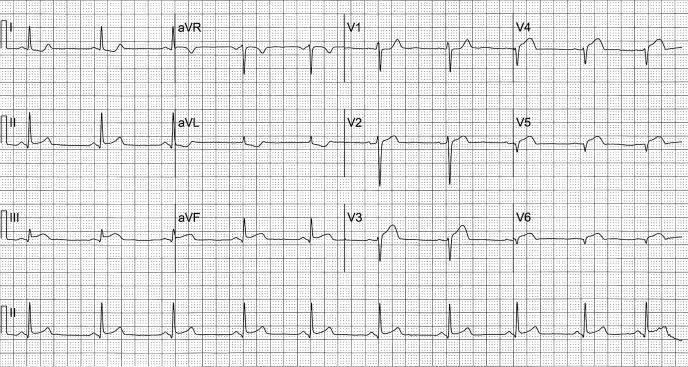
A 52-year-old man came to the emergency department at 3:00 am with constant retrosternal pain that had awakened him at 1:47 am and was accompanied by nausea. A standard 12-lead electrocardiogram showed 1 mm of ST-segment elevation in lead III with slightly less elevation in lead aVF and >0.5 mm elevation in lead II (Figure 1). The reciprocal ST-segment depression noted in leads I and aVL confirmed that the minor ST-segment elevation in leads II, III, and aVF represented inferior acute myocardial injury (1).
Figure 1.
Standard 12-lead electrocardiogram recorded when the patient first presented to the emergency department. See text for explication.
In the presence of inferior acute injury, the minor ST-segment depression in leads V2 to V6 suggested changes reciprocal to acute posterior myocardial injury. Lead V1 did not participate in the ST-segment depression because of a neutralizing anterior current of injury resulting from acute infarction of the right ventricle, which was located immediately behind lead V1.
A 12-lead electrocardiogram recorded 20 minutes later with the precordial leads on the right side of the chest showed obvious ST-segment elevation in leads V2R (lead V1L) through V6R, confirming acute infarction of the right ventricle (Figure 2). Lead V1R (V2L) showed slight ST-segment depression rather than elevation because it did not face the right ventricle, had an unimpeded look at the injured posterior wall of the left ventricle, and thus showed reciprocal depression.
Figure 2.
In this electrocardiogram, recorded 20 minutes after the electrocardiogram shown in Figure 1, the limb leads were recorded in the standard fashion and showed slightly more ST-segment elevation in leads II, III, and aVF and slightly more reciprocal depression in leads I and aVL than were seen in Figure 1. The precordial leads were recorded on the right side of the chest and showed ST-segment elevation in leads V2R (V1L) through V6R, indicative of right ventricular acute infarction.
Some 75% to 80% of inferior myocardial infarcts are due to occlusion of the right coronary artery, with most of the others due to occlusion of the left circumflex artery (2). In addition, five features of these two electrocardiograms indicate that the right, rather than the left circumflex, is the culprit coronary artery: 1) ST-segment elevation in lead III greater than that in lead II; 2) ST-segment depression in lead I; 3) an isoelectric ST segment in lead aVR; 4) ST-segment depression in lead V2 with an elevated or isoelectric ST segment in lead V1; and 5) ST-segment elevation >1 mm in any of the right-sided precordial leads (2). Coronary arteriography, performed a week after the onset of infarction, revealed a 95% narrowing in the midportion of the right coronary artery without significant disease in any other vessel. After the stenosis was dilated, a 2.5 × 28-mm Cypher stent was placed in the midportion of the right coronary artery.
The patient's risk factors for coronary disease were long-standing systemic arterial hypertension, an 80-pack-year history of cigarette smoking, a family history of coronary artery disease, a C-reactive protein level of 2.40 mg/dL (normal <0.90), and hyperlipidemia (low-density lipoprotein cholesterol, 146 mg/dL; high-density lipoprotein cholesterol, 43 mg/dL; triglycerides, 163 mg/dL). His infarct was small, with a peak serum troponin level of 9.67 ng/mL (normal <0.09), a peak creatine kinase level of 607 U/L (normal <230), and a level of the MB fraction of creatine kinase of 124.5 ng/mL (normal <8.1). Most importantly, except for mild left ventricular hypertrophy, his echocardiogram was normal with normal left ventricular segmental wall motion and ejection fraction (>55%).
Because the number of standard electrocardiographic leads with ST-segment elevation predicts the extent of left ventricular damage, and consequently the death rate, in ST-segment elevation myocardial infarction, this patient's electrocardiogram predicted a good outcome (3).
References
- 1.Glancy DL, Doghmi W. Use of indicative and reciprocal electrocardiographic changes to help localize the site of coronary occlusion. Proc (Bayl Univ Med Cent) 2001;14(1):104–105. doi: 10.1080/08998280.2001.11927740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nair R, Glancy DL. ECG discrimination between right and left circumflex coronary arterial occlusion in patients with acute inferior myocardial infarction: value of old criteria and use of lead aVR. Chest. 2002;122(1):134–139. doi: 10.1378/chest.122.1.134. [DOI] [PubMed] [Google Scholar]
- 3.Mauri F, Gasparini M, Barbonaglia L, Santoro E, Grazia Franzosi M, Tognoni G, Rovelli F. Prognostic significance of the extent of myocardial injury in acute myocardial infarction treated by streptokinase (the GISSI trial) Am J Cardiol. 1989;63(18):1291–1295. doi: 10.1016/0002-9149(89)91037-0. [DOI] [PubMed] [Google Scholar]