Abstract
Recently, a potential neuroprotective effect of rimonabant, independent of the CB1 receptor interaction, has been proposed. In the present study, the role of transient receptor potential channel vanilloid subfamily member 1, named VR1, on neuroprotective effect of rimonabant, on global cerebral ischemia in gerbils, was investigated.
Rimonabant (0.05–3 mg kg−1), given i.p. 5 min after recirculation, dose dependently antagonized the ischemia-induced decrease in electroencephalographic (EEG) total spectral power and restored relative frequency band distribution 7 days after ischemia.
Rimonabant (0.125–0.5 mg kg−1) fully prevented ischemia-induced hyperlocomotion 1 day after ischemia and memory impairment evaluated in a passive avoidance task, 3 days after ischemia.
At 7 days after ischemia, the survival of pyramidal cells, in the CA1 subfield, was respectively 91 and 96%, in the animals given rimonabant 0.25 and 0.5 mg kg−1, compared to the vehicle group. Higher doses were not protective.
The protection induced by rimonabant followed a bell-shaped curve, the maximal active doses being 0.25 and 0.5 mg kg−1.
Capsazepine (0.01 mg kg−1), a selective VR1 vanilloid receptor antagonist, completely reversed rimonabant-induced neuroprotective effects against EEG flattening, memory impairment and CA1 hippocampal neuronal loss.
These findings suggest that VR1 vanilloid receptors are involved in rimonabant's neuroprotection even if other mechanisms can contribute to this effect.
Keywords: SR 141716, vanilloid receptor, cannabinoid antagonist, global cerebral ischemia, EEG, memory, motor activity gerbil
Introduction
In addition to preventing the effects of cannabinoid agonists at CB1 cannabinoid receptor (Pertwee, 1997; 1999; Nakamura-Palacios et al., 1999), rimonabant has been previously shown to possess a number of biochemical and behavioral effects when administered alone. For example, at normal pharmacological doses (1–5 mg kg−1), rimonabant increases gastrointestinal motility and intestinal transit (Calignano et al., 1997; Colombo et al., 1998; Izzo et al., 1999), reduces food intake and enhances memory as well as produces conditioned place preference (reviewed in Chaperon & Thiebot, 1999). It is also effective in alleviating neuropathic pain in rats (Costa et al., 2005). At moderate to large doses (5–40 mg kg−1), it produces head twitching and scratching in rodents (Aceto et al., 1995; Cook et al., 1998; Rubino et al., 1998; Darmani & Pandya, 2000; Darmani et al., 2003) and vomiting in the least shrew (Cryptotis parva) (Darmani, 2001; Darmani et al., 2003). The mechanisms by which rimonabant produces these effects are not yet fully elucidated. Furthermore, Hansen et al. (2002) also has provided strong evidence for an intrinsic neuroprotective effect of rimonabant on NMDA-damaged neurons, not mediated by CB1 cannabinoid receptor activation. Rimonabant by itself attenuated the evoked release of [3H]glutamate from rodent hippocampal synaptosomes, suggesting a potential neuroprotective effect independent of the CB1 receptor (Kofalvi et al., 2003). In a rat stroke model, rimonabant, given 30 min after initiation of permanent middle cerebral artery occlusion, reduced infarct volume approximately of 40% (Berger et al., 2004).
Pathological changes in brain temperature or pH, for example after a severe stroke, may influence the transient receptor potential channel vanilloid subfamily member 1 (TRPV1), known as VR1 vanilloid receptor (Tominaga et al., 1998), suggesting an important role in events occurring after ischemia (like glutamate release and consequent activation of excitatory aminoacid receptors). VR1 vanilloid receptor can be activated by endogenously generated compounds such as anandamide and lipoxygenase products which accumulate during brain injury (Marinelli et al., 2002). In addition, VR1 is present in brain regions (hippocampus) that are highly susceptible to neurodegenerative insults, so this ion channel might contribute to the cellular processes involved in neuronal death (Mezey et al., 2000). The involvement of VR vanilloid receptor has been postulated in the protective effect of capsaicin (Veldhuis et al., 2003; Pegorini et al., 2005) in different ischemic models in rats and gerbils.
Rimonabant inhibits VR1-mediated effect of anandamide on cytosolic Ca2+ concentration, although at concentrations higher than those required for cannabinoid receptor CB1 antagonism (De Petrocellis et al., 2001).
The current study investigated the possible neuroprotective effect of rimonabant using a model of transient global cerebral ischemia in the gerbil. Capsazepine (CPZ), administered peripherally was used as vanilloid antagonist, to verify the role of VR1. To quantify the ischemic damage, from 1 h to 7 days after reperfusion we measured different parameters known to be influenced by global cerebral ischemia: electroencephalographic (EEG) spectral power, spontaneous motor activity, memory function and hippocampal CA1 neuronal count. We measured motor activity on day 1, since ischemia-induced hyperlocomotion is maximal 24 h after occlusion (Araki et al., 1986), memory function on day 3 according to Sala et al. (1997). Since the decrease in EEG has been related to pronounced damage of neurons on day 7 (Suzuki et al., 1983; Hunter et al., 1995; Peruche et al., 1995), EEG spectral power and neuronal counts were measured at this time.
Methods
Animals
Male Mongolian gerbils (Meriones unguiculatus) (Charles River, Calco, Como, Italy) weighing 60–80 g were housed singly in standard laboratory conditions: air-conditioned room (22±2°C), 12-h light/12-h dark light cycle, free access to food and water. The gerbils were allowed to acclimatize themselves to the environment for 1 week before surgical implantation of cortical electrodes. After implanting the EEG electrodes the gerbils were divided into different groups on the basis of the treatment assigned. Each animal received all tests.
All procedures were approved under Italian Governmental decree No. 32/2004.
