Abstract
Objective
To ascertain the cost-effectiveness and benefit-cost ratios of 2 public health campaigns conducted in Dallas and Houston in 1998–2000 for “catch-up” hepatitis B vaccination of Vietnamese-Americans born 1984–1993.
Design
Program evaluation.
Setting
Houston and Dallas, Texas.
Participants
A total of 14 349 Vietnamese-American children and adolescents.
Interventions
Media-led information and education campaign in Houston, and community mobilization strategy in Dallas. Outcomes were compared with a control site: Washington, DC.
Main outcome measures
Receipt of 1, 2, or 3 doses of hepatitis B vaccine before and after the interventions, costs of interventions, cost-effectiveness ratios for intermediate outcomes, intervention cost per discounted year of life saved, and benefit-cost ratio of the interventions.
Results
The number of children who completed the series of 3 hepatitis B vaccine doses increased by 1176 at a total cost of $313 904 for media intervention, and by 390 and at $169 561 for community mobilization. Costs per child receiving any dose, per dose, and per completed series were $363, $101, and $267 for media intervention and $387, $136, and $434 for community mobilization, respectively. For media intervention, the intervention cost per discounted year of life saved was $9954 and 131 years of life were saved; for community mobilization, estimates were $11 759 and 60 years of life. The benefit-cost ratio was 5.26:1 for media intervention and 4.47:1 for community mobilization.
Conclusion
Although the increases in the number of children who completed series of 3 doses were modest for both the Houston and Dallas areas, both media education and, to a lesser degree, community mobilization interventions proved cost-effective and cost-beneficial.
Keywords: cost-effectiveness analysis, benefit-cost analysis, hepatitis B vaccination, media education, community mobilization, Vietnamese-Americans
ABBREVIATIONS: HBV, hepatitis B virus; HepB, hepatitis B vaccine; VFC, Vaccines for Children; ACIP, Advisory Committee on Immunization Practices; CDC, Centers for Disease Control and Prevention; API, Asian and Pacific Islander; VCHPP, Vietnamese Community Health Promotion Project; CE, cost-effectiveness
Hasymptomatic,epatitis B virus (HBV) infection is most often acute, and resolves without serious long-term effects.1 However, 70% to 90% of infants infected at birth, 30% to 50% of children infected between 1 year and 5 years, and 5% to 10% of people infected after the age of 7 years will develop chronic HBV infection, which often results in chronic hepatitis, cirrhosis, or primary hepatocellular carcinoma.1 Studies have shown that 1 of every 4 people with chronic HBV infection eventually dies of cirrhosis or liver cancer.2 Among children in the United States, HBV infection disproportionately affects those in Asian and Pacific Islander (API) populations, including Vietnamese.3–9 Among US Viet-namese adults, the prevalence of those ever infected with HBV is as high as 80%10 compared with 3.8% in US whites.9 Studies also have documented chronic HBV infection rates ranging from 7% to 14%11–14 among US Vietnamese adults compared with 0.2% in US white adults.15 Vietnamese-American males have the highest liver cancer incidence rate of any racial/ethnic group (41.8 per 100 000), 11 times that among white males,16 and 80% of their liver cancers are caused by HBV infection.17
Hepatitis B vaccination of API infants and children was first recommended in 1982 by the US Public Health Service Advisory Committee on Immunization Practices (ACIP) as a 3-dose series administered over 6 months.18 By 1995, fewer than 10% of the estimated 1 million API children in the United States born in 1984 through 1993 had received the hepatitis B vaccine (HepB) 3-dose series.3 Consequently, in October 1995, “catch-up” vaccination for most API children born after 1983 was recommended.3 In 1997, the ACIP recommended universal vaccination of all children through age 18. These and other increasingly stronger ACIP recommendations have made it easier to provide HepB to API children in the United States. However, effectively conveying the message that HBV infection is a serious problem that can be easily prevented by 3 doses of vaccine to parents of many different cultural and language groups and their physicians, has been a difficult and slow process.19
A previous study of a hepatitis B catch-up vaccination program among an ethnically diverse community of APIs in Philadelphia found that their catch-up intervention was cost-effective and cost beneficial, although the increase in coverage was modest.20 This Philadelphia intervention was conducted in 2 communities with a diverse Southeast Asian population and primarily used community outreach with some donated media assistance. The intervention used a personalized approach in that the investigators formed a registry with the names and addresses of each targeted child and used in-home education and vaccination to accomplish their goals.
In this article, we document the cost-effectiveness (CE) and the benefit-cost ratios of a federally funded project designed to raise hepatitis B vaccination coverage among 1 API ethnic group—Vietnamese-Americans—in the Houston and Dallas areas using 2 types of intervention.21–23 One intervention was a community mobilization strategy similar to most local public health interventions without a professionally developed media campaign. A coalition of local leaders conducted educational outreach via registration of physicians as Vaccines for Children (VFC) providers, distribution of referral lists of VFC providers, distribution of health education brochures, health fairs, targeted mailings, educational presentations, and use of free local media. The other intervention was media education that relied only on a professionally developed advertising campaign with billboards, prime-time radio spots, newspaper articles and ads, brochures and calendars, and telephone hot-line. As reported elsewhere, both intervention strategies resulted in statistically significantly increased vaccination coverage among Vietnamese-American children aged 3 to 18 years and increased their parents’ knowledge about hepatitis B.23
Since 1994 when the first ACIP catch-up recommendation was made, the Centers for Disease Control and Prevention (CDC) had monitored progress using the birth cohorts 1984–1993.24 Thus, we chose to confine our economic evaluation to these birth cohorts. The 1984–1993 birth cohorts are a subset of the cohorts analyzed in our companion epidemiology article.23
Here our economic focus is on intervention-related costs, such as vaccine/administration fees, parent time lost, personnel costs, and subcontractor payments. Other important costs and benefits, such as preventing pain and suffering among family and friends of the ill patient are difficult to quantify, and are not included here. Our analyses and conclusions here must be viewed in this context.
