Abstract
Keratinocyte growth factor (KGF), a member of the fibroblast growth factor (FGF) family, is a specific mitogen for different types of epithelial cells and a potent survival factor for these cells under stress conditions. KGF expression increases strongly after injury to various tissues, including the skin and the intestine, and signaling via the KGF receptor was shown to be crucial for repair of skin wounds and for liver regeneration. Here we demonstrate an increased expression of KGF in chronic liver disease associated with fibrosis. The extent of KGF overexpression correlated strongly with the stage of fibrosis. As the cellular source of KGF we identified activated hepatic stellate cells (HSCs)/myofibroblasts. In contrast to the ligand, the KGF receptor, FGFR2-IIIb, was exclusively expressed by hepatocytes, but not by activated HSCs or other parenchymal or nonparenchymal liver cells. Based on the known effects of KGF on hepatocytes in vitro, our findings suggest that HSC/myofibroblast-derived KGF may enhance liver regeneration and/or hepatocyte survival in patients with chronic liver disease.
Keratinocyte growth factor [KGF = fibroblast growth factor 7 (FGF-7)] is a potent mitogen for different types of epithelial cells.1 In addition, it regulates migration and differentiation of these cells and protects them from various insults under stress conditions.2 KGF is produced by mesenchymal cells, including fibroblasts and vascular smooth muscle cells, as well as by γδT cells in wounded skin and in the inflamed gut.1,3–5 It exerts its biological effects via binding to its high-affinity receptor, a splice variant of FGF receptor 2 (FGFR2-IIIb).6 This transmembrane tyrosine kinase receptor is expressed by various types of epithelial cells, including epidermal keratinocytes, intestinal epithelial cells, and hepatocytes.2 This expression pattern of KGF and its receptor suggests that KGF acts predominantly in a paracrine manner.
Most interestingly, KGF expression is strongly up-regulated after acute injury to various tissues, including the skin,7 the bladder,8 and the kidney9 as well as in chronically injured tissue as seen, for example, in patients with inflammatory bowel disease.10–12 This up-regulation is likely to be important for the healing of injured epithelia, because signaling via the KGF receptor was shown to be crucial for re-epithelialization of skin wounds.13 Furthermore, KGF-deficient mice showed impaired regeneration of the intestinal epithelium in a dextran sulfate sodium induced mouse model of colitis.14 The latter finding suggested that the elevated expression of KGF seen in the gut of patients with inflammatory bowel disease is important for the repair of the injured gut epithelium during the remission phase of the disease. In addition, KGF could also exert a protective effect on these cells. Thus it has been shown that exogenous KGF can reduce the development of oral mucositis and intestinal injury in rodents and also in patients on treatment with chemotherapy or radiotherapy.15,16 Therefore, KGF is currently used in clinical trials for the treatment of mucositis in cancer patients (Amgen: AMGEN Announces Positive Results of Phase 3 Study rHu-KGF. January 23, 2003. http://www.amgen.com/news/news03/pressRelease030123.pdf).16
Based on these properties of KGF, we speculated about a role of KGF in human liver disease. In previous studies, hepatocytes were shown to express the KGF receptor, in particular after liver injury.17,18 The importance of this hepatic FGFR2-IIIb expression was demonstrated in a recent study, in which expression of a dominant-negative FGFR2-IIIb mutant in hepatocytes of transgenic mice strongly inhibited hepatocyte proliferation after partial hepatectomy.19 Surprisingly, however, expression of KGF has as yet not been found in the liver, not even after hepatectomy.18,19 This suggests that other FGFs bind to the KGF receptor in injured liver. In addition, it seems possible that expression of KGF occurs only under fibrotic conditions. To address this possibility, we analyzed the expression of KGF and its receptor in patients suffering from hepatic fibrosis and cirrhosis. These conditions develop as a consequence of chronic injury to the liver by a variety of insults, including viral infection, autoimmune disease, cholestasis, and chronic alcohol abuse. Hepatic fibrosis is viewed as a relatively uniform response to these different types of injury. It is characterized by an increased deposition of extracellular matrix proteins as a result of increased fibrogenesis and decreased fibrolysis.20,21 Activated hepatic stellate cells (HSCs) are the effector cells of hepatic fibrosis. After hepatic injury, HSCs undergo an activation process and transform to an activated, myofibroblast-like phenotype. They are responsible for the excessive hepatic matrix deposition and their activity is recognized as a central event in the development of hepatic fibrosis.22,23 In addition, recent studies indicate that hepatic myofibroblasts comprise not only HSCs but also cells of other (mainly portal) origin.24,25 Here we show that activated HSCs/myofibroblasts are an important source of KGF in patients with hepatic fibrosis, suggesting a novel role of KGF in the pathogenesis of fibrotic liver disease.
Materials and Methods
Human Liver Tissue
Cirrhotic human liver tissue samples were obtained from eight patients who underwent liver transplantation. The underlying liver disease was chronic hepatitis C infection (HCV) (n = 2), autoimmune hepatitis (n = 2), primary biliary cirrhosis (n = 1), chronic alcohol abuse (Alc) (n = 1), chronic hepatitis B infection in combination with hepatitis D infection (n = 1), or with chronic alcohol abuse (n = 1), respectively. Furthermore, liver biopsies were obtained from 30 patients with chronic hepatitis C infection (positive for HCV-RNA and HCV antibodies) before initiation of antiviral therapy (naive patients) by percutaneous Menghini needle biopsy. These patients were negative for hepatitis B surface antigen or antibodies to human immunodeficiency virus and none of them had evidence of other types of liver disease.
In addition, human liver tissue samples were obtained from patients undergoing partial hepatectomy for metastatic liver tumors of colorectal cancer. Surrounding nontumorous liver tissue (judged as noncancerous by local pathologists) served as control if there was no histological evidence for liver fibrosis or inflammation, and if known liver diseases were excluded. Liver tissue samples were immediately frozen in liquid nitrogen and stored at −80°C for RNA isolation or formalin-fixed for immunohistochemistry. Histologically detectable fibrosis and inflammation were graded and staged numerically by a single pathologist according to a score proposed by Desmet and colleagues.26 Informed consent was obtained from all patients, and the study was approved by the local ethics committee, Regensburg.
Cell Isolation and Cell Culture
Human Liver Cells
Tissue samples from human liver resections obtained from patients undergoing partial hepatectomy for metastatic liver tumors of colorectal cancer (see above) were used for the preparation of human liver cells. Cells were isolated using a modified two-step EGTA/collagenase perfusion procedure and one part of the cell suspension was used for isolation of hepatocytes as described previously.27 RNA was isolated directly from the freshly isolated cells.