Surgical procedure
Gerbils were anesthetised with an i.p. injection of chloral hydrate (450 mg kg−1, Sigma, St Louis, MO, U.S.A.) dissolved in saline and given in a volume of 9 ml kg−1. Four electrodes (Bilaney, Dusseldorf, Germany) were implanted for EEG recordings, as described elsewhere (Sala et al., 1997), on the right and left of the parieto-occipital cortex according to brain atlas coordinates (anterior +2, posterior –3, lateral 2, ventral 1.6 from bregma) (Loskota et al., 1974). Another electrode was inserted into the nasal bone as reference ground. The five electrodes were connected to a pedestal (Bilaney, Dusseldorf, Germany) and fixed with acrylic cement (Palavit, New Galetti and Rossi, Milan, Italy). The animals were allowed a week for recovery from surgery before starting the experiment.
EEG recording
Freely moving, awake gerbils were acclimatized in a sound-attenuated Faraday chamber, then their electroencephalogram (EEG) was recorded for 1 h a day, for 3 days, to determine the basal total and relative spectral power. Spectral powers between 0 and 25 Hz (0.2–4.0 Hz δ, 4.2–8.0 Hz ϑ, 8.2–13 Hz α, 13.2–25 Hz β) were evaluated using a resolution of 0.2 Hz. The signals were recorded and processed for fast Fourier transform spectral analysis by means of PC software (PowerLab, AD Instruments Pty Ltd, Australia). EEG recordings were also made during and 7 days after ischemia. Each 1-h spectral power was calculated as the mean of six 1-min recordings taken at 10-min intervals.
Cerebral ischemia
After basal EEG recordings, each gerbil was again lightly anesthetised with 2,2,2-tribromoethanol (200 mg kg−1, 10 ml kg−1 Sigma Aldrich, St Louis, MO, U.S.A.). Throughout surgery, body temperature was kept at 37°C with a heating lamp and 10-min ischemia was induced by bilateral common carotid arteries occlusion as previously described (Braida et al., 2000). The ischemia was verified qualitatively on paper by the complete flattening of the EEG. A group of animals (sham operated) underwent the same surgical procedure except that the carotid arteries were not clamped.
Locomotor activity
Spontaneous motor activity was evaluated as previously described (Braida et al., 2000) in an activity cage (43 cm long × 43 cm wide × 32 cm high: Ugo Basile, Varese, Italy), placed in a sound-attenuating room. The cage was fitted with two parallel horizontal infrared beams 2 cm off the floor. Cumulative horizontal movements were counted every 5 min for 30 min, 1 day after ischemia.
Passive avoidance task
On the 3rd day after ischemia each gerbil was examined in the passive avoidance task. The apparatus (Ugo Basile, Varese, Italy) consisted of a box divided by a guillotine door into two compartments of the same size (22 cm long × 22 cm wide × 21 cm high) in which the floor was a stainless rod grid. One compartment was lit with a 10 W electric light bulb, while the other was dark. The step-through-type passive avoidance task was used, as described by Katoh et al. (1992), with some modifications. Animals were allowed to adapt for 10 min before the training, and retention was checked 1 day after the training. For the adaptation a gerbil was placed in the light compartment, and allowed to explore both compartments by leaving the guillotine door open for 5 min. After 10 min, training started during which each gerbil was placed in the light compartment and allowed to enter the dark. When the gerbil entered the dark compartment, the door automatically closed and an unavoidable scrambled foot shock (1.5 mA) was delivered for 5 s. Each gerbil was then allowed to stay there for 10 s. The procedure was immediately repeated twice. For the retention test, gerbils were placed in the light compartment and the latency to re-enter the dark compartment was recorded for up to 180 s.
Histology
At 7 days after the ischemic injury, all the gerbils were anesthetized with an overdose of chloral hydrate 5% and transcardially perfused with 4% paraformaldehyde (Sigma Aldrich, St Louis, MO, U.S.A.) for histological determination, as previously described (Braida et al., 2003). Brains were removed and placed in the same fixative overnight, then embedded in paraffin wax. Five serial 5-μm coronal hippocampal sections were cut at 1.5, 1.7 and 1.9 mm caudal to the bregma, using a microtome (Leica, Mod. RM2125RT, Solms, Germany), and stained with cresyl violet (Sigma Aldrich, St Louis, MO, U.S.A.). Neurons with a normal appearance in the pyramidal cell layer of the CA1 sector were counted blind (from coded slides) in each section for each group.
Treatment
Gerbils submitted to ischemia were divided into 10 groups of five animals each, receiving acutely: vehicle s.c.+vehicle i.p.; vehicle s.c.+rimonabant (0.05, 0.125, 0.25, 0.5, 1 and 3 mg kg−1 i.p.), (a kind gift from Sanofi Aventis, Montpellier, France); CPZ (0.01 mg kg−1 s.c.) (Tocris Cookson Ltd, U.K.)+vehicle i.p.; CPZ (0.01 mg kg−1 s.c.)+rimonabant (0.05, 0.125, 0.25, 0.5, 1 and 3 mg kg−1 i.p.). CPZ was given 15 min before bilateral carotid occlusion and rimonabant was injected 5 min after recirculation. Vehicle was given 5 min before or 15 min after ischemia, either s.c. or i.p. Both drugs were dissolved in an appropriate vehicle (Tween-80, ethanol, saline, 1 : 1 : 8 for CPZ and cremophor, ethanol, saline 1 : 1 : 18 for rimonabant) and injected in a volume of 5 ml kg−1 s.c. and i.p. The sham-operated group received the same volume of vehicle.
Statistical analysis
Data were presented as mean (±s.e.m.). Vehicle groups (s.c. and i.p) were pooled for analysis. Total EEG spectral data were expressed as the mean percentage difference from the preischemic value, and relative power as a percentage of the total. EEG, motor activity, latency time, and neuronal counts were analyzed by one-way ANOVA for multiple comparisons, followed by Tukey's or Student's t-test. The accepted level of significance was P<0.05. All statistical analyses were done using Prism version 4 software (GraphPad, U.S.A.).
Results
Physiological parameters – food and water consumption and body weight – were stable throughout the study in all groups (data not shown). Only animals treated with 3 mg kg−1 showed a decrease of body weight (−20%) and a lethality of 20%.