METHODS
Study Sites
The Vietnamese Community Health Promotion Project (VCHPP, also known as Suc Khoe La Vang! Health is Gold!) at the University of California, San Francisco conducted the “Promoting Hepatitis B Catch-up Immunizations Project” between April 1998 and March 2000. The VCHPP conducted a media education campaign in the Houston metropolitan area (Harris and Fort Bend Counties) and a community mobilization campaign in the Dallas metropolitan area (Dallas and Tarrant Counties). The VCHPP subcontracted with community-based Vietnamese-American organizations in both intervention sites: the Research Development Institute in Houston and the East Dallas Counseling Center. No other promotional hepatitis B vaccination efforts for Vietnamese-American children were conducted in the Houston and Dallas areas before or during the interventions. The control site, chosen because of all available US sites it was the most comparable in demographics and size to the intervention sites, was the Washington, DC metropolitan area (the District of Columbia; Fairfax County and the City of Arlington, VA; and Prince Georges County and Montgomery County, MD).
Study Population
The study population consisted of ~1200 families of 8692 Vietnamese-American children who were born between 1984 and 1993 residing in the Houston area in 1998, and 5657 in the Dallas area. Pre- and postintervention hepatitis B vaccination coverage rates were ascertained by conducting computer-assisted telephone interviews with random samples of Vietnamese households in each of the 3 study sites in the spring of 1998 and between April 2000 and March 2001.21,23 The preintervention surveys showed that 50% of the children were born outside the United States, 40% of parents had less than a high school education, 25% lived below the poverty line, and most demonstrated the need for HBV-related education. Approximately 50% of parents said they knew nothing about HBV, and 77% did not know that vaccine was available at no cost.21
Media Intervention Campaign in the Houston Area
Between April 1998 and March 2000, the VCHHP organized a Vietnamese-language media campaign and distributed information though outdoor billboards, radio ads, print ads and news articles, brochures, calendars, and a telephone hotline. The content of this campaign was reviewed in focus groups before the start of the campaign. Campaign messages with meaningful cultural symbols were posted on billboards in Vietnamese commercial and residential areas for 41 billboard-months. The presence of the billboards was publicized through press releases, radio spots, and print ads.
Campaign radio spots were aired on 2 Vietnamese-language radio stations (Voice of Vietnam and Little Saigon). Eight 30- to 60-second Vietnamese spots were aired 3663 times over 15 months in the daytime and early evenings. The campaign had 10 advertisements and 6 articles published in 5 local Vietnamese newspapers with a combined circulation of 5000.
Using print media, the campaign distributed 6000 26-page, 4-color ink, glossy paper, Vietnamese-language educational booklets and 8000 special calendars with hepatitis B information at Vietnamese Buddhist temples, churches, community festivals, physicians’ offices, housing complexes, and supermarkets. A telephone hotline staffed by the Vietnamese-American Community Health Network at Research Development Institute answered questions about hepatitis B, immunizations, and other health topics.
Community Mobilization Interventions in the Dallas Area
VCHPP conducted a community mobilization campaign in Dallas with the assistance of a subcontractor, East Dallas Counseling Center. A coalition of Vietnamese groups in Dallas was formed. Its 19 members included representatives from health care, public health, education, business, community-based organizations, and press, as well as veterans, seniors, and researchers. They met quarterly and worked through 3 subcommittees—advisory, planning, and outreach—and had a full-time bicultural Vietnamese-American project coordinator. They developed an action plan to raise hepatitis B awareness and increase vaccination rates.
The coalition members conducted outreach to doctors’ offices, clinics, churches, temples, schools, day-care centers, Special Supplemental Nutrition Program for Women, Infants and Children sites, Aid to Families With Dependent Children sites, service organizations, other Vietnamese-American community-based organizations, and public housing blocks with large proportions of Vietnamese-American residents. The campaign encouraged 6 Vietnamese physicians to enroll in the federal VFC Program. The coalition provided Vietnamese parents with referral lists of all VFC providers through the community-based organizations, and at health fairs, markets, and shopping centers.
The coalition distributed health education brochures and pamphlets through health fairs, mailings, educational presentations, and free local media. They mailed and handed out 5300 bilingual hepatitis B brochures and pamphlets. Coalition members assisted in organizing 13 health fairs for Vietnamese-Americans in shopping centers, community centers, churches, temples, lunar New Year events, mid-autumn festivals, and Christmas events. Members made 8 oral presentations at health fairs and Vietnamese-American community-based organization meetings. Every Sunday, staff made presentations at Vietnamese Buddhist temples, churches, and language schools. Staff visited Vietnamese families at home and served as translators twice a week at 2 community clinics to help children receive vaccinations. Staff solicited donations from charitable organizations, companies, and local businesses to offer “prizes” to kids who received vaccinations. Three Vietnamese-language newspapers printed 8 news articles and 8 announcements about the campaign. Vietnamese Public Radio and the Vietnamese Broadcasting Network Radio interviewed the coalition chair and staff twice and broadcast 8 announcements 3 times daily just before the health fairs and community events.
