Abstract
Mutants of attenuated Bacillus anthracis with high-level ciprofloxacin resistance were isolated using a three-step in vitro selection. Ciprofloxacin MICs were 0.5 μg/ml for first-step mutants, which had one of two gyrA quinolone resistance-determining region (QRDR) mutations. Ciprofloxacin MICs were 8 and 16 μg/ml for second-step mutants, which had one of three parC QRDR mutations. Ciprofloxacin MICs for third-step mutants were 32 and 64 μg/ml. Mutants for which MICs were 64 μg/ml had one of two additional mutations within the gyrA QRDR or one of two mutations within the gyrB QRDR. Mutants for which MICs were 32 μg/ml had no additional target modifications but showed evidence of enhanced ciprofloxacin efflux.
Bacillus anthracis is a spore-forming zoonotic pathogen that occasionally infects humans, causing cutaneous, intestinal, or pulmonary forms of anthrax (9, 11). Although all three human disease forms are rare, the potential for using B. anthracis as a biological weapon makes development of antimicrobial resistance a particularly relevant concern. The two recommended therapeutics for human anthrax are doxycycline (DOX) and ciprofloxacin (CIP) (3, 4, 11). Natural resistance to CIP and DOX is undocumented (4, 5, 6); however, resistance to each has been obtained in vitro (2, 22). DOX resistance was conferred on B. anthracis by transfection with the pBC16 plasmid carrying the tetracycline resistance gene, tet (22). CIP resistance was selected through serial passage, though the genotypic determinants eliciting resistance were not characterized (2).
The bactericidal action of CIP results from the binding of gyrase-DNA and topoisomerase IV-DNA complexes and the release of DNA with double-stranded breaks (for review, see references 7 and 21). Most fluoroquinolone-resistant mutants have amino acid changes in quinolone resistance-determining regions (QRDRs) of the GyrA subunit of gyrase and the ParC subunit of topoisomerase IV. However, resistance can also arise from the overexpression of multidrug transporters and residue changes in the QRDRs of the GyrB and ParE subunits of gyrase and topoisomerase IV. Low-level resistance can be acquired with a single missense mutation within a QRDR or a point mutation in the regulatory region of an efflux pump, but high-level resistance requires a combination of mutations. The stepwise accumulation of QRDR mutations required for high-level CIP resistance follows a species-specific pathway in vitro (8, 19). However, the utility of these in vitro studies for predicting the progression of a given species to a high-level fluoroquinolone-resistant phenotype in vivo is not clear (12, 25).
In order to characterize CIP resistance determinants and mutation rates in B. anthracis, we used an in vitro stepwise selection procedure (8) to develop high-level CIP-resistant mutants. Mutation rates were determined using a Luria-Delbruck model (15), and genotypes of resistant strains were determined at each step. CIP MICs were determined for each unique mutant. Finally, multidrug efflux inhibitors were used to test for enhanced CIP efflux.
Stepwise selection and isolation of high-level CIP-resistant mutants.
Spontaneous CIP-resistant mutants of the attenuated B. anthracis ΔANR strain (plasmid-cured Ames strain) were selected in a three-step process using standard microbiological techniques. Colonies from blood agar plates were used to inoculate culture tubes containing 5 ml of Mueller-Hinton (MH) broth (Difco). Cultures were incubated overnight at 37°C and then transferred to 0.45-μm-pore-size nitrocellulose membrane filters (Millipore). Membranes were placed cell side up onto MH agar containing CIP at three to four times the MIC for the parent strain (8) and incubated for ∼40 h. A single colony from each positive plate was cataloged (either as a frozen stock or as a spore stock) and analyzed for topoisomerase mutations in the gyrA and parC QRDRs by fluorescent DNA sequence analysis (gyrB and parE QRDRs were analyzed at the end of the study). QRDRs were amplified by PCR using primers designed from the incomplete B. anthracis genome sequence (Table 1; The Institute for Genomic Research, Rockville, Md.). Fifty-microliter PCRs were prepared in PCR buffer (20 mM Tris [pH 8.4], 50 mM KCl) (Gibco) using 0.10 mM deoxynucleoside triphosphates, 2 mM MgCl2, ∼5 ng of template DNA prepared as described previously (14), 0.04 U of Taq DNA polymerase/μl (Gibco), and 0.2 μM forward and reverse primers. Reactions were heated to 94°C for 5 min and then cycled 35 times at 94, 60, and 72°C for 20 s at each temperature. PCR products were sequenced on either an ABI377 or an ABI3100 fluorescent sequencer using the ABI PRISM Ready Reaction BigDye terminator cycle sequencing kit according to the manufacturer’s specifications (Applied Biosystems). The most common unique genotype from each selection step was used for subsequent selections until high-level CIP-resistant strains were identified.