EEG
A quantitative EEG analysis of gerbils treated with increasing doses of rimonabant is given in Figure 1. On day 7 there was a significant overall group effect, in terms of the percentages of preischemic mean total spectral power (F[12,52]=23.32 P<0.0001, ANOVA). Post hoc analysis showed that, in comparison with sham-operated values, the vehicle group had an 84% decrease in EEG power. Rimonabant significantly antagonized the ischemia-induced EEG flattening at doses of 0.25 and 0.5 mg kg−1. Higher doses (1 and 3 mg kg−1) were ineffective. CPZ per se (0.01 mg kg−1) did not cause any change in comparison with the vehicle group (data not shown). This dose was therefore chosen to study the antagonism. Pretreatment with CPZ significantly antagonized the protective effect of rimonabant alone at the doses of 0.25 and 0.5 mg kg−1.
Figure 1.
Cortically derived EEG total spectral power on day 7 after recirculation, as the difference (Δ%) from the preischemic value in freely moving, awake gerbils given increasing doses (mg kg−1) of rimonabant, 5 min after recirculation, either alone or with capsazepine (CPZ) (0.01 mg kg−1) s.c. 15 min before bilateral carotid occlusion. Each column represents the mean (±s.e.m.) of five animals. aP<0.05, bP<0.01, cP<0.001 compared with sham-operated animals; dP<0.001 compared with vehicle; eP<0.02 compared with rimonabant alone (one-way ANOVA followed by Tukey's test).
There was a treatment effect in the relative distribution of power over frequency bands (F[12,52]=10.48, P<0.0001, ANOVA for δ) (F[12,52]=9.60, P<0.0001, ANOVA for ϑ) (F[12,52]=5.80, P<0.0001, ANOVA for α) (F[12,52]=1.90, <0.05, ANOVA for β) 7 days after recirculation. Post hoc analysis indicated that ischemia significantly increased the relative EEG power density in the δ band, and reduced the ϑ and α frequency bands in the vehicle-treated group (Table 1). All the rimonabant doses significantly restored the power density except 3 mg kg−1. Rimonabant increased the β frequency band, though not significantly, starting from 0.125 until 0.5 mg kg−1. No differences were found between vehicle- and CPZ-treated gerbils. The dose of 3 mg kg−1 significantly decreased α frequency band in comparison with sham, vehicle and CPZ alone groups.
Table 1.
Effect of rimonabant and capsazepine on spectral power distribution evaluated 7 days after ischemia, in gerbils
| Drug dose (mg kg−1) | δ (0.2–4.0 Hz) | ϑ (4.2–8.0 Hz) | α (8.2–13 Hz) | β (13.2–25Hz) |
|---|---|---|---|---|
| Sham | 45.00±3.00 | 44.00±2.00 | 10.00±0.40 | 1.00±0.30 |
| Vehiclea | 62.00±2.00** | 32.00±2.20** | 5.00±1.70** | 1.50±0.50 |
| Rimonabant (0.05)b | 40.79±4.64$$ | 50.50±2.93$$$ | 8.50±1.50 | 0.75±0.05 |
| Rimonabant (0.125)b | 39.15±2.14$$ | 46.86±1.57$ | 12.35±1.47$$ | 1.80±0.37 |
| Rimonabant (0.25)b | 37.60±1.15$$$ | 49.60±1.15$$ | 11.20±1.15$$$ | 2.20±1.17 |
| Rimonabant (0.5)b | 38.33±2.18$$ | 45.33±1.20$ | 13.33±0.88$$ | 2.66±1.20 |
| Rimonabant (1) | 41.67±3.18$$ | 49.00±1.73$$$ | 8.67±1.20 | 1.00±0.50 |
| Rimonabant (3) | 71.67±3.69** | 26.67±3.66** | 0.83±0.17***,$ | 0.50±0.01 |
| Capsazepine (0.01) | 63.00±1.00** | 31.00±2.50** | 5.00±1.50** | 1.00±0.50 |
| Capsazepine (0.01)c+Rimonabant (0.05) | 36.00±1.0$$$ | 48.00±1.0$$ | 15.50±0.3**,$$ | 0.50±0.20 |
| Capsazepine (0.01)c+Rimonabant (0.125) | 37.50±2.50$$ | 52.50±1.5$$$ | 9.50±3.50 | 0.75±0.25# |
| Capsazepine (0.01)c+Rimonabant (0.25) | 47.00±9.50 | 44.00±5.6 | 9.00±3.80 | 0.70±0.20### |
| Capsazepine (0.01)c+Rimonabant (0.5) | 37.50±2.5$$ | 50.50±3.5$$$ | 11.50±0.50$$ | 0.75±0.25### |
Vehicle was given 15 min before carotid occlusion or 5 min after recirculation.
Rimonabant was administered i.p. 5 min after recirculation.
Capsazepine was injected s.c. 15 min before carotid occlusion. Each value represents mean (±s.e.m.) of five animals.
P<0.01 compared with sham-operated group;
P<0.05,
P<0.01,
P<0.001 compared with the vehicle group and CPZ alone;
P<0.05,
##P<0.01,
P<0.001 compared with rimonabant, alone (ANOVA followed by Tukey's test).
Treatment with the VR1 vanilloid receptor antagonist did not change the power spectral distribution obtained with rimonabant alone at all tested doses. However, in comparison with rimonabant alone, there was a significant decrease in the relative spectral power of the β band starting from the dose of 0.125 mg kg−1.
Spontaneous locomotor activity
There were significant between-group changes in spontaneous locomotor activity 1 day after recirculation (F[12,52]=10.09, P<0.0001, ANOVA) (Figure 2). As expected, the vehicle group showed a motor increase compared to the sham-operated group (Tukey's test). Post hoc Tukey's test showed that rimonabant completely antagonized ischemia-induced hyperlocomotion at all doses except the lowest and the two higher. CPZ (0.01 mg kg−1), which per se did not affect ischemia-induced hyperlocomotion (data not shown), did not reverse the protective effect of rimonabant.
Figure 2.
Effect of increasing doses (mg kg−1) of rimonabant given s.c. 5 min after recirculation either alone or with capsazepine (CPZ) 0.01 mg kg−1 s.c. 15 min before bilateral carotid occlusion, on spontaneous motor activity evaluated for 30 min, 1 day after ischemia in gerbils. Each column represents the total horizontal counts (mean±s.e.m.) of five animals. aP<0.01, bP<0.001 compared with sham-operated animals; cP<0.01, dP<0.001 compared with vehicle; eP<0.001 compared with rimonabant alone (one-way ANOVA followed by Tukey's test).
