Abstract
Burkholderia pseudomallei, the causative agent of melioidosis, is inherently resistant to a variety of antibiotics including aminoglycosides, macrolides, polymyxins, and β-lactam antibiotics. Despite resistance to many β-lactams, ceftazidime and β-lactamase inhibitor-β-lactam combinations are commonly used for treatment of melioidosis. Here, we examine the enzyme kinetics of β-lactamase isolated from mutants resistant to ceftazidime and clavulanic acid inhibition and describe specific mutations within conserved motifs of the β-lactamase enzyme which account for these resistance patterns. Sequence analysis of regions flanking the B. pseudomallei penA gene revealed a putative regulator gene located downstream of penA. We have cloned and sequenced the penA gene from B. mallei and found it to be identical to penA from B. pseudomallei.
Burkholderia pseudomallei is the causative agent of melioidosis, an endemic disease of Southeast Asia and Northern Australia (6). The severity of the disease can vary from asymptomatic infection to a severe form leading to acute sepsis and death. B. pseudomallei is a facultative intracellular pathogen which is able to survive inside phagocytic cells and thereby escape the host's humoral response. The disease can be reactivated after a very long remission (3, 5, 12). Currently, prolonged antibiotic treatment is advised to ensure complete eradication of the organism. Unfortunately, this practice creates a strong positive selection for antibiotic resistant strains resulting in many cases of treatment failure. Many reports have described successful treatment using a combination of β-lactam antibiotics and a β-lactamase inhibitor, such as amoxicillin plus clavulanic acid (19). Livermore, et al. described a clavulanic acid-inhibitable β-lactam resistance phenotype of B. pseudomallei (13), and recently, the cloning of B. pseudomallei class A and D β-lactamases has been reported (4, 14).
Godfrey et al. described three different phenotypes of clinical isolates from three patients which had undergone antibiotic treatment, and demonstrated that the resistance was due to derepressed β-lactamase production and structural mutations in the enzyme (10). Here, we examine the B. pseudomallei penA gene encoding a class A β-lactamase in the clinical isolates of B. pseudomallei described by Godfrey et al. and from B. mallei ATCC 23344. We have identified point mutations in two of the isolates which likely account for their altered phenotypes. Finally, the enzyme kinetics of these mutants were compared to the wild type enzyme.
MATERIALS AND METHODS
Bacterial strains and plasmids.
The bacterial strains and plasmid used in this study are shown in Table 1. B. pseudomallei strains used in this study were collected from blood and urine samples from melioidosis patients both before and during antibiotic treatment at Sappasitprasong Hospital, Ubon Ratchatani, Thailand, between 1986 and 1989 and have been described previously (7, 10). All bacterial strains were grown at 37°C on Luria-Bertani (LB) agar or in LB broth. Media used for growing B. mallei were supplemented with 4% glycerol. When used, antibiotics were added at the indicated concentrations.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Description | Reference or source |
|---|---|---|
| Strains | ||
| E. coli TOP10 | F−mcrA Δ(mrr-hsdRMS-mcrBC) φ80lacZΔM15 ΔlacX74 deoR recA1 araD139 Δ(ara-leu)7697 galU galK rpsL (Strr) endA1 nupG | Invitrogen |
| E. coli BL21 (DE3) | F−ompT hsdSB (rB−mB−) gal dcm (DE3) pLysS (Camr) | Invitrogen |
| E. coli BL21 (DE3)pLysS | BL21(DE3)pLysS: F−ompT hsdSB (rB−mB−) gal dcm (DE3) pLysS (Camr) | Invitrogen |
| B. cepacia K56-2 | CF isolate, Toronto, Canada | 8 |
| B. mallet ATCC 23344 | Type strain (human isolate) | USAMRIIDa |
| B. pseudomallei 316a | Clinical isolate, wild-type phenotype | 8 |
