TCA) or a combination of the 2. Sixty-four patients completed the 12–20 weeks of acute-phase treatment. Data on response rates (50% reduction in Hamilton Rating Scale for Depression [HAM-D]) showed that, for the hospital outpatients, CT was minimally more effective than pharmacotherapy, and the combination of CT and medication had an additive effect, bringing about the highest degree of change. For the general practice patients, CT and combination therapy were superior to medication alone. Rates of full remission, as reported in a follow-up study, revealed that antidepressant therapy was less effective than CT or the combination therapy for both patient groups.14 Of note is the fact that the rate of response in the general practice medication group was lower in this trial than that generally quoted for placebo groups. The superiority of CT alone or in combination with pharmacotherapy may have been related to poor compliance with TCA therapy. No plasma levels were monitored during this study, and compliance issues have been noted with patients seen in general practice in other trials.15
Responders from this trial were followed naturalistically for 2 years. Although most patients maintained their improvement, 30% in the TCA group, 6% in the CT group and no patients in the combined treatment group had relapsed at 6 months.14 This pattern was maintained over the 2-year follow-up period, suggesting a preventative effect with acute CT. Over the 2 years, 23% of patients in the CT group, 78% in the pharmacotherapy group and 21% of the combined therapy group experienced a recurrence of depression. Conclusions are limited by the size of the groups during follow-up, particularly the TCA group, which included only 9 patients.
Since few individual studies have been adequately powered to detect differences between active treatments, meta-analysis is usually required to address this issue. A “mega”-analysis of pooled data of 595 patients with unipolar MDD provided evidence that combined therapy was superior to psychotherapy alone, particularly in the treatment of more severe recurrent depression.16 Patients received 16 weeks of CT alone, IPT alone or IPT and antidepressant therapy. No significant differences were seen between treatments in less severely ill patients, where the remission rate (HAM-D17 < 7 for 4 weeks) for psychotherapy alone was 37% compared with 48% for combined treatment. For more severely ill patients, however, remission rates were significantly better with combined treatment than with psychotherapy alone (43% v. 25%, p = 0.001). In addition, although severity was associated with a longer time to remission among all patients studied, in recurrently depressed patients, combined therapy led to shorter time to remission than psychotherapy alone.
The combination of psychotherapy and pharmacotherapy was also found to be more effective than either treatment alone in a study of 681 patients with chronic MDD for at least 2 years.11 The CBASP, an interpersonally oriented variant of CT developed specifically for the treatment of chronic depression and dysthymia, was compared with antidepressant therapy with nefazodone and with a combination of both therapies. Similar to the findings of the pooled analysis of Thase et al,16 about half the patients who completed the study (n = 519) responded to acute-phase treatment with either nefazodone (55%) or CT (52%) alone, but again the combined treatment was significantly more effective than either treatment alone (85%, p < 0.001).11 Similarly, remission rates were significantly higher for the combination group than they were for CBASP or nefazodone alone (42% v. 24% and 22%, p < 0.001). A preliminary analysis of economic aspects of these acute-phase treatment alternatives estimated mean direct costs per patient, irrespective of response, to be $770 for nefazodone, $1800 for CBASP and $2500 for the combination.17
Despite these promising results, conclusions from earlier studies regarding the advantages of combined therapy over either monotherapy are less definitive. No significant differences in acute-phase response rates were reported in a study comparing imipramine, CT and the combination of imipramine and CT in 107 patients with major depression.7 Initial severity predicted poorer response for the pharmacotherapy group but not for the CT patients. Although not statistically significant, the rate of full remission was higher in the combination therapy group (52%) than in the monotherapy groups (32% and 33%).
A 2-year, post-treatment, follow-up to the CT–imipramine study monitored the 44 subjects who had responded during the 12-week acute-phase treatment.18 Patients who had been treated with CT in the acute phase, either alone or with imipramine, had a significantly lower risk of relapse (64% less) than patients treated with imipramine alone. The rate for those patients who received CT was similar to those who received pharmacotherapy during a 1-year maintenance phase. This suggests that CT during acute-phase treatment may prevent relapse.