Passive avoidance
The mean latency measured 3 days after recirculation differed significantly between groups (F[12,52]=9.327, P<0.0001, ANOVA) (Figure 3). Post hoc analysis indicated that vehicle-treated gerbils suffered significant impairment, as shown by the decrease in mean escape latency in comparison with the sham-operated group. Rimonabant improved memory deficit only at 0.25 and 0.5 mg kg−1. When CPZ was given in combination with rimonabant (0.25 and 0.5 mg kg−1) complete antagonism was obtained (Tukey's test). CPZ alone did not affect the ischemia-induced mean escape latency (data not shown).
Figure 3.
Mean (±s.e.m.) escape latency in the passive avoidance task 3 days after ischemia. Increasing doses (mg kg−1) of rimonabant were given s.c. 5 min after recirculation either alone or with capsazepine (CPZ) (0.01 mg kg−1) s.c. 15 min before bilateral carotid occlusion. Each column represents the mean (±s.e.m.) of five animals. aP<0.01, bP<0.001 compared with sham-operated animals; cP<0.001 compared with vehicle; dP<0.05, eP<0.01 compared with rimonabant alone (one-way ANOVA followed by Tukey's test).
Histology
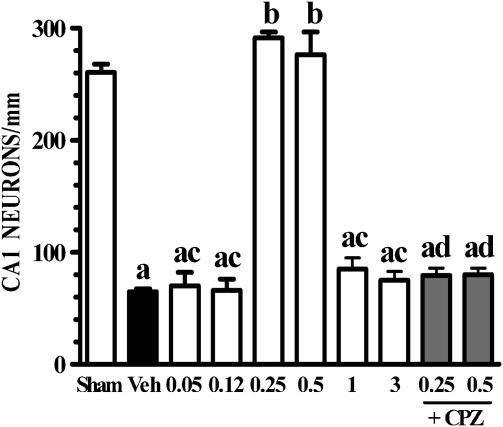
At 7 days after 10-min ischemia a difference was found in the number of surviving neurons in the CA1 region (F[5,24]=256.30, P<0.0001, ANOVA) (Figures 4 and 5). Histological examination of the hippocampus showed a mean loss of 80% of neuronal cells in vehicle-treated gerbils in comparison with the sham-operated group. Survival in the animals given rimonabant 0.25 and 0.5 mg kg−1 was, respectively, 91 and 96%, compared to the vehicle group. Pretreatment with CPZ significantly antagonized rimonabant's neuroprotective effect. CPZ per se caused a mean loss of neuronal cells similar to vehicle (data not shown).
Figure 4.
Photomicrographs of the hippocampal CA1 region of gerbils with or without 10-min ischemia, 7 days after recirculation. (a) CA1 hippocampal region. (b) Sham-operated animal. (c) Ischemic animal treated with vehicle, 5 min after recirculation. (d) Ischemic animal treated with CPZ. (e–h) Capsazepine was given 5 min before bilateral carotid occlusion and rimonabant 5 min after recirculation. Doses are mg kg−1. Bar=25 μm.
Figure 5.
Effect of increasing doses of rimonabant (mg kg−1) on neuronal counts 7 days after reperfusion in the CA1 region of the hippocampus of sham-operated or ischemic gerbils. Rimonabant was given i.p. 5 min after recirculation either alone or with capsazepine (CPZ) (0.01 mg kg−1) s.c. 15 min before bilateral carotid arteries occlusion. Each column represents the mean (±s.e.m.) of five hippocampal sections from the same coronal plane for each animal. n=5 for each group. aP<0.001 compared with sham-operated animals; bP<0.001 compared with vehicle; cP<0.001 compared with rimonabant 0.25 and 0.5 mg kg–1; dP<0.001 compared with corresponding rimonabant alone (one-way ANOVA followed by Tukey's test).
Discussion
The main finding of the present study was that postischemic treatment with the CB1 cannabinoid receptor antagonist, rimonabant, facilitated neuroprotection, quantified in terms of complete recovery of total and relative spectral power, spontaneous motor activity, memory function and hippocampal CA1 neuronal density.
EEG and behavioral findings followed a bell-shaped curve, the dose of 0.25 and 0.5 mg kg−1 being protective and the higher being ineffective. A similar trend has been also observed after treatment with some exogenous cannabinoids (including anandamide) for ambulation, defecation and analgesia (Sulcova et al., 1998) neuroprotective (Braida et al., 2003) and rewarding effects (Braida et al., 2004) and also for the head twitch and scratching induced by rimonabant itself (Darmani et al., 2003). The involvement of more than one receptor cannot be excluded to explain the observed biphasic effect. However, the exact mechanism is still to be elucidated.
Some cognitive and sensorimotor deficits have been seen in several human pathologies (heart attack and coronary artery bypass surgery) (Hunter et al., 1998) similar to those observed in our gerbils submitted to global cerebral ischemia and in other reports (Suzuki et al., 1983; Araki et al., 1986; Hunter et al., 1995; Peruche et al., 1995; Sala et al., 1997). Furthermore, the histopathology in the gerbil is similar to that in the hippocampal CA1 region of human brain after cardiac arrest (Hunter et al., 1995).
Rimonabant prevented ischemia-induced damage, evaluated from the EEG, memory and histology, at doses of 0.25 and 0.5 mg kg−1, with hyperlocomotion starting from 0.125 mg kg−1. Higher doses (1 and 3 mg kg−1) were ineffective in all the parameters. In addition, the dose as 3 mg kg−1 decreased body weight and increased lethality suggesting some degree of toxicity of the drug in this species.
The observed protection indicates that the compound may contrast the cascade of pathological events that lead to neuronal death. Hippocampal CA1 is the most selectively vulnerable sector to reduced cerebral blood flow (Schmidt-Kastner & Freund, 1991). The survival of CA1 neurons 7 days after ischemia with rimonabant (0.25 and 0.5 mg kg−1) may explain the protection against EEG flattening, which has been related to severe neuronal damage (Peruche et al., 1995).