Isolation and Culture of HSCs
Another part of the cell suspension was sequentially incubated with pronase and HSCs were separated from other nonparenchymal liver cells by arabinogalactan gradient ultracentrifugation, as previously described.28 This procedure yielded HSCs that were more than 85% pure and 90% viable, as determined by phase contrast and UV-excited fluorescence microscopy, and trypan blue exclusion, respectively. HSCs were cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% heat-inactivated fetal calf serum, 100 IU/ml penicillin, and 100 μg/ml streptomycin in a 95% air and 5% CO2-humidified atmosphere. Growth medium was changed daily during the first 4 days in culture and every second day thereafter. For activation, HSCs were cultured on uncoated tissue culture dishes for 20 days and then plated in six-well plates for subsequent analysis.
Isolation of Kupffer Cells (KCs) and Liver Endothelial Cells (ECs)
For isolation of KCs and ECs another part of the liver cell suspension was used. Cells were purified by immunomagnetic purification using CD68 MicroBeads (Miltenyi Biotech, Bergisch Gladbach, Germany) for KCs and CD105 MicroBeads (Miltenyi Biotech) for ECs as previously described.29 It was previously shown by Theuerkauf and colleagues30 that CD105-positive ECs were predominantly found at the end of the sinusoidal blood stream.
Because the expression of CD105 is dependent on the location of the ECs along the sinusoid, we also purified ECs by immunomagnetic purification using CD68 MicroBeads (Miltenyi Biotech) as previously described.29 Here, ECs were isolated by magnetic cell sorting with indirect MicroBeads (Miltenyi Biotech) according to the manufacturer’s instructions. Briefly, the cell suspension was washed and subsequently resuspended in minimal essential medium and incubated with anti-CD146 antibody (Biocytex, Marseille, France) (1:10 dilution) for 45 minutes at 4°C. After two washing steps cells were resuspended in minimal essential medium, incubated with anti-mouse IgG MicroBeads (Miltenyi Biotech), and subsequently purified on a positive selection column by magnetic separation. RNA was isolated directly from the freshly sorted KCs and ECs.
Dermal Fibroblasts and Keratinocytes
Primary human fibroblasts were isolated and cultured as described previously.31 Human keratinocytes were obtained from CellSystems (St. Katharinen, Germany). Fibroblasts and keratinocytes were cultured on uncoated tissue culture flasks in Dulbecco’s modified Eagle’s medium supplemented with 10% heat-inactivated fetal calf serum, 100 IU/ml penicillin, and 100 μg/ml streptomycin in a humidified atmosphere of 5% CO2 in air.
Carbon Tetrachloride (CCl4) Model of Liver Fibrosis
Male C57BL6 mice were injected intraperitoneally with CCl4 (1 μl/g/body weight, diluted 1:20 in mineral oil) three times weekly, for 5 or 8 weeks (six animals per group). Animals were killed 24 hours after the last intraperitoneal injection. In addition, four mice were killed 3 days after a single injection of CCl4. The livers of the sacrificed animals were immediately frozen in liquid nitrogen and stored for RNA isolation. Three animals were injected intraperitoneally with mineral oil alone for 8 weeks. These control animals revealed no histological signs of fibrosis or increased collagen I mRNA expression compared to untreated mice.
KGF Secretion of HSCs
Freshly isolated HSCs were seeded in six-well plates. Medium was changed after 24 hours and every 48 hours thereafter, adding a defined volume (1.5 ml) per plate. After 48 hours of conditioning, the tissue culture media were collected, centrifuged to remove cellular debris, and then frozen and stored at −80°C. KGF concentrations in the supernatants (collected at days 1, 3, 5, 7, 9, 11, 13, and 15, respectively) were analyzed by a sandwich enzyme-linked immunosorbent assay following the instructor’s manual (R&D Systems, Wiesbaden-Nordenstadt, Germany). The KGF concentration in the supernatants was normalized to the concentration of total cellular protein determined by the Biuret method.
Isolation of RNA
Total RNA from liver or cultured cells was isolated using the RNeasy mini kit, including a RNase-free DNase treatment following the instructor’s manual (Qiagen, Hilden, Germany). For RNase protection assays, RNA isolation was performed according to Chomczynski and Sacchi.32 RNA concentrations were determined using a fluorescence microplate reader and following the instructor’s manual of the RiboGreen RNA quantitation reagent kit (MoBiTec, Göttingen, Germany).
Quantification of mRNA Expression by Real-Time Reverse Transcriptase (RT)-Polymerase Chain Reaction (PCR)
Integrity of the RNA was verified by agarose gel electrophoresis and by visualization of ribosomal RNAs by ethidium bromide staining. First strand cDNA was synthesized using 1 μg of total RNA and the AMV-reverse transcription reaction (Promega, Madison, WI). Transcript levels of human KGF, FGFR2-IIIb, α-smooth muscle actin (α-SMA), collagen α1(I) (Coll-I), and β-actin were quantified using the real-time RT-PCR technology (Lightcycler; Roche, Mannheim, Germany) with specific sets of primers based on published sequences: β-actin forward 5′-CTA CGT CGC CCT GGA CTT CGA GC-3′ and β-actin reverse 5′-GAT GGA GCC GCC GAT CCA CAC G-3′; KGF forward 5′-GGC AAT CAA AGG GGT GGA-3′ and KGF reverse 5′-CCT CCG TTG TGT GTC CAT TTA-3′; FGFR2-IIIb forward 5′-TGC TGG CTC TGT TCA ATG TG-3′ and FGFR2-IIIb reverse 5′-GGC GAT TAA GAA GAC CCC TA-3′, FGFR4 forward 5′-CGG CCT CTC CTA CCA GTC T-3′ and FGFR4 reverse 5′-TGC CGG AAG AGC CTG AC-3′; α-SMA forward 5′-CGT GGC TAT TCC TTC GTT AC and α-SMA reverse 5′-TGC CAG CAG ACT CCA TCC; Coll-I forward 5′-CGG CTC CTG CTC CTC TT-3′ and Coll-I reverse 5′-GGG GCA GTT CTT GGT CTC-3′.
Quantification of mRNA Expression by RNase Protection Assay
RNase protection assays were performed as described.33 Templates for human and murine KGF, FGFR2-IIIb, interleukin-1β, and GAPDH, have been described before.7,10,34,35
Immunohistochemistry
For immunohistochemistry, standard 5-μm sections of formalin-fixed and paraffin-embedded tissue blocks were used. Immunohistochemical staining was performed using an indirect immunoperoxidase protocol according to the Vectastain kit (Vector Laboratories, Burlingame, CA). Briefly, slides were deparaffinated by incubation in xylene, followed by a series of graded alcohols. Then, endogenous peroxidase was inhibited by incubation in 0.3% H2O2 and unspecific binding was blocked by incubating the sections in 20% horse serum/phosphate-buffered saline. Specimens were incubated with the following primary antibodies: goat anti-human KGF (1:75 dilution; R&D Systems, Wiesbaden, Germany), rabbit anti-human FGFR2 (1:200 dilution; Sigma, Deisenhofen, Germany), or mouse monoclonal anti-α-SMA (M0634, 1:50 dilution; DAKO, Glostrup, Denmark), respectively. Subsequently, after incubation with secondary anti-goat, anti-rabbit, or anti-mouse antibodies (Vector Laboratories), color was developed applying the Vectastain peroxidase detection kit and diaminobenzidine as a substrate. Counterstaining was performed with hematoxylin and eosin.
