Abstract
Objective
The purpose of this study was to validate a 3-stage asthma case-detection procedure for elementary school-aged children.
Methods
The study was performed in 10 elementary schools in 4 inner-city school systems, with a total enrollment of 3539 children. Results of the case-detection procedure were compared with the diagnosis of an asthma specialist study physician, to determine the sensitivity and specificity of the case-detection procedure.
Results
Ninety-eight percent of children returned the asthma symptoms questionnaires, and 79% of those children consented to additional testing. Results indicated that the 3-stage procedure had good validity, with sensitivity, specificity, and predictive value of 82%, 93%, and 93%, respectively. A 2-stage procedure using questionnaires and spirometry had similar validity, with sensitivity, specificity, and predictive value of 78%, 93%, and 93%, respectively. However, given the time and expense associated with the 2- or 3-stage procedure and the difficulty of obtaining physician follow-up evaluation of the case-detection diagnosis, schools may prefer to use a 2-item questionnaire that has a lower sensitivity (66%) but higher specificity (96%) and predictive value (95%).
Conclusions
Case-detection programs are generally well received by school personnel and can identify children with unrecognized or undiagnosed disease, as well as those with a current diagnosis but poorly controlled disease. This study yields substantial information regarding the validity, yield, and specific types of children who might be identified with the use of such procedures. For the choice of the method of case detection used in a school, the strengths and weaknesses of each procedure, as well as the resources available for case detection, physician referral, and follow-up procedures, must be considered.
Asthma is the most common chronic childhood disease, with a prevalence of ∼69.8 cases per 1000 children among those 5 to 14 years of age.1 Approximately 9.2 million children <18 years of age have at some point in their lives been diagnosed as having asthma.2 Studies suggest that asthma is both undertreated and underdiagnosed,3-7 which leads to increased morbidity. Asthma-related morbidity is largely preventable with optimal diagnosis and treatment and improved patient education.8 Therefore, it may be beneficial to identify and treat children with undiagnosed or uncontrolled disease.
Case detection is a process to identify persons with unrecognized or undiagnosed disease and to distinguish those who have symptoms of the disease from those who do not.9 Schools provide an ideal setting for asthma case-detection programs for children. Asthma accounts for ∼14 million missed school days per year,10 more than any other chronic childhood condition,11-14 and these absenteeism rates can cause poor performance in school.13,15-17 In addition, the school setting can be used to implement therapeutic and educational interventions for students. Case detection and educational interventions are generally well received by school personnel and can identify children with unrecognized or undiagnosed disease,18,19 as well as those with a current diagnosis but poorly controlled disease.
School-based case-detection programs are currently hampered by the lack of validated tools. History recording, physical examinations, tests such as spirometry, and tests of bronchial hyperresponsiveness (BHR) are currently the primary means of diagnosing asthma. However, the costs of such methods have led researchers to attempt to use questionnaires for school-based asthma case-detection programs. Many questionnaires exist for use in detecting children who may have asthma; however, few have been validated by examining which questions are most predictive of abnormal lung function tests, positive exercise challenge tests, and physician diagnoses. Furthermore, many of those that have been validated produce large numbers of false-positive diagnoses.20-23 A high false-positive rate means that many children must undergo additional evaluation to determine whether a diagnosis of asthma is indicated. Although questionnaire programs are relatively inexpensive, they may not be cost-effective if they result in large numbers of children without the disease being referred to physicians. In areas where access to health care is difficult, such as for innercity, low-income populations, it is important to have a more cost-effective and specific case-detection procedure. Therefore, we developed and used a multistage procedure with questionnaires, spirometry, and exercise testing.18,24 This article reports on a study designed to determine the validity of the University of Alabama at Birmingham (UAB) multistage case-detection procedure.
METHODS
Study Design
This study was conducted in 10 elementary schools in 4 innercity school systems and was approved and monitored by the UAB institutional review board. Study enrollment was a 2-stage process. Asthma symptom questionnaires were distributed to the entire school population (n = 3539). Children who returned the questionnaires (n = 3463, 98%) were asked to enroll in the study. Written informed consent was obtained from the child's parent or guardian, and assent was obtained from each child.
Description of the Case-Detection Procedure Under Study
The UAB multistage asthma case-detection procedure has 3 stages, involving a symptoms questionnaire, spirometry testing, and a submaximal exercise challenge.24,25 The procedure is shown in Fig 1 and was originally developed by a group of pediatric asthma specialists as a method for detecting children with asthma for a school-based asthma management intervention (NHLBI N01 HR 56077). This case-detection procedure was designed to mimic the process through which a diagnosis of asthma is made in a clinical setting, using symptom histories, tests such as spirometry, and tests for BHR. Because the procedure was multistage, the questionnaire was designed to be as inclusive as possible. Items were adapted from existing measures used in community surveys, as well as criteria for diagnosis specified in National Asthma Education and Prevention Program (NAEPP) Expert Panel Report 2.8 The questionnaire was followed by spirometry, to test for airflow obstruction, and step testing, to evaluate BHR. Although methacholine challenge testing is the most widely used method for evaluating BHR, exercise challenge testing is an accepted method and is more feasible in a community-based setting, given the costs and strict medical supervision required for the use of methacholine challenge testing. Although different modes of exercise can be used for exercise challenge tests (eg, treadmill, free-run, or bicycle ergometer), the rationale behind all of them is the same. The participant starts at a slow speed and then advances until he or she reaches a heart rate of 80% to 90% of his or her predicted maximum. The patient continues to exercise at this rate for 4 to 6 minutes, and spirometry is performed at various times (ranging from 3 to 30 minutes) after cessation of exercise. The step test was chosen as the method for evaluating BHR in this school-based setting because it is a simple, portable, and reproducible measure that can be performed in a limited space, as opposed to the free-run test, which requires a large space in which to conduct the test.
