Abstract
A 67-year-old left-handed woman with a diagnosis of pseudodementia was being treated for depression with little benefit. Neuropsychological evaluations revealed features of angular gyrus syndrome, namely, agraphia, alexia, Gerstmann's syndrome and behavioural manifestations such as depression, poor memory, frustration and irritability. A computed tomographic scan showed a right occipito-temporal infarction, which had occurred 18 months earlier. The patient demonstrated aspects of language dysfunction associated with the syndrome and showed reversed lateralization of cerebral functions. Recognizing and distinguishing between angular gyrus syndrome and depression is important because the appropriate therapies differ. The use of the term pseudodementia can be misleading.
Medical subject headings: depressive disorder; dementia; dementia, multi-infarct; Gerstmann syndrome; language disorders
Abstract
Une femme gauchère âgée de 67 ans chez laquelle on avait diagnostiqué une pseudodémence suivait des traitements contre la dépression qui donnaient peu de résultats. Les évaluations neuropsychologiques ont révélé des caractéristiques du syndrome du gyrus angulaire, soit l'agraphie, l'alexie, le syndrome de Gerstmann et des manifestations comportementales comme la dépression, une mauvaise mémoire, la frustration et l'irritabilité. Une tomodensitométrie a révélé un infarctus occipito-temporal du côté droit survenu 18 mois plus tôt. La patiente avait des aspects du dysfonctionnement du langage associés au syndrome et manifestait une latéralisation inversée des fonctions cérébrales. Il importe de reconnaÎtre le syndrome du gyrus angulaire et la dépression et de distinguer les deux parce que les thérapies pertinentes diffèrent. L'utilisation du terme pseudodémence peut être trompeuse.
Introduction
Lesions causing damage to the angular gyrus can give rise to a constellation of symptoms. The classic symptoms include alexia with agraphia, constructional disturbances with or without Gerstmann's tetrad and behavioural manifestations such as depression, poor memory, frustration and belligerence.1 The symptom profile can resemble a number of other disorders; it has been mistaken, for instance, for dementia.1 Because patients with angular gyrus syndrome meet the criteria for dementia (i.e., verbal recall deficit and one or more additional cognitive disturbances), they are often misdiagnosed as suffering from Alzheimer's disease. In a study of 14 patients with features of angular gyrus syndrome, experienced clinicians misdiagnosed 7 patients with Alzheimer's disease.1
The term pseudodementia is often used to refer to apparent dementia in depressed patients or in patients with nonorganic psychiatric disorders. It is sometimes difficult to distinguish dementia from depression; there are several clinical similarities between the 2 disorders, and depression is often accompanied by cognitive symptoms. Thus, patients with dementia have been erroneously diagnosed with depression and vice versa.2 Dementia has a number of causes, but an incorrect diagnosis of depression as the cause of dementia in an elderly patient can be hazardous.3
We report a case of angular gyrus syndrome that went unrecognized and was mistakenly treated as depressive pseudodementia.
Case report
A 67-year-old left-handed woman was referred with a diagnosis of possible dementia or pseudodementia. Her memory was poor, and she had suffered from anxiety and irritability for over a year. A year and a half earlier, she had suddenly collapsed, and the computed tomographic (CT) scan of her brain that was done at the time showed a subarachnoid hemorrhage. Subsequent investigations revealed a right occipitotemporal infarction and bifrontal subdural collections. Neuroimaging with spiral CT and magnetic resonance imaging (MRI) did not reveal any evidence of an aneurysm. Clinically, the patient showed evidence of language dysfunction. She was enrolled in an active rehabilitation program and, at the time of discharge, was moving around independently.
The patient lived with her daughter for 2 weeks and was then able to live on her own and function independently. When she was seen 6 weeks later, it was established that she had difficulty writing. She had left-sided visual inattention but no focal or lateralizing signs. She was strongly left-handed, but there was no family history of left-handedness. Her only son was right-handed. About 6 months later, she was seen by her treating physician and was diagnosed with depression and prescribed antidepressants (paroxetine, fluoxetine and sertraline), which were given serially for more than 3 months with little effect.