There was an increase in the relative power of the δ band in vehicle-treated gerbils, which can be interpreted as a sign of synchronization of neuronal activity (Frigeni et al., 2001). In contrast, ϑ and α frequency bands decreased. Similar EEG changes have been reported for different kinds of focal brain ischemia in different animal species (Gloor et al., 1977; Hossmann & Schuier, 1980; Kataoka et al., 1987). Rimonabant, at all the tested doses, except the highest, caused a significant recovery of the spectral power distribution toward basal values, suggesting recovery of neuronal activity. The cannabinoid antagonist increased the β frequency band, though not significantly. This might reflect the fact that rimonabant per se increased the time spent in wakefulness in freely moving rats (Santucci et al., 1996).
The protection against motor hyperactivity in rimonabant-treated gerbils suggests that the compound reversed the ischemia-induced inability to form spatial maps (O'Neill & Clemens, 2000) because of the loss of CA1 neurons. We can exclude any stimulating effect of rimonabant, as shown by Compton et al. (1996), since the evaluation was carried out 24 h after treatment.
Rimonabant prevented ischemia-induced memory impairment, since it promoted a survival of CA1 pyramidal cells, the most vulnerable to hypoxic insult and involved in learning and memory function (LaPoncin-Lafitte et al., 1981; Kiyota et al., 1985). This memory disturbance has been clinically demonstrated during cardiac arrest as revealed by an amnesic syndrome characterized by impaired learning and memory of events after the injury (Volpe & Hirst, 1983).
In agreement with our findings, showing a protective effect of rimonabant, there was a significant reduction of infarct size in rat pups, pretreated with rimonabant, in response to NMDA receptor-induced neurotoxicity (Hansen et al., 2002). Rimonabant also attenuated the evoked [3H]glutamate release from rodent hippocampal synaptosomes with a mechanism independent of the CB1 receptor (Kofalvi et al., 2003). Berger et al. (2004) showed that treatment with rimonabant, 30 min after permanent middle cerebral artery occlusion, had no significant effect on glutamate release or anandamide levels but reduced infarct volume at 5 h by approximately 40%, suggesting a mechanism other than the activation of cannabinoid receptors. Rimonabant appears to have also its own signalling potential in that it stimulates ERK phosphorylation and, to a lesser degree, AP-1 activity (Berdyshev et al., 2001). ERK activation is a crucial common pathway in the initial stages of stroke pathophysiology regulating cell survival or death.
Pretreatment with CPZ reversed the protective effects of rimonabant, suggesting an involvement of the VR1 receptor in neuroprotection against ischemic damage. The fact that CPZ did not completely reverse the protective effect of rimonabant on spontaneous motor activity and spectral power distribution, may be attributed to the employed low dose.
Endogenously generated compounds such as anandamide and lipoxygenase products which accumulate during brain injury (Marinelli et al., 2002) have been found to activate both VR1 vanilloid and CB1 cannabinoid receptors (Zygmunt et al., 1999; De Petrocellis et al., 2001; Hermann et al., 2003) (even if with different affinity). Both receptors are coexpressed in brain areas including hippocampus which is highly susceptible to neurodegenerative insults (Mezey et al., 2000).
We suggested that, in presence of rimonabant, which blocks CB1 cannabinoid receptors as antagonist (Rinaldi-Carmona et al., 1994), the increased N-acylethanolamines, including anandamide, can activate and quickly desensitize VR1 receptors, as already suggested by Veldhuis et al. (2003). This study shows that arvanil, a synthetic AEA analog, attenuated excitotoxic brain injury and cotreatment of arvanil with CPZ reduced the neuroprotective effect of arvanil, indicative of VR1-mediated neuroprotection. However, it is worthy to note that Veldhuis et al. (2003) also showed that CPZ alone reduced brain injury caused by excitotoxicity. This neuroprotective action of CPZ may imply VR1-mediated neurotoxicity, arguing against a VR1-mediated neuroprotection, although the neuroprotection of CPZ is not always via an action on VR1 (Ray et al., 2003). This apparent discrepancy (neurotoxicity versus neuroprotection) is probably a result of the use of different experimental conditions as proposed by Kim et al. (2005).
Alternatively rimonabant might act as a partial and weak agonist and, subsequently, as a competitive antagonist for VR1 receptors (De Petrocellis et al., 2001). However, it seems unlikely since rimonabant activates VR1 receptors at least in vitro at concentrations >5 μM against >1 μM to activate CB1 receptors (De Petrocellis et al., 2001). Anandamide has been also shown to directly inhibit T-type calcium channels (Chemin et al., 2001), preventing neuronal damage.
Finally, we cannot exclude the possibility that rimonabant acts on glutamate release with a mechanism independent from CB1 cannabinoid receptor, as reported in vitro in hippocampal synaptosomes of rats and mice by Kofalvi et al. (2003).
A further explanation for the neuroprotection operated by rimonabant may be the presence, in the CNS, of an as yet undefined CBn/VRn receptor, sensitive also to capsaicin, anandamide, arvanil as already suggested by different authors (Brooks et al., 2002; Hajos & Freund, 2002; Veldhuis et al., 2003; Pegorini et al., 2005).
In conclusion, the present data support a potential therapeutic effect of rimonabant as an anti-ischemic drug, as shown by its ability to antagonize ischemia-induced EEG flattening, hyperlocomotion, memory impairment, and CA1 hippocampal neuronal loss, when given 5 min after recirculation. This effect was inhibited by CPZ, suggesting that the block operated by CB1 cannabinoid receptor may promote activation of VR1 receptors by endogenously generated compounds such as anandamide and lipoxygenase products with subsequent desensitization.
Acknowledgments
This research was supported by a Grant (FIRST 2003) from the Ministry of Scientific Research and Technology to M.S.