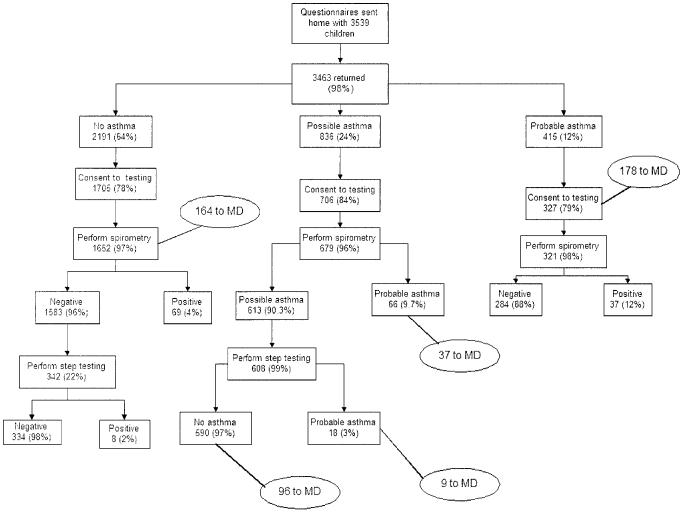
Fig 1.
Case-detection procedure.
First Phase
The parents of children are asked to complete a 5-item questionnaire (Table 1). On the basis of responses to the questionnaire, children are classified as having probable asthma, possible asthma, or no evidence of asthma (Fig 1). Children with probable asthma are referred to a physician and no additional testing is conducted. Children who are considered to have no evidence of asthma on the questionnaire undergo no additional testing.
TABLE 1.
Five-Item Questionnaire Used in the UAB Asthma Case-Detection Procedure
| 1. Has your child ever had wheezing or a whistling sound in the chest? | Yes □ | No □ |
| 1a. If yes, has this been in the past 12 months? | Yes □ | No □ |
| 2. Has your child ever had breathing problems (coughing, wheezing, whistling in the chest, shortness of breath, chest tightness) when he/she first woke up in the morning? | Yes □ | No □ |
| 2a. If yes, has this been in the past 12 months? | Yes □ | No □ |
| 3. Has your child ever had breathing problems (coughing, wheezing, whistling in the chest, shortness of breath, chest tightness) that woke him/her up at night? | Yes □ | No □ |
| 3a. If yes, has this been in the past 12 months? | Yes □ | No □ |
| 4. Has a doctor ever said your child has asthma? | Yes □ | No □ |
| 4a. If yes, has this been in the past 12 months? | Yes □ | No □ |
| 5. Has your child ever taken asthma medicine (pills, inhaler, or puffers) prescribed by a doctor? | Yes □ | No □ |
| 5a. If yes, has this been in the past 12 months? | Yes □ | No □ |
Probable asthma, yes to questions 4 and 5a; possible asthma, yes to ≥1 question; negative for asthma, no to all questions.
Second Phase
Consent forms requesting permission for the child to undergo spirometry and exercise challenge testing are sent to parents of children who were classified as having possible asthma with the questionnaire. Children with possible asthma whose parents give consent to testing perform a preexercise spirometry test. This test is performed with a portable Multispiro spirometer (Creative Biometrics, San Clemente, CA), which is calibrated daily. Children are tested by technicians with extensive experience and training in performing pulmonary function tests with children. Three forced vital capacity (FVC) maneuvers are performed for each child, and predicted values are determined on the basis of the standards of Polgar and Promadhat.26 Children with a forced expiratory volume in 1 second (FEV1)/FVC ratio of <80% are considered to have probable asthma and are referred to a physician for an asthma evaluation.27
Third Phase
Children with normal spirometry results (FEV1/FVC of ≥80%) perform a submaximal exercise challenge test as a test of BHR.24,25 This test involves stepping up and down on a single step (The Step; The Step Company). A step height of 6 inches is used for most children. However, if children are very fit (such that their heart rates do not increase to the required level) or taller than 5 feet 3 inches, then the step height is increased to 8 inches. The step height is always set so that the knee does not flex >90° when it is not bearing weight. The level of exercise intensity is selected to maintain a heart rate of ∼200 beats per minute and is maintained for 5 minutes. A heart rate monitor (Polar Electro, Woodbury, NY) is used to continuously monitor the heart rate during exercise. A standard metronome is used to maintain the stepping rate, and children are encouraged to “step” to the beat. Personnel step with the child and provide encouragement.
Spirometry is performed 3 and 10 minutes after cessation of the exercise challenge. Children are considered to have probable asthma and are referred to a physician for an asthma evaluation if they show a >15% decrease in FEV1 or a ≥25% decrease in FEF25-75 (forced expiratory rate between 25% and 75% of the FVC) from baseline after the exercise challenge.24 The procedures for and performance of the exercise challenge have been reported.24
Validation of the Case-Detection Procedure
The case-detection procedure under study is described above. The procedures used to validate the case-detection procedure are shown in Fig 2. The case-detection procedure requires no additional follow-up testing for children who are classified as having probable asthma or no evidence of asthma with the questionnaire. To validate the case-detection procedure, however, consent for additional testing was obtained from parents of all children (regardless their classification with the questionnaire). All children performed spirometry testing to provide test results for the physician to use at the clinic visit and to allow evaluation of the validity of the case-detection procedure. In addition, a sample (20%) of the children who were classified as having no evidence of asthma with the questionnaire underwent step testing to allow evaluation of the validity of the exercise challenge test. Children who were classified as having probable asthma with the questionnaire (those with a previous diagnosis who took medications in the past year) were not step tested because of the risk of adverse events.