Estimation of Doses Administered
The sampling criterion used in this article is similar to those used in the secondary analysis of the companion article,23 and provides a conservative estimate of coverage. Children whose parents and provider(s) did not have a written vaccination record showing dates for hepatitis B vaccination were counted as not receiving the vaccine. We compared estimates of raw changes in rates of children who completed the series of 3 doses (HepB3) for each age group in both Houston and Dallas, and then applied the rate changes to the population to estimate the number of doses administered in both sites.
Measurement of Intervention Costs
Intervention costs included vaccine and associated administration, parent time lost, subcontractor payments, and VCHPP personnel costs. Although the work of volunteers in Dallas did not cost the program anything, the worth of their time was estimated and included in the analysis. Also included were the media and billboards purchase costs in Houston. The contractual costs and personnel time spent on this project were collected quarterly. Contractual costs included personnel of local agency, travel, supplies, freight/postage, and other operating expenses. Personnel costs included salary and benefits.
At the time of the intervention, the federal contract and private sector prices for HepB were $9.00 and $22.285 per dose, respectively. The distributions of publicly purchased versus privately purchased vaccine were derived from the CDC VACMAN database25 and voluntary manufacturers’ reports to CDC (CDC, unpublished data, 2000). Approximately 42.9% of these doses were purchased by public funds and 57.1% by private providers in Texas. Approximately 36% of publicly purchased HepB were administered by private providers in Dallas and 48% in Houston (CDC, National Immunization Survey, 2001). The administration cost for vaccination during a visit to a public clinic was estimated at $5 (CDC, Houston mobile clinic study, unpublished data, 2000). In the private sector, the estimated administration cost was $15.09 (in 1995 dollars).26 Other costs of vaccination include the caregiver’s travel to the clinic at $3.50, and 2 hours time off from work to take the child for vaccination. We assumed that 85% of the caregivers were female,27 and the average wage for these caregivers was $8.25 per hour. All costs are estimated from societal perspective and are reported in 2000 dollars.
CE Analysis of Intermediate Outcomes
To examine the CE of intermediate outcomes, 4 CE ratios were calculated: intervention cost per child receiving any dose, cost per dose delivered, cost per completed series of 3 doses, and cost per additional child rendered seroprotected (antibodies to hepatitis B surface antigen of ≥10 mIU/mL). Similar to the method used by Deuson et al,20 the CE ratios were calculated as:
Seroprotection rate for receipt of only the first dose (HepB1) was assumed to be 50%.5,28–32 Accepted estimates of second- and third-dose seroprotection rates are 85% and 95%, respectively.5,28–32 To estimate the number of recipients rendered immune, a proportion of each of 3 groups of vaccine recipients were summed. Recipients who received only the first dose were multiplied by 0.50, those who received only 2 doses by 0.85, and those who received all 3 doses by 0.95. We performed sensitivity analysis to see the effect of the assumptions for the first-dose seroprotection rate with 20% or 35%.
CE and Benefit-Cost Analysis of Lifetime Outcomes
Measures of long-term outcomes are vital for understanding if money invested in an intervention will be repaid by benefits that accrue over years. We quantified long-term outcomes in 2 ways: intervention cost per discounted year of life saved, and benefit-cost over the life expectancy of the children in this population, when costs of HBV infections or costs savings from averted infections would become apparent.
Using a discount rate provides a method of adjusting the value of receiving benefits today versus receiving benefits in the future, or of incurring costs in the present versus incurring costs in the future. For example, a dollar that an individual receives this year is worth more than a dollar that is received 10 years from now, because this year’s dollar can be invested so that in 10 years’ time it will be worth more than a dollar. Therefore, if discounted at 3%, the value of 1.00 dollar received 10 years from today would equal 0.74 dollar received today. The discount rate is not related to inflation.33
We computed the base-case estimate of intervention cost per discounted year of life saved and benefit-cost ratio, using a 3% discount rate34 and an estimated 60% whole-life infection rate among Vietnamese-Americans. This discount rate is the standard used for economic analysis in the United States, and this rate of infection is estimated to be within the conservative range of rates likely to prevail among first-generation immigrant Vietnamese-American children in unvaccinated populations.
The benefits were quantified through the following assumptions: 60% of infections are asymptomatic, and 15% of persons infected in late childhood or as adolescents are at risk of chronic liver disease.
The costs for the treatment of the patients with HBV infection included direct (medical) and indirect (work loss) costs. Direct medical costs included the inpatient, outpatient, laboratory, radiologic, drug, and liver transplantation costs for HBV infection. Indirect costs included loss of earnings for HBV-related illness and for premature mortality caused by HBV infection.
All cost data in the model came from the Bureau of Labor Statistics, the Bureau of the Census, the Medstat Marketscan database, refereed publications, interviews of experts in the field, and CDC data.35–38 We used a modified spreadsheet program (Bencost HepB model) developed at the CDC and based on the work of Margolis et al.5 In this model, we considered vaccination age and whole-life infection risk to estimate the risk of children in the different age groups who were unvaccinated or partially vaccinated.
