Abstract
Hysterectomy is the most common major surgical procedure performed in the United States. The frequency of hysterectomy among women in the general population is of interest because it affects the population at risk for uterine diseases and because the procedure itself carries significant personal and socioeconomic consequences. We studied factors related to the occurrence of hysterectomy by interviewing a representative sample of women ages 35-74 (n= 1087) in two urban Washington counties during 1976-1977.
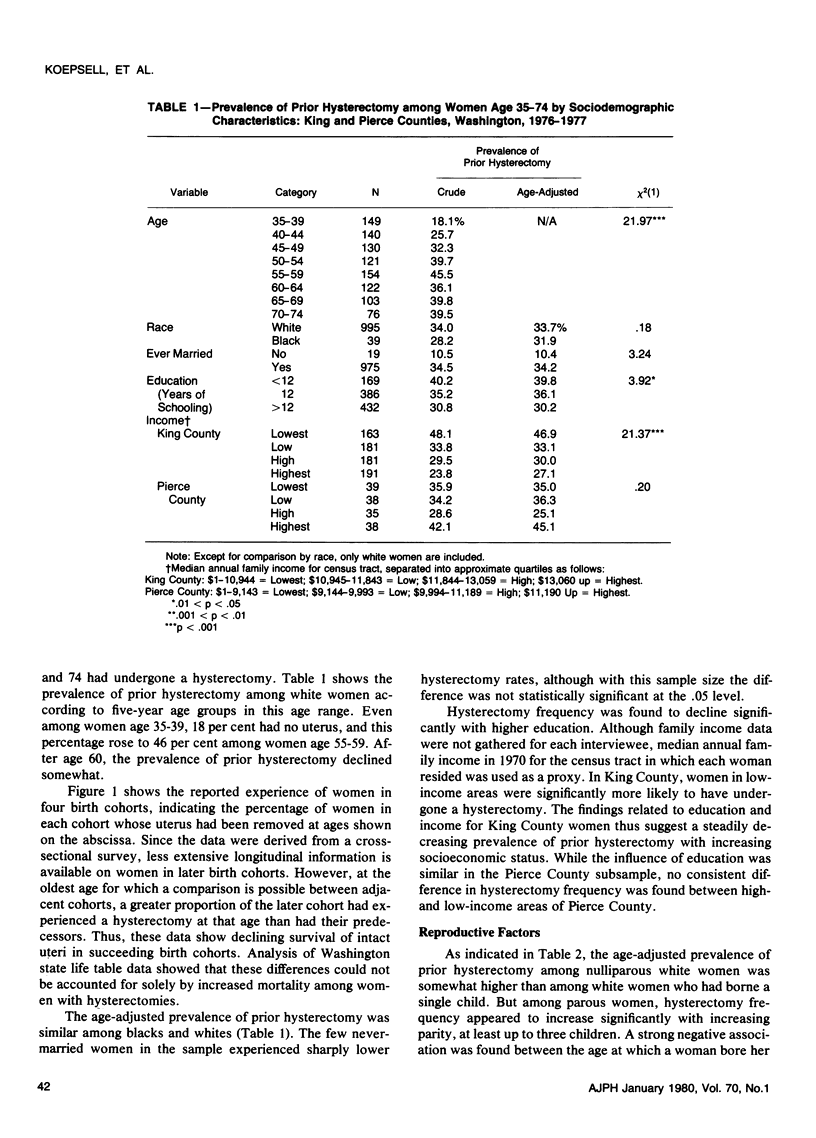