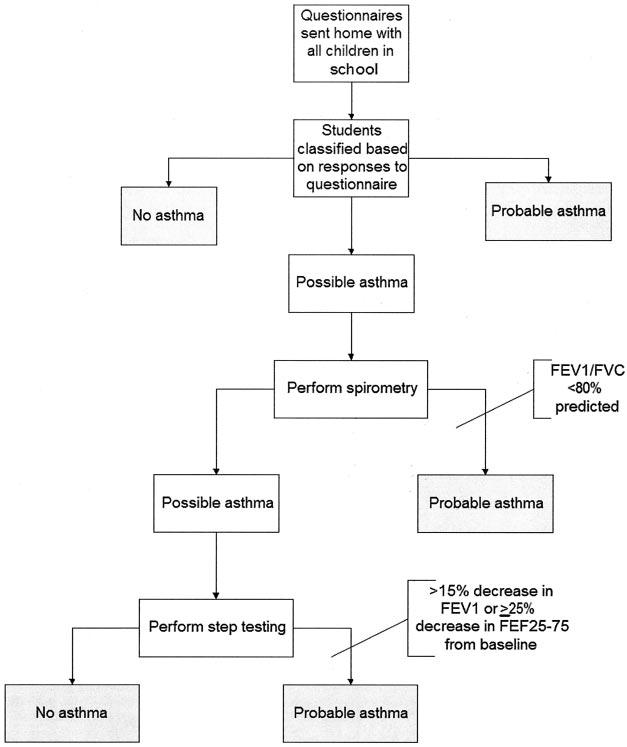
Fig 2.
Results from the validation study.
A diagnosis of asthma by a pediatric asthma specialist was used as the standard method8,28,29 for validation of the case-detection procedure. All children with a positive indication of asthma from the procedure (those classified as having probable asthma with the questionnaire and those classified as having probable asthma with spirometry or step testing) were to be examined by 1 of 4 asthma specialists. A random sample of children from the negative-indication group (those classified as having no evidence of asthma with the questionnaire and those classified as having no evidence of asthma with spirometry and step testing) was examined.
A clinic site was established at each school for the physician examinations, and a standard protocol for the diagnosis of asthma was developed with the NAEPP Guidelines for the Diagnosis and Management of Asthma.8,28 Pulmonary function tests and comprehensive medical history recording and physical examinations were performed for all children. A parent or guardian was present with the child during the clinic visit. The physicians were blinded with respect to the case-detection procedure indication but had access to spirometry and step test results.
Sensitivity and specificity were determined for the 3-stage (full) procedure, a 2-stage procedure (without the step test), and 2 questionnaire definitions (narrow and broad). The primary aim of the study was to estimate the sensitivity and specificity of the full (3-stage) procedure; however, we were interested in determining the validity of shorter procedures because these may be more feasible to implement in a school-based setting.
Asthma Education and Management Plans
Although this project was designed to determine the sensitivity and specificity of the asthma case-detection procedure, we felt ethically responsible for providing asthma management plans and education for children diagnosed with asthma. Individual asthma action plans (IAAPs) were developed by the study physicians for all children who were evaluated by 1 of the study physicians. IAAPs were adjusted for the level of asthma severity in accordance with the NAEPP guidelines.8,28 Written IAAPs were given to the school, the child's family, and the child's primary care provider. Rescue medication was provided for each child at home and school during the study period, and a prescription for rescue medication was given to the child's parent. Asthma education was provided to all children identified as having probable asthma in the screening procedure with the Open Airways curriculum30 and to the general student body with the Asthma Awareness curriculum.31 Managing Asthma: A Guide for Schools32 was used to educate school faculty and staff members.
Sample-Size Calculations
Estimates were based on data from a previous study conducted in a school system with similar demographic characteristics (N = 52 schools, 13 247 students).18 Previous response and participation rates indicated that the current population would yield 215 students classified as positive for asthma and 2561 students classified as negative for asthma. Assuming that no more than 25% of the 215 students classified as positive for asthma and no more than 10% of a stratified random sample of 240 of the 2561 no-asthma students were misclassified, we would estimate the sensitivity of the procedure with a 95% confidence interval (margin of error no greater than .032) for the best case (sensitivity: ≥95%) or 0.072 for the worst case (sensitivity: 50%). The specificity of the procedure would be estimated with a 95% confidence interval (margin of error no greater than .026) for the best case (specificity: ≥95%) or 0.06 for the worst case (specificity = 50%).
RESULTS
Overall Results
The demographic characteristics of the children participating in the study are shown in Table 2. Ninety-one percent of the children in these 4 city school systems were black, 8% were white, and 1% were Hispanic. A total of 2738 children (77% of the entire school population and 79% of those who returned the screening questionnaires) enrolled in the study.
TABLE 2.
Demographic Characteristics of Children Participating in the Study (n = 2738)
| No. (%) | |
|---|---|
| Gender | |
| Male | 1366 (50%) |
| Female | 1372 (50%) |
| Race | |
| Asian | 2 (<1%) |
| Black | 2482 (91%) |
| Hispanic | 23 (<1%) |
| White | 231 (8%) |
| Age, y, mean ± SD | 8.7 ± 1.65 |
Figure 2 shows the results of the case-detection procedure. Questionnaires were sent home with 3539 children in the 10 elementary schools, and 3463 (98%) were returned. Twenty-one of these were blank; therefore, 3442 children were classified on the basis of their parent's responses to the questionnaire. Twelve percent of the children (415 children) were classified as having probable asthma, 64% (2191 children) were classified as having no evidence of asthma, and 24% (836 children) were classified as having possible asthma.
Seven hundred six parents (84%) of children classified as having possible asthma consented to additional testing for their children. Six hundred seventy-nine (96%) of these children performed spirometry. Reasons for not performing spirometry for the 27 children who consented but did not undergo spirometry testing included repeated absences (n = 4) and physical or mental disabilities that rendered the child unable to perform spirometry (n = 23). Sixty-six of the 679 children (9.7%) tested were considered to have probable asthma with spirometry. Six hundred eight of the remaining 613 children (99%) performed the exercise challenge test. The primary reason for not performing the exercise challenge test was repeated absences. Eighteen of the 608 children (3%) who were tested were classified as having probable asthma with the exercise challenge test.