Statistical Analysis
Results are expressed as mean ± SD (range) or percent. Comparison between groups was made using the Student’s unpaired t-test. Welch’s correction was performed when required. A two-sided chi-square test was used for comparison of qualitative variables. Correlation between parameters was calculated with the Spearman test. A P value <0.05 was considered statistically significant. All calculations were performed using the SPSS-10 for Windows statistical computer package (SSPS, Inc., Chicago, IL).
Results
KGF and FGFR2-IIIb mRNA Expression in Healthy and Cirrhotic Human Livers
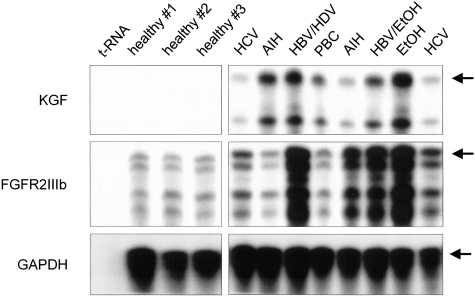
To gain insight into a possible role of KGF and its receptor in liver cirrhosis, we first analyzed the expression of these genes in surgical specimens from healthy (n = 3) and cirrhotic human livers (n = 8). The latter were obtained from patients suffering from different types of chronic liver disease, including hepatitis B, C, and/or D infection; autoimmune hepatitis; primary biliary cirrhosis; and cirrhosis caused by chronic alcohol abuse. KGF mRNA was not detectable by RNase protection assay in healthy human livers. However, all cirrhotic livers expressed KGF to a variable degree (Figure 1). In contrast to the ligand, FGFR2-IIIb mRNA was detectable in all healthy liver tissues. In most of the cirrhotic livers we found increased expression of this type of receptor compared to control tissue, but there was no obvious correlation between KGF and FGFR2-IIIb expression (Figure 1).
Figure 1-4237.
Enhanced expression of KGF in patients with liver cirrhosis. Samples of 20 μg of total cellular RNA of surgical specimens from healthy human liver of control patients and from affected areas of patients suffering from different types of liver disease were analyzed by RNase protection assay for the expression of KGF and FGFR2-IIIb. Hybridization of the same samples with a GAPDH riboprobe served as a loading control and 50 μg of tRNA as a negative control. The major protected fragments are indicated by arrows. Abbreviations stand for liver cirrhosis associated with the following diseases: HCV, hepatitis C virus infection; HBV/HDV, hepatitis B and hepatitis D virus infection; AIH, autoimmune hepatitis; PBC, primary biliary cirrhosis; EtOH, alcoholic liver disease.
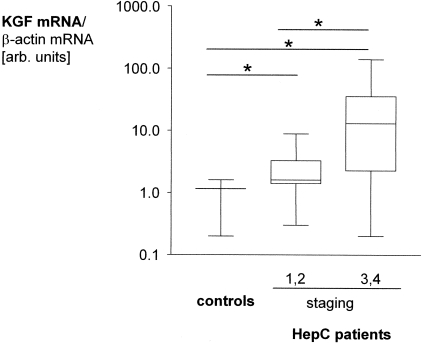
KGF mRNA Levels in Human Liver with Different Degrees of Fibrosis and Inflammation
To investigate if the extent of KGF expression correlates with the degree of liver damage, we analyzed KGF mRNA levels in liver tissue of patients chronically infected with the HCV, showing different histological stages of fibrosis (n = 30). Using real-time RT-PCR, hepatic KGF mRNA levels correlated significantly with the stage of fibrosis in hepatitis C patients (r = 0.53, P = 0.003). Patients with no or only mild periportal fibrosis (staging 1 or 2, n = 18) revealed significantly lower hepatic KGF transcript levels than patients with more advanced septal fibrosis or cirrhosis (staging 3 or 4, n = 12): 2.6 ± 0.5 versus 30.4 ± 12.5 (P = 0.010) (Figure 2). Compared to healthy livers (n = 4), KGF mRNA expression was significantly elevated in hepatitis C patients with staging 1 or 2: 1.0 ± 0.3 versus 2.6 ± 0.5 (P = 0.020). Staging of hepatic fibrosis and grading of hepatic inflammation correlate strongly in patients with chronic hepatitis C. Also in our study, staging and grading revealed high correlation (r = 0.84, P < 0.0001). Most importantly, grading also correlated significantly with hepatic KGF mRNA expression (r = 0.59, P = 0.004).
Figure 2-4237.
KGF mRNA levels correlate with the stage of fibrosis in human livers. KGF mRNA levels were measured by quantitative RT-PCR in specimens from healthy human liver of control patients (n = 4) and in liver biopsies taken from hepatitis C patients with no or only mild periportal fibrosis (staging 1 or 2, n = 18) or with more advanced septal fibrosis or cirrhosis (staging 3 or 4, n = 12), respectively. KGF mRNA levels were normalized to β-actin and are depicted as box blots. *, P < 0.05.
FGFR2-IIIb mRNA Levels in Human Liver with Different Degrees of Fibrosis and Inflammation
Next we analyzed the hepatic expression of the KGF receptor, FGFR2-IIIb, in the same samples from hepatitis C patients as used for the KGF mRNA analysis. In contrast to its ligand, FGFR2-IIIb mRNA levels correlated inversely with the stage of fibrosis in hepatitis C patients (r = −0.57, P = 0.005). Hepatitis C patients with no or only mild periportal fibrosis (staging 1 or 2) showed significantly higher hepatic FGFR2-IIIb mRNA expression than hepatitis C patients with more advanced septal fibrosis or cirrhosis (staging 3 or 4): 12.7 ± 2.6 versus 3.8 ± 1.8 (P = 0.013) (Figure 3).
Figure 3-4237.
FGFR2-IIIb mRNA levels are enhanced in the liver of patients with mild fibrosis. FGFR2-IIIb mRNA levels were measured by quantitative RT-PCR in specimens from healthy human liver of control patients (n = 4), and from hepatitis C patients with no or only mild periportal fibrosis (staging 1 or 2, n = 18) or with more advanced septal fibrosis or cirrhosis (staging 3 or 4, n = 12), respectively. KGF mRNA levels were normalized to β-actin and are depicted as box blots. *, P < 0.05.
Similar to the result observed for the ligand, hepatic FGFR2-IIIb mRNA levels were significantly higher in hepatitis C patients with staging 1 or 2 compared to nondiseased hepatic tissue: 12.7 ± 2.6 versus 0.6 ± 0.5 (P = 0.039). However, mean hepatic FGFR2-IIIb mRNA expression in hepatitis C patients with more advanced septal fibrosis or cirrhosis (staging 3 or 4) did not differ significantly from those of controls (3.8 ± 1.8 versus 0.6 ± 0.5, n.s.) because of the wide variation of FGFR2-IIIb expression found in livers with more advanced fibrosis or cirrhosis.