| B. pseudomallei 316c | Clinical isolate, selectively resistant to ceftazidime | 8 |
| B. pseudomallei 365c | Clinical isolate, wild-type phenotype | 8 |
| B. pseudomallei 365a | Clinical isolate, derepressed phenotype | 8 |
| B. pseudomallei 392a | Clinical isolate, wild-type phenotype | 8 |
| B. pseudomallei 392f | Clinical isolate, decreased susceptibility to clavulanic acid inhibition | 8 |
| B. thailandensis ATCC 700388 | Type strain (soil isolate) | 16 |
| Plasmids | ||
| pCR2.1-TOPO | Topoisomerase-mediated cloning vector: Apr Kmr | Invitrogen |
| pEM7/Zeo | Expression vector, Zeor | Invitrogen |
| pUCP31T | Broad-host-range vector. OriT pRO1600 ori; Gmr | 16 |
| p316a31T | pUCP31T containing cloned penA from 316a | This study |
| p316c31T | pUCP31T containing cloned penA from 316c | This study |
| p365a31T | pUCP31T containing cloned penA from 365a | This study |
| p365c31T | pUCP31T containing cloned penA from 365c | This study |
| p392a31T | pUCP31T containing cloned penA from 392a | This study |
| p392f31T | pUCP31T containing cloned penA from 392f | This study |
| pJES307 | pT7-7 derivative, expression vector with T7 promoter | 15 |
| pT7Zeo | pJES307 derivative with disrupted blaTEM-1, Zeor | This study |
| p316aT7Z | pT7Zeo containing cloned penA from 316a | This study |
| p316cT7Z | pT7Zeo containing cloned penA from 316c | This study |
| p392fT7Z | pT7Zeo containing cloned penA from 392f | This study |
U.S. Army Medical Research Institute of Infectious Diseases
PCR amplification and cloning of PCR products.
PCR products were generated in a 100-μl reaction mixture using the following cycling program: 95°C, 5 min; 95°C 1 min, 55°C 1 min, and 72°C 1 min for 30 cycles; and 72°C 10 min. Mixtures were then held at 4°C. Primers used in the amplification of the 580-bp penA from B. pseudomallei 1026b were (i) 5′-GCAGCACATCCAAGATGATG C-3′ and (ii) 5′-GCCGATCGTGTTCATCGTCTA-3′. The primers used in reverse PCR to amplify flanking regions of penA using XhoI-digested and ligated chromosomal DNA of 1026b were (i) 5′out (5′-GCATCATCTTGGATGTGCTGC-3′) and (ii) 3′out (5′-GCCGATCGTGTTCATCGTCTA-3′). The primers used to amplify the entire penA gene were (i) 5′penA (5′-GAGAGCTGATACGCTAGCGAG-3′) and (ii) 3′penA (5′-GCGGCTTCCGGAAGGTTCA-3′). The zeocin resistance gene was amplified with (i) Zeo1 (5′-TGGCCTTTTGCTCACATGTGT-3′) and (ii) Zeo2 (5′-TCTAGAGTCGACCTGCAGGCA-3′).
Cloning of β-lactamase genes from B. pseudomallei and B. mallei.
The penA gene was amplified from various B. pseudomallei mutants and from B. mallei using the 5′ penA and the 3′ penA primers. The PCR products were subsequently cloned into pCR2.1-TOPO (Invitrogen) as per the manufacturer's instructions. The cloned penA genes were transferred from the pCR2.1-TOPO cloning vector to pUCP31T (17) for MIC testing and to pT7Zeo (Invitrogen) for β-lactamase expression. Restriction enzymes and T4 ligase were purchased from BRL/Invitrogen. Plasmids were purified using a QIAprep Spin Miniprep Kit (Qiagen), and chromosomal DNA was prepared using a Wizard DNA purification kit (Promega). When required, PCR products were purified using GenElute PCR DNA purification kit (Sigma).
MIC determination.
MICs were determined using agar dilution or E-test strips (AB Biodisk, Solna, Sweden). For agar dilution, Mueller-Hinton agar plates were prepared containing twofold dilutions of antibiotic ranging from 1 to 256 μg/ml for ampicillin, amoxicillin, and cefazolin; from 0.25 to 128 μg/ml for amoxicillin plus clavulanic acid (8:1 ratio), cefoxitin, ceftriaxone, and aztreonam; and from 0.25 to 128 μg/ml for ceftazidime and imipenem. Plates were spotted with approximately 104 organisms diluted from overnight liquid cultures and examined after overnight incubation. E-test strips were used as per the manufacturer's instruction.