Clinical evaluation
When she was seen for evaluation, her vital signs were unremarkable. There was no evidence of cardiac decompensation, and there were no overt abnormalities in the respiratory and gastrointestinal systems. Examination of the nervous system revealed a left inferior quadrantanopia (i.e, blindness in 1 quarter of the visual field). There was no optic ataxia. Muscle strength was preserved, and there was no sensory impairment for either cutaneous or discriminative (topographical localization, direct simultaneous stimulation and stereognosis) sensations. She had no history of mental illness, and there was no family history of mental illness. Inquiry into sleep, appetite, weight loss, thoughts about the future and capacity for pleasure did not reveal any symptoms of significant depression. Her mood was normal, but she appeared anxious. Her score on the Geriatric Depression Scale4 was 6 out of 15, indicating no significant depression. The Geriatric Depression Scale was designed for the elderly who often have real physical complaints; because questions on health status may give rise to false-positive results, the questions focus instead on psychiatric and quality-of-life issues.5 Routine hematological and biochemical investigations (including thyroid function, vitamin B12 and red cell folate levels) were within normal limits.
Imaging results
A CT scan of the brain was performed, and slices were labelled according to lesion localization maps of Naeser and Hayward.6 The scan showed a hypodense area in the right occipital region involving of the mesial aspect of the occipital cortex and the middle and inferior temporal gyri (Fig. 1).
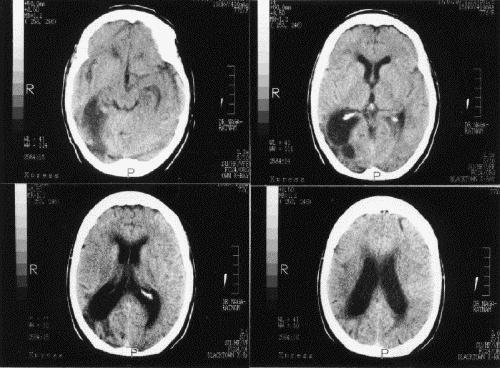
Fig. 1: Computed tomographic scan shows a deep right temporal lesion in the occipital lobe with localized enlargement of the posterior horn of the lateral ventricle and some involvement of the angular gyrus.
Memory and cognition
The patient's score on the Mini-Mental State Examination was 26 out of 30 (considered “normal”).7 She could draw the face of a clock but had some difficulty copying geometric designs. Her ability to abstract was not impaired.
Language
Communicative ability was assessed using the Apraxia Battery for Adults and informally assessed using sections of the Boston Diagnostic Aphasia Examination. Speech output was generally fluent, and automatic speech, repetition of words and phrases, visual confrontation and responsive naming remained intact. Comprehension was functional.
Word finding: Despite being unable to identify mathematic symbols, the patient had no difficulty naming objects and their function, colours and geometric forms.
Reading: This was dysfluent, with the output being contaminated by literal paraphasias and frequent pausing. The patient self-corrected without assistance, but abnormal prosodic features were evident. There was a distinct absence of appropriate phrasing, reduced melodic contour and a somewhat “stumbling” delivery. She also exhibited audible searching on several occasions.
Writing: The patient demonstrated a preference for block writing, stating that she was unable to produce lower-case cursive writing. Letters were occasionally malformed, and no effort was made to correct them. Overall, written output was legible, but she had difficulty differentiating between certain letters (e.g., lower-case p's and a's and upper-case R's and G's). Although spontaneous writing was accurate, writing from dictation proved less so, and repetition was necessary. During dictation, the patient was producing only 4–5 words independently. Copying was unimpaired.
Oral agility: Both verbal and nonverbal agility were rated to be accurate, although a slight delay in the execution of some movements was noted.
Limb and oral apraxia: Apraxia was tested with 5 transitive and 5 intransitive limb gestures, 2 transitive and 2 intransitive buccofacial movements and 2 serial acts. To eliminate comprehension difficulties, the method of Kertesz and Hooper8 was used. No significant impairment was identified in this area.
Prosody: The ability to repeat affective prosody in speech was assessed using the method described by Speedie et al.9 The patient performed remarkably well and was able to vary her tone to demonstrate happiness, sadness, anger and neutral affect when repeating statements.
Neurobehavioural results
Calculia and number writing: Despite continual assistance, only 1 of 9 responses was accurate. On several occasions, the name of the number was written instead of the figure; other times, digits were omitted or large numbers were written as separate components (e.g., eight hundred and twenty was written as 800 20). The patient was unaware of these errors. She also exhibited errors in transcoding numbers and had difficulty recognizing the symbols for multiplication (х) and division (÷), yet had no spatial difficulties, including with the alignment of numbers. When presented with mathematical problems verbally, the subject had difficulty writing the sum; she found the task easier when problems were written out.
