Abstract
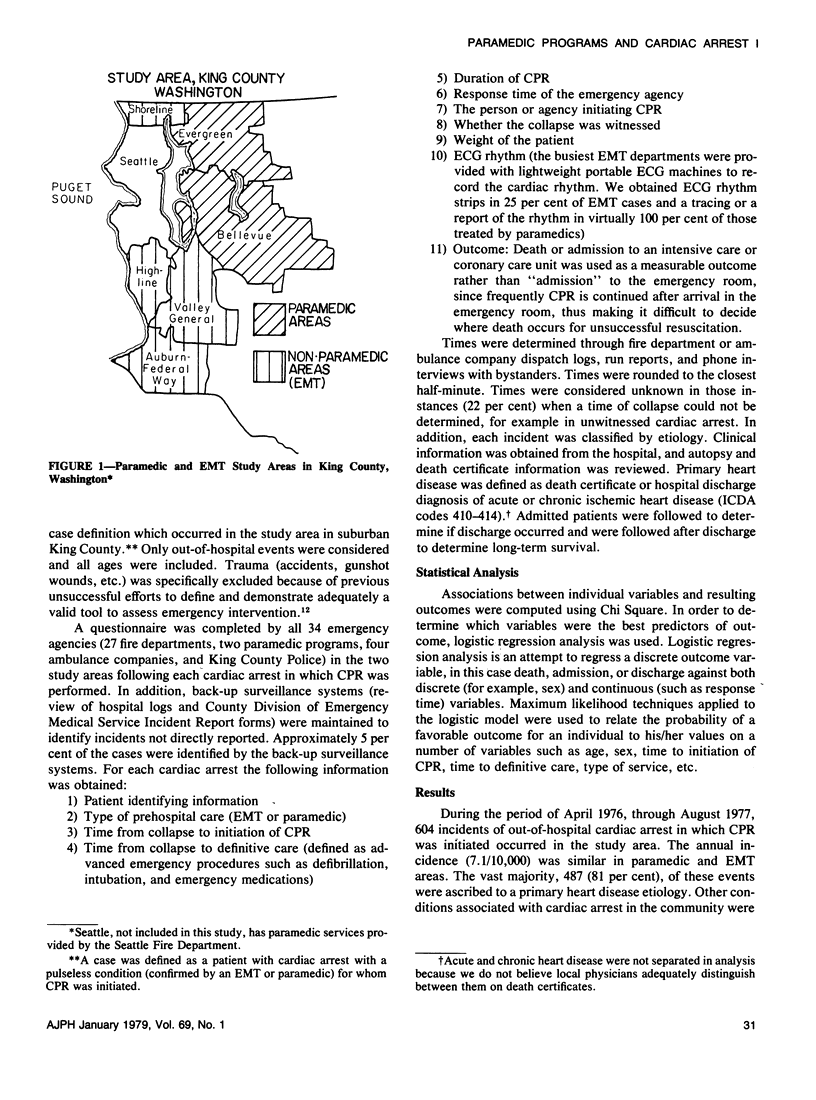
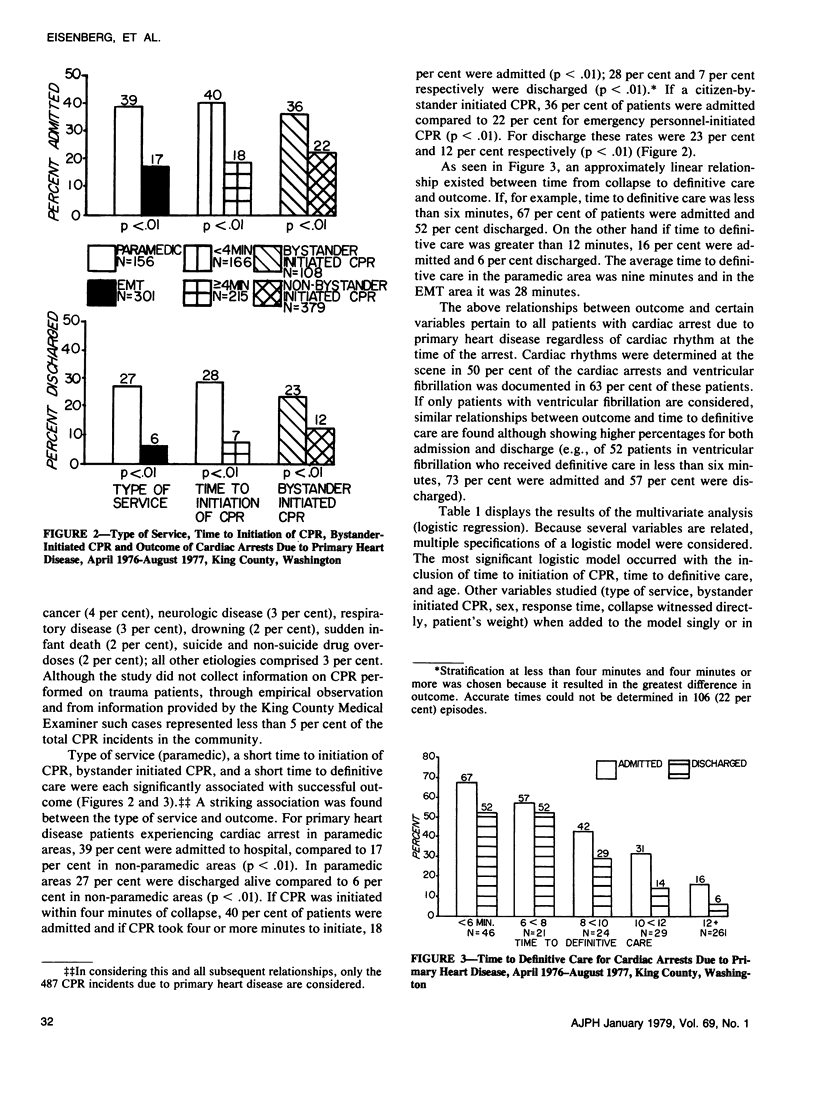
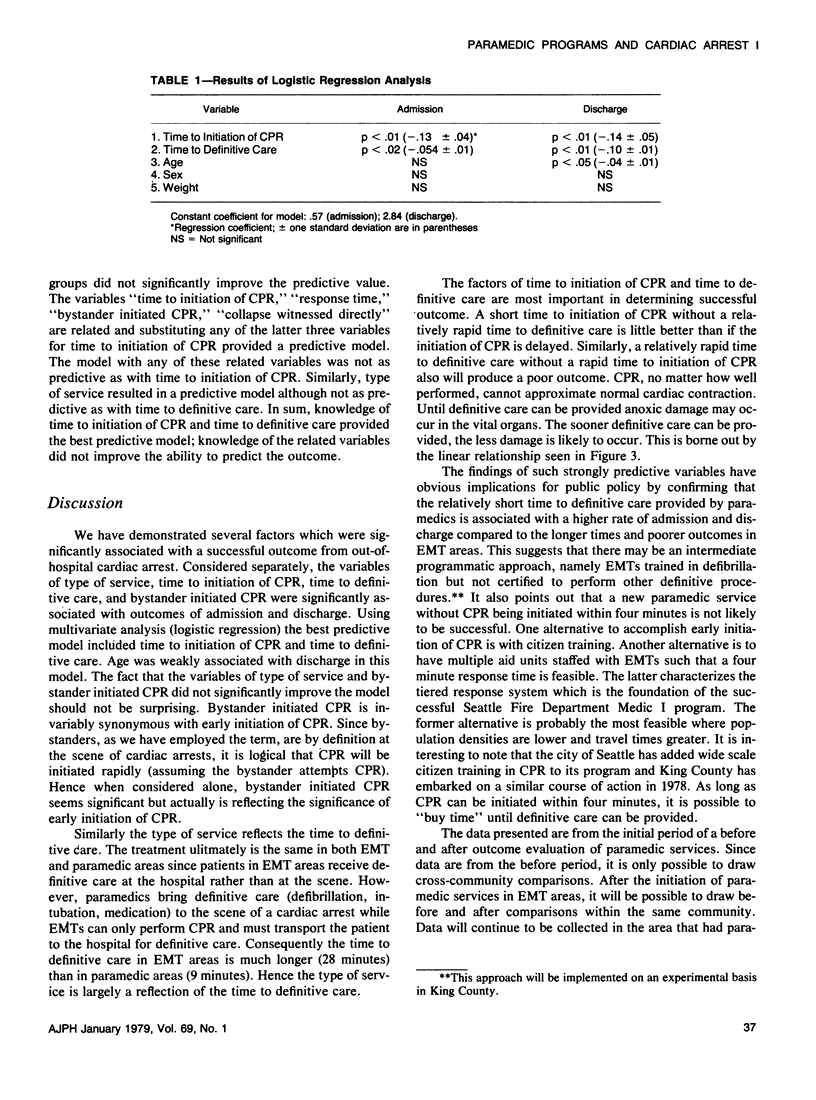
As part of an evaluation of whether the addition of paramedic services can reduce mortality from out-of-hospital cardiac arrest compared to previously existing emergency medical technician (EMT) services, factors associated with successful resuscitation were studied. A surveillance system was established to identify cardiac arrest patients receiving emergency care and to collect pertinent information associated with the resuscitation. Outcomes (death, admission, and discharge) were compared in two areas with different types of prehospital emergency care (basic emergency medical technician services vs. paramedic services). During the period April 1976 through August 1977, 604 patients with out-of-hospital cardiac arrest received emergency resuscitation. Eighty-one per cent of these episodes were attributed to primary heart disease. Considered separately, four factors were found to have a significant association with higher admission and discharge rates :1) paramedic service, 2) rapid time to initiation of cardiopulmonary resuscitation (CPR), 3) rapid time to definitive care, and 4) bystander-initiated CPR. Using multivariate analysis, rapid time to initiation of CPA and rapid time to definitive care were most predictive of admission and discharge. Age was also weakly predictive of discharge. These findings suggest that if reduction in mortality is to be maximized, cardiac arrest patients must have CPR initiated within four minutes and definitive care provided within ten minutes.