DNA sequencing and sequence analysis.
DNA sequencing was performed by University Core DNA Services (University of Calgary). The CLUSTAL W program (20) was used to align penA genes and their translated protein sequences.
Purification of β-lactamase and analysis of enzyme kinetics.
The β-lactamase enzyme from B. pseudomallei 316a, 316c, and 392f was purified in the following manner. Escherichia coli BL21(DE3) (Invitrogen) cells were transformed with p316aT7Z or p392fT7Z, and from the transformants periplasmic proteins were obtained using an osmotic shock procedure.
For B. pseudomallei 316c β-lactamase purification, E. coli BL21(DE3)LysS (Invitrogen) was used in an effort to obtain higher β-lactamase expression. For osmotic shock, four liters of each E. coli transformant was grown overnight, and cells were harvested by centrifugation and resuspended in 30 to 50 ml of 0.5 M sucrose for approximately 15 min. Periplasmic proteins were released by gently resuspending centrifuged cells in 20 ml of sterile distilled water. The periplasmic protein extracts were filter-sterilized and adjusted to 40 mM Tris-HCl, pH 8.5, to a final volume of 10 ml. The adjusted extracts were loaded into a Q-Sepharose fast flow 16/20 chromatography column. The B. pseudomallei β-lactamase enzyme was collected in the pass-through fraction. The pass through fraction was then concentrated to 2 ml with a Centriprep Centricon-10 and loaded into a MonoS HR 5/5 fast-performance liquid chromatography column (Amersham Pharmacia). The β-lactamase fraction was then eluted with a 0 to 2 M NaCl gradient to obtain a pure fraction of the enzyme. The pH of the enzyme extract was adjusted to 7.0, and this material was used for kinetic studies.
Enzyme purity was assessed by SDS-14% PAGE (data not shown). The kinetic analysis of β-lactam hydrolysis was performed with a Beckman DU640 spectrophotometer using 0.1 M phosphate buffer, pH 7.0.
Competition assays were performed in a total volume of 500 μl of buffer in 5- or 10-mm path length quartz cuvettes. Reporter (nitrocefin) was added to a final concentration of 100 μ M and inhibitor to a concentration of 50 or 100 μM. The extinction coefficients (Δɛ) and UV absorption wavelength of each antibiotic used in this study were as follows: nitrocefin, +15,000 M−1 cm−1 and 482 nm; ampicillin −1,100 M−1 cm−1 and 232 nm; amoxicillin, −1,100 M−1 cm−1 and 232 nm; cefazolin, −7,900 M−1 cm−1 and 260 nm; cefoxitin, −7,700 M−1 cm−1 and 260 nm; ceftriaxone, −9,400 M−1 cm−1 and 260 nm; ceftazidime, −8,660 M−1 cm−1 and 260 nm; aztreonam, −640 M−1 cm−1 and 318 nm; and imipenem, −9000 M−1 cm−1 and 300 nm.
Km and Vmax were calculated using nonlinear regression analysis by Prism software. The kcat was obtained using the known amount of enzyme measured by bicinchoninic acid protein assay (Pierce, Rockford, Ill.). Ki was obtained using the method described by Galleni et al. (9) and was used as Km when the hydrolysis rate could not be measured.
Nucleotide sequence accession numbers.
The penA sequences were submitted to GenBank under accession numbers AY032868, AY032869, AY032870, AY032871, AY032872, AY032873, and AY032874.
RESULTS
Reverse PCR and flanking region of the penA gene.
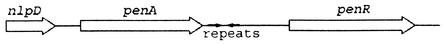
Reverse PCR was performed in order to obtain the sequence of flanking regions of the penA gene. The orientation of penA and flanking genes are shown in Fig. 1. The penA gene is downstream of the nlpD gene which is presumably involved in lipoprotein synthesis and is upstream of a putative regulator gene, penR. The nlpD, penA, and penR genes have the same orientation. The intergenic region between nlpD and penA and that between penA and penR are approximately 150 and about 700 bp, respectively.
FIG. 1.