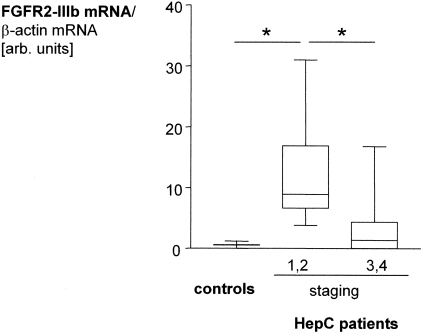
KGF and FGFR2-IIIb mRNA Expression in an Animal Model of Hepatic Fibrosis
Next we wanted to analyze KGF and FGFR2-IIIb mRNA expression during the course of liver injury. For this purpose we chose chronic toxic liver injury by CCl4 application to mice as an animal model of hepatic fibrosis. Hepatic KGF and FGFR2-IIIb mRNA levels were determined by RNase protection assays (Figure 4A). Analysis of the obtained bands by phosphoimaging revealed an increase in the number of KGF transcripts 5 weeks after chronic CCl4 intoxication, with a further increase at week 8 (Figure 4B). This increase correlated with the degree of inflammation as revealed by expression of the proinflammatory cytokine interleukin-1β (Figure 4C). Hepatic FGFR2-IIIb mRNA expression levels showed a wide variation during the course of fibrosis development, with higher expression levels in some, but not all animals at week 8 (Figure 4D).
Figure 4-4237.
KGF and FGFR2-IIIb mRNA expression in an animal model of hepatic fibrosis. Mice were injected intraperitoneally with carbon tetrachloride (CCl4; 1 μl/g body weight, diluted 1:20 in mineral oil) three times weekly, for 5 or 8 weeks, respectively (six animals per group). Animals were sacrificed 24 hours after the last intraperitoneal injection and hepatic RNA was isolated. Control animals were injected intraperitoneally with mineral oil alone for 8 weeks (n = 3). In addition, four mice received only a single injection of CCl4 and were sacrificed 3 days thereafter. A: Hepatic KGF, interleukin-1β, and FGFR2-IIIb mRNA levels were analyzed by RNase protection assays. Hybridization of the same samples with a GAPDH riboprobe served as a loading control and 50 μg of tRNA as a negative control. The major protected fragments are indicated by arrows. B–D: Analysis of the obtained KGF, interleukin-1β, and FGFR2-IIIb bands by phosphoimaging. Data are expressed as fold-induction compared to controls (mean ± SD).
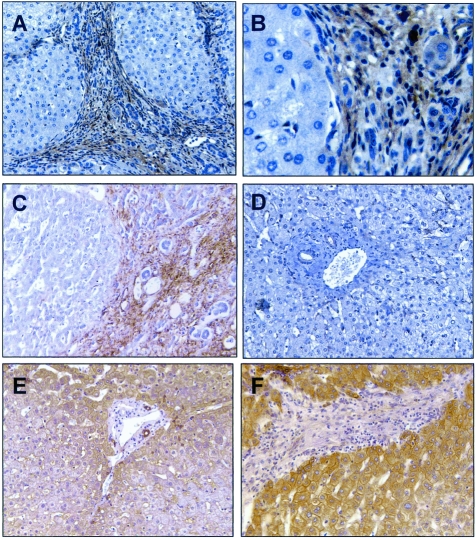
KGF and FGFR2-IIIb Expression in Chronic Liver Disease in Situ
Next we localized KGF and FGFR2-IIIb expression in diseased livers. For this purpose, we performed immunohistochemistry with a specific antibody for KGF using sections from cirrhotic livers of patients with different underlying liver disease. Figure 5 shows representative immunohistochemical KGF staining of cirrhotic tissue of a patient with chronic hepatitis C (Figure 5, A and B). Immunosignals were exclusively localized in the fibrotic septa corresponding to myofibroblast-like cells. Furthermore, consecutive cirrhotic liver sections were stained for α-SMA, a marker for activated HSCs and myofibroblasts36(Figure 5C). Co-localization of α-SMA and KGF immunosignals confirmed activated HSCs/myofibroblasts as the cellular source of KGF expression in situ. In contrast, no KGF immunostaining was visible in healthy livers (Figure 5D). Immunohistochemical staining applying a specific antibody raised against the cytoplasmic region of FGFR2 revealed expression of this receptor strictly localized to hepatocytes in healthy human liver tissue (Figure 5E). In accordance with the mRNA expression data, FGFR2 immunostaining was more intense in hepatic tissue of patients with chronic hepatitis C infection and moderate fibrosis (staging 1 or 2) (Figure 5F) whereas in cirrhotic liver tissues the FGFR2 immunosignal revealed strong variations between individual patients (data not shown). However, also in diseased livers FGFR2 immunostaining was exclusively found in hepatocytes independent of the stage of fibrosis. Control experiments using an equivalent amount of serum or isotype antibody, or the secondary antibody alone confirmed specificity of the immunosignals (data not shown).
Figure 5-4237.
KGF and FGFR2-IIIb expression in chronic liver disease in situ. KGF (A, B, D), FGFR2-IIIb (E, F), and α-SMA immunostaining (C) of cirrhotic (A–C), mildly fibrotic (stage 2) (F), and healthy (D, E) human liver tissue. Color was developed using diaminobenzidine as a substrate. Counterstaining was performed with H&E. Original magnifications: ×200 (A, C–F); ×630 (B).
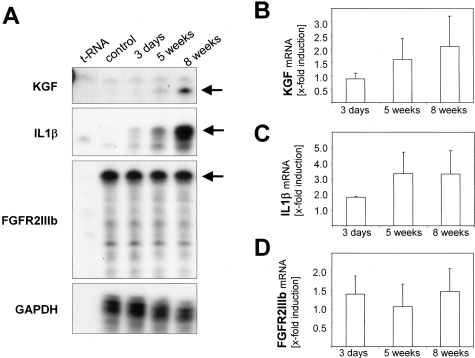
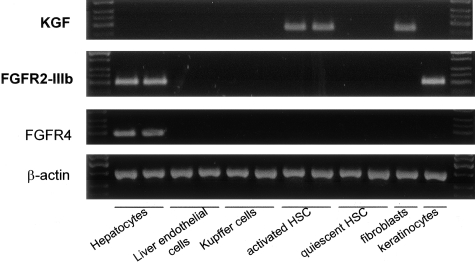
KGF and FGFR2-IIIb Expression in Parenchymal and Nonparenchymal Liver Cells
To further characterize and identify the cells responsible for KGF and FGFR2-IIIb expression in healthy and diseased livers, we analyzed the expression of the ligand and its receptor in freshly isolated human hepatocytes, KCs, ECs, and HSCs by RT-PCR. Furthermore, based on the findings that KGF mRNA expression was increased in fibrotic tissues, we analyzed activated human HSCs. Interestingly, KGF mRNA expression was found only in activated, but not in quiescent HSCs or other liver cells (Figure 6, first panel). FGFR2-IIIb mRNA expression was exclusively detected in hepatocytes (Figure 6, second panel). The expression of this receptor in freshly isolated hepatocytes was also confirmed by RNase protection assay (data not shown). RNA from fibroblasts was used as a positive control for KGF expression and as a negative control for FGFR2-IIIb expression. RNA from keratinocytes was used as a positive control for FGFR2-IIIb expression and as a negative control for KGF expression.2 For comparison, FGFR4 expression was analyzed because it has been shown previously that this receptor plays an important role in hepatic fibrosis.37 In accordance with previous studies analyzing mRNA and protein expression of this FGF receptor in human and rat tissues,38,39 FGFR4 expression was found exclusively in human hepatocytes (Figure 6, third panel).