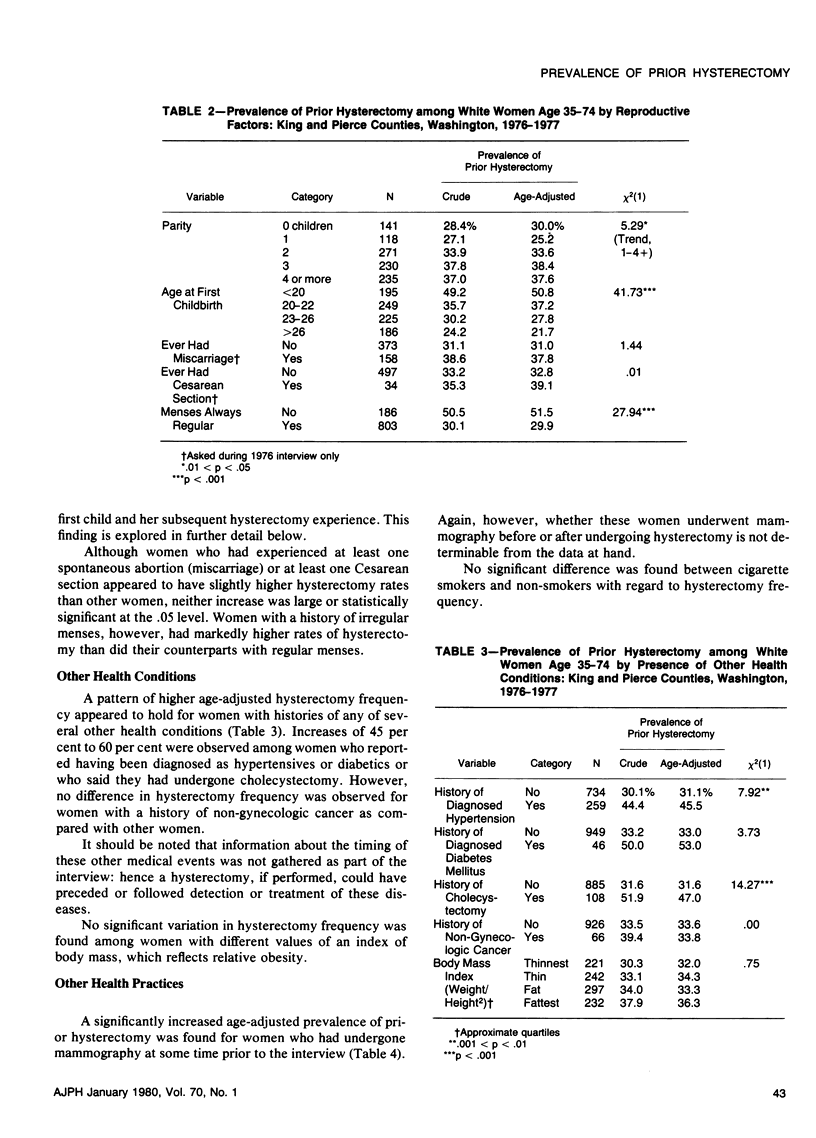
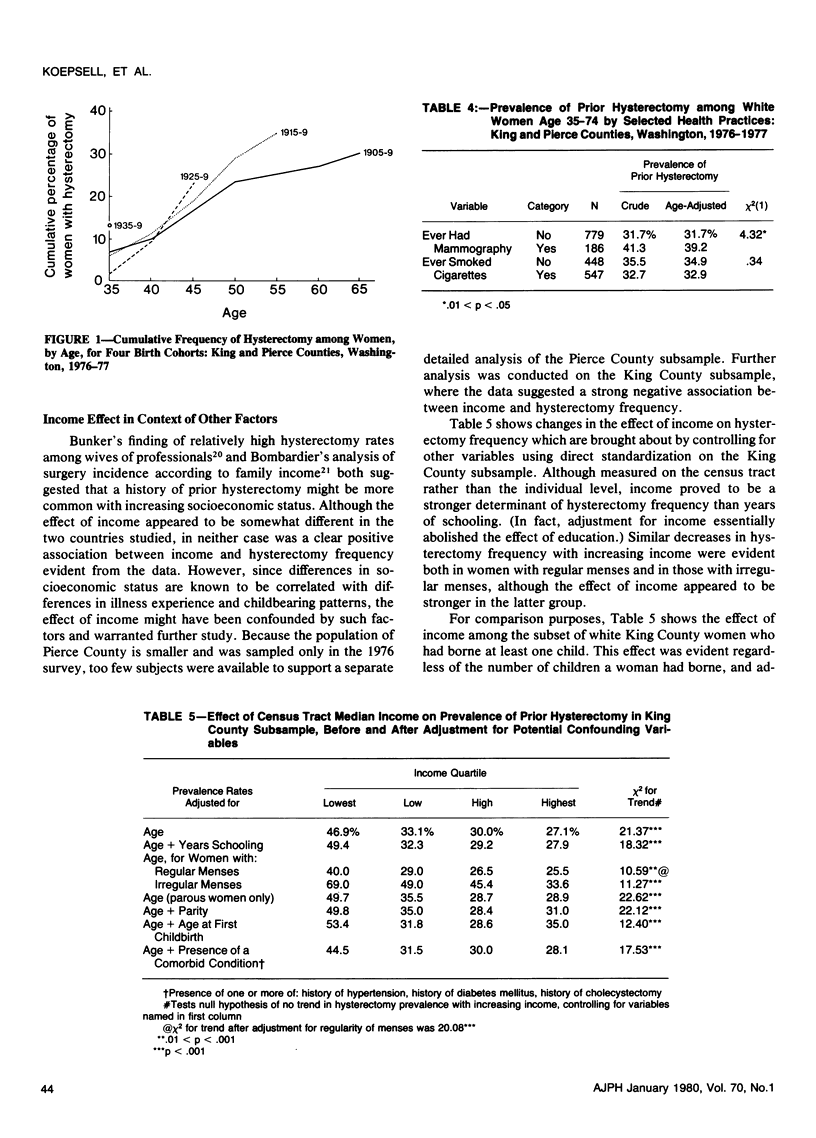
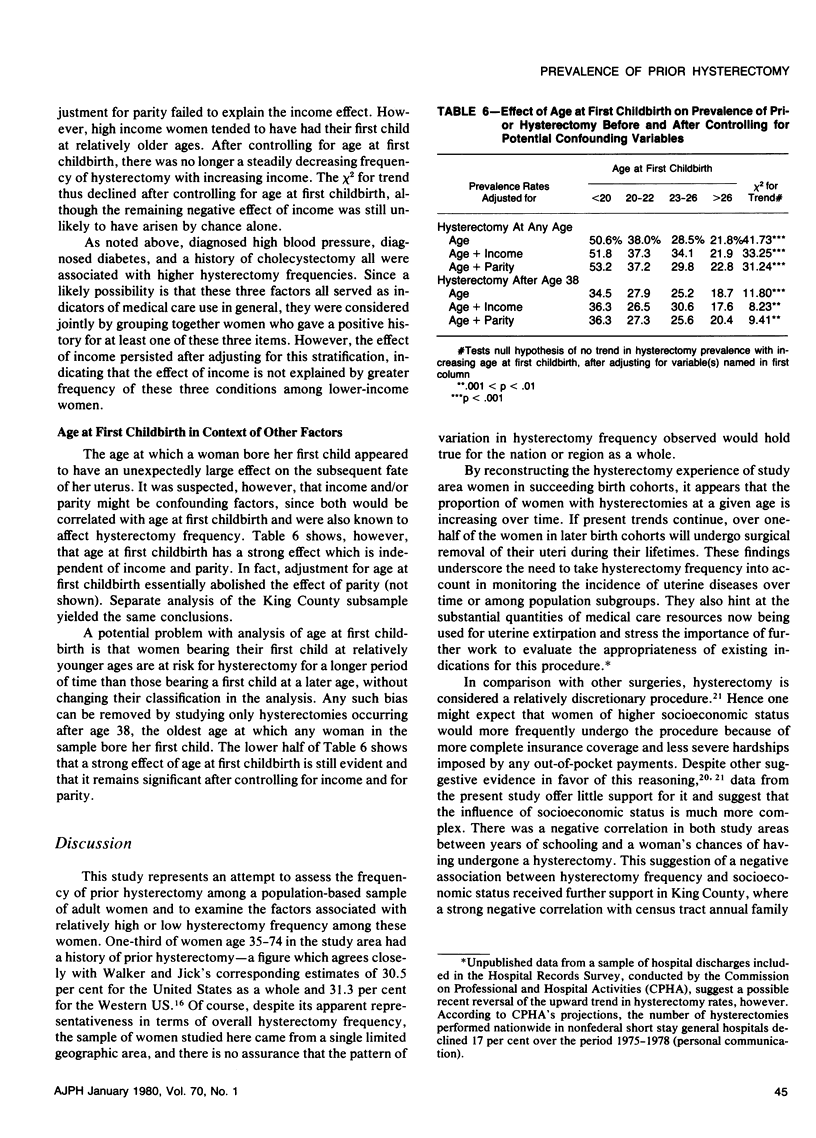
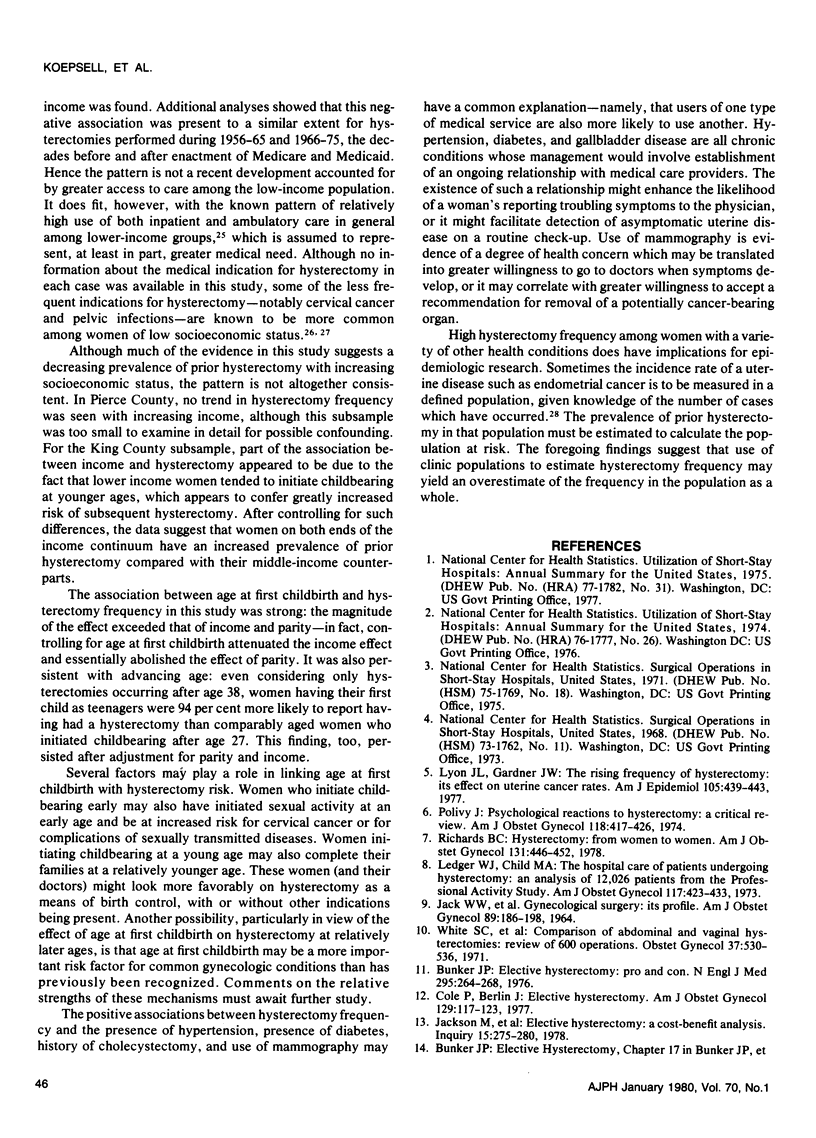
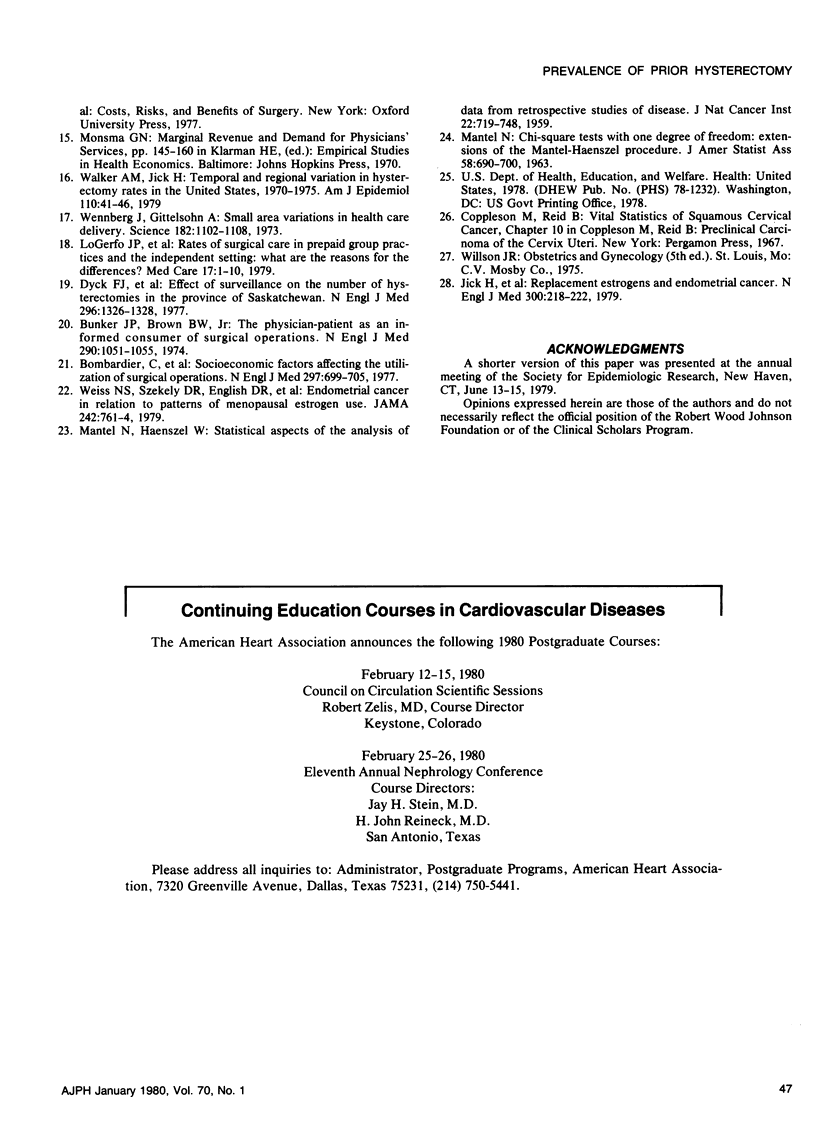
One-third of the women studied had had a hysterectomy. Later birth cohorts were at higher risk. The ageadjusted prevalence of prior hysterectomy was negatively associated with education and age at first childbirth; it was positively associated with parity, history of irregular menses, and history of a variety of other health conditions. Contrary to expectation, income was negatively associated with hysterectomy rates in one county and showed no association in the other. Part of the income effect was due to confounding by age at first childbirth, which was a surprisingly strong predictive factor.