Orientation of penA and penR in B. pseudomallei and B. mallei. nlpD, putative enzyme involved in lipoprotein synthesis; penA, class A β-lactamase gene; repeats, inverted repeats (not to scale); penR, putative regulator gene.
DNA sequence analysis.
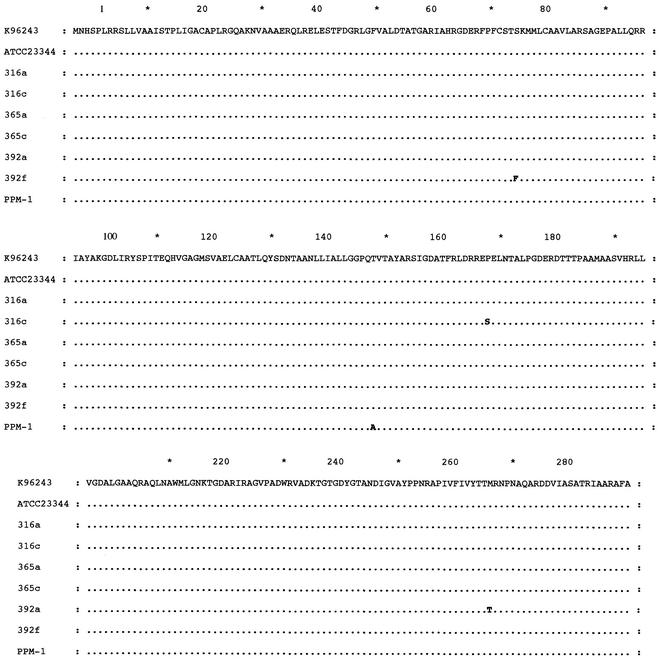
The PCR amplified penA gene from six different isolates of B. pseudomallei and B. mallei ATCC 23344 was sequenced and compared using the CLUSTAL W program (Fig. 2). The DNA sequences of these seven strains were almost identical in that only a few single base changes were identified. The presumptive translated protein sequences were identical between B. mallei and B. pseudomallei strains 316a (wild-type phenotype), 365a (derepressed), and 365c (wild-type phenotype). When strain 316c (ceftazidine resistant) was compared to strain 316a (wild-type phenotype), a single nucleotide change (C to T) was found resulting in a change of proline to serine at position 167 (P167S, ABL numbering scheme [R. P. Ambler, A. F. Coulson, J. M. Frere, J. M. Ghuysen, B. Joris, M. Forsman, R. C. Levesque, G. Tiraby, and S. G. Waley, Letter, Biochem. J. 276:269-270, 1991]). The clavulanic acid resistant strain 392f had a single nucleotide change (C to T) at S72F. Nucleotide changes in both 316c and 392f resulted in amino acid changes within conserved regions of class A β-lactamases. A single base change (T to C) in strain 392a (wild-type phenotype) resulted in a substitution of methionine with threonine (M266T) and was outside of the conserved regions of class A β-lactamases. Sequence comparison of the putative regulator region in all of the strains examined did not reveal any differences at the amino acid level (data not shown).
FIG. 2.
CLUSTAL W alignment of nine β-lactamases from B. pseudomallei and B. mallei. K96243, B. pseudomallei K96243; ATCC 23344, B. mallei ATCC 23344; PPM-1, B. pseudomallei Hong Kong strain (4). Dots indicate amino acids identical to those in the sequence for strain K96243. Letters indicate changed amino acids. Amino acids are numbered in accordance with the Ambler (ABL) numbering scheme (Ambler et al., letter).
MIC determination in parental strains and their corresponding clones.
The MICs of ten different β-lactam antibiotics were determined and compared in pairs of B. pseudomallei and E. coli TOP10 containing the corresponding penA clone. The results are shown in Table 2. The MICs of ceftazidime for both 316c and TOP10(p316c31T) were relatively high, although that for TOP10(p316c31T) was not significantly higher than many of the other E. coli Top10 penA clones. Also, both 392f and TOP10(p392f31T) showed a small but consistent decrease in susceptibility to clavulanic acid inhibition compared with 392a or TOP10(p392a31T).
TABLE 2.