Figure 6-4237.
Expression of KGF mRNA in HSCs and of FGFR2-IIIb mRNA in hepatocytes. KGF and FGFR2-IIIb mRNA levels were determined by RT-PCR in freshly isolated human hepatocytes, KCs, ECs, HSCs, and in culture-activated HSCs, respectively. Liver cells from two different donors were analyzed. Primary human fibroblasts and keratinocytes served as positive controls for KGF or FGFR2-IIIb expression, respectively. For comparison, FGFR4 expression was also determined. β-Actin expression was analyzed to demonstrate equal loading and integrity of the RNA.
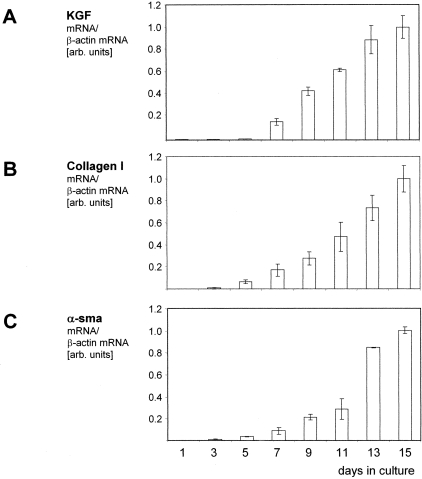
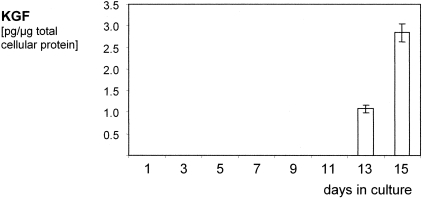
KGF Expression in HSCs
As a next step, we determined the expression of KGF during the course of in vitro activation of human HSCs. In parallel to KGF, we determined collagen type I and α-SMA expression by real-time RT-PCR. Beginning at day 5 of culture, there was little KGF mRNA detectable. However, between day 7 and day 13 there was a remarkable increase in KGF mRNA expression in activated HSCs (Figure 7A). The time course of KGF mRNA expression widely paralleled the one of collagen α1(I) and α-SMA (Figure 7, B and C). However, both collagen α1(I) and α-SMA mRNAs were detectable already earlier than KGF mRNA during the course of HSC activation. Furthermore, we determined KGF protein expression by HSCs during the course of in vitro activation. Secretion of KGF into the supernatant was analyzed by enzyme-linked immunosorbent assay. Consistent with the RNA data, KGF was detectable only in the supernatant of fully activated HSCs (day 13) (Figure 8).
Figure 7-4237.
Up-regulation of KGF mRNA expression during the course of HSC activation in vitro. Freshly isolated human HSCs were cultured on plastic for the indicated periods of time (1 to 15 days). Subsequently, RNA was isolated and KGF (A), collagen I (B), and α-SMA (C) mRNA expressions were analyzed by quantitative RT-PCR. Data represent the mean (±SD) of three independent analyses.
Figure 8-4237.
KGF is secreted by HSCs during in vitro activation. Freshly isolated human HSCs were cultured on plastic, supernatants were harvested at the indicated time points (days 1 to 15). KGF concentrations were determined by enzyme-linked immunosorbent assay and normalized to total cellular protein content. Data represent the mean (±SD) of three independent analyses.
Discussion
The aim of this study was to investigate the expression and the cellular sources of KGF and its receptor, FGFR2-IIIb, in normal and diseased liver. Although there are only very low levels of KGF mRNA in healthy murine and human liver, we found a strongly increased expression of this growth factor in diseased liver. Most importantly, KGF mRNA levels correlated significantly with the stage of fibrosis in patients chronically infected with hepatitis C (HCV). Highest expression levels were found in HCV patients with advanced fibrosis or cirrhosis, and our data obtained from cirrhotic patients with several other underlying liver diseases indicate that enhanced KGF expression is a general feature of cirrhotic liver. This was also confirmed in a mouse model of liver cirrhosis in which the levels of KGF mRNA correlated with the extent of fibrosis and inflammation.
The activation of HSCs is widely considered as the key event of hepatic fibrosis. Studies assessing both experimental models of liver fibrosis and human fibrogenesis demonstrated a positive correlation between the degree of fibrosis and the accumulation of activated HSCs in the damaged liver.40,41 Interestingly, we found that in vitro-activated human HSCs express KGF. In accordance with the results obtained with nondiseased liver tissue, quiescent HSCs and other nonparenchymal and parenchymal liver cells did not express KGF. Immunohistochemistry revealed localized KGF signals in myofibroblast-like cells in fibrotic septa of diseased livers and herewith confirmed that activated HSCs/myofibroblasts are also in vivo the cellular source of KGF.
The activation of HSCs occurs early after the onset of a hepatic injury. However, analysis of the murine hepatic fibrosis model reveals that the single application of a toxic CCl4 dose does not result in a significant up-regulation of hepatic KGF mRNA expression. The latter occurs later during the progression to the chronic stage. This is in accordance with the time course of KGF expression during the in vitro activation of HSCs. In comparison to α-SMA and collagen I, KGF mRNA expression occurs delayed in the fully activated HSCs.
KGF activity is mediated via binding to a specific FGFR2 isoform generated by an alternative splicing mechanism.6,42,43 It has been shown previously that murine and rat hepatocytes express functional KGF receptors in vivo17 and in vitro,44 and that KGF induces proliferation of these cells44 and protects them from tumor necrosis factor-induced apoptosis.45 However, it was unclear if this is also true for human hepatocytes, because they did not show a mitogenic response to KGF in vitro.44 In this study we show that human hepatocytes express FGFR2-IIIb in vivo. This discrepancy between our in vivo results and the previous in vitro data may be because of down-regulation of the KGF receptor in human hepatocytes in culture. Alternatively, culturing may select for a specific subpopulation of hepatocytes, which does not express FGFR2-IIIb but FGFR2-IIIc. Thus, in first experiments we also found low levels of FGFR2-IIIc mRNA in freshly isolated hepatocytes (data not shown). Because expression of FGFR2-IIIb and IIIc has been shown to be mutually exclusive,46,47 a subpopulation of hepatocytes may express the IIIc splice variant, possibly as a first step toward epithelial-mesenchymal transition.48 These cells may be enriched on culturing of hepatocytes.