Abbreviations
- ANOVA
analysis of variance
- CNS
central nervous system
- CPZ
capsazepine
- EEG
electroencephalographic
- TRPV1
transient receptor potential channel vanilloid subfamily member 1
- VR1
vanilloid receptor
References
- ACETO M.D., SCATES S.M., LOWE J.A., MARTIN B.R. Cannabinoid precipitated withdrawal by the selective cannabinoid receptor antagonist, SR 141716A. Eur. J. Pharmacol. 1995;282:R1–R2. doi: 10.1016/0014-2999(95)00447-s. [DOI] [PubMed] [Google Scholar]
- ARAKI H., NOJIRI M., KAWASHIMA K., KIMURA M., AIHARA H. Behavioral, electroencephalographic and histopathological studies on Mongolian gerbils with occluded common carotid arteries. Physiol. Behav. 1986;38:89–94. doi: 10.1016/0031-9384(86)90136-8. [DOI] [PubMed] [Google Scholar]
- BERDYSHEV E.V., SCHMID P.C., KREBSBACH R.J., HILLARD C.J., HUANG C., CHEN N., DONG Z., SCHMID H.H.O. Cannabinoid receptor cell signalling by N-acylethanolamines. Biochem. J. 2001;360:67–75. doi: 10.1042/0264-6021:3600067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BERGER C., SCHMID P.C., SCHABITZ W.R., WOLF M., SCHWAB S., SCHMID H.H. Massive accumulation of N-acylethanolamines after stroke. Cell signalling in acute cerebral ischemia. J. Neurochem. 2004;88:1159–1167. doi: 10.1046/j.1471-4159.2003.02244.x. [DOI] [PubMed] [Google Scholar]
- BRAIDA D., POZZI M., SALA M. CP 55,940 protects against ischemia-induced electroencephalographic flattening and hyperlocomotion in Mongolian gerbils. Neurosci. Lett. 2000;296:69–72. doi: 10.1016/s0304-3940(00)01634-7. [DOI] [PubMed] [Google Scholar]
- BRAIDA D., PEGORINI S., ARCIDIACONO M.V., CONSALEZ G.G., CROCI L., SALA M. Post-ischemic treatment with cannabidiol prevents electro-encephalographic flattening, hyperlocomotion and neuronal injury in gerbils. Neurosci. Lett. 2003;346:61–64. doi: 10.1016/s0304-3940(03)00569-x. [DOI] [PubMed] [Google Scholar]
- BRAIDA D., IOSUÈ S., PEGORINI S., SALA M. Δ9-tetrahydrocannabinol-induced conditioned place preference and intracerebroventricular self-administration in rats. Eur. J. Pharmacol. 2004;506:63–69. doi: 10.1016/j.ejphar.2004.10.043. [DOI] [PubMed] [Google Scholar]
- BROOKS J.W., PRYCE G., BISOGNO T., JAGGAR S.I., HANKEY D.J., BROWN P., BRIDGES D., LEDENT C., BIFULCO M., RICE A.S., DI MARZO V., BAKER D. Arvanil-induced inhibition of spasticity and persistent pain: evidence for therapeutic sites of action different from the vanilloid VR1 receptor and cannabinoid CB(1)/CB(2) receptors. Eur. J. Pharmacol. 2002;439:83–92. doi: 10.1016/s0014-2999(02)01369-9. [DOI] [PubMed] [Google Scholar]
- CALIGNANO A., LA RANA G., MAKRIYANNIS A., LIN S.Y., BELTRAMO M., PIOMELLI D. Inhibition of intestinal motility by anandamide, an endogenous cannabinoid. Eur. J. Pharmacol. 1997;340:R7–R8. [PubMed] [Google Scholar]
- CHAPERON F., THIEBOT M.H. Behavioral effects of cannabinoid agents in animals. Crit. Rev. Neurobiol. 1999;13:243–281. doi: 10.1615/critrevneurobiol.v13.i3.20. [DOI] [PubMed] [Google Scholar]
- CHEMIN J., MONTEIL A., PEREZ-REYES E., NARGEOT J., LORY P. Direct inhibition of T-type calcium channels by the endogenous cannabinoid anandamide. EMBO J. 2001;20:7033–7040. doi: 10.1093/emboj/20.24.7033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COLOMBO G., AGABIO R., LOBINA C., REALI R., GESSA G.L. Cannabinoid modulation of intestinal propulsion in mice. Eur. J. Pharmacol. 1998;344:67–69. doi: 10.1016/s0014-2999(97)01555-0. [DOI] [PubMed] [Google Scholar]
- COMPTON D.R., ACETO M.D., LOWE J., MARTIN B.R. In vivo characterization of a specific cannabinoid receptor antagonist (SR141716A): inhibition of Δ9-tetrahydrocannabinol-induced responses and apparent agonist activity. J. Pharmacol. Exp. Ther. 1996;277:586–594. [PubMed] [Google Scholar]
- COOK S.A., LOWE J.A., MARTIN B.R. CB1 receptor antagonist precipitates withdrawal in mice exposed to Delta9-tetrahydrocannabinol. J. Pharmacol, Exp. Ther. 1998;285:1150–1156. [PubMed] [Google Scholar]
- COSTA B., TROVATO A.E., COLLEONI M., GIAGNONI G., ZARINI E., CROCI T. Effect of the cannabinoid CB1 receptor antagonist, SR141716, on nociceptive response and nerve demyelination in rodents with chronic constriction injury of the sciatic nerve. Pain. 2005;116:52–61. doi: 10.1016/j.pain.2005.03.043. [DOI] [PubMed] [Google Scholar]
- DARMANI N.A. Δ9-tetrahydrocannabinol and synthetic cannabinoids prevent emesis produced by the cannabinoid CB(1) receptor antagonist/inverse agonist SR 141716A. Neuropsychopharmacology. 2001;24:198–203. doi: 10.1016/S0893-133X(00)00197-4. [DOI] [PubMed] [Google Scholar]
- DARMANI N.A., JANOYAN J.J., KUMAR N., CRIM J.L. Behaviorally active doses of the CB1 receptor antagonist SR 141716A increase brain serotonin and dopamine levels and turnover. Pharmacol. Biochem. Behav. 2003;75:777–787. doi: 10.1016/s0091-3057(03)00150-3. [DOI] [PubMed] [Google Scholar]