Disturbances of body schema (right–left disorientation): When orientation to her own body was tested, (i.e., when touched by the examiner or, later, when requested verbally), the patient had no difficulty identifying lateral body parts. She did have difficulty executing double uncrossed and crossed movements on verbal command, and accuracy decreased with her eyes closed. When orientation toward the examiner was tested, the patient successfully named several of the examiner's body parts, with her eyes closed and open, but when verbally asked to identity various parts, she was hesitant and tended to look at her body to help her. Crossed and uncrossed movements proved difficult, and when the patient quickly became despondent, and the tasks were abandoned.
Finger identification: All fingers were accurately identified on verbal command; she made only 1 error.
Discussion
The left cerebral hemisphere controls the production and comprehension of spoken and written language, and hand preference is associated with hemisphere dominance. The left hemisphere is dominant for right-handed individuals and most left-handed people. The right hemisphere (nondominant) is known to contribute to certain linguistic features such as affective prosody and emotional gesturing. For the patient we described, there is sufficient evidence to suggest the right hemisphere is the dominant hemisphere.10
The angular gyrus, located in the left temporal lobe, is part of the language system of the brain, which also includes Broca's area and Wernicke's area; damage to the angular gyrus gives rise to alexia and agraphia.11 Even if the angular gyrus is spared, it can still be isolated by lesions immediately subcortical to it or by lesions involving the mesial part of the occipital cortex (Fig. 1) and the splenium of the corpus callosum,12 which will result in alexia and agraphia.
Agraphia can be associated with language dysfunction (aphasic agraphia) or with the inability to perform the motor act (apraxic agraphia); the latter can occur with normal praxis.13 The anatomic abnormality can be found in the hemisphere contralateral to the hand used for writing14 or in the ipsilateral hemisphere.13 Our patient had a preference for upper-case cursive writing. The production of correct case (upper or lower) and style (cursive) is directed by the allographic store.15 Interestingly, the case of a man with selective ideational agraphia for lower-case letters, led Kartsounis16 to suggest that the representation of upper- and lower-case letters were independent.
Gerstmann's syndrome, characterized by a disturbance of the body schema, includes the loss of the ability to express thoughts in writing (agraphia), to perform simple arithmetic problems (acalculia), to recognize or indicate one's own or another's fingers (finger agnosia) and to make a distinction between right and left. This patient demonstrated most features of the tetrad. She had agraphia, alexia for numerals and difficulty with mathematic symbols. Although Gerstmann17 describes the acalculia associated with the syndrome as anarithmetria (i.e., a computational impairment), others18 suggest it is due to spatial difficulties. Finger agnosia and left–right discrimination are the other components of the syndrome. Our patient did not have finger agnosia but did have difficulties with crossed and uncrossed movements. She had no anomia and, apart from difficulty with arithmetic symbols, had no difficulty naming objects and their function, parts of objects, colours or geometric figures.
In general, 30%–50% of stroke patients develop major or minor depressive disorders.19 Although the mechanisms involved are likely complex, the nature of the depressive symptoms may be associated with the site of the lesion. Major depression has been found to occur more frequently in patients with left anterior lesions (frontal or basal ganglia), whereas minor depression has been associated with either right or left parieto-occipital lesions.19,20 Symptoms can be delayed months or years after an initial insult.19,21
There are reports of pseudodementia being associated with organic brain lesions.22,23 The use of the term “pseudodementia” can be misleading, for some may dismiss the possibility that underlying dementia or other organic disorders are present. However, Sachdev et al24 report that their longitudinal study of 19 patients diagnosed with pseudodementia validated the clinical usefulness of the term. In most patients, they found no evidence of dementing illness; the course of the illnesses remained the primary psychiatric disorders responsible for the pseudodementia diagnosis. However, 1 of the patients had dressing apraxia, acalculia, finger agnosia and disorientation in space, another made mistakes with finger recognition and naming tasks, and a third had minor expressive aphasia and constructional apraxia. Two other patients had difficulty copying geometric figures. There were no CT results reported for these 5 patients who closely resemble the one we have described, but the depressive symptoms in these patients were most likely a manifestation of the angular gyrus-like syndrome.
