Abstract
Nipah virus (NiV), a paramyxovirus, was first discovered in Malaysia in 1998 in an outbreak of infection in pigs and humans and incurred a high fatality rate in humans. Fruit bats, living in vast areas extending from India to the western Pacific, were identified as the natural reservoir of the virus. However, the mechanisms that resulted in severe pathogenicity in humans (up to 70% mortality) and that enabled crossing the species barrier were not known. In this study, we established a system that enabled the rescue of replicating NiVs from a cloned DNA by cotransfection of a constructed full-length cDNA clone and supporting plasmids coding virus nucleoprotein, phosphoprotein, and polymerase with the infection of the recombinant vaccinia virus, MVAGKT7, expressing T7 RNA polymerase. The rescued NiV (rNiV), by using the newly developed reverse genetics system, showed properties in vitro that were similar to the parent virus and retained the severe pathogenicity in a previously established animal model by experimental infection. A recombinant NiV was also developed, expressing enhanced green fluorescent protein (rNiV-EGFP). Using the virus, permissibility of NiV was compared with the presence of a known cellular receptor, ephrin B2, in a number of cell lines of different origins. Interestingly, two cell lines expressing ephrin B2 were not susceptible for rNiV-EGFP, indicating that additional factors are clearly required for full NiV replication. The reverse genetics for NiV will provide a powerful tool for the analysis of the molecular mechanisms of pathogenicity and cross-species infection.
Keywords: henipavirus, infectious clone, recombinant virus, reverse genetics
Nipah virus (NiV) was isolated in 1998 after an outbreak of fatal encephalitis with >40% mortality among pig farmers in Malaysia and Singapore (1). It was found to be antigenically and genomically related to Hendra virus (HeV), which was isolated in Australia in 1994 (2–4). In 1998, the virus spread from fruit bats to pigs and then to humans. In more recent outbreaks in Bangladesh with up to 70% mortality, NiV was probably transmitted directly from bats to humans, and it has been suggested that human-to-human transmission may occur (5–8). NiV has a broad host range, and high mortality rates are associated with human infections. In humans, NiV causes severe encephalitis with high fatality rates in both the Malaysian outbreak in 1998–1999 (1) and the Bangladesh outbreak in 2004 (9, 10). In contrast, the virus was responsible for a highly infectious respiratory disease with low mortality in pigs. Because of the broad host range and the high mortality rates associated with these infections, NiV has been classified as a biosafety level 4 (BSL-4) agent.
NiV has been assigned to a new genus, Henipavirus, within the subfamily Paramyxovirinae, family Paramyxoviridae (11). Molecular characterization of NiV showed that it is very closely related to another zoonotic paramyxovirus, HeV (70–85% sequence homology). In contrast to all other paramyxoviruses, NiV and HeV infect a wide range of species, including pigs, cats, and humans (12). The NiV genome is a single-stranded, negative-sense and nonsegmented RNA that is 18,246 nt (Malaysia isolate) or 18,252 nt (Bangladesh isolate) (3) in length, which is much larger than the other viruses in family Paramyxoviridae (≈15,100∼15,900 nt for ruburaviruses, avulaviruses, respiroviruses, morbilliviruses, and pneumoviruses; 13,000 nt for metapneumoviruses). The predicted gene-start, gene-end, RNA editing site and intergenic sequences are conserved, when compared with the morbilliviruses (4, 13–16). The number and order of genes are identical to those found in the respiroviruses and morbilliviruses. NiV has six transcription units encoding six structural proteins, the nucleocapsid (N), phosphoprotein (P), matrix protein (M), fusion protein (F), glycoprotein (G), and polymerase (L). The P gene is predicted to encode accessory proteins, namely V, W, and C proteins, as is the case for other paramyxoviruses. It was also shown that NiV conforms to the rule of six and uses a replication strategy that is similar to those of other paramyxoviruses (17).
To examine the role played by the different virus proteins in the pathology of NiV infections, it is necessary to be able to manipulate the virus genes within the complete virus genome. The technology, called reverse genetics, has revolutionized the field of negative-stranded RNA viruses. Recent fundamental observations from the studies based on the reverse genetics on various negative-stranded RNA viruses have provided a basis for the prevention of these viruses and for the development of novel therapies (18). In the present study, to establish this powerful technology for NiV, a full-length cDNA of the NiV genome was constructed and a reverse genetics system developed, using helper plasmids encoding N, P, and L proteins. To facilitate the study of NiV infections, a recombinant NiV that expresses enhanced green fluorescent protein (EGFP) was also constructed. These recombinant viruses were compared with the original NiV.
Results
Construction and Rescue of Recombinant NiVs.