Full text
PDF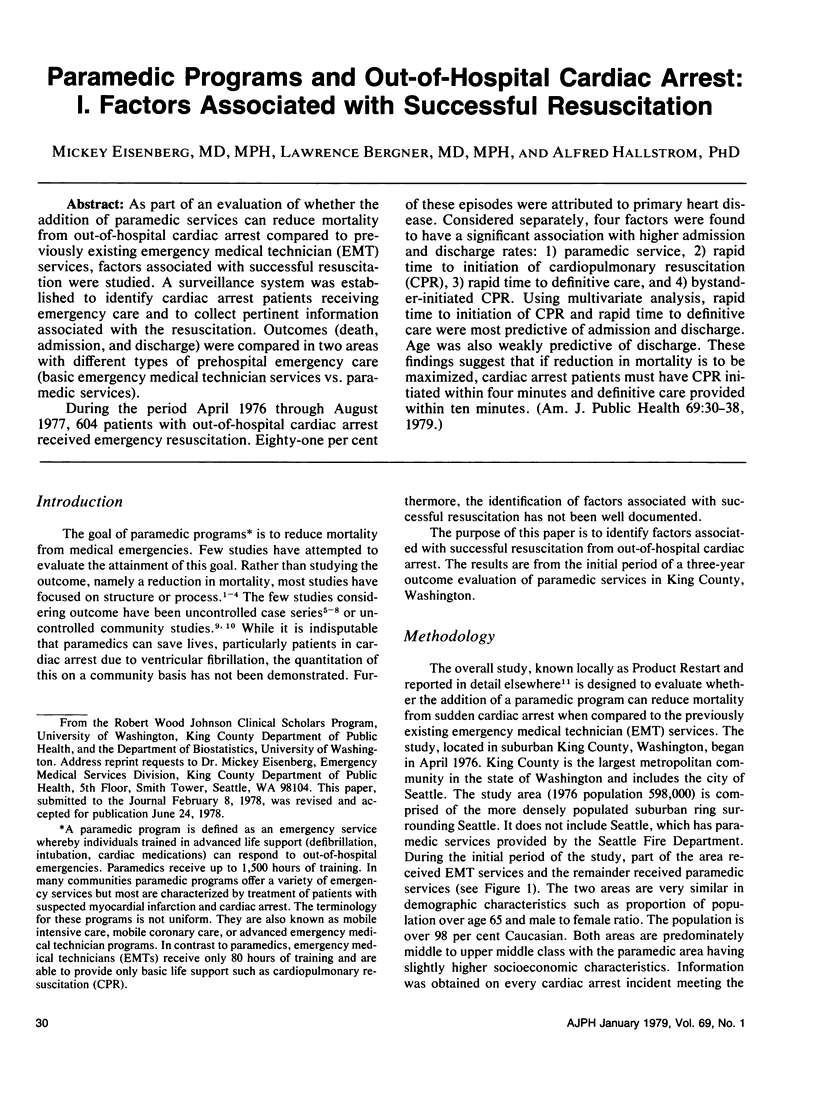
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baum R. S., Alvarez H., 3rd, Cobb L. A. Survival after resuscitation from out-of-hospital ventricular fibrillation. Circulation. 1974 Dec;50(6):1231–1235. doi: 10.1161/01.cir.50.6.1231. [DOI] [PubMed] [Google Scholar]
- Carveth S. W. Eight-year experience with a stadium- based mobile coronary-care unit. Heart Lung. 1974 Sep-Oct;3(5):770–774. [PubMed] [Google Scholar]
- Crampton R. S., Michaelson S. P., Wynbeek A., Miles J. R., Jr, Gascho J. A., Stillerman R., Aldrich R. F. Reduction of pre-hospital, ambulance, and hospital coronary death by the pre-hospital emergency cardiac care system: a rationale for training emergency medical technicians, nurses, and physicians. Heart Lung. 1974 Sep-Oct;3(5):742–747. [PubMed] [Google Scholar]
- Graf W. S., Polin S. S., Paegel B. L. A community program for emergency cardiac care. A three-year coronary ambulance-paramedic evaluation. JAMA. 1973 Oct 8;226(2):156–160. [PubMed] [Google Scholar]
- Liberthson R. R., Nagel E. L., Hirschman J. C., Nussenfeld S. R. Prehospital ventricular defibrillation. Prognosis and follow-up course. N Engl J Med. 1974 Aug 15;291(7):317–321. doi: 10.1056/NEJM197408152910701. [DOI] [PubMed] [Google Scholar]
- Pace N. A. Emergancy cardiac care in a metropolitan office building. Heart Lung. 1974 Sep-Oct;3(5):775–778. [PubMed] [Google Scholar]
- Waller J. A. Urban-oriented methods. Failure to solve rural emergency care problems. JAMA. 1973 Dec 17;226(12):1441–1446. doi: 10.1001/jama.226.12.1441. [DOI] [PubMed] [Google Scholar]