In summary, overlapping symptoms often make it difficult to distinguish mood and cognitive disorders. However, angular gyrus syndrome and pseudodementia have different clinical patterns, which can help to differentiate them. Disturbances in cognitive function, particularly those relating to language function, are defining features of angular gyrus syndrome. In depression, the depressive symptoms precede the cognitive symptoms, and they resolve with the resolution of the illness.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. N. Nagaratnam, Consultant Physician, Blacktown–Mount Druitt Health, Blacktown NSW 2148, Australia; fax 61-2-98818020; nage@mail2me.com.au
Submitted Jul. 25, 2001 Revised Mar. 1, 2002 Accepted Apr. 25, 2002
References
- 1.Benson DF, Cummings JL, Tsai SY. Angular gyrus syndrome simulating Alzheimer's Disease. Arch Neurol 1982;38:616-20. [DOI] [PubMed]
- 2.Nagaratnam N, Lewis-Jones M. Predictive properties of referral communications for mental illness and dementia in a community. Dement Geriatr Cogn Disord 1998;9:117-20. [DOI] [PubMed]
- 3.Taylor MA. Pseudo-pseudodementia [editorial]. Neuropsychiatry Neuropsychol Behav Neurol 1999;12:81. [PubMed]
- 4.Sheikh JJ, Yesavage JD. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontologist 1986;5:165-75.
- 5.Yesavage JA. Depression in the elderly. How to recognise masked symptoms and choose appropriate therapy. Postgrad Med 1992;91:255-8,261. [DOI] [PubMed]
- 6.Naeser MA, Hayward RW. Lesion localization in aphasia with cranial computed tomography and the Boston Diagnostic Aphasia Examination. Neurology 1978;28:545-51. [DOI] [PubMed]
- 7.Folstein MF, Folstein E, McHugh PR. Mini-Mental State: practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1977;12:189-92. [DOI] [PubMed]
- 8.Kertesz A, Hooper P. Praxis and language: the extent and variety of apraxia and aphasia. Neuropsychology 1982;20:275-86. [DOI] [PubMed]
- 9.Speedie J, Coslett HB, Heilmab KM. Repetition of affective prosody in mixed transcortical aphasia. Arch Neurol 1984;41: 268-70. [DOI] [PubMed]
- 10.Nagaratnam N, Barnett C, Yeoh J. Neurobehavioural deficits following right cerebral infarction. Neurocase 1999;5:441-6.
- 11.Greenblatt SH. Alexia without agraphia or hemianopsia. Anatomical analysis of an autopsied case. Brain 1973; 96:307-16. [DOI] [PubMed]
- 12.Friedman R, Wren DE, Albert ML. Alexia. In: Heilman KM, Valenstein E, editors. Clinical neuropsychology. New York: Oxford University Press; 1993. p. 49-73.
- 13.Roeltgen DP, Heilman KM. Apraxic agraphia in a patient with normal praxis. Brain Lang 1983;15:35-46. [DOI] [PubMed]
- 14.Baxter DM, Warrington EK. Ideational agraphia: a single study. J Neurol Neurosurg Psychiatry 1986;49:369-74. [DOI] [PMC free article] [PubMed]
- 15.DeBastian K, Barry CA. A cognitive analysis of an acquired dysgraphic patient with an “allographic” writing disorder. Cogn Neuropsychology 1989;6:25-41.
- 16.Kartsounis LD. Selective lower case letter ideational dysgraphia. Cortex 1992;28:145-50. [DOI] [PubMed]
- 17.Gerstmann J. Syndrome of finger agnosia disorientation for right and left agraphia and acalculia. Arch Neurol Psychiatry 1940; 44:398-408.
- 18.Critchley M. The parietal lobes. London: Edward Arnold; 1953.
- 19.Starkstein SE, Robinson RG. Affective disorders and cerebrovascular disease. Br J Psychiatry 1989;154:170-82. [DOI] [PubMed]
- 20.Nagaratnam N, Pathma-Nathan N. Behavioural and psychiatric aspects of silent cerebral infarction. Br J Clin Pract 1997;51:160-3. [PubMed]
- 21.Levine DM, Finkelstein S. Delayed psychosis after right temporo-parietal stroke or trauma relation to epilepsy. Neurology 1983; 32:267-73. [DOI] [PubMed]
- 22.Ron MA, Toone BK, Garralda ME, Lishman WN. Diagnostic accuracy in presenile dementia. Br J Psychiatry 1979;134:161-8. [DOI] [PubMed]
- 23.Shraberg D. The myth of pseudo-dementia. Depression and the aging brain. Am J Psychiatry 1978;35:601-3. [DOI] [PubMed]
- 24.Sachdev PS, Smith JS, Angus-Lepean H, Rodriguez I. Pseudo-dementia twelve years on. J Neurol Neurosurg Psychiatry 1990; 53: 254-9. [DOI] [PMC free article] [PubMed]