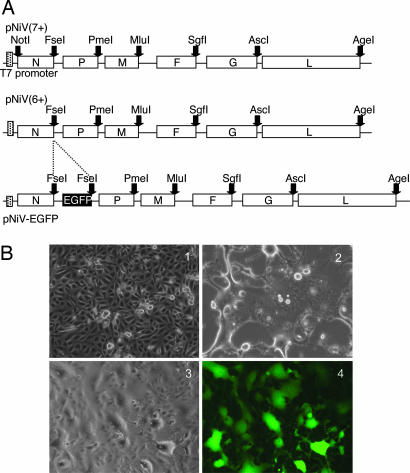
A cDNA representing the full length of the NiV genome [NiV isolate from Malaysia (2)] was constructed. This was inserted in the plasmid pMDB1. Unique restriction sites were included at the end of each gene (pNiV6+), and, in a further construction, an extra restriction site was included at the end of the leader sequence [pNiV(7+)]. A third construction expressed the EGFP gene, which was inserted downstream of the N gene. The different constructions are shown in Fig. 1A.
Fig. 1.
Construction of plasmids and CPE induced by rNiVs. (A) Schematic representation of the pNiV full-length clones constructed. The unique restriction sites used in the cloning procedure are shown. pNiV(6+) has six unique restriction enzyme sites. pNiV(7+) has an extra restriction site in the leader sequence. (B) Infection of Vero cells with rNiV and rNiV-EGFP. Noninfected Vero cells (1) were compared with cells infected with either rNiV (2) or rNiV-EGFP (3 and 4) at a multiplicity of infection of 0.01 pfu per cell. The cells were observed after 24 h in a light microscope (1-3) or by fluorescence (4).
To rescue infectious virus from the full-length clones, CV-1 cells were infected with MVAGKT7, a highly host-restricted strain of vaccinia virus MVA that expresses the T7 polymerase (19). A mixture of the genome plasmid [pNiV(6+)], N, P, and L supporting plasmids were transfected to the infected CV-1 cells. The ratio of the plasmids used was that determined by Halpin et al. (17) using a minigenome system for NiV.
The transfected CV-1 cells were cultured for 7 days with the addition of new cells. Syncytia were successfully visible 2 days after transfection. Virus was then passaged in Vero cells (Fig. 1B2) in which it induced a large number of syncytia within 24 h, characteristic of NiV infection. The rescued NiVs (rNiVs) were further passaged in Vero cells to produce a stock. The presence of the engineered restriction site between the N and P genes was confirmed by amplifying this region by RT-PCR and sequencing (data not shown). The recombinant virus expressing EGFP (rNiV-EGFP) was also recovered by using the same procedure (Fig. 1B3). The expression of EGFP in the rNiV-EGFP-infected cells was verified by using fluorescence microscopy (Fig. 1B4). The fluorescence was stably detected after the rNiV-EGFP was grown for three passages in cell culture. The extent of the cytopathic effect (CPE) induced by rNiV or rNiV-EGFP was similar to that of their parental NiV. In the construction in which we engineered a restriction site into the leader sequence [pNiV(7+)] (1), we failed to rescue the virus despite numerous attempts.
Replication and Pathogenicity of rNiV.
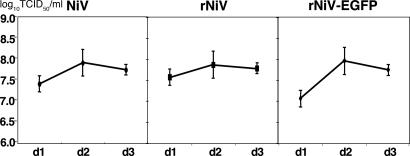
The replication of rNiV and rNiV-EGFP in Vero cells at a multiplicity of infection of 0.01 pfu per cell was compared with that of the parental NiV. The growth curves of the three viruses show that they all reached their maximum titer at 48 h postinfection and replicated at similar rates giving approximately the same maximum titers, although the titer of the rNiV-EGFP on day 1 was slightly lower than for the other two viruses (Fig. 2). Because the viral RNA polymerase of paramyxoviruses (P and L) initiates transcription at the 3′ end and the efficiency of reinitiation of transcription at the boundary of each gene is not perfect, the transcription level decreases toward the 5′ end (20, 21). Therefore, the introductions of foreign gene between N and P genes may reduce the expression level of the downstream genes without altering the expression level of the upstream N gene. In this study, it was shown that the insertion of short foreign gene (≈0.8 kbp) between N and P genes did not affect the rate of NiV replication.
Fig. 2.
Comparison of the replication in Vero cells of the parent WT and recombinant viruses, rNiV and rNiV-EGFP. Vero cells were infected with the parental WT NiV, rNiV, and rNiV-EGFP at a multiplicity of infection of 0.01 pfu per cell for 1 h. Samples of the cell medium were taken at the times indicated for the determination of virus titer. Values means ± SD from three experiments.