In an earlier trial, 87 moderately-to-severely depressed outpatients were randomly assigned to receive 12 weeks of CT, TCA, CT plus TCA or CT plus placebo.19 At 1-month follow-up assessment, the 70 patients who had completed treatment maintained all treatment gains. Both CT and antidepressant drug therapy were found to be effective, and the combination of the treatments did not lead to either additive or negative effects. Again, although the remission rates for combination therapy were the highest, this trial was not adequately powered to detect significant differences between treatments. Of the 44 patients who responded to treatment in this study, 28 were still in remission at a 1-year follow-up.20 Relapse rates were 67% among patients receiving pharmacotherapy alone, 43% in the CT plus TCA group, 20% in the CT monotherapy group and 18% in the CT plus placebo group. When the groups were pooled, patients who had received CT, with or without TCA, had a significantly lower relapse rate than those who received medication (28% v. 66%, p = 0.02). As has been reported in many other trials, sustained improvement was more likely in patients who had very few, if any, residual symptoms after the acute phase of treatment, than it was in those patients who had residual symptoms.
Lower rates of recurrence in 2- and 3-year follow-up studies are often due to patients continuing to take medication into the period of remission or to the effects of acute-phase psychological treatment extending into remission. In many cases, combination treatment has fared only as well as either therapy alone.
The combination of maintenance medication and IPT had demonstrated efficacy in preventing recurrence in a 3-year, double-blind, placebo-substitution trial involving patients aged 60 years and older.9 Patients received open-label therapy with nortriptyline and IPT (9 weeks acute plus 16 weeks continuation therapy). Those with a sustained remission (n = 107) for at least 6 months were randomly assigned to 1 of 4 maintenance groups: IPT plus nortriptyline, nortriptyline plus clinic visits, IPT plus placebo or placebo plus clinic visits for 3 years. Cumulative recurrence rates over 3 years were 20% with IPT plus nortriptyline, 43% with nortriptyline plus clinic visits, 64% with IPT plus placebo and 90% with placebo plus clinic visits. The time to recurrence was significantly better for all 3 active treatment groups than it was for the placebo group. Combination treatment with nortriptyline and IPT was superior to IPT alone but not to nortriptyline monotherapy. Nortriptyline or IPT used singly were not significantly different. In addition, in patients taking maintenance nortriptyline, 53% of the recurrences were associated with noncompliance. Results may have been different if an antidepressant with better tolerability and compliance rates had been used.
In a 3-year maintenance trial of 128 subjects with recurrent depression, maintenance pharmacotherapy was as effective as combined maintenance IPT and imipramine in preventing recurrence.3 Patients were randomly assigned to maintenance therapy with 1 of the following: imipramine plus medication clinic visits, IPT plus imipramine, placebo plus medication clinic visits, IPT alone or IPT plus placebo. Imipramine treatment and the combination therapy effectively delayed recurrence; however, they were not significantly different from each other. Monthly IPT also appeared to have a modest prophylactic effect, lengthening the time between episodes in patients not receiving medication. The risk of recurrence for those not receiving drug therapy was 4.9, compared with 1.7 for those not receiving IPT.
The cost implications of combination therapy are important to consider as well. A cost-effectiveness analysis of CBT and fluoxetine projected CBT to be the most cost-effective treatment, followed by combined treatment and then fluoxetine alone. It was estimated that compared with CBT alone, the costs over a 2-year period would be 33% higher with fluoxetine alone and 23% higher with the combination treatment.21
To summarize, combination therapy for MDD may offer an advantage over psychotherapy alone or pharmacotherapy alone, especially for patients with more severe, chronic and recurrent depression.13 However, many of the studies published to date were not adequately powered to detect significant differences. Larger samples are necessary to fully examine this question. Combination therapy may also offer an advantage in the prevention of relapse or recurrence, but again, in most cases, the samples were too small and the differences between groups did not achieve statistical significance.7,18,19,20 The modalities most often considered for inclusion in studies of combined treatment are CBT, IPT and CBASP. Although the number of patients studied with CBASP is impressive (i.e., in Keller et al,11 n = 681), this is only 1 study, and replication studies are required.
Consecutive sequencing of pharmacotherapy and psychotherapy
Combination therapy for depression can also be administered in a fashion that uses psychotherapy to augment any initial response to pharmacotherapy or vice versa. Although very little data are available examining this strategy, 1 study22 examined the addition of CT to pharmacotherapy, and another,23 the addition of pharmacotherapy to previous CT. The focus remains on obtaining a robust acute-phase treatment response, but there is also increased interest in whether this particular type of combination can have an impact on long-term outcomes as well. In light of the fact that a common problem after acute-phase treatment is partial remission, with the presence of residual symptoms, it is not surprising that this issue has been addressed.