MICs (μg/ml) of different β-lactams for E. coli, B. pseudomallei, and B. mallei
| Strain | MICa (μg/ml)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| AMP | AMX | AMC | CFZ | CRO | FOX | CAZ | ATM | IPM | |
| TOP10 | 4 | 4 | 4 | 2 | <1 | 4 | 0.25 | <1 | 0.25 |
| TOP10(p316a31T) | >256 | >256 | 128 | 256 | 4 | 4 | 2 | 8 | 0.25 |
| TOP10(p316c31T) | 256 | >256 | >128 | >256 | 4 | >128 | 4 | 2 | 1 |
| TOP10(p365a31T) | >256 | >256 | 32 | 256 | 16 | 8 | 4 | 8 | 0.25 |
| TOP10(p365c31T) | 256 | >256 | 32 | 128 | 16 | 8 | 4 | 8 | 0.25 |
| TOP10(p392a31T) | 128 | >256 | 8 | 128 | 4 | 8 | 2 | 8 | 0.25 |
| TOP10(p392f31T) | 128 | >256 | 16 | 64 | 4 | 8 | 1 | 8 | 0.25 |
| ATCC 23344 | 64 | 128 | 8 | >256 | 8 | >128 | 1 | 32 | 0.25 |
| 316a | 64 | 128 | 8 | >256 | 8 | >128 | 4 | 32 | 0.5 |
| 316c | 64 | 128 | 8 | >256 | 8 | >128 | 64 | 32 | 0.5 |
| 365a | >256 | >256 | 128 | >256 | 128 | >128 | 16 | >256 | 2 |
| 365c | 64 | 128 | 128 | >256 | 128 | >128 | 16 | >256 | 0.5 |
| 392a | 64 | 128 | 16 | >256 | 4 | >128 | 2 | 32 | 0.5 |
| 392f | 64 | 128 | 32 | >256 | 8 | >128 | 4 | 64 | 0.5 |
Abbreviations for antibiotics: AMP, ampicillin; AMX, amoxicillin; AMC, amoxicillin-clavulanic acid; CFZ, cefazolin; CRO, ceftriaxone; FOX, cefoxitin; CAZ, ceftazidime; ATM, aztreonam; IPM, imipenem.
β-Lactamase purification and kinetic parameters.
Enzyme obtained from periplasmic extracts and subjected to ion exchange column purification yielded β-lactamase with greater than 90% purity. The enzyme preparations were used to examine the kinetics of β-lactam hydrolysis in 3 of the B. pseudomallei strains. In general, the β-lactams used in this study could be divided into five groups. The first group consisted of “good” substrates, such as nitrocefin, cefazolin and ceftriaxone, which exhibited high kcat/Km. The second group represented poor substrates, such as ampicillin and aztreonam. The third group were very poor substrates, such as amoxicillin, in that the hydrolysis rate could not be measured but could be derived by using the competitive hydrolysis method. The fourth group consisted of nonsubstrates as the enzyme could not recognize those β-lactams either as substrates or inhibitors. The last group was the inhibitor group and consisted of a single substrate, clavulanic acid. The hydrolysis rates of nine different β-lactams, representing the five groups described above, were examined using the “good” substrate nitrocefin as a reporter and the Ki obtained from these competitive analysis experiments was used as a Km for comparison. The kinetic parameters obtained from β-lactamases from three of the B. pseudomallei strains are shown in Table 3. Ceftazidime was not recognizable by 316a and 392f enzymes; however, it was a substrate for the 316c enzyme, in that it was recognizable via competitive hydrolysis, albeit very poorly. Ampicillin and aztreonam were very poor substrates for the 316c enzyme yet good substrates for 316a and 392f. The Km (Ki) of 392f for clavulanic acid was about fivefold higher than that of 316a indicating lower affinity of the 392f enzyme for clavulanic acid; however, the 316c enzyme had the highest Km for clavulanic acid among the three strains.
TABLE 3.