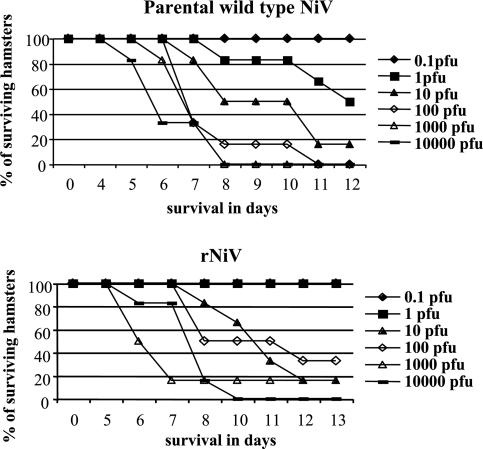
To study whether the introduction of the restriction sites introduced into the infectious clone of rNiV affected its virulence, we compared the infection of rNiV and its parent virus in a golden hamster model (22). Eight-week-old animals (six per group) were inoculated with 10-fold dilutions of either the parental WT virus or the rNiV (Fig. 3). The rNiV and the parental virus induced encephalitis and death at similar rates in the hamsters over the virus dose range studied.
Fig. 3.
Survival curves of hamsters infected by different amounts of parental WT NiV and rNiV. Hamsters (six per group) were inoculated i.p. with 10-fold dilutions of either NiV or rNiV.
Host Range of NiV Characterized by the rNiV-EGFP.
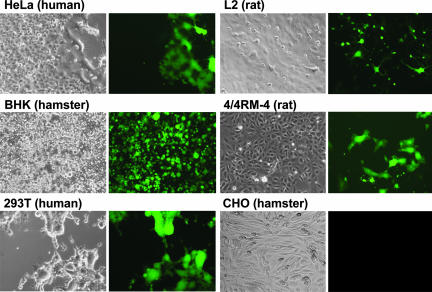
The rNiV-EGFP virus was used to investigate the host range of NiV. After infecting different cell lines (0.01 pfu per cell) derived from human, hamster, rat, and mice, we studied the CPE and analyzed the cells by fluorescence. All three viruses (NiV, rNiV, and rNiV-EGFP) produced large multinucleate giant cells in Vero, HeLa, and 293T cells, and a moderate size of CPE in 4/4RM-4 cells. However, the size of CPE was much smaller in BHK21 cells, and both size and number of CPE were markedly reduced in L2 cells. CPE was apparent after 1 day in most of these cells but was delayed by 24 h in L2 and 4/4RM-4 cells. The expression of the GFP, observed by fluorescence, appeared simultaneously and paralleled the CPE, including the delay in L2 and 4/4RM-4 cells. Using the above CPE and fluorescence criteria, no infection was observed in CHO, 208f, or P815 cells. Typical examples of CPE and fluorescence in the different cells are shown in Fig. 4.
Fig. 4.
Infection of different cell lines with rNiV-EGFP. Cells were infected with rNiV-EGFP at a multiplicity of infection of 0.01 pfu per cell and observed 48 h later, either by light microscopy or by fluorescence. The rNiV-GFP produced large multinucleate giant cells in HeLa and 293T cells and a moderate size of the CPE in 4/4RM-4 cells, but the size of the CPE was much smaller in BHK, and the size and number were significantly reduced in L2 cells. The expression of the EGFP, observed by fluorescence, appeared simultaneously and paralleled the CPE. Using the above CPE and fluorescence criteria, no infection was observed in CHO cells.
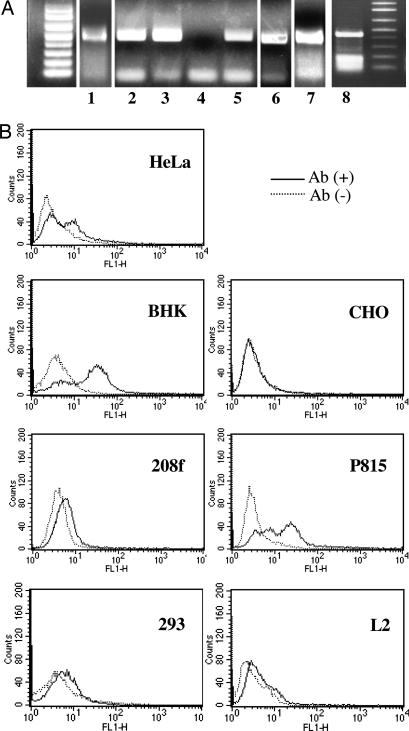
Recently, ephrin B2 was identified as a cellular receptor for Nipah and Hendra viruses (23, 24). To examine whether the presence of this receptor correlated with our observations of permissibility with our rNiV-EGFP, we tested by RT-PCR the presence of ephrin B2 mRNA. Oligo(dT) was used for reverse transcription priming. The primers except for P815 cells were designed to amplify the region nucleotides 82–572 of human ephrin B2 gene, and primers for P815 were designed to amplify the region nucleotides 534–952 of mouse ephrin B2. The expected size of the amplified fragments was ≈490 and 420 bp, respectively. With the exception of two cell lines, 208f and P815, there was a correlation between the expression of the mRNA and rNiV-EGFP replication (Fig. 5A). To confirm surface expression of ephrin B2 on the different cells, we also performed flow cytometry analysis. From the results, it was clearly shown that the 208f and P815 cells also express ephrin B2 on the cell surfaces (Fig. 5B). CHO cells did not express ephrin B2. These results are summarized in Table 1.