Interestingly, our results demonstrate that FGFR2-IIIb is up-regulated during the early stage of liver fibrosis. This finding is consistent with results from Hu and colleagues,19 who showed increased expression of FGFR2 in the regenerating liver. Interestingly, hepatocytes seem to be the only cells that express this type of receptor in healthy and diseased livers. Therefore, the relatively high loss of hepatocytes in livers with advanced fibrosis or cirrhosis may explain the overall lower FGFR2-IIIb levels compared to diseased livers with no or only mild fibrosis.
In addition to KGF, the activation of HSCs is known to be associated with the de novo expression of numerous genes, some of which encode other growth factors such as hepatocyte growth factor, transforming growth factor-β1, or platelet-derived growth factor. However, in contrast to KGF, activated HSCs also express the corresponding receptors for these growth factors. In addition to paracrine effects, hepatocyte growth factor, transforming growth factor-β1, platelet-derived growth factor, and other factors are known to play important roles in the initiation and perpetuation of the activation process of HSCs by autocrine mechanisms. In contrast, the lack of detectable FGFR2-IIIb expression in quiescent, as well as in activated HSCs indicates that KGF acts exclusively as a paracrine factor for hepatocytes. This is consistent with results obtained in other tissues, in which KGF is expressed by mesenchymal cells or γδT cells, whereas the receptor is present on epithelial cells.2
Under physiological conditions HSCs are present in their quiescent stage in healthy livers and do not express KGF. After hepatic injury, HSCs transform to their activated stage and secrete KGF. They are present in acute as well as in chronically diseased livers and they accumulate with the ongoing process of fibrosis. Cirrhosis may result as the consequence of sustained fibrosis, a condition that is the major risk factor for the development of hepatocellular carcinoma. Therefore, one might speculate about possible functions of KGF during development and/or progression of hepatocellular carcinoma. However, there is as yet little evidence for a role of KGF in tumorigenesis, and FGFR2-positive human carcinomas transplanted subcutaneously into nude mice were not growth-stimulated by systemic treatment with recombinant KGF or KGF-2.49,50 In contrary, recent studies demonstrated that expression of FGFR2-IIIb by tumor cells correlates with a well-differentiated phenotype, whereas loss of this receptor correlates with malignancy. Thus, it has been suggested that FGFR2-IIIb even acts as a tumor suppressor.51–53
The complex role of different FGFs and their receptors in controlling hepatic cell-cell interactions and fibrosis has been recently shown by elegant studies with FGFR4-deficient and FGF1/FGF2 double-knockout mice.54 In these studies, FGFR4 deficiency was shown to enhance fibrosis, whereas loss of FGF1 and FGF2 had the opposite effect.37 In this context, the mutually exclusive expression of KGF and its high-affinity receptor FGFR2-IIIb on activated HSCs/myofibroblasts and primary hepatocytes appears unique and intriguing. Further functional studies have to be performed to fully elucidate the role of KGF signaling in different types of liver disease. However, because KGF exerts mitogenic and anti-apoptotic effects on hepatocytes,17,44,45,55,56 we would like to propose that the high levels of KGF expressed by activated HSCs/myofibroblasts during chronic liver disease may have a beneficial effect because of enhancement of hepatocyte survival and proliferation. This would suggest the use of exogenous KGF for the treatment of cirrhotic liver disease and this possibility should be experimentally addressed in the future.
Acknowledgments
We thank Christiane Born-Berclaz for excellent technical assistance and Dr. Katalin Korodi for help with the mouse experiments.
Footnotes
Address reprint requests to Claus Hellerbrand, M.D., Dept. of Internal Medicine I, University of Regensburg, D-93042 Regensburg, Germany. E-mail: claus.hellerbrand@klinik.uni-regensburg.de.
Supported by grants from the Swiss National Science Foundation (grant 31-61358.00 to S.W.), the Deutsche Forschungsgemeinschaft (to C.H.), and by the Else Kröner Fresenius-Stiftung (to C.H.).
H.S. and M.M. contributed equally to this study.
References
- Rubin JS, Osada H, Finch PW, Taylor WG, Rudikoff S, Aaronson SA. Purification and characterization of a newly identified growth factor specific for epithelial cells. Proc Natl Acad Sci USA. 1989;86:802–806. doi: 10.1073/pnas.86.3.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner S. Keratinocyte growth factor: a unique player in epithelial repair processes. Cytokine Growth Factor Rev. 1998;9:153–165. doi: 10.1016/s1359-6101(98)00010-0. [DOI] [PubMed] [Google Scholar]
- Boismenu R, Havran WL. Modulation of epithelial cell growth by intraepithelial gamma delta T cells. Science. 1994;266:1253–1255. doi: 10.1126/science.7973709. [DOI] [PubMed] [Google Scholar]
- Winkles JA, Alberts GF, Chedid M, Taylor WG, DeMartino S, Rubin JS. Differential expression of the keratinocyte growth factor (KGF) and KGF receptor genes in human vascular smooth muscle cells and arteries. J Cell Physiol. 1997;173:380–386. doi: 10.1002/(SICI)1097-4652(199712)173:3<380::AID-JCP10>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Jameson J, Ugarte K, Chen N, Yachi P, Fuchs E, Boismenu R, Havran WL. A role for skin gamma delta T cells in wound repair. Science. 2002;296:747–749. doi: 10.1126/science.1069639. [DOI] [PubMed] [Google Scholar]
- Miki T, Fleming TP, Bottaro DP, Rubin JS, Ron D, Aaronson SA. Expression cDNA cloning of the KGF receptor by creation of a transforming autocrine loop. Science. 1991;251:72–75. doi: 10.1126/science.1846048. [DOI] [PubMed] [Google Scholar]
- Werner S, Peters KG, Longaker MT, Fuller-Pace F, Banda MJ, Williams LT. Large induction of keratinocyte growth factor expression in the dermis during wound healing. Proc Natl Acad Sci USA. 1992;89:6896–6900. doi: 10.1073/pnas.89.15.6896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskin LS, Sutherland RS, Thomson AA, Nguyen HT, Morgan DM, Hayward SW, Hom YK, DiSandro M, Cunha GR. Growth factors in bladder wound healing. J Urol. 1997;157:2388–2395. [PubMed] [Google Scholar]