Kinetic parameters of B. pseudomallei β-lactamasesa
| Substrate | PenA | Vmax | Km | kcat | kcat/Km |
|---|---|---|---|---|---|
| Nitrocefin | 316a | 159 ± 7.4 | 10.9 ± 2.1 | 4.91 | 446 |
| 316c | 67.6 ± 4.2 | 3.34 ± 0.7 | 1.01 | 303 | |
| 392f | 351 ± 7.2 | 38 ± 2.1 | 46.2 | 1,214 | |
| AMP | 316a | 1,316 ± 114 | 126 ± 29.5 | 0.18 | 1.45 |
| 316c | NM | 13.8 | 0.04 | 2.74* | |
| 392f | 4,087 ± 601 | 1,051 ± 237 | 37.2 | 35.4 | |
| AMX | 316a | NM | 2.22* | NM | NM |
| 316c | NM | 0.88* | 0.09 | 96.9* | |
| 392f | NM | 74.6* | NM | NM | |
| CFZ | 316a | 1,024 ± 106 | 59.5 ± 17.8 | 21.35 | 359 |
| 316c | 168 ± 5.9 | 12.6 ± 1.8 | 0.63 | 50 | |
| 392f | 2,390 ± 383 | 255 ± 52.8 | 78.6 | 307 | |
| FOX | 316a | NH | NR | NH | NH |
| 316c | NM | 15.4* | 0.02 | 1.02* | |
| 392f | NH | NR | NH | NH | |
| CRO | 316a | 1,514 ± 389 | 287 ± 117 | 63.1 | 219 |
| 316c | 253 ± 29.4 | 29.4 ± 8.5 | 0.95 | 32.4 | |
| 392f | 802 ± 128 | 138 ± 34.4 | 26.3 | 191 | |
| CAZ | 316a | NM | NR | NM | NM |
| 316c | NM | 10.3* | 0.02* | 2.33* | |
| 392f | NM | NR | NM | NM | |
| ATM | 316a | 1,645 ± 211 | 179 ± 61.4 | 3.2 | 17.9 |
| 316c | NM | 48.1* | 0.15* | 3.2* | |
| 392f | 1,939 ± 144 | 336 ± 51.9 | 17.6 | 52.5 | |
| IPM | 316a | NH | NR | NH | NH |
| 316c | NH | NM** | NH | NM** | |
| 392f | NH | NR | NH | NH | |
| CLA | 316a | ND | 0.61* | ND | ND |
| 316c | ND | 17.7* | ND | ND | |
| 392f | ND | 3.18* | ND | ND |
Units are μMs−1 for Vmax, μM for Km, s−1 for kcat, and mM−1s−1 for kcat/Km. CLA; clavulanic acid. Other antibiotic abbreviations are as listed in Table 1. NR, antibiotic was not recognized by that particular enzyme; NM, the rate of hydrolysis is too slow to be measured accurately; ND, not determined; NH, hydrolysis was not detected after 30 minutes. ∗, Ki was used as Km ; ∗∗, the enzyme was completely inactivated by imipenem and no nitrocefin hydrolysis was detected.
DISCUSSION
This study examines the penA gene and the class A β-lactamase enzyme which it encodes from several B. pseudomallei clinical isolates. In addition, we have sequenced the penA gene from B. mallei and have found it to be identical to that found in B. pseudomallei. We have shown that the β-lactamase resistant phenotype in B. pseudomallei can be attributed to amino acid changes in conserved regions of the β-lactamase enzyme.
Although the sequence of B. pseudomallei penA has recently been reported (4), reverse PCR experiments revealed a unique arrangement of the penA structural gene with a putative regulator downstream and in the same orientation. Sequence analysis of the putative regulator region did not reveal any differences between all B. pseudomallei strains examined at the amino acid level suggesting that the observed derepressed phenotypes are not a result of mutations within this region and that other factors contribute to the elevated enzyme levels in these strains.
The approximately 700-bp region which separates the penA gene and the putative regulator contains repeats and inverted repeats and may possibly contain unknown regulatory features. This region remains a target for further studies aimed at understanding the regulation of the β-lactamase enzyme.