We conclude that: 1) despite economic predictions based on the discretionary nature of the procedure, hysterectomies are not necessarily more common among high-income women; 2) age at first childbirth may be a more important risk factor for uterine disease than previously thought; and 3) estimates of hysterectomy frequency based on clinic populations may be misleading. (Am J Public Health 70:40-47, 1980.)
Full text
PDF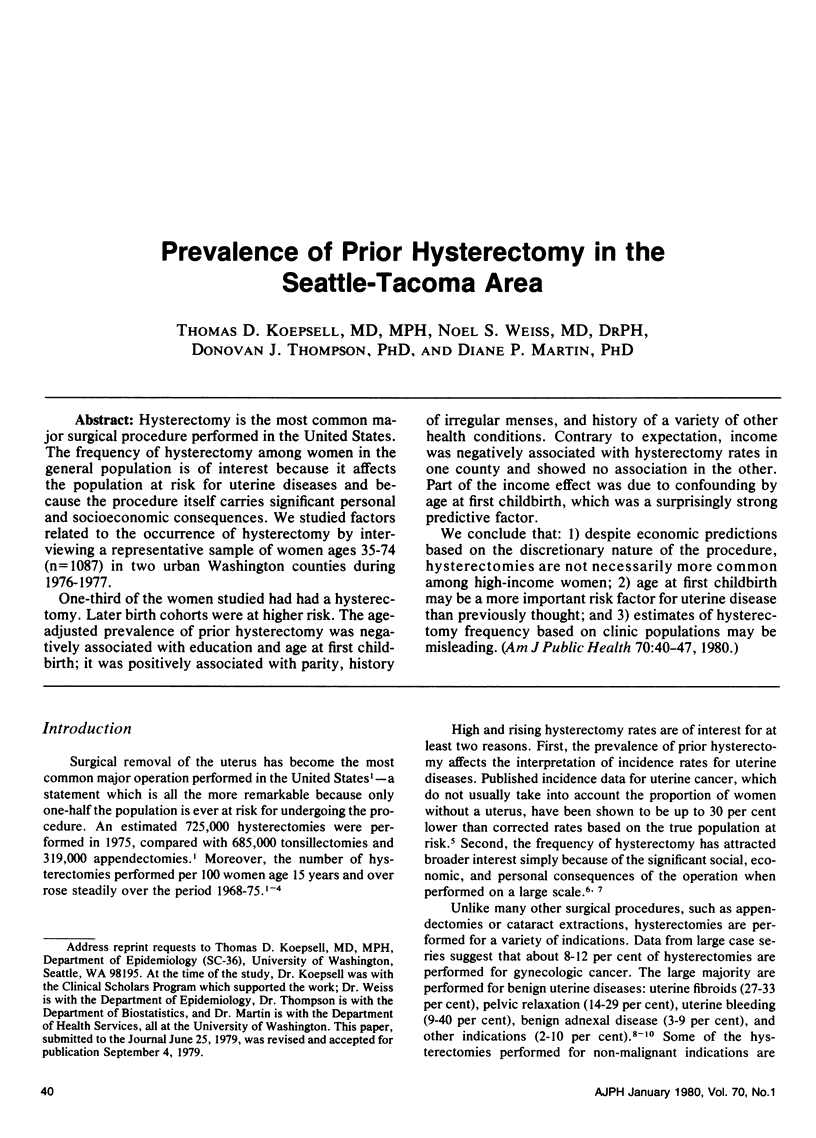
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bombardier C., Fuchs V. R., Lillard L. A., Warner K. E. Socioeconomic factors affecting the utilization of surgical operations. N Engl J Med. 1977 Sep 29;297(13):699–705. doi: 10.1056/NEJM197709292971305. [DOI] [PubMed] [Google Scholar]
- Bunker J. P., Brown B. W., Jr The physician-patient as an informed consumer of surgical services. N Engl J Med. 1974 May 9;290(19):1051–1055. doi: 10.1056/NEJM197405092901905. [DOI] [PubMed] [Google Scholar]
- Bunker J. P. Public-health rounds at the Harvard School of Public Health. Elective hysterectomy: pro and con. N Engl J Med. 1976 Jul 29;295(5):264–268. doi: 10.1056/NEJM197607292950509. [DOI] [PubMed] [Google Scholar]
- Cole P., Berlin J. Elective hysterectomy. Am J Obstet Gynecol. 1977 Sep 15;129(2):117–123. doi: 10.1016/0002-9378(77)90730-x. [DOI] [PubMed] [Google Scholar]
- Dyck F. J., Murphy F. A., Murphy J. K., Road D. A., Boyd M. S., Osborne E., De Vlieger D., Korchinski B., Ripley C., Bromley A. T. Effect of surveillance on the number of hysterectomies in the province of Saskatchewan. N Engl J Med. 1977 Jun 9;296(23):1326–1328. doi: 10.1056/NEJM197706092962306. [DOI] [PubMed] [Google Scholar]
- JACK W. W., SLEE V. N., HEADLY P. D. GYNECOLOGICAL SURGERY: ITS PROFILE. Am J Obstet Gynecol. 1964 May 15;89:186–198. doi: 10.1016/0002-9378(64)90710-0. [DOI] [PubMed] [Google Scholar]
- Jackson M. N., LoGerfo J. P., Diehr P., Watts C. A., Richardson W. Elective hysterectomy: a cost-benefit analysis. Inquiry. 1978 Sep;15(3):275–280. [PubMed] [Google Scholar]