Fig. 5.
Expression of ephrinB2 in different cell lines. (A) RT-PCR was performed to test for the presence of mRNA to ephrin B2. The PCR products (upper bands) were detected in lane HeLa (lane 1), 293 (lane 2), BHK (lane 3), 208f (lane 5), L2 (lane 6), 4/4RM4 (lane 7), and P815 (lane 8), but not in CHO (lane 4). (B) Ephrin B2 expression was measured by flow cytometry on the cell surface of each cell line. The data showed that all of the tested cell lines except for CHO expressed ephrin B2.
Table 1.
Permissivity of different cell lines to NiV infection and the presence of ephrin B2
| Cells | Species tissue | Ephrin B2 | Virus growth |
|---|---|---|---|
| BHK | Hamster kidney | + | + |
| 293T | Human endothelial | + | + |
| HeLa | Human uterus | + | + |
| CHO | Hamster ovary | − | − |
| P815 | Mouse mast cells | + | − |
| 208f | Rat embryonic fibroblasts | + | − |
| L2 | Rat lung epithelial | + | + |
| 4/4RM4 | Rat epithelial | + | + |
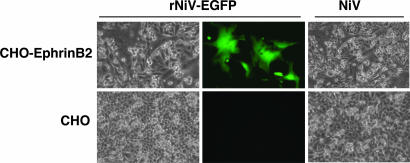
Previous studies by the Lee laboratory have shown that NiV-F/G pseudotyped vesicular stomatitis viruses could infect nonpermissive cells such as CHO after they were transfected with a human ephrin B2 plasmid (24). We therefore examined whether such transfected CHO cells would be permissive to NiV infection. One day after transfection with a plasmid that expresses the human ephrin B2 (OriGene Technologies, Rockville, MD), CHO cells were inoculated with the rNiV-EGFP. Expression of the EGFP as well as large CPE in the transfected CHO cells was well observed 24 h after the infection (Fig. 6). Thus, in CHO cells, the presence of human ephrin B2 renders them permissive for NiV.
Fig. 6.
NiV infection of CHO cells transfected with a human ephrin B2 expression plasmid. CHO cells were transfected with a plasmid expressing human ephrin B2 and 1 day later were infected with either the WT NiV or rNiV-EGFP (0.1 pfu per cell). One day later, the cells were observed for fluorescence and morphology.
Discussion
In 1994, HeV was the first member of the newly classified Henipavirus genus to be isolated (25). Although a large proportion of certain fruit bats were shown to be seropositive for this virus (26, 27), there was little cross-species contamination. However, epidemics of the closely related NiV in Malaysia in 1998 showed the virus to have greater repercussions on the economic and health situation (28). Subsequent studies have shown that NiV is widespread throughout Asia and may even produce annual epidemics in countries such as Bangladesh (6, 10). The viruses involved in the outbreaks incurred mortality rates in humans varying from 40% to 70% and can be distinguished by nucleic acid sequencing (29, 30). To analyze the different parameters involved in the disease induced by the henipaviruses, we developed an animal model in hamsters (22). The disease induced in these animals is similar to that observed in man. To determine the contribution of the individual viral proteins to the pathogenesis of the disease, it was necessary to develop the reverse genetics technology for NiV. Although many clinically significant viral pathogens including newly emerged viruses, such as Ebola, Marburg, Hendra, and Nipah viruses, belong to the negative and single-stranded nonsegmented RNA viruses, the mechanisms for the severe pathogenicity and for crossing species barrier are not known. The studies based on the new technology of reverse genetics for the minus-stranded RNA viruses over the last several years have had a dramatic effect in expanding our knowledge of the negative-stranded RNA viruses and in the development of recombinant vaccines including emerging viruses (31–36). In the present study, a rescue system was established that enabled the generation of infectious recombinant NiVs. Our strategy was based on one that we had developed previously for morbilliviruses (37) that was similar to previously reported systems for other viruses. Despite our success with the two recombinants [pNiV(6+) and pNiV-EGFP], we failed to rescue a third construction in which a restriction site was included at the end of the leader sequence. Our previous studies with morbilliviruses using similar constructions were successful.