The case-detection procedure identified 499 children as “positive for asthma,” ie, either a probable diagnosis of asthma with the questionnaire (n = 415) or probable asthma detected with spirometry (n = 66) or step testing (n = 18). Three hundred twenty-seven of the 415 children (79%) identified with the questionnaire enrolled in the study, and 178 (54%) attended the physician visit. Seven hundred six of the children (84%) identified as having possible asthma with the questionnaire enrolled in the study. The case-detection procedure identified 84 of these as positive for asthma with spirometry (n = 66) or step testing (n = 18), and 46 (55%) came to the physician visit. Two thousand one hundred ninety-one children were classified as having no asthma with the questionnaire, and 1705 (78%) enrolled in the study. A random sample of 260 children (11%) who were classified as “negative for asthma” with the screening procedure, ie, classified as having no asthma with the symptom questionnaire (n = 1705) or classified as having possible asthma with the questionnaire but demonstrating negative spirometry and step test results (n = 590), attended the physician visit.
Full Procedure
Table 3 shows the comparison of each of the case-detection procedures with the physician diagnosis. The sensitivity of the full procedure was 82% and the specificity was 93%. The predictive value was 93%. The sensitivity and specificity of the procedure without the step test were very similar to those of the full procedure. The sensitivity was 78% and the specificity was 93%. The predictive value was 93%.
TABLE 3.
Comparison of the Case-Detection Procedures and the Physician Diagnosis
| Procedure | Physician Diagnosis | Case Detection Diagnosis, No. of Cases |
Sensitivity, % | Specificity, % | Predictive Value, % | ||
|---|---|---|---|---|---|---|---|
| Negative | Positive | Total | |||||
| Full procedure | Negative | 213 | 16 | 229 | |||
| Positive | 47 | 208 | 255 | ||||
| Total | 260 | 224 | 484 | 82 | 93 | 93 | |
| Without step test | Negative | 215 | 15 | 230 | |||
| Positive | 55 | 200 | 255 | ||||
| Total | 270 | 215 | 485 | 78 | 93 | 93 | |
| Broad questionnaire | Negative | 133 | 98 | 231 | |||
| Positive | 31 | 225 | 256 | ||||
| Total | 161 | 323 | 487 | 88 | 58 | 70 | |
| Narrow questionnaire | Negative | 222 | 9 | 231 | |||
| Positive | 87 | 169 | 256 | ||||
| Total | 309 | 178 | 487 | 66 | 96 | 95 | |
Questionnaire Only
We also examined the sensitivity and specificity of the questionnaire alone in detecting asthma. We did this by using 2 different definitions of asthma with the questionnaire. First, we used a very broad definition of asthma. With this definition, persons who answered yes to any single item on the questionnaire were classified as having asthma with the questionnaire. This is the group of children for whom we performed additional testing (spirometry and exercise challenge testing). Table 3 shows the validity of the questionnaire with this very broad definition of asthma. The sensitivity of the questionnaire was 88% and the specificity was 58%. The predictive value was 70%. Next, we examined the sensitivity and specificity of the questionnaire with a very narrow definition of asthma. With this narrow definition, persons who answered yes to both questions 4 and 5a were considered to have asthma with the questionnaire. This is the group that we called probable asthma in our case-detection procedure. Table 3 shows the comparison of the results determined with this narrow definition of asthma. The sensitivity was 66% and the specificity was 96%. The predictive value was 95%.
Tables 4 and 5 detail the physician visits. Four hundred ninety-nine children were classified as positive for asthma with the case-detection procedure. Children could be classified as positive for asthma in 1 of 3 ways, ie (1) probable asthma with the questionnaire (n = 415; 327 enrolled in the study), (2) possible asthma with the questionnaire and positive spirometry results (n = 66), or 3) possible asthma with the questionnaire and positive step test results (n = 18). Of the 415 children who were classified as positive for asthma on the basis of their questionnaire diagnosis, 327 enrolled in the study and 178 (54%) were examined by the study physicians. One hundred sixty-nine (95%) were determined to have asthma. Of the 66 children who were determined to have probable asthma on the basis of their spirometry results, 37 (56%) went to the study physician. Thirty-one (84%) were diagnosed as having asthma. Eighteen children were determined to have probable asthma on the basis of their exercise challenge test results, and 9 (50%) went to the study physician. Of these 9, 8 (89%) were diagnosed as having asthma. Two thousand seven hundred eighty-one children were classified as negative for asthma with the case-detection procedure. Children could be classified as negative for asthma in 1 of 2 ways, ie (1) negative for asthma with the questionnaire (n = 2191; 1705 enrolled in the study) or (2) possible asthma with the questionnaire but negative for asthma with spirometry and step testing (n = 590). Of the 2191 children who tested negative for asthma with the symptom questionnaire, 1705 (78%) enrolled in the study. A random sample of 10% of these children attended the physician visit (n = 164). Of these 164, 31 (19%) were determined to have asthma. Of the 590 children who were classified as having possible asthma with the questionnaire but were negative for asthma with spirometry and step testing, 96 (16%) went to the study physician and 16 (17%) were determined to have asthma.
TABLE 4.
Percentage of Children Attending the Physician Visit According to Case Detection Procedure Results
| Total Study Enrollment, No. | Physician Visit, No. (%) |
|||
|---|---|---|---|---|
| To Physician | Asthma | No Asthma | ||
| Positive | 411 | 224 (55) | 208 (93) | 16 (7) |
| Questionnaire | 327 | 178 (54) | 169 (95) | 9 (5) |
| Spirometry | 66 | 37 (56) | 31 (84) | 6 (16) |
| Step test | 18 | 9 (50) | 8 (89) | 1 (11) |
| Negative | 2295 | 260 (11) | 47 (18) | 213 (82) |
| Questionnaire | 1705 | 164 (10) | 31 (19) | 133 (81) |
| Spirometry/step test | 590 | 96 (16) | 16 (17) | 80 (83) |
| Total | 2706 | 484 | 255 | 229 |
TABLE 5.