In a recent controlled clinical trial conducted in the United Kingdom, CT showed a benefit in a difficult-to-treat population of patients who had achieved only partial remission with antidepressant treatment.22 The study involved 158 patients who had been taking either fluoxetine or a TCA for at least 8 weeks but who had a HAM-D score of ≥ 8 for the past 2 months. Patients were randomly assigned to continue pharmacotherapy alone or combine it with CT for 20 weeks. The same pharmacotherapy regimen was maintained for 1 year. CT had an additive effect with medication for the prevention of relapse; it significantly reduced the relapse rates from 47% in the pharmacotherapy only group to 29% in the group also receiving CT (p = 0.02). Furthermore, CT was started after partial remission, avoiding the potential difficulties of a differential sieve as a function of treatments offered. This study is complicated by the fact that few patients achieved remission in the initial 20 weeks of treatment.
Successive cohorts were used to compare the rates of remission when pharmacotherapy was added to psychotherapy and when both were used from the outset of treatment.23 One group of women with recurrent depression received the combination of IPT and imipramine at the outset; in the second group, those who did not remit with IPT alone were offered the combination of IPT and an selective serotonin reuptake inhibitor. Both groups were demographically comparable, but the women in the sequential group were in at least their second depressive episode, whereas those in the combination treatment protocol were in at least their third episode, potentially indicating a more severe illness. A significantly greater percentage of women achieved remission in the sequential group than in the combination therapy from the outset (79% v. 66%, p < 0.02). The greatest difference was seen in patients with more severe illness, where remission was 81% with sequential and 58% with combination therapy. The authors suggest that providing initial IPT alone in the sequential treatment strategy acted like a sieve, thereby selecting the group who would be responsive to pharmacotherapy. Despite the differences in severity levels and medications, it appears that in women with recurrent depression who have not achieved remission with IPT alone, adding an antidepressant may be an effective treatment strategy.
Sequencing psychotherapy and pharmacotherapy may be effective for patients who show a partial or nonresponse to initial treatment (antidepressant or CT), particularly for patients with more severe depression.22 Effects have been noted for the conversion of partial to full response and the prevention of relapse and recurrence. However, more data on the utility of this strategy are needed.
A Depression Guideline Panel24 suggested adding psychotherapy to medication in the treatment of depression if:
· the patient shows a partial response to pharmacotherapy,
· there is a partial or complete response to pharmacotherapy but significant psychosocial stressors remain or
· there are problems with adherence.
From the perspective of managing nonresponse to psychotherapy alone, the recommendation is that adding an antidepressant would be warranted in cases where the patient shows a poor response to psychotherapy alone after 6 weeks or a partial response after 12 weeks. In both instances, the physician would have to decide whether to continue with psychotherapy or discontinue it in favour of clinical management.24
Crossover of treatments during the maintenance phase
Studies of crossover of treatments focus on increasing survival time to relapse and recurrence rather than boosting the acute-phase response. In fact, a full acute-phase remission is often required for patients to be eligible for switching to a second treatment.
In a long-term study of 75 outpatients, the efficacy of switching patients from acute-phase treatment with antidepressant medication to CT or continuing with medication was equal to that of acute and maintenance CT.4 Analysis of the 16-week acute phase revealed no significant differences in full remission rates across the 3 groups. At the 2-year follow-up, all 3 groups continued to exhibit the same pattern of improvement, with no significant difference between treatments. CT was as effective as antidepressant medication in the short-term and maintenance periods, and maintenance CT after acute treatment with antidepressant medication was a viable alternative to maintenance medication.
Although one must always be careful when accepting the null hypothesis (i.e., no differences among treatments), it is important to bear in mind the intent behind these comparisons. If a psychological intervention is found to be as effective as the current standard of care (i.e., maintenance pharmacotherapy), this is an important outcome from a public health perspective. It translates into more options being available for the care of those with depression.
In a long-term study, 40 patients who were successfully treated with antidepressant drugs were randomly assigned to receive either CBT or clinical management for 20 weeks.25,26,27 In both groups, antidepressant drugs were tapered and discontinued. The group that received CBT had a significantly lower level of residual symptoms after drug discontinuation than the clinical management group. These patients were followed up for 6 years. At the 2-, 4- and 6-year follow-up, the CBT group demonstrated a lower rate of relapse, which reached statistical significance at the 4-year follow-up. At that time, relapse was reported in 35% of patients in the CBT group and in 70% of the clinical management group. Beyond year 4, the protective effects of CBT appeared to fade; the difference in relapse rates was no longer significant at the 6-year follow up. However, the total number of depressive episodes was lower in the CBT group during the entire follow-up period, and CBT appeared to extend the time to relapse. The treatment of residual symptoms with CBT led to a significantly lower risk of relapse over 4 years and was associated with a more favourable course overall.