The penA gene in Burkholderia spp. encodes a class A β-lactamase which is susceptible to clavulanic acid inhibition. The predicted protein sequence contains all four conserved motifs found in other class A enzymes—namely, SXXK, SDN, omega loop (EXXLN), and KTG motifs (11)—and according to its activity, penA would be classified in the Bush group 2e (2, 4). The enzymes from two strains, 316c and 392f, had mutations that resulted in amino acid changes within the conserved motifs of the catalytic site. The mutation of 316c at the omega loop (P167S) may explain the observed ceftazidime resistance as this mutation has been shown to be associated with ceftazidine resistance in K. pneumoniae (15). Although the rates of ceftazidime hydrolysis by β-lactamase from 316c and 316a were not directly measurable, the 316c enzyme could recognize ceftazidime as competitive substrate and thereby allowed calculation of Ki, kcat, and kcat/Km ratio values. It is likely that the increased affinity for ceftazidime of the 316c enzyme may account for the increased resistance of this strain to this antibiotic.
The 392f enzyme also contained a point mutation in a conserved motif resulting in a S72F mutation. Although the phenylalanine at this position can be found in many β-lactamases, it is convincing that in this case, the change resulted in a decreased susceptibility to clavulanic acid inhibition in both B. pseudomallei strain 392f and in E. coli TOP10(p392f31T) as the Ki for clavulanic acid was higher for the 392f enzyme than the wild type, 316a enzyme. The higher Ki would indicate decreased affinity of clavulanic acid, resulting in a higher MIC for amoxicillin plus clavulanic acid for strain 392f and E. coli TOP10(p392f31T) compared to strain 392a and TOP10 (p392a31T).
The Ki obtained for clavulanic acid and strain 316c was higher than for strains 392f and 316a, which may explain decreased susceptibility to clavulanic acid inhibition. However, the MIC of amoxicillin/clavulanic acid in 316c was not higher than 392f. This may be explained by the fact that 316c enzyme hydrolyzed amoxicillin more poorly than the wild type enzyme, so the decreased susceptibility to clavulanic acid inhibition could not raise the MIC of amoxicillin/clavulanic acid.
The MICs for B. pseudomallei penA genes cloned into E. coli TOP10 may not accurately reflect actual enzyme activity in B. pseudomallei. Efflux mechanisms and/or differences in outer membrane permeability may alter periplasmic β-lactam concentrations and thus may affect apparent enzyme activity.
While this work was being reviewed the cloning of a class D β-lactamase from B. pseudomallei was reported (14). The authors reported increased transcription of the class D β-lactamase gene in laboratory generated ceftazidime resistant mutants. However, extracts of E. coli carrying the cloned gene from parent and mutant showed no detectable ceftazidime or imipenem hydrolyzing activity. Thus, the role of the B. pseudomallei class D β-lactamase in β-lactam resistance remains unclear.
Other factors outside the coding region of the penA gene may also contribute to highly resistant phenotypes as seen in 365a and 365c. Currently, we are studying the function of penR, the putative regulator and the intergenic 700bp region on the expression of β-lactamase in B. pseudomallei.
Acknowledgments
This work was funded by the Department of Defense (contract DAMD 17-98-C-8003) and the Canadian Bacterial Diseases Network of Centres of Excellence Program.
REFERENCES
- 1.Brett, P. J., D. DeShazer, and D. E. Woods. 1998. Burkholderia thailandensis sp. nov., description of a Burkholderia pseudomallei-like species. Int. J. Syst. Bacteriol. 48:317-320. [DOI] [PubMed] [Google Scholar]
- 2.Bush, K., G. A. Jacoby, and A. A. Medeiros. 1995. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 39:1211-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaowagul, W., A. J. Simpson, Y. Suputtamongkol, M. D. Smith, B. J. Angus, and N. J. White. 1999. A comparison of chloramphenicol, trimethoprim-sulfamethoxazole, and doxycycline with doxycycline alone as maintenance therapy for melioidosis. Clin. Infect. Dis. 29:375-380. [DOI] [PubMed] [Google Scholar]