The rNiV-EGFP produced in this study is useful for analyses of permissibility of cells for NiV infection. Although we have only grown the recombinant viruses for three passages in cell culture, many similar constructs based on negative-strand viruses have shown that expression from such genes is very stable in vitro (28, 35, 38). Expression of fluorescence from EGFP-expressing morbilliviruses produced in our laboratory is stable at least for 20 passages (data not shown). Therefore, the EGFP within the NiV in the present study may be also quite stable. Using the rNiV-EGFP, we showed that infection could be followed in a variety of cell lines. The fluorescence marker correlated with the development of the CPE. All permissive cell lines expressed the receptor ephrin B2. However, the rat cell line 208f and the mouse cell line P815, which express ephrin B2, were not permissive. In addition, although two other rat cell lines, L2 and 4/4RM4, were ephrin B2-positive and -permissive, the efficiency of virus replication in them seemed to be markedly lower than that in human cells, HeLa or 293T, as well as in the hamster cell line CHO with induced human ephrin B2 expression. These results suggested that factors other than receptors may also be involved in the control of NiV replication.
The availability of the NiV infectious clone, which retains its virulence and pathological properties in the golden hamster model, will enable us to extend our studies to define viral pathological determinants. In addition to these aspects, it will be interesting to determine which viral factors are responsible for the increase in virulence when the virus crosses the species barrier as revealed in our previous studies with morbilliviruses (39, 40).
Materials and Methods
Cells and Viruses.
Vero (monkey kidney), CV-1 (monkey kidney), HeLa (human uterus), BHK21 (baby hamster kidney), 293T (human kidney), and CHO (Chinese hamster ovary) cells were maintained in DMEM (Invitrogen GIBCO, Grand Island, NY) containing 5% FBS, l-glutamine, and antibiotics. L2 (epithelial cells derived from rat lung), 4/4RM-4 (epithelium-like cells derived from visceral pleura of Fischer rats), 208f (fibroblast cells derived from embryos of Fischer rats), and P815 (mouse mast cells) were maintained in RPMI medium 1640 supplemented with 5% FBS, l-glutamine, and antibiotics. The MVAGKT7 recombinant vaccinia virus strain that expresses the bacteriophage T7 RNA polymerase gene was provided by G. Sutter (National Research Centre for Environment and Health, Oberschleissheim, Germany). Because NiV is classified as a class 4 agent, all infectious virus manipulations were performed in the Jean Mérieux BSL-4 Laboratory in Lyons, France. NiV isolated from the cerebrospinal fluid of a patient was provided by Kaw Bing Chua (University of Malaya, Kuala Lumpur, Malaysia). The complete nucleotide sequence of this virus is deposited as GenBank entry AY029767. Virus stocks were grown in Vero cells, and the virus used was the fifth passage on Vero cells after isolation. The virus titer of the stock was 3.2 × 107 TCID50/ml.
Construction of Plasmids.
NiV RNA was extracted from infected cells as described in ref. 32. RT-PCR was performed by using SuperScript II reverse transcriptase (Invitrogen, Carlsbad, CA). All cloning procedures were conducted by following protocols. To clone the full genome of the NiV, we designed a large number of primer pairs based on the NiV sequence in GenBank (accession no. AY029767). PCR amplifications were performed by using LA Taq DNA polymerase (Takara) or Pfu DNA polymerase (Stratagene, La Jolla, CA). PCR products were first cloned into pGEM-T easy (Promega, Madison, WI) and then subcloned into pKS, pGEM, or pMDB1. We obtained at least four clones from each amplification and confirmed that the sequence in each was identical. The fragments were joined by using internal enzyme sites, and the sequence of the joined fragments was confirmed. The leader and trailer sequences were amplified by using primers including EagI and EcoRI sites (leader) and EcoRI and BsmI sites (trailer). Each fragment was digested by EcoRI and EagI or BsmI, and cloned into pMDB1 by using the EcoRI and EagI or BsmI sites, respectively. Amplification of the six NiV genes was performed with primers containing unique restriction sites: N (NotI–FseI), P (FseI–PmeI), M (PmeI–MluI), F (MluI–SgfI), G (SgfI–AscI), and L (AscI–AgeI) (Fig. 1A). These six unique restriction enzyme sites were designed for future use. All amplified fragments were cloned into pGEM-T Easy (Invitrogen). The NiV genes were excised with the two appropriate enzymes within the pMDB1-MV plasmid. Finally, the assembled genes were excised with NotI and AgeI and were inserted into the plasmid pMDB1 with the leader and trailer sequences. The resulting plasmid was designated pNiV(7+). A second construction, pNiV(6+), was also made without the restriction enzyme recognition site in its leader sequence containing the original viral sequence. The complete cloned genome was sequenced. Three nucleotides changes (3022 C-T, 9248 C-T, and 11564 G-A) found compared with the parent virus were mutated back to the original published sequence.