To calculate intervention cost per discounted year of life saved for each intervention site, the total intervention costs incurred in each site were divided by the discounted years of life saved by the intervention. The present value (net saving) is the sum of the discounted benefits from the intervention minus the sum of the discounted costs of the intervention. To calculate benefit-cost ratio, the discounted benefits was divided by discounted costs incurred in the intervention in each area.
We then performed sensitivity analyses to explore the effect of the assumptions for discount rate and infection rate. We computed ratios for all combinations of 3% and 5% discount rates and 30% to 75% rates of infection, at increments of 15%. We used a broad range of infection rates to account for the potential variability resulting from differences in baseline vaccination levels, risk levels, and different ages at immigration. Because the percentage of vaccines administered by the private sector is increasing, we also explored the impact on CE and benefit-cost ratios of conducting such a project at private sector prices.
RESULTS
Doses Administered
At the end of the intervention, the number of children receiving any dose increased by 865 (from 1953 [22.5%] to 2818 [32.4%]) in the media intervention (Houston) area and 437 (from 1181 [20.9%] to 1618 [28.6%]) in the community mobilization (Dallas) area (Table 1). During the intervention, it is estimated that 3116 doses of HepB were administered to children born 1984–1993 in the media (Houston) area and 1243 doses in the community mobilization (Dallas) area.
TABLE 1.
Estimated Changes in Number of HepB Doses Received by Vietnamese Children Born 1984–1993 Before and After a Media Intervention (Houston, TX) or Community Mobilization Intervention (Dallas, TX) Was Conducted, Vietnamese American Hepatitis B Catch-up Project, 1998–2000
| Media Intervention (Houston) N = 8692
|
Community Mobilization Intervention (Dallas) N = 5657
|
|||||
|---|---|---|---|---|---|---|
| Dose No. | Preintervention 1998 | Postintervention 2000 | Marginal Doses | Preintervention 1998 | Postintervention 2000 | Marginal Doses |
| 1st dose | 1953 | 2818 | 865 | 1181 | 1618 | 437 |
| 2nd dose | 1567 | 2642 | 1075 | 976 | 1392 | 416 |
| 3rd dose | 1238 | 2414 | 1176 | 801 | 1191 | 390 |
| Total no. of doses | 4758 | 7874 | 3116 | 2958 | 4201 | 1243 |
The number of children who completed the series of 3 doses (HepB3) increased in birth cohorts 1984–1993, by 1176 (13.5%) for the media intervention site(Houston), 390 (6.9%) for the community mobilization site (Dallas), and 0 (0%) for the control site (Washington, DC area). We based our cost and benefit calculations of the interventions in the Dallas and Houston areas on the relative increase in estimated doses delivered, and vaccination coverage levels.
Numbers of doses administered for each 1998 age group are shown in Fig 1. The majority of doses administered during the interventions in the Houston and Dallas areas were to those 9 years old and older (born before 1990). We evaluated the receipt of HepB1 by month and by quarter over the length of the interventions using a Cochran-Armitage Trend Test and found no statistically significant differences between intervention cities and the control city.
Fig 1.
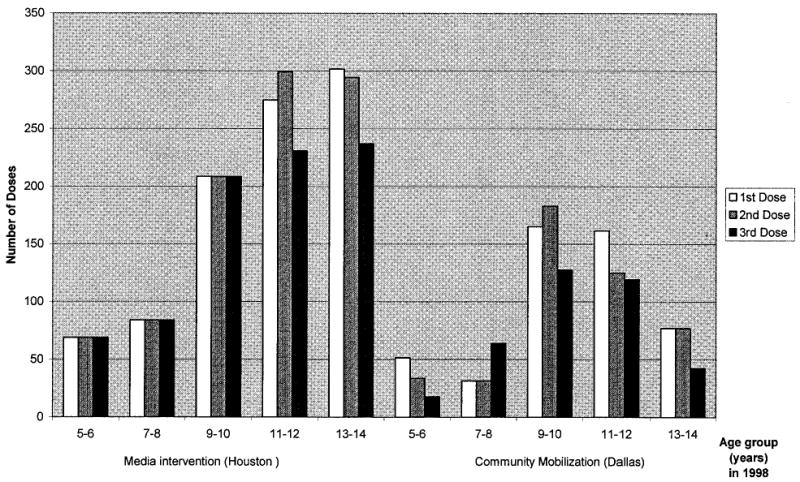
HepB doses administered by age of child for Vietnamese children in the media (Houston) and community mobilization intervention (Dallas) areas, 1998–2000.
If we assume seroprotection is 95%, 85%, and 50% for doses 3, 2, and 1, the estimated number of additional immune children is 926 (10.7%) by media intervention and 403 (7.1%) by community mobilization.
Intervention Costs
Total intervention and vaccination costs were $313 904 for the media intervention site (Houston) and $169 561 for the community mobilization site (Dallas) (Table 2). The majority of the costs in the Houston area were vaccination costs ($160 581, 51.2%). In the Dallas area, the majority of the costs were personnel cost (personnel at VCHPP + personnel at local agency + volunteers, $91 380, 53.9%), but vaccination costs were 37.3% of the total.
TABLE 2.