TABLE 1.
Primers used in this study
| Name | Sequence (5′ → 3′) | QRDR gene |
|---|---|---|
| ParCQRDR1F | GTGTTAGGTGACCGCTTTGCACGTTATAGTAAATA | parC |
| ParCQRDR1R | GTAAAACAACCGGTTCTTCACTCGTATCATC | parC |
| GyrAQRDR1F | ACGTATTAATTCCATAGAGATTTTAGACATTCTTGCTTCTGTATA | gyrA |
| GyrAQRDR1R | CATTTTTAGATTACGCAATGAGTGTTATCGTATCTCG | gyrA |
| gyrAQRDR1 - 03F | ACGCAATGAGTGTTATCGTATCT | gyrA |
| gyrAQRDR1 - 03R | AATATCGGGATTATGACTTA | gyrA |
| parCQRDR1 - 03F | CTCCCGCTTGAAGACGTGTTAGGT | parC |
| parCQRDR1 - 03R | AACCGGTTCTTCACTCGTAT | parC |
| parEQRDR1 - 03F | GCCATTGTATCAGAGCATTTAGCTTACTTTT | parE |
| parEQRDR1 - 03R | ATCGGTCATGATTACAACTTTATCGTA | parE |
| gyrBQRDR1 - 03F | AGAGGCATTTGAAAAGTTCTTACTA | gyrB |
| gyrBQRDR1 - 03R | CAATAATTTGACGCATATAACGATAGA | gyrB |
Susceptibility testing.
MICs were determined by the agar dilution method. Cultures were grown overnight on MH agar supplemented with 5% sheep blood. Colonies were suspended in MH broth to a density equivalent of a 0.5 McFarland standard. Two microliters of this suspension was dropped onto agar dilution plates. Once the spots had been absorbed, the plates were inverted and incubated for 24 h at 35°C. B. anthracis ΔANR was used as the reference strain for determinations of MICs for mutants.
Mutation rate estimation.
Mutation rates for first-, second-, and third-step CIP-resistant mutants were estimated with 96 independent cultures of B. anthracis ΔANR, S1-1, and S2-1, respectively (Table 2). A single colony of the starting isolate was suspended in Luria-Bertani (LB) broth and used to inoculate each of the independent cultures with approximately 1,000 cells. For first- and third-step mutants, 96 1-ml cultures were grown in LB broth in four 24-well plates (Costar). For step 2, 96 100-μl cultures were grown in LB broth in a single 96-well plate (Costar). All plates were incubated overnight at 37°C in a G24 environmental incubator shaker (New Brunswick Scientific) with shaking at 225 rpm. Six cultures were chosen at random for each step and used to determine the average total number of cells present in each culture. The remaining 90 cultures were plated onto MH plates with CIP concentrations of 0.25, 1.5, and 24 μg/ml for steps 1, 2, and 3, respectively. For step 2, the 100-μl cultures were plated directly. For steps 1 and 3, the 1-ml cultures were transferred to sterile 1.5-ml microcentrifuge tubes and centrifuged at 3,000 × g for 5 min. Approximately 850 μl of the supernatant was removed, and the pellet was resuspended in the remaining broth and plated. All of the plates were incubated at 37°C for ∼48 h. Up to four putative resistant colonies from each positive plate were transferred to fresh selective medium and incubated at 37°C for ∼48 h to confirm resistance. The number of plates devoid of resistant mutants represents zero mutational events. This value was used with the cell count in the Poisson distribution to estimate the mutation rate for each step (15).
TABLE 2.