- 4.Cheung, T. K., P. L. Ho, P. C. Woo, K. Y. Yuen, and P. Y. Chau. 2002. Cloning and expression of class A β-lactamase gene blaA (BPS) in Burkholderia pseudomallei. Antimicrob. Agents Chemother. 46:1132-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Currie, B. J., D. A. Fisher, N. M. Anstey, and S. P. Jacups. 2000. Melioidosis: acute and chronic disease, relapse and re-activation. Trans. R. Soc. Trop. Med. Hyg. 94:301-304. [DOI] [PubMed] [Google Scholar]
- 6.Dance, D. A. 1991. Melioidosis: the tip of the iceberg? Clin. Microbiol. Rev. 4:52-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dance, D. A., V. Wuthiekanun, W. Chaowagul, Y. Suputtamongkol, and N. J. White. 1991. Development of resistance to ceftazidime and co-amoxiclav in Pseudomonas pseudomallei. J. Antimicrob. Chemother. 28:321-324. [DOI] [PubMed] [Google Scholar]
- 8.Darling, P., M. Chan, A. D. Cox, and P. A. Sokol. 1998. Siderophore production by cystic fibrosis isolates of Burkholderia cepacia. Infect. Immun. 66:874-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galleni, M., N. Franceschini, B. Quinting, L. Fattorini, G. Orefici, A. Oratore, J. M. Frere, and G. Amicosante. 1994. Use of the chromosomal class A β-lactamase of Mycobacterium fortuitum D316 to study potentially poor substrates and inhibitory β-lactam compounds. Antimicrob. Agents Chemother. 38:1608-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godfrey, A. J., S. Wong, D. A. Dance, W. Chaowagul, and L. E. Bryan. 1991. Pseudomonas pseudomallei resistance to β-lactam antibiotics due to alterations in the chromosomally encoded β-lactamase. Antimicrob. Agents Chemother. 35:1635-1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joris, B., P. Ledent, O. Dideberg, E. Fonze, J. Lamotte-Brasseur, J. A. Kelly, J. M. Ghuysen, and J. M. Frere. 1991. Comparison of the sequences of class A β-lactamases and of the secondary structure elements of penicillin-recognizing proteins. Antimicrob. Agents Chemother. 35:2294-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leelarasamee, A. 1998. Burkholderia pseudomallei: the unbeatable foe? Southeast Asian J. Trop. Med. Public Health 29:410-415. [PubMed] [Google Scholar]
- 13.Livermore, D. M., P. Y. Chau, A. I. Wong, and Y. K. Leung. 1987. β-lactamase of Pseudomonas pseudomallei and its contribution to antibiotic resistance. J. Antimicrob. Chemother. 20:313-321. [DOI] [PubMed] [Google Scholar]
- 14.Niumsup, P., V. Wuthiekanun. 2002. Cloning of the class D-β-lactamase gene from Burkholderia pseudomallei and studies in its expression in ceftazidime-susceptible and -resistant strains. J. Antimicrob. Chemother. 50:445-455. [DOI] [PubMed] [Google Scholar]
- 15.Poirel, L., T. Naas, I. Le Thomas, A. Karim, E. Bingen, and P. Nordmann. 2001. CTX-M-type extended-spectrum β-lactamase that hydrolyzes ceftazidime through a single amino acid substitution in the omega loop. Antimicrob. Agents Chemother. 45:3355-3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reckseidler, S. L., D. DeShazer, P. A. Sokol, and D. E. Woods. 2001. Detection of bacterial virulence genes by subtractive hybridization: identification of capsular polysaccharide of Burkholderia pseudomallei as a major virulence determinant. Infect. Immun. 69:34-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tabor, S., and C. C. Richardson. 1985. A bacteriophage T7 RNA polymerase/promoter system for controlling exclusive expression of specified genes. Proc. Natl. Acad. Sci. USA 82:1074-1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schweitzer, H. P., T. Klassen, and T. Hoang. 1996. Improved methods for gene analysis and expression ion pseudomonas spp., p. 229-237. In T. Nakazawa, K. Furukawa, D. Haas, and S. Silver (ed.), Molecular biology of pseudomonads. American Society for Microbiology, Washington, D.C.
- 19.Suputtamongkol, Y., A. Rajchanuwong, W. Chaowagul, D. A. Dance, M. D. Smith, V. Wuthiekanun, A. L. Walsh, S. Pukrittayakamee, and N. J. White. 1994. Ceftazidime vs. amoxicillin/clavulanate in the treatment of severe melioidosis. Clin. Infect. Dis. 19:846-853. [DOI] [PubMed] [Google Scholar]
- 20.Thompson, J. D., D. G. Higgins, and T. J. Gibson. 1994. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 22:4673-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]