Severity Classification of Asthma According to Case-Detection Procedure Results
| No. of Cases |
|||||
|---|---|---|---|---|---|
| Mild Intermittent* | Mild Persistent | Moderate Persistent | Severe | Total | |
| Positive | |||||
| Questionnaire | 60 | 62 | 45 | 2 | 169 |
| Spirometry | 9 | 8 | 14 | 0 | 31 |
| Step test | 5 | 2 | 1 | 0 | 8 |
| Negative | |||||
| Questionnaire | 16 | 7 | 8 | 0 | 31 |
| Spirometry/step test | 11 | 4 | 1 | 0 | 16 |
| Total | 101 | 83 | 69 | 2 | 255 |
Asthma severity.
Table 5 indicates the asthma severity ratings assigned by the study physicians, according to the case-detection procedure diagnoses. The majority of children who were examined by a physician and were diagnosed with asthma had mild persistent asthma (33%). All of the children with severe persistent asthma were classified as positive for asthma with the case-detection procedure, as a result of their answers to the questionnaire. In addition, a majority of children with either mild or moderate persistent asthma were classified as positive for asthma as a result of their answers to the questionnaire (75% and 65%, respectively).
DISCUSSION
The feasibility of a case-detection program is determined by a number of factors related to program performance, 1 of which is the yield of cases. One measure that is commonly considered in determining the success of programs is the predictive value of the case-detection procedure. The predictive value measures whether or not an individual actually has the disease, given the results of the case-detection procedure. It is the percentage of persons with the disease of those with positive test results. The predictive value is determined not only by factors that determine the validity of the test itself (such as sensitivity and specificity) but also by the characteristics of the population to which the test is applied. The major determinants of the predictive value are the specificity of the test and the prevalence of disease in the population. The more specific the test, the less likely an individual with a positive test result will be to be free of the disease and the greater the predictive value. Even slight decreases in specificity can dramatically decrease the predictive value of a test. As the prevalence of disease increases, the predictive value increases. No matter how specific the test, if the population is at low risk of having the disease, then results that are positive are mostly false-positive findings.
Table 6 compares the predictive values of the different procedures with different prevalences of disease. The high predictive values found in this study are a result of the high prevalence of asthma in the test population. To properly estimate the validity of the test (ie, sensitivity and specificity), we needed to enroll large numbers of persons with asthma. In addition, we needed to enroll only a sample of those who were classified as negative for asthma with the screening procedure. Therefore, the study population had a disease prevalence of ∼50%. Recent studies indicated that the prevalence of asthma among elementary school-aged children ranges from 10 to 20%.18,19,33,34 Therefore, the predictive values of the procedures described are likely to be lower in practice than seen in this study population. Furthermore, when these procedures are used in a community setting, children will most likely be referred to their primary care practitioner, who may be less apt to make a diagnosis of asthma than were the specialists participating in this study. This would also decrease the predictive value of the procedures.
TABLE 6.
Comparison of Predictive Values for the Different Procedures
| Procedure | Predictive Value, % |
|||
|---|---|---|---|---|
| 5%* | 10% | 25% | 50% | |
| Full procedure | 39 | 57 | 80 | 92 |
| Without step test | 38 | 56 | 79 | 92 |
| Questionnaire (broad) | 10 | 19 | 41 | 68 |
| Questionnaire (narrow) | 47 | 65 | 85 | 94 |
Prevalence of asthma.
It can be seen that the predictive values decrease dramatically as the prevalence of disease decreases. The best predictive value is achieved by using the narrow definition of asthma on the questionnaire. Use of a broader definition of asthma on the questionnaire gives a very low predictive value and would result in referral to the physician of many children who do not actually have the disease. Studies have shown that it is difficult to get parents to follow-up on the referral,33,35 and access to health care is difficult in many low-income areas. Therefore, one must be careful of overdiagnosing with a case-detection procedure. Case-detection procedures that result in fewer false-positive results may be more effective, because staff members can concentrate their efforts on the referral of fewer children. Undue emphasis on sensitivity may result in high costs and other problems engendered by excessive numbers of diagnostic evaluations.
In addition to consideration of the predictive value of the asthma case-detection procedure, the false-negative values of the different procedures must be considered. Table 7 shows the asthma severity rating for children who were incorrectly identified as negative for asthma with each of the case-detection procedures. Use of the broad definition of asthma with the questionnaire misses the fewest children, whereas use of the narrow definition of asthma with the questionnaire misses the most children. With all of the procedures, however, the majority of children missed would be classified as having mild intermittent asthma.
TABLE 7.
Comparison of False-Negative Results for the Different Procedures
| Procedure | No. of Cases |
|||
|---|---|---|---|---|
| Mild Intermittent* | Mild Persistent | Moderate Persistent | Total | |
| Full procedure | 27 (58%) | 11 (23%) | 9 (19%) | 47 (100%) |
| Without step test | 32 (58%) | 13 (24%) | 10 (18%) | 55 (100%) |
| Questionnaire (broad) | 16 (52%) | 7 (22%) | 8 (26%) | 31 (100%) |
| Questionnaire (narrow) | 42 (48%) | 21 (24%) | 24 (28%) | 87 (100%) |
Asthma severity.