The effect of a form of CBT, modified to include elements of lifestyle management, on residual symptoms after pharmacotherapy has been assessed in patients with recurrent depression.8 Forty patients with recurrent major depression who had been successfully treated with antidepressants were randomly assigned to receive either modified CBT or clinical management for 20 weeks. The modified CBT group had a significantly lower level of residual symptoms after discontinuation of drug therapy and at the 2-year follow-up had a much lower rate of relapse (25%) than the clinical management group (80%). In the absence of a maintenance medication group, it is unclear whether the modified CBT conferred additional benefit over standard maintenance pharmacotherapy. The authors speculate that CBT may act on those residual symptoms of major depression that progress to become prodromal symptoms of relapse.
In a multicentre randomized controlled trial of patients with recurrent major depression but in remission or recovery, Teasdale and colleagues12 examined the benefit of adding MBCT to usual treatment for preventing relapse.12 MBCT is designed specifically for formerly depressed patients and is aimed at decreasing stress reactivity and improving patients' early recognition of relapse-related negative thinking. One hundred and forty-five recovered depressed patients were randomly assigned to receive treatment as usual (TAU) or TAU plus MBCT for 8 weeks. Over the 60-week study period, for patients with 3 or more previous episodes of depression (77% of the sample), MBCT significantly reduced the relapse–recurrence rate. For those with 2 previous episodes of depression, the addition of MBCT did not reduce relapse or recurrence. Again, in the absence of a maintenance medication group, it is unclear whether the MBCT provided additional benefit over standard maintenance pharmacotherapy. This is important because, in patients with residual depression who are at high risk for further episodes, continuation of medication may more accurately reflect clinical practice. Future studies of MBCT should include a group that receives continuation pharmacotherapy for comparison purposes.
Evidence suggests that switching patients with unipolar major depression from one treatment to another after an adequate response to the first may help prevent relapse or recurrence. The effects of this strategy have largely been observed in lower relapse rates with the addition of CT than without after the discontinuation of successful pharmacotherapy. The one comparison of switching treatments in which acute pharmacotherapy and maintenance psychotherapy was compared with acute and maintenance psychotherapy found both conditions to be equally effective.3 The psychological treatments found to be most effective have been variants of CBT and IPT that have been modified specifically to address residual symptoms in depressed patients in recovery.
Finally, it is important to recognize that, at present, the generalizability of many of these empirical findings may be limited because of community-based practice patterns that embrace less well-studied and more generic forms of psychological treatment. Further work is needed, not only to validate the enduring effects of combined and sequenced phase-specific treatments for depression, but also to educate practitioners about the benefits to their patients of adopting these treatments.
Summary
CT may play a role in improving remission rates and decreasing relapse and recurrence rates. Although most studies are small, evidence suggests better outcomes with combination therapy than with either medication or CT alone. Benefits may be greater in patients with more severe depression. For patients who continue to experience residual symptoms after antidepressant treatment, time-limited structured psychotherapy may improve long-term outcomes, but it appears to have little effect on short-term remission rates.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. Zindel Segal, Departments of Psychiatry and Psychology, University of Toronto, Toronto ON M5T 1R8; fax 416 979-6821; zindel_segal@camh.net
Submitted Jun. 11, 2001 Revised Mar. 18, 2002 Accepted Mar. 28, 2002
References
- 1.Wells KB, Sturm R, Sherbourne CD, Meredith LS. Caring for depression. Boston (MA): Harvard University Press; 1996.
- 2.Mintz J, Mintz LI, Arruda MJ, Hwang SS. Treatment of depression and the functional capacity to work. Arch Gen Psychiatry 1992;49:761-8. [DOI] [PubMed]
- 3.Frank E, Kupfer DJ, Perel JM, Cornes C, Jarrett DB, Mallinger AG, et al. Three-year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiatry 1990;47:1093-9. [DOI] [PubMed]
- 4.Blackburn IM, Moore RG. Controlled acute and follow-up trial of cognitive therapy and pharmacotherapy in outpatients with recurrent depression. Br J Psychiatry 1997;171:328-34. [DOI] [PubMed]
- 5.Basco MR, Rush AJ. Compliance with pharmacology in mood disorders. Psychiatric Ann 1995;25:269-79.