- Ichimura T, Finch PW, Zhang G, Kan M, Stevens JL. Induction of FGF-7 after kidney damage: a possible paracrine mechanism for tubule repair. Am J Physiol. 1996;271:F967–F976. doi: 10.1152/ajprenal.1996.271.5.F967. [DOI] [PubMed] [Google Scholar]
- Brauchle M, Madlener M, Wagner AD, Angermeyer K, Lauer U, Hofschneider PH, Gregor M, Werner S. Keratinocyte growth factor is highly overexpressed in inflammatory bowel disease. Am J Pathol. 1996;149:521–529. [PMC free article] [PubMed] [Google Scholar]
- Finch PW, Cheng AL. Analysis of the cellular basis of keratinocyte growth factor overexpression in inflammatory bowel disease. Gut. 1999;45:848–855. doi: 10.1136/gut.45.6.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj-Elliott M, Breese E, Poulsom R, Fairclough PD, MacDonald TT. Keratinocyte growth factor in inflammatory bowel disease Increased mRNA transcripts in ulcerative colitis compared with Crohn’s disease in biopsies and isolated mucosal myofibroblasts. Am J Pathol. 1997;151:1469–1476. [PMC free article] [PubMed] [Google Scholar]
- Werner S, Smola H, Liao X, Longaker MT, Krieg T, Hofschneider PH, Williams LT. The function of KGF in morphogenesis of epithelium and reepithelialization of wounds. Science. 1994;266:819–822. doi: 10.1126/science.7973639. [DOI] [PubMed] [Google Scholar]
- Chen Y, Chou K, Fuchs E, Havran WL, Boismenu R. Protection of the intestinal mucosa by intraepithelial gamma delta T cells. Proc Natl Acad Sci USA. 2002;99:14338–14343. doi: 10.1073/pnas.212290499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell CL, Rex KL, Chen JN, Bready JV, DiPalma CR, Kaufman SA, Rattan A, Scully S, Lacey DL. The effects of keratinocyte growth factor in preclinical models of mucositis. Cell Prolif. 2002;35(Suppl 1):S78–S85. doi: 10.1046/j.1365-2184.35.s1.8.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meropol NJ, Somer RA, Gutheil J, Pelley RJ, Modiano MR, Rowinsky EK, Rothenberg ML, Redding SW, Serdar CM, Yao B, Heard R, Rosen LS. Randomized phase I trial of recombinant human keratinocyte growth factor plus chemotherapy: potential role as mucosal protectant. J Clin Oncol. 2003;21:1452–1458. doi: 10.1200/JCO.2003.10.079. [DOI] [PubMed] [Google Scholar]
- Housley RM, Morris CF, Boyle W, Ring B, Biltz R, Tarpley JE, Aukerman SL, Devine PL, Whitehead RH, Pierce GF. Keratinocyte growth factor induces proliferation of hepatocytes and epithelial cells throughout the rat gastrointestinal tract. J Clin Invest. 1994;94:1764–1777. doi: 10.1172/JCI117524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Z, Evarts RP, Fujio K, Marsden ER, Thorgeirsson SS. Expression of fibroblast growth factor receptors flg and bek during hepatic ontogenesis and regeneration in the rat. Cell Growth Differ. 1995;6:1019–1025. [PubMed] [Google Scholar]
- Steiling H, Wustefeld T, Bugnon P, Brauchle M, Fassler R, Teupser D, Thiery J, Gordon JI, Trautwein C, Werner S. Fibroblast growth factor receptor signaling is crucial for liver homeostasis and regeneration. Oncogene. 2003;22:4380–4388. doi: 10.1038/sj.onc.1206499. [DOI] [PubMed] [Google Scholar]
- Friedman SL. Molecular regulation of hepatic fibrosis, an integrated cellular response to tissue injury. J Biol Chem. 2000;275:2247–2250. doi: 10.1074/jbc.275.4.2247. [DOI] [PubMed] [Google Scholar]
- Friedman SL. Liver fibrosis—from bench to bedside. J Hepatol. 2003;38(Suppl 1):S38–S53. doi: 10.1016/s0168-8278(02)00429-4. [DOI] [PubMed] [Google Scholar]
- Marcellin P, Asselah T, Boyer N. Fibrosis and disease progression in hepatitis C. Hepatology. 2002;36:S47–S56. doi: 10.1053/jhep.2002.36993. [DOI] [PubMed] [Google Scholar]
- Reeves HL, Friedman SL. Activation of hepatic stellate cells—a key issue in liver fibrosis. Front Biosci. 2002;7:808–826. doi: 10.2741/reeves. [DOI] [PubMed] [Google Scholar]
- Cassiman D, Roskams T. Beauty is in the eye of the beholder: emerging concepts and pitfalls in hepatic stellate cell research. J Hepatol. 2002;37:527–535. doi: 10.1016/s0168-8278(02)00263-5. [DOI] [PubMed] [Google Scholar]
- Ramadori G, Saile B. Mesenchymal cells in the liver—one cell type or two? Liver. 2002;22:283–294. doi: 10.1034/j.1600-0676.2002.01726.x. [DOI] [PubMed] [Google Scholar]
- Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ. Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology. 1994;19:1513–1520. [PubMed] [Google Scholar]
- Weiss TS, Jahn B, Cetto M, Jauch KW, Thasler WE. Collagen sandwich culture affects intracellular polyamine levels of human hepatocytes. Cell Prolif. 2002;35:257–267. doi: 10.1046/j.1365-2184.2002.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellerbrand, Wang SC, Tsukamoto H, Brenner DA, Rippe RA. Expression of intracellular adhesion molecule 1 by activated hepatic stellate cells. Hepatology. 1996;24:670–676. doi: 10.1002/hep.510240333. [DOI] [PubMed] [Google Scholar]
- Rogler G, Hausmann M, Vogl D, Aschenbrenner E, Andus T, Falk W, Andreesen R, Scholmerich J, Gross V. Isolation and phenotypic characterization of colonic macrophages. Clin Exp Immunol. 1998;112:205–215. doi: 10.1046/j.1365-2249.1998.00557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theuerkauf I, Zhou H, Fischer HP. Immunohistochemical patterns of human liver sinusoids under different conditions of pathologic perfusion. Virchows Arch. 2001;438:498–504. doi: 10.1007/s004280000364. [DOI] [PubMed] [Google Scholar]
- Wach F, Bosserhoff A, Kurzidym U, Nowok K, Landthaler M, Hein R. Effects of mometasone furoate on human keratinocytes and fibroblasts in vitro. Skin Pharmacol Appl Skin Physiol. 1998;11:43–51. doi: 10.1159/000029807. [DOI] [PubMed] [Google Scholar]
- Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- Werner S, Weinberg W, Liao X, Peters KG, Blessing M, Yuspa SH, Weiner RL, Williams LT. Targeted expression of a dominant-negative FGF receptor mutant in the epidermis of transgenic mice reveals a role of FGF in keratinocyte organization and differentiation. EMBO J. 1993;12:2635–2643. doi: 10.1002/j.1460-2075.1993.tb05924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun S, Hanselmann C, Gassmann MG, auf dem Keller U, Born-Berclaz C, Chan K, Kan YW, Werner S. Nrf2 transcription factor, a novel target of keratinocyte growth factor action which regulates gene expression and inflammation in the healing skin wound. Mol Cell Biol. 2002;22:5492–5505. doi: 10.1128/MCB.22.15.5492-5505.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner S, Weinberg W, Liao X, Peters KG, Blessing M, Yuspa SH, Weiner RL, Williams LT. Targeted expression of a dominant-negative FGF receptor mutant in the epidermis of transgenic mice reveals a role of FGF in keratinocyte organization and differentiation. EMBO J. 1993;12:2635–2643. doi: 10.1002/j.1460-2075.1993.tb05924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hautekeete ML, Geerts A. The hepatic stellate (Ito) cell: its role in human liver disease. Virchows Arch. 1997;430:195–207. doi: 10.1007/BF01324802. [DOI] [PubMed] [Google Scholar]