The results of this study show that a 3-stage case-detection procedure for identifying children with asthma in schools has good validity. However, the feasibility of a case-detection procedure also depends on the ease of implementation of the procedure. Given the time and expense associated with exercise testing in the school setting and the low yield of asthmatics, the addition of the step test does not appear to be warranted for this population. These results are consistent with those of Gruchalla et al36 and Johansson et al,37 who also found that the step test was not effective for case detection of asthma among inner city children because of the large number of false-positive results and the lack of predictive ability. The broad definition of asthma with the questionnaire has a low predictive value and results in many unnecessary referrals to the physician; therefore, 2 better options are the narrow definition of asthma with the questionnaire or the questionnaire plus spirometry. The use of a narrow definition of asthma (only 2 questions) is simple and easy to use and has a good predictive value. However, it misses more children with persistent asthma than does use of the questionnaire plus spirometry. Furthermore, the use of the narrow definition of asthma yields only students who currently have a diagnosis of asthma and are taking medication for their asthma.
Use of the questionnaire plus spirometry has higher sensitivity and specificity and misses fewer children with asthma, compared with the 2-item questionnaire. In addition, children with asthma who are missed are more likely to have mild intermittent asthma. Recent research has found that spirometry screening in schools by community nurses is technically feasible.18,38 However, such testing can be difficult and requires training. In addition, some spirometry tests need to be reviewed by experts. Furthermore, it can be expensive to implement, and some communities, particularly those in inner-city areas, may not have the resources required to conduct spirometry testing.
In choosing a method of case detection, communities must consider the strengths and weaknesses of each procedure, as well as the resources available for case detection and physician referral. In consideration of costs, not only the costs of the case-detection procedure itself but also the costs of follow-up procedures for persons who are classified as positive for asthma with the case-detection procedure (including diagnosis and treatment) must be considered. The potential cost savings of the improvement in health for the children identified with the case-detection program must also be included. Such savings might include decreased emergency care and hospitalizations, increased school attendance, and decreased work loss for parents.
In this population of inner-city, low-income children, we found that, among children with a diagnosis of asthma (classified as having probable asthma with our questionnaire), health care visits were infrequent. Among the children who did not have a diagnosis of asthma but reported symptoms or had abnormal spirometry or exercise challenge test results, many did not identify a primary care practitioner to whom we could refer them for additional evaluation. This same difficulty was observed in our previous work in inner-city school systems.18 Yawn et al35 found that the process of linking children to health care was difficult even when health care was available. They found that very few parents followed up on referrals after the case-detection procedure. In fact, the case-detection procedure did not increase the identified prevalence of asthma.35 However, the case-detection procedure did increase the rates of asthma-related office visits and medication changes for children with previously diagnosed asthma.33 These changes might have long-term effects on days of school missed and numbers of emergency department visits and hospitalizations. Furthermore, all health care practitioners do not provide quality medical care for asthma that is delivered in accordance with NAEPP guidelines. Research has not documented that better identification of children with asthma leads to better asthma management. Better asthma management depends on many factors, including access to health care, the quality of that health care, and patient adherence with physician recommendations.
The primary limitation of this study is the use of a single physician evaluation as the standard method. Pierce et al40 argued that a series of physician examinations over time represents the best standard method for asthma detection; however, this is rarely practical in large epidemiologic studies. Validation studies vary in their use of a standard method for asthma detection, including measures of BHR, spirometry, and doctor diagnosis determined with chart review or self-report. However, validation of a questionnaire, compared with a single physiologic measure or self-report of a diagnosis, does not adequately capture the clinical presentation of asthma. Therefore, we chose to use a study physician's diagnosis as the standard method. Nonetheless, because pediatric asthma often requires follow-up visits to confirm peak flow variability, responses to treatment, and seasonal variability, this was a limitation of our study. Our study physicians did comment that it was sometimes difficult to make a diagnosis of asthma on the basis of a single visit.
Another limitation was the use of >1 practitioner for diagnosis. Although asthma diagnoses may vary considerably according to practitioner, the use of a standardized history form and diagnosis protocol reduced this possibility in our study. The study physicians designed a standardized history and physical diagnosis intake form and a standard protocol for the diagnosis of asthma, using the NAEPP Guidelines for the Diagnosis and Management of Asthma.8,28
Attendance at the physician visit was not universal. However, the response to the questionnaires was excellent (98% returned), and there were no differences in rates of consent for testing among the 3 groups (no asthma, possible asthma, and probable asthma). Among those who were classified as positive for asthma with the case-detection procedure, 55% attended the physician visit. This rate is very good for an inner-city population and was achieved through flexible scheduling and the creation of clinics at the schools.
Only a sample of those who were classified as negative for asthma with the case-detection procedure were asked to attend the physician visit. Of the 459 children classified as negative who were requested to attend the visit, 57% did so, giving us 11% of those classified as negative. It is conceivable that children who had symptoms of asthma or other types of respiratory problems were more likely to attend the physician visit. If this was the case, then our estimates are likely to underestimate the sensitivity and specificity of the procedure. In fact, with an examination of the data, it seems likely that some bias in attendance at the physician visit existed. Of the 164 children who were classified as negative for asthma with the questionnaire, 31 (19%) were diagnosed with asthma by the physician. Furthermore, 15 (48%) were classified as having persistent asthma. These children were classified as negative with the questionnaire because they reported no symptoms on the questionnaire. One speculation is that, considering the low literacy rate of this population, some parents might have responded with all negative answers to the questionnaire but reported significant symptoms at the physician visit. Furthermore, in our clinical experience, symptom histories can change drastically with time, depending on the method of questioning (self-report or interview), the interviewer, and external circumstances (such as the stress level or distraction level of the parent). We are currently conducting a detailed examination of the children who were classified as negative with the case-detection procedure but were diagnosed as having asthma at the physician visit.
Finally, it is important to recognize that this study was conducted in an inner-city population that was >90% black. Therefore, the generalizability of results may be limited with respect to other racial and ethnic groups.