Costs of Media Intervention (Houston) and Community Mobilization Intervention (Dallas) Including Vaccination, Vietnamese American Hepatitis B Catch-up Project, 1998–2000
| Item | Media Intervention(Houston) | Community Mobilization Intervention(Dallas) |
|---|---|---|
| Direct intervention costs | ||
| Media | $138 412 | $0 |
| Personnel at VCHPP | $6453 | $10 390 |
| Personnel at local agency | $7589 | $71 956 |
| Volunteers’ time | $0 | $9034 |
| Other costs* | $869 | $14 896 |
| Subtotal | $153 323 | $106 276 |
| Vaccination costs | ||
| Vaccine | $51 672 | $20 631 |
| Administration | $46 600 | $17 776 |
| Parents time lost | $62 309 | $24 878 |
| Subtotal | $160 581 | $63 285 |
| Total | $313 904 | $169 561 |
Other costs include travel, supplies, freight/postage and other operating expenses.
CE of Intermediate Outcomes
The intervention cost per child receiving any dose, cost per dose delivered, cost per completed series, and cost per additional child rendered seroprotected were $363, $101, $267, and $339 for media intervention, and $387, $136, $434, and $420 for community mobilization, respectively. Under the assumptions of 20% and 35% first-dose seroprotection rates, the costs per additional child rendered seroprotected were $317 and $328 for media intervention, and $427 and $424 for community mobilization, respectively.
CE Analysis and Benefit-Cost Analysis of Lifetime Outcomes
In the base-case analysis (60% rate of infection and 3% discount rate), years of life saved by media intervention were 131 and by community mobilization were 60; the intervention cost per discounted year of life saved was $9954 for the media intervention and $11 759 for the community mobilization. The net saving was $1336,667 by the media intervention and $588 184 by the community mobilization. Benefit-cost ratio was 5.26 for the media intervention and 4.47 for the community mobilization (Table 3).
TABLE 3.
Years of Life Saved, CE Ratios and Benefit-Cost Ratios for Lifetime Outcomes, 30% to 75% Rates of Infection, and 3% and 5% Discount Rates for the Media Intervention (Houston) and the Community Mobilization Intervention (Dallas), Vietnamese American Hepatitis B Catch-up Project, 1998–2000
| Media Intervention (Houston)
|
Community Mobilization Intervention (Dallas)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Rate of Infection
|
Rate of Infection
|
|||||||
| Item | 30%‡ | 45%‡ | 60%* | 75%‡ | 30%‡ | 45%‡ | 60%* | 75%‡ |
| Years of life saved | 65 | 98 | 131 | 163 | 30 | 45 | 60 | 75 |
| Intervention cost per discounted year of life saved, discounted at: | ||||||||
| 3% | $19 909 | $13 272 | $9954 | $7963 | $23 519 | $15 679 | $11 759 | $9407 |
| 5% | $45 035 | $34 591 | $22 517 | $18 014 | $53 583 | $35 722 | $26 792 | $21 433 |
| Benefit-cost ratios, discounted at: | ||||||||
| 3% | 2.63 | 3.94 | 5.26 | 6.57 | 2.23 | 3.35 | 4.47 | 5.59 |
| 5% | 1.32 | 1.72 | 2.64 | 3.30 | 1.11 | 1.67 | 2.23 | 2.78 |
Base case analysis.
Sensitivity analysis.
In the sensitivity analyses, years of life saved ranged from 65 to 163 for the media intervention, and from 30 to 75 for the community mobilization, as the assumed rate of infection increased from 30% to 75%. The intervention cost per discounted year of life saved ranged from $7963 (75% rate of infection, 3% discount rate) to $45 035 (30% rate of infection, 5% discount rate) for the media intervention and from $9407 to $53 583 for the community mobilization (Table 3). The benefit-cost ratios range from 1.32:1 (30% rate of infection, 5% discount rate) to 6.57:1 (75% rate of infection, 3% discount rate) for the media intervention, and from 1.11:1 to 5.59:1 for the community mobilization. All of these benefit-cost ratios are over the threshold point (1.0) where benefits cover costs exactly. Assuming that 100% of the vaccines were purchased at the higher private sector price, the discounted cost per discounted year of life saved for the base-case analysis was $11 655 for the media intervention and $13 244 for the community mobilization, and the benefit-cost ratio was 4.49:1 for the media intervention and 3.97:1 for the community mobilization.
DISCUSSION
This analysis indicates that both interventions, media intervention in Houston and community mobilization in Dallas, were cost-effective and cost-beneficial. However, the community mobilization was more labor-intensive, and had lower impact on coverage. The media intervention was more expensive, but appears to be slightly more cost-effective and cost-beneficial. Therefore, media education specifically targeted to the Vietnamese community is highly recommended as an effective intervention to boost the very low hepatitis B vaccination coverage among Vietnamese-American children and adolescents. However, since we did not investigate other potential benefits of the community mobilization (such as developing a network of community-based groups and capacity building), we cannot exclude the possibility that community mobilization may have more long-term benefits in addition to raising hepatitis B vaccination levels.