For the construction of the full-length genome plasmid to express the EGFP, the EGFP gene was amplified from pEGFP-N1 (Clontech) by using the following primers. EGFP-F, 5′-GAGCTCATGGTGAGCAAGGGCGAGGA-3′ (SacI site in italics); and reverse primer EGFP-R, 5′-GGCCGGCCTATATCTACTTGTACAGCTCGTCCATGCC-3′ (FseI site in italics; additional five nucleotides for rule of six in boldface). The intergenic region between the N and P junction was amplified by using the following primers. NP-F, GGCCGGCCTCCAATATTCTA (FseI site in italics); and reverse primer NP-R, GAGCTCCATTGGATGAATTGTTATTA (SacI site in italics). The PCR products were cloned into pGEM-T Easy. The EGFP fragment was inserted downstream of the N-P intergenic region, followed by digestion by SacI. Finally, the fragment of EGFP connected to the N-P intergenic region was cloned into the FseI site of the pNiV(6+) (pNiV-EGFP).
To construct supporting plasmids for virus rescue, the sequence coding for the N protein was amplified by PCR with primers containing NotI and KpnI, and that for the P protein was amplified with primers containing BamHI and XhoI. Both PCR products were digested with NotI and KpnI or BamHI and XhoI, respectively, and cloned into a pKS(+) vector. The coding sequence for the L protein, to which NcoI and NotI were added, was generated in four cloning steps by using a pGEM-T Easy vector and was then cloned into pGEM5zf(+).
Recovery of Viruses from cDNA.
CV-1 cells were seeded into six-well plates (2 × 105 cells per well) 1 day before infection and transfection. The cells were infected with replication-deficient MVAGKT7 vaccinia virus in DMEM supplemented with 2% FBS 1 h before transfection. Before transfection, 28.4 μl of FuGENE 6 (Roche, Basel, Switzerland) was mixed and incubated with 300 μl of serum-free DMEM for 5 min. Plasmids (7 μg of pNiV and the plasmids encoding transacting proteins, 1.25 μg of pKS-N, 0.8 μg of pKS-P, and 0.4 μg of pGEM-L) were mixed into 100 μl of serum-free DMEM. MVAGKT7 was removed from the cells and replaced with 2 ml of maintenance medium containing the plasmids and FuGene 6. Three days later, 1.5 × 105 CV-1 cells per well were added. After 7 days, 500 μl of the supernatant was removed and added to a confluent monolayer of CV-1 or Vero-E6 cells in a 75-cm2 flask. When an advanced CPE was observed (after 1–2 days), the cells and medium were harvested and stored at −80°C.
Virus Growth.
Vero cells (1 × 106 per six-well plate) were infected with NiV, rNiV, or recombinant NiV expressing EGFP (rNiV-EGFP) at a multiplicity of infection of 0.01 for 1 h. The inoculum was removed, and the cells were washed once with medium and then incubated in DMEM plus 2% FBS. Cells and supernatants of wells infected with these viruses were harvested immediately, 24, 48, and 72 h later, centrifuged, and stored at −80°C. The TCID50/ml of samples was measured by standard methods. The experiment was repeated three times.
Infection of Hamsters.
Eight-week-old golden hamsters (Mesocricetus auratus) were injected i.p. with NiV after anesthetization with isoflurane (Aerrane; Baxter Healthcare, Old Toongabbie, New South Wales, Australia). The animals were housed in ventilated containers equipped with HEPA filters in the BSL-4 laboratory and were individually identified by using microchips.
Expression of Ephrin B2 in Various Cell Types.
Total RNA was extracted from HeLa, BHK, 293, L2, 4/4RM-4, 208f, CHO, and P815 cells by using the commercial reagent ISOGEN (Nippon Gene, Tokyo, Japan). Subsequently, single-stranded DNA was synthesized by reverse transcription, using SuperScript II (Invitrogen GIBCO) with oligo(dT) primer. The cDNA corresponding to the selected region of ephrin B2 was amplified by RT-PCR. The primers for the cells, except for P815, were designed to amplify the region nucleotides 82–572 of human ephrin B2 gene, and primers for P815 were designed to amplify the region nucleotides 534–952 of mouse ephrin B2.
HeLa, 293, BHK, CHO, L2, 208f, and P815 cells were stained with mouse anti-human ephrin B2 polyclonal antibody and analyzed by using flow cytometry. Cells were also stained with an anti-ephrin B2 antibody (P-20 from Santa Cruz Biotechnology, Santa Cruz, CA) followed by an Alexa Fluor 488-conjugated goat anti-rabbit IgG secondary antibody (Molecular Probes, Eugene, OR). FACS analysis was carried out by using a FACSCalibur machine (Becton Dickinson, San Jose, CA). The data were acquired and analyzed with CellQuest software (Becton Dickinson). Cells that were not stained with antibody were used as the negative control.