One of the strengths of this study was its excellent response rate of 98% for the symptoms questionnaire, with 79% consenting to the study. This high rate was achieved with the use of small incentives for children, classroom teachers, and the school principal. In previous school-based studies, we used incentives only for the children and achieved a response rate of slightly more than 80% for the questionnaire, with 60% consenting to the study.18 These rates were achieved only after multiple distributions of the questionnaires and many discussions with the classroom teachers. That previous experience in the schools taught us that distribution and collection of forms in a classroom setting are time-consuming for teachers. In addition, a primary motivation for teachers is the priority of the task to the school principal. In the current study, we continued to provide children with a small incentive (a pencil and stickers) for return of the questionnaire and consent form. We also added incentives for the classroom teachers and the school principal. The teachers received a small gift certificate to the local mall if they had ≥80% of the consent forms from children in their classroom returned. Consent forms were distributed only to children whose parents returned the symptoms questionnaire. The school principal received a check for $150, made payable to the school, if all teachers in the school achieved at least an 80% response rate for their classrooms. It is important to note that incentives were given on the basis of the number of consent forms returned, not on the basis of the number of children whose parents consented to be in the study. We were ensuring that parents received, read, and responded to the consent forms, rather than coercing individuals to participate in the study. It is important to achieve high response rates in asthma case-detection efforts because children with asthma are more likely to be absent from school. Therefore, procedures that involve testing at school must take into account the need to be present in the school for an extended period of time. To attain the high rates of testing reported in this study, our staff was present for testing at each school for at least a 2-week period.
CONCLUSIONS
Case detection and educational interventions are generally well received by school personnel and can identify children with unrecognized or undiagnosed disease, as well as those with a current diagnosis but poorly controlled disease. This study yields substantial information regarding the validity, yield, and specific types of children who might be identified with the use of such procedures. For the choice of the method of case detection used in a school, the strengths and weaknesses of each procedure, as well as the resources available for case detection, physician referral, and follow-up procedures, must be considered.
ACKNOWLEDGMENTS
This work was supported by National Heart, Lung, and Blood Institute grant 1R01HL65529, Polar Electro Company (donation of heart rate monitors), and GlaxoSmithKline (donation of peak flow meters and Flovent)
We acknowledge the support and cooperation of the Bessemer, Fairfield, Midfield, and Tarrant school systems and the faculty and staff of the 10 elementary schools who participated in this project. In addition, we acknowledge the work of the UAB Lung Health Center Validation Study staff.
ABBREVIATIONS
- UAB
University of Alabama at Birmingham
- BHR
bronchial hyperresponsiveness
- FEV1
forced expiratory volume in 1 second
- FVC
forced vital capacity
- NAEPP
National Asthma Education and Prevention Program
- IAAP
individualized asthma action plan
Footnotes
Dr Feinstein's present address is School of Medicine, Louisiana State University Health Science Center, New Orleans, LA.
REFERENCES
- 1.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma: United States, 1980–1999. MMWR CDC Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- 2.National Center for Health Statistics . National Health Interview Survey, 2001 (data file and documentation) National Center for Health Statistics; Hyattsville, MD: 2001. [Google Scholar]
- 3.Anderson HR, Bland JM, Patel S, Peckham C. The natural history of asthma in childhood. J Epidemiol Community Health. 1986;40:121–129. doi: 10.1136/jech.40.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGill KA, Sorkness CA, Fergson-Page C, Gern JE, Havighurst TC, Knipfer B. Asthma in non-inner city Head Start children. Pediatrics. 1998;102:77–83. doi: 10.1542/peds.102.1.77. [DOI] [PubMed] [Google Scholar]
- 5.Speight ANP, Lee DA, Hey EN. BMJ. 1983;286:1253–1256. doi: 10.1136/bmj.286.6373.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siersted H, Boldsen J, Hansen H, Mostgaard G, Hyldebrandt N. Population based study of risk factors for underdiagnosis of asthma in adolescence: Odense schoolchild study. BMJ. 1998;316:651–655. [PMC free article] [PubMed] [Google Scholar]
- 7.Sole D, Yamada E, Vana AT, Costa-Carvalho B, Naspitz C. Prevalence of asthma and related symptoms in school-age children in Sao Paulo, Brazil: International Study of Asthma and Allergies in Children (ISAAC) J Asthma. 1999;36:205–212. doi: 10.3109/02770909909056318. [DOI] [PubMed] [Google Scholar]
- 8.National Asthma Education and Prevention Program Expert Panel . National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute; Bethesda, MD: 1997. [Google Scholar]
- 9.Boss LP, Wheeler LSM, Williams PV, Bartholomew LK, Taggart VS, Redd SC. Population-based screening or case detection for asthma: are we ready? J Asthma. 2003;40:335–342. doi: 10.1081/jas-120018627. [DOI] [PubMed] [Google Scholar]
- 10.Mannino DM, Homa DM, Akinbami LJ, Moorman J, Gwynn C, Redd S. Surveillance for asthma: United States, 1980–1999. MMWR Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- 11.Newacheck P, Halfon N. Prevalence and impact of disabling chronic conditions in childhood. Am J Public Health. 1998;88:610–617. doi: 10.2105/ajph.88.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Public Health. 2003;82:364–371. doi: 10.2105/ajph.82.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parcel GS, Gilman S, Nader P, Bunce H. A comparison of absentee rates of elementary school children with asthma and nonasthmatic school-mates. Pediatrics. 1979;64:878–881. [PubMed] [Google Scholar]