When education, outreach, and planning costs are held constant, examining each aspect of the costs suggests that if more children completed the 3-dose series, cost per completed series would decline appreciably, because ~49% of the costs of the intervention in Houston and 63% in Dallas were not related to vaccination itself. If higher coverage was achieved (90% receiving at least 1 dose, 80% at least 2 doses, and 70% all 3 doses) for both areas in the base-case scenario, model simulations (not shown here) suggest that 794 years of life would be saved in the media intervention area and 555 years in the community mobilization area, that the cost per discounted year of life saved would be $5300 for the media intervention and $5034 for the community mobilization intervention, and that the benefit-cost ratio would likely be 10.01:1 for the media intervention and 10.58:1 for the community mobilization intervention.
Economic analyses of projects such as this are important because results can help policy makers compare programs to maximize return on investment by selecting the most effective programs. In general, costs for these interventions compare favorably to other life-saving health interventions, despite a relatively low increase in HepB coverage. Tengs et al39 reported the CE of 587 life-saving interventions in the United States. The median medical intervention cost per year of life saved was $19 000 (no net savings). Hence, while the interventions appear modest by some measures (eg, 1176 more children completed the HepB series by media intervention [Houston] and 390 by community mobilization [Dallas]), these interventions result in net savings; therefore, they compare very favorably with other medical interventions.
Sensitivity analyses are important for testing how strongly the outcomes depend on assumptions. This is particularly useful in cases where input values cannot be precisely defined. In this study, because all the ratios calculated in the sensitivity analyses show a net benefit, we conclude that model results are not qualitatively affected by differing assumptions about discount and infection rates.
Although this analysis results from the accurate measurement of all program costs and reflects the epidemiologic conditions prevailing in Houston and Dallas, caution should be exercised in comparing this study with others. For example, we calculated ratios using years of life saved, rather than quality-adjusted life years,40 because it is very difficult to obtain reliable health utilities used in calculating quality-adjusted life years for measuring the different health states of chronic hepatitis B patients. In addition, we did not consider the cost of adverse events attributable to vaccination (because these are rare),41 nor did we use estimates of wage and workforce participation rates specific to the Houston and Dallas areas. Analyses of similar programs that use dissimilar methods or sources of data may have limited comparability.
In this article, we limited our population to those born 1984–1993 to keep it similar to other studies assessing progress with API hepatitis B catch-up.20,24 Because this differs from the broader age inclusion criterion in our companion article,23 it might underestimate the benefits of the interventions. In addition, the use in this article of a sampling criterion similar to the secondary analysis of our companion article resulted in our finding the media intervention in Houston to be the more cost-effective. If we had used the same sampling criteria as used in the companion article’s primary analysis, we would have found the community mobilization to be the more cost-effective of the 2 interventions (data not shown). However, for the economic analysis, we thought it more appropriate to use the sampling criterion that includes all the children to estimate coverage.
Keeping in mind the cautions mentioned above, the CE of these catch-up hepatitis B vaccination efforts may be compared with those conducted in Philadelphia.20 Both projects focused on API populations; however, there are a number of differences in methods and analyses. We included parental time lost and travel costs for vaccination in the current analysis. Had we omitted these costs, the benefit-cost ratios would be 6.56:1 for the media intervention, and 5.24:1 for the community mobilization. However, both of these ratios are still lower than the benefit-cost ratio (8.80:1) seen in Philadelphia. This may be because the Philadelphia target age group did not include high school-aged adolescents, the intervention used a vaccination registry of all targeted children allowing for tracking/reminder/recall activities for each child, and the investigators provided family-specific transportation/translator and in-home education and vaccination services.20
The findings presented here may be applied to similar catch-up hepatitis B vaccination programs among API. There are many smaller outreach and vaccination programs being conducted in the major metropolitan areas of the United States that include community coalitions and media outreach at a less intensive level. Their benefits most likely outweigh their more modest costs as well. The community mobilization conducted in this project has likely been duplicated in other places. However, the media campaign in this project was unique to the study, implemented without other types of community outreach, and more professional than what has been done or is likely to be done in other places. Its impact is thus difficult to compare to that of other media interventions that are often combined with community outreach activities. The findings here do indicate that media alone would be cost-effective for others to do if they can spend the funds necessary.
Recent published articles suggest that the measurable impact of most public health interventions is usually relatively small, and often statistically non-significant.42–44 In this instance, the interventions produced statistically significant increases in complete vaccination coverage (in 24 months, 1176 [13.5%] completed the series of 3 HepB doses with media intervention and 390 [6.9%] with community mobilization), and their impact was both cost-effective and cost-beneficial. Nationwide in cities with relatively high concentrations of APIs, media education and community mobilization could be adopted to substantially increase API childhood and adolescent hepatitis B vaccination coverage in the next few years. Using these 2 methods together may result in even more cost-effective and cost-beneficial outcomes.
Acknowledgments
This research was supported by funds provided by the CDC under Cooperative Agreement U66/CCU915175. We thank Sang Nguyen, MSW, at the East Dallas Counseling Center, Dallas; and Martin Quach Huynh Ha, PhD, at Research Development Institute, Houston, for their contributions to this study; Son Do, MD, of Dallas for his expertise and support of this initiative; Christopher N. H. Jenkins, MA, MPH (deceased), for project design and direction; Joyce Bird, PhD, Yifei Ma, MA, MS, Drew Baughman, PhD, and Pengjun Lu, PhD, for their invaluable assistance in data analysis; and Mary McCauley, MTSC, for her assistance in manuscript preparation.