Mutants identified in this study
| Straina | CIP MIC (μg/ml) | Mutation rate | Frequency (%) |
gyrA mutationb
|
parC mutationb
|
gyrB mutation
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Nucleotide | Amino acid | Nucleotide | Amino acid | Nucleotide | Amino acid | ||||
| ΔANR | 0.06 | —d | — | — | — | — | — | — | — |
| S1-1 | 0.5 | 5.3 × 10−10 | 80 | C254→T | S85→L | — | — | — | — |
| S1-2 | 0.5 | 1.3 × 10−10 | 20 | G265→A | E89→K | — | — | — | — |
| S2-1 | 8 | 7.3 × 10−9 | 73 | C254→T | S85→L | C242→T | S81→F | — | — |
| S2-2 | 8 | 1.6 × 10−9 | 16 | C254→T | S85→L | C242→A | S81→Y | — | — |
| S2-3 | 16 | 1.1 × 10−9 | 11 | C254→T | S85→L | G253→A | E85→K | — | — |
| S3-1c | 32 | 3.1 × 10−10 | 65 | C254→T | S85→L | C242→T | S81→F | — | — |
| S3-6 | 64 | 6.7 × 10−11 | 14 | C254→T | S85→L | C242→T | S81→F | A1423→G | N475→D |
| S3-8 | 64 | 3.4 × 10−11 | 7 | C254→T | S85→L | C242→T | S81→F | G1309→A | D437→N |
| S3-11 | 64 | 3.4 × 10−11 | 7 | C254→T | S85→L | C242→T | S81→F | — | — |
| G265→A | E89→K | ||||||||
| S3-16 | 64 | 3.4 × 10−11 | 7 | C254→T | S85→L | C242→T | S81→F | — | — |
| A266→C | E89→A | ||||||||
Strain designations are based upon selection step, CIP MIC, and DNA sequence analysis of the QRDRs. The first part of the designation represents the step at which the strain was identified (e.g., S1-1 was isolated during the first selection step). The second part of the designation is a unique numerical identifier indicating genotype and phenotype. In some cases this designation represents more than one isolate with identical phenotypic and genotypic characteristics.
Mutations not underlined are those that were gained in the previous step(s).
S3-1 isolates are genotypically identical to the parent strain (S2-1) at gyrA, gyrB, parC, and parE QRDRs but are phenotypically distinct based on CIP MIC and INF271 susceptibility.
—, not applicable (ΔANR) or no mutation (all other strains).
Mutations and mutation rates.
The sequential selection of B. anthracis on increasing CIP concentrations resulted in a stepwise accumulation of mutations, leading to mutants for which CIP MICs were as high as 64 μg/ml (∼1,000-fold higher than that for the wild type) (Table 2). First-step mutants developed at a rate of 6.6 × 10−10 and had one of two mutations within the gyrA QRDR (Table 2). Eighty percent of these mutants possessed a C254→T missense mutation in gyrA (Table 2). (Note that other, rarer gyrA mutations were identified; however, these strains died during the cataloging process due to an asporogenic state and remain unconfirmed.) Second-step mutants developed at a rate of 1.0 × 10−8 and possessed one of three mutations within the parC QRDR (Table 2). As with the S1 mutants, one transition, C242→T, was overrepresented (73%) (Table 2). Third-step mutants developed at a rate of 4.8 × 10−10. In total, fourteen S3 mutants were isolated, nine for which CIP MICs were 32 μg/ml and five for which MICs were 64 μg/ml. Mutants for which MICs were 64 μg/ml had one of two additional mutations within the gyrA QRDR or one of two mutations within the gyrB QRDR (Table 2). Mutants for which MICs were 32 μg/ml were devoid of additional mutations within any of the topoisomerase QRDRs, gyrA, gyrB, parC and parE.
Evidence of multidrug efflux.
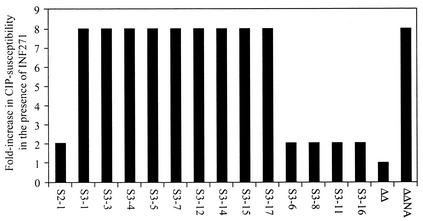
The absence of additional missense mutations in the QRDRs of many (65%) third-step mutants led to investigations into multidrug transport. Blast searches of the partial B. anthracis genome sequence with the gene sequences of the B. subtilis multidrug efflux pumps bmr (gb L25604) and blt (gb L32599) (1) revealed homologues of each. Both of these pumps are members of the major facilitator superfamily and can externalize a diverse group of chemicals, including fluoroquinolones, ethidium bromide, rhodamine dyes, and chloramphenicol (1, 17, 18). Interestingly, ethidium bromide MICs were not increased for any of the CIP-resistant mutants. However, susceptibility to CIP in the presence of the potent efflux inhibitor INF271 (20 μg/ml) was increased eightfold in the nine S3 mutants devoid of additional QRDR mutations (Fig. 1) (16). The susceptibility of the S2 parent strain and the other five S3 mutants was increased only twofold (a one- to twofold increase in CIP susceptibility was observed for all S1 and S2 strains [data not shown]). Disruption of the high-level resistant phenotype among the nine putative efflux mutants was confirmed with another structurally unrelated multidrug transport inhibitor, reserpine (Sigma) (16; data not shown).