- DARMANI N.A., PANDYA D.K. Involvement of other neurotransmitters in behaviors induced by the cannabinoid CB1 receptor antagonist SR 141716A in naive mice. J. Neural Transm. 2000;107:931–945. doi: 10.1007/s007020070043. [DOI] [PubMed] [Google Scholar]
- DE PETROCELLIS L., BISOGNO T., MACCARRONE M., DAVIS J.B., FINAZZI-AGRÒ A., DI MARZO V. The activity of anandamide at vanilloid VR1 receptors requires facilitated transport across the cell membrane and is limited by intracellular metabolism. J. Biol. Chem. 2001;276:12856–12863. doi: 10.1074/jbc.M008555200. [DOI] [PubMed] [Google Scholar]
- FRIGENI V., MIRAGOLI L., GROTTI A., LORUSSO V. Neurotolerability of contrast agents in rats with brain ischemia induced by transient middle cerebral artery occlusion: EEG evaluation. Invest. Radiol. 2001;36:1–8. doi: 10.1097/00004424-200101000-00001. [DOI] [PubMed] [Google Scholar]
- GLOOR P., BALL G., SCHAUL N. Brain lesions that produce delta waves in the EEG. Neurology. 1977;27:326–333. doi: 10.1212/wnl.27.4.326. [DOI] [PubMed] [Google Scholar]
- HAJOS N., FREUND T.F. Pharmacological separation of cannabinoid sensitive receptors on hippocampal excitatory and inhibitory fibers. Neuropharmacology. 2002;43:503–510. doi: 10.1016/s0028-3908(02)00157-0. [DOI] [PubMed] [Google Scholar]
- HANSEN H.H., AZCOITIA I., PONS S., ROMERO J., GARCIA-SEGURA L.M., RAMOS J.A., HANSEN H.S., FERNANDEZ-RUIZ J. Blockade of cannabinoid CB (1) receptor function protects against in vivo disseminating brain damage following NMDA-induced excitotoxicity. J. Neurochem. 2002;82:154–158. doi: 10.1046/j.1471-4159.2002.00961.x. [DOI] [PubMed] [Google Scholar]
- HERMANN H., DE PETROCELLIS L., BISOGNO T., SCHIANO MORIELLO A., LUTZ B., DI MARZO V. Dual effect of cannabinoid CB1 receptor stimulation on a vanilloid VR1 receptor-mediated response. Cell. Mol. Life Sci. 2003;60:607–616. doi: 10.1007/s000180300052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOSSMANN K.A., SCHUIER F.J. Experimental brain infarcts in cats. Stroke. 1980;11:583–592. doi: 10.1161/01.str.11.6.583. [DOI] [PubMed] [Google Scholar]
- HUNTER A.J., GREEN A.R., CROSS A.J. Animal models of acute ischaemic stroke: can they predict clinically successful neuroprotective drugs. TiPS. 1995;16:123–128. doi: 10.1016/s0165-6147(00)88999-3. [DOI] [PubMed] [Google Scholar]
- HUNTER A.J., MACKAY K.B., ROGERS D.C. To what extent have functional studies of ischaemia in animals been useful in the assessment of potential neuroprotective agents. TiPS. 1998;19:59–66. doi: 10.1016/s0165-6147(97)01157-7. [DOI] [PubMed] [Google Scholar]
- IZZO A.A., MASCOLO N., BORRELLI F., CAPASSO F. Defecation, intestinal fluid accumulation and motility in rodents: implications of cannabinoid CB1 receptors. Naunyn Schmiedebergs Arch Pharmacol. 1999;359:65–70. doi: 10.1007/pl00005325. [DOI] [PubMed] [Google Scholar]
- KATAOKA K., GRAF R., ROSNER G. Differentiation between cortical and subcortical lesions following focal ischemia in cats by multimodality evoked potentials. J. Neurol. Sci. 1987;79:117–127. doi: 10.1016/0022-510x(87)90266-8. [DOI] [PubMed] [Google Scholar]
- KATOH A., ISHIBASHI C., SHIOMI T., TAKAHARA Y., EIGYO M. Ischemia-induced irreversible deficit of memory function in gerbils. Brain Res. 1992;577:57–63. doi: 10.1016/0006-8993(92)90537-j. [DOI] [PubMed] [Google Scholar]
- KIM S.R., LEE D.Y., CHUNG E.S., OH U.T., KIM S.E., JIN B.K. Transient receptor potential vanilloid subtype 1 mediates cell death of mesencephalic dopaminergic neurons in vivo and in vitro. J. Neurosci. 2005;19:662–671. doi: 10.1523/JNEUROSCI.4166-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KIYOTA Y., HAMAJO K., MIYAMOTO M., NAGAOKA M. Effect of idebenone (CV-2619) on memory impairment observed in passive avoidance task in rats with cerebral embolization. Jpn. J. Pharmacol. 1985;37:300–302. doi: 10.1254/jjp.37.300. [DOI] [PubMed] [Google Scholar]
- KOFALVI A., VIZI E.S., LEDENT C., SPERLAGH B. Cannabinoids inhibit the release of [3 H] glutamate from rodent hippocampal synaptosomes via a novel CB1 receptor-independent action. Eur. J. Neurosci. 2003;18:1973–1978. doi: 10.1046/j.1460-9568.2003.02897.x. [DOI] [PubMed] [Google Scholar]
- LAPONCIN-LAFITTE M., GROSDEMOUGE C., BILLON C.R., DUTERTE D., PONTRAT P., LESINASSE P., RAPIN J.R. Short-term memory and cerebral ischemia: pharmacological application. Eur. J. Neurol. 1981;20:265–269. doi: 10.1159/000115245. [DOI] [PubMed] [Google Scholar]
- LOSKOTA W.J., LOMAX P.L., VERITY M.A. A stereotaxic atlas of the Mongolian gerbil (Meriones unguiculatus) Ann Arbor: Ann Arbor Science Publishers; 1974. pp. 1–157. [Google Scholar]