References
- 1.Robinson WS. Hepatitis B virus and hepatitis D virus. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. 4th ed. New York, NY: Churchill Livingstone; 1995. pp. 1406–1439. [Google Scholar]
- 2.Beasley RP, Hwang L-Y. Epidemiology of hepatocellular carcinoma. In: Vyas GN, Dienstag JL, Hoofnagle JH, editors. Viral Hepatitis and Liver Disease. New York, NY: Grune & Stratton; 1984. pp. 209–224. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Update: recommendations to prevent hepatitis B virus transmission—United States. MMWR Morb Mortal Wkly Rep. 995;44:574–575. [PubMed] [Google Scholar]
- 4.Hurie M, Mast EE. Horizontal transmission of hepatitis B virus infection to United States-born children of Hmong refugees. Pediatrics. 1992;89:269–273. [PubMed] [Google Scholar]
- 5.Margolis HS, Coleman PJ, Brown RE, Mast EE, Sheingold SH, Arevalo JA. Prevention of hepatitis B virus transmission by immunization: an economic analysis of current recommendations. JAMA. 1995;274:1201–1208. [PubMed] [Google Scholar]
- 6.Mahoney F. Update on diagnosis, management, and prevention of hepatitis B virus infection. Clin Microbiol Rev. 1999;12:351–366. doi: 10.1128/cmr.12.2.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahoney F, Smith N, Alter M, Margolis HS. Progress towards the elimination of hepatitis B virus transmission in the United States. Viral Hepatitis Rev. 1997;3:105–119. [Google Scholar]
- 8.Margolis HS, Alter M, Hadler S. Hepatitis B: evolving epidemiology and implications for control. Semin Liver Dis. 1991:1184–1192. doi: 10.1055/s-2008-1040427. [DOI] [PubMed] [Google Scholar]
- 9.Coleman P, McQuillan G, Moyer L, Lambert S, Margolis H. Incidence of hepatitis B virus infection in the United States, 1976–1994: estimates from the National Health and Nutrition Examination Surveys. J Infect Dis. 1998;178:954–959. doi: 10.1086/515696. [DOI] [PubMed] [Google Scholar]
- 10.Nelson KR, Bui H, Samet JH. Screening in special populations: a “case study” of recent Vietnamese Immigrants. Am J Med. 1997;102:435–440. doi: 10.1016/S0002-9343(97)89443-0. [DOI] [PubMed] [Google Scholar]
- 11.Klontz KC. A program to provide hepatitis B immunoprophylaxis to infants born to HbsAg-positive Asian and Pacific Islander women. West J Med. 1987;146:195–199. [PMC free article] [PubMed] [Google Scholar]
- 12.Mahoney FJ, Lawrence M, Scott C, Le Q, Lambert S, Farley TA. Continuing risk for hepatitis B virus transmission among Southeast Asian infants in Louisiana. Pediatrics. 1995;96:1113–1116. [PubMed] [Google Scholar]
- 13.Tong MJ, Hwang S-J. Hepatitis B infection in Asian Americans. Gastro-enterol Clin North Am. 1994;23:532–536. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Screening for hepatitis B infection among refugees arriving in the United States, 1979–91. MMWR Morb Mortal Wkly Rep. 1991;40:784–786. [PubMed] [Google Scholar]
- 15.Advisory Committee for Immunization Practices. Recommendations for protection against viral hepatitis. MMWR Recomm Rep. 1990;39(RR2):1–26. [PubMed] [Google Scholar]
- 16.Miller BA, Kolonel LN, Bernstein L, et al., editors. Bethesda, MD: National Cancer Institute; 1996. Racial/Ethnic Patterns of Cancer in the United States: 1988–92. NIH Publ. No. 96-4104. [Google Scholar]
- 17.Taylor VM, Jackson JC, Pineda M, et al. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. J Cancer Educ. 2000;15:51–55. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control. Recommendation of the Immunization Practices Advisory Committee (ACIP): inactivated hepatitis B virus vaccine. MMWR Morb Mortal Wkly Rep. 1982;31:317–322. 327–328. [PubMed] [Google Scholar]
- 19.Euler GL. The epidemiology of hepatitis B vaccination catch-up among AAPI children in the United States. Asian Am Pacific Isl J Health. 2001;9:154–161. [PubMed] [Google Scholar]
- 20.Dueson RR, Brodovicz KG, Barker L, Zhou F, Euler GL. Economic analysis of a child vaccination project among Asian Americans in Philadelphia, Pa. Arch Pediatr Adolesc Med. 2001;155:909–914. doi: 10.1001/archpedi.155.8.909. [DOI] [PubMed] [Google Scholar]
- 21.Jenkins CNH, McPhee SJ, Wong C, Nguyen T, Euler GL. Hepatitis B immunization coverage among Vietnamese-American children 3–18 years old. Pediatrics. 2000;106(6) doi: 10.1542/peds.106.6.e78. Available at: www.pediatrics.org/cgi/content/full/106/6/e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jenkins CNH, Buu C, Berger W, Son DT. Liver carcinoma prevention among Asian Pacific Islanders: getting shots into arms. Cancer. 2001;91:252–256. doi: 10.1002/1097-0142(20010101)91:1+<252::aid-cncr14>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 23.McPhee SJ, Nguyen T, Euler G, et al. Successful promotion of hepatitis B vaccinations among Vietnamese-American children aged 3 to 18: results of a controlled trial. Pediatrics. 2003;111:1278–1288. doi: 10.1542/peds.111.6.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Hepatitis B vaccination coverage among Asian and Pacific Islander children—United States, 1998. MMWR Morb Mortal Wkly Rep. 2000;49:616–619. [PubMed] [Google Scholar]
- 25.VACMAN. [Accessed October 12, 2001]; Available at: http://www.cdc.gov/nip/vacman.