- 6.Lin EH, Von Korff M, Katon W, Bush T, Simon GE, Walker E, et al. The role of the primary physician in patients' adherence to antidepressant therapy. Med Care 1995;33:67-74. [DOI] [PubMed]
- 7.Hollon SD, DeRubeis RJ, Evans MD, Wiemer MJ, Garvey MJ, Grove WM, et al. Cognitive therapy and pharmacotherapy for depression: singly and in combination. Arch Gen Psychiatry 1992; 49:774-81. [DOI] [PubMed]
- 8.Fava GA, Rafanelli C, Grandi S, Conti S, Belluardo P. Prevention of recurrent depression with cognitive behavioral therapy. Arch Gen Psychiatry 1998;55:816-20. [DOI] [PubMed]
- 9.Reynolds CF 3rd, Frank E, Perel JM, Imber SD, Cornes C, Miller MD, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years. JAMA 1999;281:39-45. [DOI] [PubMed]
- 10.Klerman GL, Weissmann MM. Interpersonal psychotherapy (IPT) and drugs in the treatment of depression. Pharmacopsychiatry 1987;20:3-7. [DOI] [PubMed]
- 11.Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioural-analysis system of psychotherapy and their combination therapy for the treatment of chronic depression. N Engl J Med 2000;342:1462-70. [DOI] [PubMed]
- 12.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 2000;68:615-23. [DOI] [PubMed]
- 13.Blackburn IM, Bishop S, Glen AI, Whalley LJ, Christie JE. The efficacy of cognitive therapy in depression: a treatment trial using cognitive therapy and pharmacotherapy, each alone and in combination. Br J Psychiatry 1981;139:181-9. [DOI] [PubMed]
- 14.Blackburn IM, Eunson KM, Bishop S. A two-year naturalistic follow-up of depressed patients treated with cognitive therapy, pharmacotherapy and a combination of both. J Affect Disord 1986;10:67-75. [DOI] [PubMed]
- 15.Johnston DA. Treatment of depression in general practice. BMJ 1973;11:18-20. [DOI] [PMC free article] [PubMed]
- 16.Thase ME, Greenhouse JB, Frank E, Reynolds CF 3rd, Pilkonis PA, Hurley K, et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry 1997;54:1009-15. [DOI] [PubMed]
- 17.Russell JM, Crown WH, Arnow BA, et al. Economic aspects of nefazodone, CBASP, and their combination for the treatment of chronic depression [abstract]. J Eur Coll Neuropsychopharmacol 2000;10:S239.
- 18.Evans MD, Hollon SD, DeRubeis RJ, Piasecki JM, Grove WM, Garvey MJ, et al. Differential relapse following cognitive therapy and pharmacotherapy for depression. Arch Gen Psychiatry 1992; 49:802-8. [DOI] [PubMed]
- 19.Murphy GE, Simons AD, Wetzel RD, Lustman PJ. Cognitive therapy and pharmacotherapy: singly and together in the treatment of depression. Arch Gen Psychiatry 1984;41:33-41. [DOI] [PubMed]
- 20.Simons AD, Murphy GE, Levine JL, Wetzel RD. Cognitive therapy and pharmacotherapy for depression: sustained improvement over one year. Arch Gen Psychiatry 1986;43:43-50. [DOI] [PubMed]
- 21.Antonuccio DO, Thomas M, Danton WG. A cost-effectiveness analysis of cognitive behavior therapy and fluoxetine (Prozac) in the treatment of depression. Behav Ther 1997;28:187-210.
- 22.Paykel ES, Scott J, Teasdale JD, Johnson AL, Garland A, Moore R, et al. Prevention of relapse in residual depression by cognitive therapy. Arch Gen Psychiatry 1999;56:829-35. [DOI] [PubMed]
- 23.Frank E, Grochocinski VJ, Spanier CA, Buysse DJ, Cherry CR, Houck PR, et al. Interpersonal psychotherapy and antidepressant medication: Evaluation of a sequential treatment strategy in women with recurrent major depression. J Clin Psychiatry 2000; 61:51-7. [PubMed]
- 24.Depression Guideline Panel. Depression in primary care: Vol. 2. Treatment of major depression. Clinical Practice Guideline Number 5. Rockville (MD): US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1993. AHCPR publication no 93-0551.
- 25.Fava G, Grandi S, Zielezny M, Canestrari R, Morphy MA. Cognitive behavioural treatment of residual symptoms primary major depressive disorder. Am J Psychiatry 1994;151:1295-9. [DOI] [PubMed]
- 26.Fava G, Silvana G, Zielezny M, Rafanelli C, Canestrari R. Four-year outcome for cognitive behavioural treatment of residual symptoms primary major depressive disorder. Am J Psychiatry 1996;153:945-7. [DOI] [PubMed]
- 27.Fava G, Silvana G, Zielezny M, Canestrari R, Morphy MA. Six-year outcome for cognitive behavioral treatment of residual symptoms primary major depressive disorder. Am J Psychiatry 1998; 155:1443-5. [DOI] [PubMed]