- MARINELLI S., VAUGHAN C.W., CHRISTIE M.J., CONNOR M. Capsaicin activation of glutamatergic synaptic transmission in the rat locus coeruleus in vitro. J. Physiol. 2002;543:531–540. doi: 10.1113/jphysiol.2002.022863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MEZEY E., TOTH Z.E., CORTRIGHT D.N., ARZUBI M.K., KRAUSE J.E., ELDE R., GUO A., BLUMBERG P.M., SZALLASI A. Distribution of mRNA for vanilloid receptor subtype 1 (VR1), and VR1 -like immunoreactivity, in the central nervous system of the rat and human. Proc. Natl. Acad. Sci. U.S.A. 2000;97:3655–3660. doi: 10.1073/pnas.060496197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAKAMURA-PALACIOS E.M., MOERSCHBAEKER J.M., BARKER L.A. The pharmacology of SR 141716A: a review. CNS Drug Rev. 1999;5:43–58. [Google Scholar]
- O'NEILL M.J., CLEMENS J.A.Preclinical models of neurologic and psychiatric disorders Current Protocols in Neuroscience 2000New York: Wiley; ed. Crawley, J.N., Gerfen, C.R., Mckay, R., Rogawski, M.A, Sibley, D.R., & Skolnick, P., pp. 9.5.1–9.5.2.5 [Google Scholar]
- PEGORINI S., BRAIDA D., VERZONI C., GUERINI-ROCCO C., CONSALEZ G.G., CROCI L., SALA M. Capsaicin exhibits neuroprotective effects in a model of transient global cerebral ischemia in Mongolian gerbils. Br. J. Pharmacol. 2005;144:727–735. doi: 10.1038/sj.bjp.0706115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PERTWEE R.G. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol. Ther. 1997;74:129–180. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- PERTWEE R.G. Cannabis and cannabinoids: pharmacology and rationale for clinical use. Forsch. Komplementarmed. 1999;3:12–15. doi: 10.1159/000057150. [DOI] [PubMed] [Google Scholar]
- PERUCHE B., KLAASSENS H., KRIEGLSTEIN J. Quantitative analysis of the electrocorticogram after forebrain ischemia in the rat. Pharmacology. 1995;50:229–237. doi: 10.1159/000139287. [DOI] [PubMed] [Google Scholar]
- RAY A.M., BENHAM C.D., ROBERTS J.C., GILL C.H., LANNEAU C., GITTERMAN D.P., HARRIES M., DAVIS J.B., DAVIES C.H. Capsazepine protects against neuronal injury caused by oxygen glucose deprivation by inhibiting I(h) J. Neurosci. 2003;23:10146–10153. doi: 10.1523/JNEUROSCI.23-31-10146.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RINALDI-CARMONA M., BARTH F., HEAULME M., SHIRE D., CALANDRA B., CONGY C., MARTINEZ S., MARUANI J., NELIAT G., CAPUT D., FERRARA P, SOUBRIÉ P, BRELIERE J.C., LE FUR G. SR141716A, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett. 1994;350:240–244. doi: 10.1016/0014-5793(94)00773-x. [DOI] [PubMed] [Google Scholar]
- RUBINO T., PATRINI G., MASSI P., FUZIO D., VIGANO D., GIAGNONI G., PAROLARO D. Cannabinoid-precipitated withdrawal: a time-course study of the behavioral aspect and its correlation with cannabinoid receptors and G protein expression. J. Pharmacol. Exp. Ther. 1998;285:813–819. [PubMed] [Google Scholar]
- SALA M., LEONE M.P., LAMPUGNANI P., MATTURRI L., GORI E. Polydeoxyribonucleotide (defibrotide) protects against post-ischemic behavioral, electroencephalographic and neuronal damage in the gerbil. Eur. J. Pharmacol. 1997;328:143–152. doi: 10.1016/s0014-2999(97)83040-3. [DOI] [PubMed] [Google Scholar]
- SANTUCCI V., STORME J.J., SOUBRIÉ P., LE FUR G. Arousal-enhancing properties of the CB1 cannabinoid receptor antagonist SR 141716A in rats as assessed by electroencephalographic spectral and sleep-waking cycle analysis. Life Sci. 1996;58:103–110. doi: 10.1016/0024-3205(95)02319-4. [DOI] [PubMed] [Google Scholar]
- SCHMIDT-KASTNER R., FREUND T.F. Selective vulnerability of the hippocampus in brain ischemia. Neuroscience. 1991;40:599–636. doi: 10.1016/0306-4522(91)90001-5. [DOI] [PubMed] [Google Scholar]
- SULCOVA E., MECHOULAM R., FRIDE E. Biphasic effects of anandamide. Pharmacol. Biochem. Be. 1998;59:347–352. doi: 10.1016/s0091-3057(97)00422-x. [DOI] [PubMed] [Google Scholar]
- SUZUKI R., YAMAGUCHI T., KIRINO T., ORZI F., KLATZO I. The effects of 5-minute ischemia in Mongolian gerbils: I. Blood–brain barrier, cerebral blood flow, and local cerebral glucose utilization changes. Acta Neuropathol. 1983;60:207–216. doi: 10.1007/BF00691868. [DOI] [PubMed] [Google Scholar]
- TOMINAGA M., CATERINA M.J., MALMBERG A.B., ROSEN T.A., GILBERT H., SKINNER K., RAUMANN B.E., BASBAUM A.I., JULIUS D. The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron. 1998;21:531–543. doi: 10.1016/s0896-6273(00)80564-4. [DOI] [PubMed] [Google Scholar]
- VELDHUIS W.B., VAN DER STELT M., WADMAN M.W., VAN ZADELHOFF G., MACCARRONE M., FEZZA F., VELDINK G.A., VLIEGENTHART J.F., BAR P.R., NICOLAY K., DI MARZO V. Neuroprotection by the endogenous cannabinoid anandamide and arvanil against in vivo excitotoxicity in the rat: role of vanilloid receptors and lipoxygenases. J. Neurosci. 2003;23:4127–4133. doi: 10.1523/JNEUROSCI.23-10-04127.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VOLPE B.T., HIRST W. The characterization of an amnesic syndrome following hypoxic ischemic injury. Arch. Neurol. 1983;40:436–440. doi: 10.1001/archneur.1983.04050070066017. [DOI] [PubMed] [Google Scholar]
- ZYGMUNT P.M., PETERSSON J., ANDERSSON D.A., CHUANG H., SORGARD M., DI MARZO V., JULIUS D., HOGESTATT E.D. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature. 1999;400:452–457. doi: 10.1038/22761. [DOI] [PubMed] [Google Scholar]