- Yu C, Wang F, Jin C, Wu X, Chan WK, McKeehan WL. Increased carbon tetrachloride-induced liver injury and fibrosis in FGFR4-deficient mice. Am J Pathol. 2002;161:2003–2010. doi: 10.1016/S0002-9440(10)64478-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan M, Wu X, Wang F, McKeehan WL. Specificity for fibroblast growth factors determined by heparan sulfate in a binary complex with the receptor kinase. J Biol Chem. 1999;274:15947–15952. doi: 10.1074/jbc.274.22.15947. [DOI] [PubMed] [Google Scholar]
- Hughes SE. Differential expression of the fibroblast growth factor receptor (FGFR) multigene family in normal human adult tissues. J Histochem Cytochem. 1997;45:1005–1019. doi: 10.1177/002215549704500710. [DOI] [PubMed] [Google Scholar]
- Ballardini G, Degli ES, Bianchi FB, de Giorgi LB, Faccani A, Biolchini L, Busachi CA, Pisi E. Correlation between Ito cells and fibrogenesis in an experimental model of hepatic fibrosis A sequential stereological study. Liver. 1983;3:58–63. doi: 10.1111/j.1600-0676.1983.tb00850.x. [DOI] [PubMed] [Google Scholar]
- Knittel T, Kobold D, Piscaglia F, Saile B, Neubauer K, Mehde M, Timpl R, Ramadori G. Localization of liver myofibroblasts and hepatic stellate cells in normal and diseased rat livers: distinct roles of (myo-)fibroblast subpopulations in hepatic tissue repair. Histochem Cell Biol. 1999;112:387–401. doi: 10.1007/s004180050421. [DOI] [PubMed] [Google Scholar]
- Ornitz DM, Itoh N. Fibroblast growth factors. Genome Biol. 2001;2 doi: 10.1186/gb-2001-2-3-reviews3005. REVIEWS3005. 1–3005.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basilico C, Moscatelli D. The FGF family of growth factors and oncogenes. Adv Cancer Res. 1992;59:115–165. doi: 10.1016/s0065-230x(08)60305-x. [DOI] [PubMed] [Google Scholar]
- Strain AJ, McGuinness G, Rubin JS, Aaronson SA. Keratinocyte growth factor and fibroblast growth factor action on DNA synthesis in rat and human hepatocytes: modulation by heparin. Exp Cell Res. 1994;210:253–259. doi: 10.1006/excr.1994.1037. [DOI] [PubMed] [Google Scholar]
- Senaldi G, Shaklee CL, Simon B, Rowan CG, Lacey DL, Hartung T. Keratinocyte growth factor protects murine hepatocytes from tumor necrosis factor-induced apoptosis in vivo and in vitro. Hepatology. 1998;27:1584–1591. doi: 10.1002/hep.510270618. [DOI] [PubMed] [Google Scholar]
- Jones RB, Wang F, Luo Y, Yu C, Jin C, Suzuki T, Kan M, McKeehan WL. The nonsense-mediated decay pathway and mutually exclusive expression of alternatively spliced FGFR2IIIb and -IIIc mRNAs. J Biol Chem. 2001;276:4158–4167. doi: 10.1074/jbc.M006151200. [DOI] [PubMed] [Google Scholar]
- Baraniak AP, Lasda EL, Wagner EJ, Garcia-Blanco MA. A stem structure in fibroblast growth factor receptor 2 transcripts mediates cell-type-specific splicing by approximating intronic control elements. Mol Cell Biol. 2003;23:9327–9337. doi: 10.1128/MCB.23.24.9327-9337.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savagner P, Valles AM, Jouanneau J, Yamada KM, Thiery JP. Alternative splicing in fibroblast growth factor receptor 2 is associated with induced epithelial-mesenchymal transition in rat bladder carcinoma cells. Mol Biol Cell. 1994;5:851–862. doi: 10.1091/mbc.5.8.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderson R, Gohari-Fritsch S, Olsen H, Roschke V, Vance C, Connolly K. In vitro and in vivo effects of repifermin (keratinocyte growth factor-2, KGF-2) on human carcinoma cells. Cancer Chemother Pharmacol. 2002;50:202–212. doi: 10.1007/s00280-002-0493-8. [DOI] [PubMed] [Google Scholar]
- Ning S, Shui C, Khan WB, Benson W, Lacey DL, Knox SJ. Effects of keratinocyte growth factor on the proliferation and radiation survival of human squamous cell carcinoma cell lines in vitro and in vivo. Int J Radiat Oncol Biol Phys. 1998;40:177–187. doi: 10.1016/s0360-3016(97)00561-0. [DOI] [PubMed] [Google Scholar]
- Matsubara A, Kan M, Feng S, McKeehan WL. Inhibition of growth of malignant rat prostate tumor cells by restoration of fibroblast growth factor receptor 2. Cancer Res. 1998;58:1509–1514. [PubMed] [Google Scholar]
- Ricol D, Cappellen D, El Marjou A, Gil-Diez-de-Medina S, Girault JM, Yoshida T, Ferry G, Tucker G, Poupon MF, Chopin D, Thiery JP, Radvanyi F. Tumour suppressive properties of fibroblast growth factor receptor 2-IIIb in human bladder cancer. Oncogene. 1999;18:7234–7243. doi: 10.1038/sj.onc.1203186. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wang H, Toratani S, Sato JD, Kan M, McKeehan WL, Okamoto T. Growth inhibition by keratinocyte growth factor receptor of human salivary adenocarcinoma cells through induction of differentiation and apoptosis. Proc Natl Acad Sci USA. 2001;98:11336–11340. doi: 10.1073/pnas.191377098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu C, Wang F, Jin C, Huang X, Miller DL, Basilico C, McKeehan WL. Role of fibroblast growth factor type 1 and 2 in carbon tetrachloride-induced hepatic injury and fibrogenesis. Am J Pathol. 2003;163:1653–1662. doi: 10.1016/S0002-9440(10)63522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes SJ, Themis M, Alison MR, Sarosi I, Coutelle C, Hodgson HJ. Synergistic growth factors enhance rat liver proliferation and enable retroviral gene transfer via a peripheral vein. Gastroenterology. 2000;118:591–598. doi: 10.1016/s0016-5085(00)70266-6. [DOI] [PubMed] [Google Scholar]
- Bosch A, McCray PB, Jr, Walters KS, Bodner M, Jolly DJ, van Es HH, Nakamura T, Matsumoto K, Davidson BL. Effects of keratinocyte and hepatocyte growth factor in vivo: implications for retrovirus-mediated gene transfer to liver. Hum Gene Ther. 1998;9:1747–1754. doi: 10.1089/hum.1998.9.12-1747. [DOI] [PubMed] [Google Scholar]