The plasmid expressing human ephrin B2 (OriGene Technologies) was transfected into CHO cells, a line that is not susceptive to NiV infection. One day after transfection, the cells were infected with rNiV-EGFP
Acknowledgments
We thank G. Sutter for providing the recombinant vaccinia virus strain and Kaw Bing Chua for providing the NiV isolated from the cerebrospinal fluid of a patient. Greatly acknowledged is the help of the Institut National de la Santé et de la Recherche Médicale Jean Mérieux P4 laboratory staff, without whom this study could not have been undertaken. This work was supported by grants-in-aid from the Ministry of Education, Science, Culture, and Sports of Japan.
Abbreviations
- CPE
cytopathic effect
- HeV
Hendra virus
- NiV
Nipah virus
- rNiV
rescued NiV.
Footnotes
The authors declare no conflict of interest.
References
- 1.Chua KB, Goh KJ, Wong KT, Kamarulzaman A, Tan PS, Ksiazek TG, Zaki SR, Paul G, Lam SK, Tan CT. Lancet. 1999;354:1257–1259. doi: 10.1016/S0140-6736(99)04299-3. [DOI] [PubMed] [Google Scholar]
- 2.Chua KB, Bellini WJ, Rota PA, Harcourt BH, Tamin A, Lam SK, Ksiazek TG, Rollin PE, Zaki SR, Shieh W, et al. Science. 2000;288:1432–1435. doi: 10.1126/science.288.5470.1432. [DOI] [PubMed] [Google Scholar]
- 3.Harcourt BH, Lowe L, Tamin A, Liu X, Bankamp B, Bowden N, Rollin PE, Comer JA, Ksiazek TG, Hossain MJ, et al. Emerg Infect Dis. 2005;11:1594–1597. doi: 10.3201/eid1110.050513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harcourt BH, Tamin A, Halpin K, Ksiazek TG, Rollin PE, Bellini WJ, Rota PA. Virology. 2001;287:192–201. doi: 10.1006/viro.2001.1026. [DOI] [PubMed] [Google Scholar]
- 5.Choi C. Sci Am. 2004;291:21A–22A. [PubMed] [Google Scholar]
- 6.Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, Niezgoda M, Rupprecht C, Bresee J, Breiman RF. Emerg Infect Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Centre for Diarrhoeal Disease Research; Bangladesh. Health Sci Bull. 2004;2:7–11. [Google Scholar]
- 8.International Centre for Diarrhoeal Disease Research; Bangladesh. Health Sci Bull. 2004;2:5–9. [Google Scholar]
- 9.Butler D. Nature. 2004;429:7. doi: 10.1038/429007b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enserink M. Science. 2004;303:1121. doi: 10.1126/science.303.5661.1121b. [DOI] [PubMed] [Google Scholar]
- 11.Büchen-Osmond C. Arch Virol. 2004;147:1655–1656. [Google Scholar]
- 12.Hooper P, Zaki S, Daniels P, Middleton D. Microbes Infect. 2001;3:315–322. doi: 10.1016/s1286-4579(01)01385-5. [DOI] [PubMed] [Google Scholar]
- 13.Harcourt BH, Tamin A, Ksiazek TG, Rollin PE, Anderson LJ, Bellini WJ, Rota PA. Virology. 2000;271:334–349. doi: 10.1006/viro.2000.0340. [DOI] [PubMed] [Google Scholar]
- 14.Wang LF, Yu M, Hansson E, Pritchard LI, Shiell B, Michaiski WP, Eaton BT. J Virol. 2000;74:9972–9979. doi: 10.1128/jvi.74.21.9972-9979.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu M, Hansson E, Langedijk JP, Eaton BT, Wang LF. Virology. 1998;251:227–233. doi: 10.1006/viro.1998.9302. [DOI] [PubMed] [Google Scholar]
- 16.Yu M, Hansson E, Shiell B, Michalski W, Eaton BT, Wang LF. J Gen Virol. 1998;79:1775–1780. doi: 10.1099/0022-1317-79-7-1775. [DOI] [PubMed] [Google Scholar]
- 17.Halpin K, Bankamp B, Harcourt BH, Bellini WJ, Rota PA. J Gen Virol. 2004;85:701–707. doi: 10.1099/vir.0.19685-0. [DOI] [PubMed] [Google Scholar]
- 18.Volchkov VE, Volchkova VA, Muhlberger E, Kolesnikova LV, Weik M, Dolnik O, Klenk HD. Science. 2001;291:1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 19.Kovacs GR, Parks CL, Vasilakis N, Udem SA. J Virol Methods. 2003;111:29–36. doi: 10.1016/s0166-0934(03)00132-0. [DOI] [PubMed] [Google Scholar]