- 26.Fleming GV. Elk Grove Village, IL: American Academy of Pediatrics; 1995. Vaccine administration fee survey: child health care update; pp. 11–16. [Google Scholar]
- 27.Deuson R, Hoekstra E, Sedjo R, et al. The Denver school-based adolescent hepatitis B vaccination program: a cost analysis with risk simulation. Am J Public Health. 1999;89:1722–1727. doi: 10.2105/ajph.89.11.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andre F, Zuckerman A. Protective efficacy of hepatitis B vaccines in neonates. J Med Virol. 1994;44:144–154. doi: 10.1002/jmv.1890440206. [DOI] [PubMed] [Google Scholar]
- 29.Goh KT, Kong K, Chan S. Comparison of the immune response of four different dosages of a yeast recombinant hepatitis B vaccine in Singapore children: a four year follow-up study. Bull World Health Organ. 1992;70:233–239. [PMC free article] [PubMed] [Google Scholar]
- 30.Greenberg DP, Vadheim CM, Marcy SM, et al. Comparative safety and immunogenicity of two recombinant hepatitis B vaccines given to infants at 2, 4, and 6 months of age. In: Program and abstracts of the 23rd Interscience Conference on Antimicrobial Agents and Chemotherapy; 1992; Anaheim, CA. Abstract 264. [Google Scholar]
- 31.Zajac BA, West DJ, McAleer WJ, Scolnick EM. Overview of clinical studies with hepatitis B vaccine made by recombinant DNA. J Infect. 1986;13(Suppl A):39–45. doi: 10.1016/s0163-4453(86)92668-x. [DOI] [PubMed] [Google Scholar]
- 32.Da Villa G, Piazza M, Iorio R, et al. A pilot model of vaccination against hepatitis B virus suitable for mass vaccination campaigns in hyperendemic areas. J Med Virol. 1992;36:274–278. doi: 10.1002/jmv.1890360408. [DOI] [PubMed] [Google Scholar]
- 33.Haddix AE, Teutsch SM, Shaffer PA, Dunet DO, editors. New York, NY: Oxford University Press; 1996. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. [Google Scholar]
- 34.Gold M, Siegel J, Russell L, Weinstein M. New York, NY: Oxford University Press; 1996. Cost-Effectiveness in Health and Medicine. [Google Scholar]
- 35.Brookman R, Koff RS, Shaffner W, Margolis HS. Critical issues surrounding hepatitis B vaccination for adolescents: a roundtable. J Adolesc Health. 1995;17:208–233. doi: 10.1016/1054-139X(95)00147-K. [DOI] [PubMed] [Google Scholar]
- 36.Bureau of Census. Demographics. [Accessed December 27, 2001];2000 Available at: http://www.census.gov/population/www/index.html.
- 37.Bureau of Labor Statistics. Average Hourly Earnings. Department of Labor. [Accessed December 27, 2001];2000 Available at: http://www.bls.gov/bls/wages.htm.
- 38.The MEDSTAT Group I. Ann Arbor, MI: The Medstat Group; 1998. Marketscan Database (1996) [Google Scholar]
- 39.Tengs T, Adams M, Pliskin J, Safran D. Five-hundred life-saving interventions and their cost-effectiveness. Risk Analysis. 1995;15:369–390. doi: 10.1111/j.1539-6924.1995.tb00330.x. [DOI] [PubMed] [Google Scholar]
- 40.Stratton KR, Durch JS, Lawrence RS, editors. Washington, DC: National Academy Press; 1999. Vaccines for the 21st Century: A Tool for Decision-making [Proof copy] [PubMed] [Google Scholar]
- 41.Vaccine Safety Committee Institute of Medicine. Hepatitis B Vaccine. In: Stratton KR, Howe C, Johnston R Jr, editors. Adverse Events Associated with Childhood Vaccines: Evidence Bearing on Causality. Washington, DC: National Academy Press; 1994. pp. 211–235. [PubMed] [Google Scholar]
- 42.Fishbein M. Great expectations, or do we ask too much from community-level interventions? [Editorial] Am J Public Health. 1996;86:1075–1076. doi: 10.2105/ajph.86.8_pt_1.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.LeBaron CW, Chambliss J, Chaney M. The impact of interventions by a community-based organization on inner-city vaccination coverage Fulton County, Georgia 1992–1993. Arch Pediatr Adolesc Med. 1999;152:322–332. doi: 10.1001/archpedi.152.4.327. [DOI] [PubMed] [Google Scholar]
- 44.Wood D, Schuster M, Donald-Sherbourne C, Duan N, Mazel R, Halfon N. Reduced missed opportunity to vaccinate during child health visit: how effective are parent education and case management? Arch Pediatr Adolesc Med. 1996;152:238–243. doi: 10.1001/archpedi.152.3.238. [DOI] [PubMed] [Google Scholar]