FIG. 1.
Effect of INF271 on the susceptibility of third-step, high-level CIP-resistant B. anthracis mutants. S2-1 is the parent strain for the third-step mutants; S3-1, -3, -4, -5, -7, -12, -14, -15, and -17 are third-step mutants with no additional gyrase or topoisomerase mutations. S3-6, -8, -11, and -16 are third-step mutants with additional gyrase mutations. ΔΔ, Bacillus subtilis with inactivated blt and bmr transporter genes; ΔΔNA, B. subtilis strain ΔΔ with a functional NorA transporter from the plasmid expression vector pBEV.
The spontaneous stepwise resistance rates calculated in this study (6.6 × 10−10, 1.0 × 10−8, and 4.8 × 10−10) are similar to the rate calculated for rifampin resistance in B. anthracis (1.6 × 10−9) (24) and to those reported for fluoroquinolone resistance in other species (20, 23). These data confirm a normal mutation rate in B. anthracis and argue against a reduced mutation rate as a potential explanation for the lack of genetic diversity among B. anthracis isolates (10, 13, 14). The targeted stepwise accumulation of mutations (S1 gyrA → S2 parC) in B. anthracis indicates that the primary target of CIP is GyrA and that the secondary target is ParC.
This is the first reported evidence of efflux-based CIP resistance in B. anthracis. Further characterization of this phenomenon will provide deeper insight into the different fluoroquinolone resistance mechanisms in this important pathogen.
Acknowledgments
This project was funded by the Northern Arizona University Cowden Endowment for Microbiology.
We thank the following individuals for their contributions to this project: Timothy Read at The Institute for Genomic Research, for providing the unfinished B. anthracis genome sequence; Alexander Neyfakh at the University of Chicago, Center for Pharmaceutical Biotechnology, for kindly providing control strains and advice for the drug efflux experiments; Penelope Markham and Influx, Inc., Chicago, Ill., for generously providing INF271; Christine Tipton-Hunton for literature searches; and Michelle L. Cardon for DNA sequence analysis.
REFERENCES
- 1.Ahmed, M., L. Lyass, P. N. Markham, S. S. Taylor, N. Vazquez-Laslop, and A. A. Neyfakh. 1995. Two highly similar multidrug transporters of Bacillus subtilis whose expression is differentially regulated. J. Bacteriol. 177:3904-3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brook, I., T. B. Elliott, H. I. Pryor II, T. E. Sautter, B. T. Gnade, J. H. Thakar, and G. B. Knudson. 2001. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Int. J. Antimicrob. Agents 18:559-562. [DOI] [PubMed] [Google Scholar]
- 3.Brook, I. 2002. The prophylaxis and treatment of anthrax. Int. J. Antimicrob. Agents 20:320-325. [DOI] [PubMed] [Google Scholar]
- 4.Bryskier, A. 2002. Bacillus anthracis and antimicrobial agents. Clin. Microbial. Infect. 8:467-478. [DOI] [PubMed] [Google Scholar]
- 5.Cavallo, J. D., F. Ramisse, M. Girardet, J. Vaissaire, M. Mock, and E. Hernandez. 2002. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. Antimicrob. Agents Chemother. 46:2307-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coker, P. R., K. L. Smith, and M. E. Hugh-Jones. 2002. Antimicrobial susceptibilities of diverse Bacillus anthracis isolates. Antimicrob. Agents Chemother. 46:3843-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drlica, K., and X. Zhao. 1997. DNA gyrase, topoisomerase IV, and the 4-quinolones. Microbiol. Mol. Biol. Rev. 61:377-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrero, L., B. Cameron, and J. Crouzet. 1995. Analysis of gyrA and grlA mutations in stepwise-selected ciprofloxacin-resistant mutants of Staphylococcus aureus. Antimicrob. Agents Chemother. 39:1554-1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedlander, A. M. 1999. Clinical aspects, diagnosis and treatment of anthrax. J. Appl. Microbiol. 87:303.. [DOI] [PubMed] [Google Scholar]