- 20.Lamb RA, Kolakofsky D. In: Fields Virology. 4th Ed. Fields BN, Knipe DM, Howley PM, Chanock RM, Monath TP, Melnick JL, Roizman B, Straus SE, editors. New York: Lippincott-Raven; 1996. p. 1307. [Google Scholar]
- 21.Nagai Y. Rev Med Virol. 1999;9:83–99. doi: 10.1002/(sici)1099-1654(199904/06)9:2<83::aid-rmv244>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 22.Wong KT, Grosjean I, Brisson C, Blanquier B, Fevre-Montange M, Bernard A, Loth P, Georges-Courbot MC, Chevallier M, Akaoka H, et al. Am J Pathol. 2003;164:2127–2137. doi: 10.1016/S0002-9440(10)63569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonaparte MI, Dimitrov AS, Bossart KN, Crameri G, Mungall BA, Bishop KA, Choudhry V, Dimitrov DS, Wang LF, Eaton BT, Broder CC. Proc Natl Acad Sci USA. 2005;102:10652–10657. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Negretta OA, Levroney EL, Aguilar HC, Bertolotti-Ciarlet A, Nazarian R, Tajyar S, Lee B. Nature. 2005;436:401–405. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- 25.Murray K, Rogers R, Selvey L, Selleck P, Hyatt A, Gould A, Gleeson L, Hooper P, Westbury H. Emerg Infect Dis. 1995;1:31–33. doi: 10.3201/eid0101.950107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chua KB, Koh CL, Hooi PS, Wee KF, Khong JH, Chua BH, Chan YP, Lim ME, Lam SK. Microbes Infect. 2002;4:145–151. doi: 10.1016/s1286-4579(01)01522-2. [DOI] [PubMed] [Google Scholar]
- 27.Yob JM, Field H, Rashdi AM, Morrissy C, van der Heide B, Rota P, bin Adzhar A, White J, Danieels P, Jamaluddin A, Ksiazek T. Malaysia Emerg Infect Dis. 2001;7:439–441. doi: 10.3201/eid0703.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mebastsion T, Schnell MJ, Cox JH, Finke S, Conzelmann K. Proc Natl Acad Sci USA. 1996;93:7310–7314. doi: 10.1073/pnas.93.14.7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abubakar S, Chang LY, Ali AR, Sharifah SH, Yusoff K, Zamrod Z. Emerg Infect Dis. 2004;10:2228–2230. doi: 10.3201/eid1012.040452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan YP, Chua KB, Kou CL, Lim ME, Lam SK. J Gen Virol. 2001;82:2151–2155. doi: 10.1099/0022-1317-82-9-2151. [DOI] [PubMed] [Google Scholar]
- 31.Enterlein S, Volchkov V, Weik M, Kolesnikova L, Volchkova V, Klenk HD, Muhlberger E. J Virol. 2006;80:1038–1043. doi: 10.1128/JVI.80.2.1038-1043.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Radecke F, Spielhofer P, Schneider H, Kaelin K, Huber M, Dotsch C, Chiristiansen G, Billeter MA. EMBO J. 1995;14:5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakamura T, Peng KW, Harvey M, Greiner S, Lorimer IA, James CD, Russell SJ. Nat Biotechnol. 2005;23:209–214. doi: 10.1038/nbt1060. [DOI] [PubMed] [Google Scholar]
- 34.Neumann G, Brownlee GG, Fodor E, Kawaoka Y. Curr Top Microbiol Immunol. 2004;283:121–143. doi: 10.1007/978-3-662-06099-5_4. [DOI] [PubMed] [Google Scholar]
- 35.Singh M, Cattaneo R, Billeter M. J Virol. 1999;73:4823–4828. doi: 10.1128/jvi.73.6.4823-4828.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walpita P, Flick R. FEMS Microbiol Lett. 2005;244:9–18. doi: 10.1016/j.femsle.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 37.Fujita K, Miura R, Yoneda M, Shimizu F, Sato H, Muto Y, Endo Y, Tsukiyama-Kohara K, Kai C. Virology. doi: 10.1016/j.virol.2006.09.018. in press. [DOI] [PubMed] [Google Scholar]
- 38.Baron MD, Foster-Cuevas M, Baron J, Barrett T. J Gen Virol. 1999;80:2031–2039. doi: 10.1099/0022-1317-80-8-2031. [DOI] [PubMed] [Google Scholar]
- 39.Yoneda M, Bandyopadhyay SK, Shiotani M, Fujita K, Nuntaprasert A, Miura R, Baron MD, Barrett T, Kai C. J Gen Virol. 2002;83:1457–1463. doi: 10.1099/0022-1317-83-6-1457. [DOI] [PubMed] [Google Scholar]
- 40.Yoneda M, Miura R, Barrett T, Tsukiyama-Kohara K, Kai C. J Virol. 2004;78:6676–6681. doi: 10.1128/JVI.78.12.6676-6681.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]