- Jick H., Watkins R. N., Hunter J. R., Dinan B. J., Madsen S., Rothman K. J., Walker A. M. Replacement estrogens and endometrial cancer. N Engl J Med. 1979 Feb 1;300(5):218–222. doi: 10.1056/NEJM197902013000502. [DOI] [PubMed] [Google Scholar]
- Ledger W. J., Child M. A. The hospital care of patients undergoing hysterectomy: an analysis of 12,026 patients from the Professional Activity Study. Am J Obstet Gynecol. 1973 Oct 1;117(3):423–433. doi: 10.1016/0002-9378(73)90051-3. [DOI] [PubMed] [Google Scholar]
- LoGerfo J. P., Efird R. A., Diehr P. K., Richardson W. C. Rates of surgical care in prepaid group practices and the independent setting: what are the reasons for the differences? Med Care. 1979 Jan;17(1):1–10. doi: 10.1097/00005650-197901000-00001. [DOI] [PubMed] [Google Scholar]
- Lyon J. L., Gardner J. W. The rising frequency of hysterectomy: its effect on uterine cancer rates. Am J Epidemiol. 1977 May;105(5):439–443. doi: 10.1093/oxfordjournals.aje.a112402. [DOI] [PubMed] [Google Scholar]
- MANTEL N., HAENSZEL W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959 Apr;22(4):719–748. [PubMed] [Google Scholar]
- Polivy J. Psychological reactions to hysterectomy: a critical review. Am J Obstet Gynecol. 1974 Feb 1;118(3):417–426. doi: 10.1016/s0002-9378(16)33802-9. [DOI] [PubMed] [Google Scholar]
- Richards B. C. Hysterectomy: from women to women. Am J Obstet Gynecol. 1978 Jun 15;131(4):446–452. doi: 10.1016/0002-9378(78)90421-0. [DOI] [PubMed] [Google Scholar]
- Walker A. M., Jick H. Temporal and regional variation in hysterectomy rates in the United States, 1970--1975. Am J Epidemiol. 1979 Jul;110(1):41–46. doi: 10.1093/oxfordjournals.aje.a112785. [DOI] [PubMed] [Google Scholar]
- Wennberg J., Gittelsohn Small area variations in health care delivery. Science. 1973 Dec 14;182(4117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- White S. C., Wartel J., Wade M. E. Comparison of abdominal and vaginal hysterectomies. A review of 600 operations. Obstet Gynecol. 1971 Apr;37(4):530–537. [PubMed] [Google Scholar]