- 14.Weitzman M, Gortmaker SL, Sobol AM, Perrin JM. Recent trends in the prevalence and severity of childhood asthma. JAMA. 1992;268:2673–2677. [PubMed] [Google Scholar]
- 15.Anderson H, Bailey P, Cooper J, Palmer J, West S. Morbidity and school absence caused by asthma and wheezing illness. Arch Dis Child. 1982;58:777–784. doi: 10.1136/adc.58.10.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freudenberg N, Feldman C, Clark N. The impact of bronchial asthma on school attendance and performance. J School Health. 1980;50:522–526. doi: 10.1111/j.1746-1561.1980.tb02079.x. [DOI] [PubMed] [Google Scholar]
- 17.Pless IB, Pinkerton P. Chronic Childhood Disorder: Promoting Patterns of Adjustment. Yearbook Medical Publishers; Chicago, IL: 1975. [Google Scholar]
- 18.Gerald LB, Redden D, Turner-Henson A, et al. A multi-stage asthma screening procedure for elementary school children. J Asthma. 2002;39:29–36. doi: 10.1081/jas-120000804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark N, Brown R, Joseph C, et al. Issues in identifying asthma and estimating prevalence in an urban school population. J Clin Epidemiol. 2002;55:870–881. doi: 10.1016/s0895-4356(02)00451-1. [DOI] [PubMed] [Google Scholar]
- 20.Glasgow NJ, Ponsonby AL, Yates RE, McDonald T, Attewell R. Asthma screening as part of a routine school health assessment in the Australian Capital Territory. Med J Aust. 2001;174:384–388. doi: 10.5694/j.1326-5377.2001.tb143338.x. [DOI] [PubMed] [Google Scholar]
- 21.Wolf R, Berry C, O'Connor T, Coover L. Validation of the Brief Pediatric Asthma Screen. Chest. 1999;116(suppl 1):224S–228S. doi: 10.1378/chest.116.suppl_2.224s. [DOI] [PubMed] [Google Scholar]
- 22.Hall CB, Wakefield D, Rowe TM, Carlisle PS, Cloutier MM. Diagnosing pediatric asthma: validating the Easy Breathing Survey. J Pediatr. 2001;139:267–272. doi: 10.1067/mpd.2001.116697. [DOI] [PubMed] [Google Scholar]
- 23.Bauer EJ, Lurie N, Yeh C, Grant EN. Screening for asthma in an inner-city elementary school in Minneapolis, Minnesota. J School Health. 1999;69:12–16. doi: 10.1111/j.1746-1561.1999.tb02335.x. [DOI] [PubMed] [Google Scholar]
- 24.Feinstein RA, Hains CS, Hemstreet MP, et al. A simple “step-test” protocol for identifying suspected unrecognized exercise-induced asthma (EIA) in children. Allergy Asthma Proc. 1999;20:181–188. doi: 10.2500/108854199778553019. [DOI] [PubMed] [Google Scholar]
- 25.Feinstein R, LaRussa J, Wang-Dohlman A, Bartolucci A. Screening adolescent athletes for exercise-induced asthma. J Clin Sports Med. 1996;6:119–123. doi: 10.1097/00042752-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Polgar G, Promadhat V. Pulmonary Function Testing in Children: Techniques and Standards. WB Saunders; Philadelphia, PA: 1971. [Google Scholar]
- 27.Pattishall E. Pulmonary function testing reference values and interpretations in pediatric training programs. Pediatrics. 1990;85:768–773. [PubMed] [Google Scholar]
- 28.American Academy of Allergy, Asthma, and Immunology . Pediatric Asthma: Promoting Best Practice: Guide for Managing Asthma in Children. American Academy of Allergy, Asthma, and Immunology; Rochester, NY: 1999. [Google Scholar]
- 29.Britton J, Lewis S. Objective measures and the diagnosis of asthma. BMJ. 1998;317:227–228. doi: 10.1136/bmj.317.7153.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Lung Association . Open Airways for Schools. American Lung Association; New York, NY: 1992. [Google Scholar]
- 31.National Heart, Lung, and Blood Institute . Asthma Awareness: Curriculum for the Elementary Classroom. US Department of Health and Human Services; Washington, DC: 1993. National Institutes of Health publication 93–2894. [Google Scholar]
- 32.National Asthma Education Program . Managing Asthma: A Guide for Schools. National Institutes of Health; Bethesda, MD: 1991. National Institutes of Health publication 91–2650. [Google Scholar]
- 33.Yawn BP, Wollan P, Scanlon PD, Kurland M. Outcome results of a school-based screening program for undertreated asthma. Ann Allergy Asthma Immunol. 2003;90:508–515. doi: 10.1016/S1081-1206(10)61844-3. [DOI] [PubMed] [Google Scholar]
- 34.Webber M, Carpiniello K, Oruwariye T, Lo Y, Burton W, Appel D. Burden of asthma in inner-city elementary school children. Arch Pediatr Adolesc Med. 2003;157:125–129. doi: 10.1001/archpedi.157.2.125. [DOI] [PubMed] [Google Scholar]
- 35.Yawn BP, Wollan P, Scanlon P, Kurkland M. Are we ready for universal school-based asthma screening? Arch Pediatr Adolesc Med. 2002;156:1256–1262. doi: 10.1001/archpedi.156.12.1256. [DOI] [PubMed] [Google Scholar]
- 36.Gruchalla R, Gan V, Roy L, et al. Results of an inner-city school-based asthma and allergy screening pilot study: a combined approach using written questionnaires and step testing. Ann Allergy Asthma Immunol. 2003;90:491–499. doi: 10.1016/S1081-1206(10)61842-X. [DOI] [PubMed] [Google Scholar]
- 37.Johansson H, Foucard T, Petterson LG. Exercise tests in large groups of children are not a suitable screening procedure for undiagnosed asthma. Allergy. 1997;52:1128–1132. doi: 10.1111/j.1398-9995.1997.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 38.Abramson J, Wollan P, Kurland M, Yawn B. Feasibility of school-based spirometry screening for asthma. J School Health. 2003;73:150–153. doi: 10.1111/j.1746-1561.2003.tb03594.x. [DOI] [PubMed] [Google Scholar]
- 39.Bailey WC. Treatment of atypical mycobacterial disease. Chest. 1983;84:625–628. doi: 10.1378/chest.84.5.625. [DOI] [PubMed] [Google Scholar]
- 40.Pierce N, Beasley R, Burges C, Crane J. Asthma Epidemiology: Principles and Methods. Oxford University Press; New York, NY: 1998. pp. 75–114. [Google Scholar]