- 10.Harrell, L. J., G. L. Andersen, and K. H. Wilson. 1995. Genetic variability of Bacillus anthracis and related species. J. Clin. Microbiol. 33:1847-1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inglesby, T. V., T. O'Toole, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Gerberding, J. Hauer, J. Hughes, J. McDade, M. T. Osterholm, G. Parker, T. M. Perl, P. K. Russell, K. Tonat; Working Group on Civilian Biodefense. 2002. Anthrax as a biological weapon, 2002. JAMA 288:2236-2252. [DOI] [PubMed] [Google Scholar]
- 12.Jones, M. E., D. F. Sahm, N. Martin, S. Scheuring, P. Heisig, C. Thornsberry, K. Kohrer, and F. Schmitz. 2000. Prevalence of gyrA, gyrB, parC, and parE mutations in clinical isolates of Streptococcus pneumoniae with decreased susceptibilities to different fluoroquinolones and originating from worldwide surveillance studies during the 1997-1998 respiratory season. Antimicrob. Agents Chemother. 44:462-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keim, P., A. Kalif, J. Schupp, K. Hill, S. E. Travis, K. Richmond, D. M. Adair, M. Hugh-Jones, C. R. Kuske, and P. Jackson. 1997. Molecular evolution and diversity in Bacillus anthracis as detected by amplified fragment length polymorphism markers. J. Bacteriol. 179:818-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luria, S. E., and M. Delbruck. 1943. Mutations of bacteria from virus sensitivity to virus resistance. Genetics 28:491-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Markham, P., N. E. Westhaus K. Klyachko, M. E. Johnson, and A. A. Neyfakh. 1999. Multiple novel inhibitors of the NorA multidrug transporter of Staphylococcus aureus. 43:2404-2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neyfakh, A. A. 1992. The multidrug efflux transporter of Bacillus subtilis is a structural and functional homolog of the Staphylococcus NorA protein. Antimicrob. Agents Chemother. 36:484-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neyfakh, A. A., C. M. Borsch, and G. W. Kaatz. 1993. Fluoroquinolone resistance protein NorA of Staphylococcus aureus is a multidrug efflux transporter. Antimicrob. Agents Chemother. 37:128-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng, E. Y., M. Trucksis, and D. C. Hooper. 1996. Quinolone resistance mutations in topoisomerase IV: relationship to the flqA locus and genetic evidence that topoisomerase IV is the primary target and DNA gyrase is the secondary target of fluoroquinolones in Staphylococcus aureus. Antimicrob. Agents Chemother. 40:1881-1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pan, X. S., and L. M. Fisher. 1998. DNA gyrase and topoisomerase IV are dual targets of clinafloxacin action in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:2810-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piddock, L. J. 1999. Mechanisms of fluoroquinolone resistance: an update, 1994-1998. Drugs. 58:11-18. [DOI] [PubMed] [Google Scholar]
- 22.Pomerantsev, A. P., N. A. Shishkova, and L. I. Marinin. 1992. Comparison of therapeutic effects of antibiotics of the tetracycline group in the treatment of anthrax caused by a strain inheriting tet-gene of plasmid pBC16. Antibiot. Khimioter. 37:31-34. [PubMed] [Google Scholar]
- 23.Schedletzky, H., B. Wiedemann, and P. Heisig. 1999. The effect of moxifloxacin on its target topoisomerases from Escherichia coli and Staphylococcus aureus. J. Antimicrob. Chemother. 43:31-37. [DOI] [PubMed] [Google Scholar]
- 24.Vogler, A. J., J. D. Busch, S. Percy-Fine, C. M. Tipton-Hunton, K. L. Smith, and P. Keim. 2001. Molecular analysis of rifampicin resistance in Bacillus anthracis and Bacillus cereus. J. Antimicrob. Chemother. 46:511-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weigel, L. M., G. J. Anderson, R. R. Facklam, and F. C. Tenover. 2001. Genetic analysis of mutations contributing to fluoroquinolone resistance in clinical isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:3517-3523. [DOI] [PMC free article] [PubMed] [Google Scholar]