Abstract
Both cytotoxic and invasive strains of Pseudomonas aeruginosa can damage corneal epithelial cells in vitro, but neither can infect healthy corneas in vivo. We tested the hypothesis that whole human tear fluid can protect corneal epithelia against P. aeruginosa virulence mechanisms. Cultured corneal epithelial cells were inoculated with 106 CFU of one of 10 strains of P. aeruginosa (five cytotoxic, five invasive)/ml with or without reflex tear fluid collected from the conjunctival sacs of human volunteers. Cytotoxicity was assessed by observation of trypan blue staining and measurement of lactate dehydrogenase release; invasion was quantified by using gentamicin survival assays. Tear fluid retarded growth of only 50% of the P. aeruginosa strains (three of five invasive strains, two of five cytotoxic strains) yet protected corneal cells against invasion by or cytotoxicity of 9 of 10 strains. The only strain resistant to the tear cytoprotective effects was susceptible to tear bacteriostatic activity. Dilution of tear fluid threefold significantly reduced cytoprotection, while bacteriostatic activity prevailed with dilutions beyond 100-fold. Sulfacetamide (1 mg/ml) with bacteriostatic activity matching that of tear fluid was less cytoprotective than tear fluid (80% protection with tear fluid, 48% with sulfacetamide). Video microscopy revealed bacterial chain formation in both tear fluid and sulfacetamide, but tear fluid also blocked bacterial swimming motility. After prolonged tear contact, bacteria regained normal growth rates, swimming motility, and cytotoxic activity, suggesting a breakdown of protective tear factors. Boiled tear fluid lost bacteriostatic activity and effects on bacterial motility but retained cytoprotective function. These results suggest that human tear fluid can protect corneal epithelial cells against P. aeruginosa virulence mechanisms in a manner not dependent upon bacteriostatic activity or effects on bacterial motility. Whether overlapping tear film components are involved in these defense functions is to be determined.
Pseudomonas aeruginosa is a gram-negative opportunistic bacterium capable of causing severe corneal infection. There are at least two types of P. aeruginosa isolated from infected corneas; those that invade corneal epithelial cells (5) and those that cause ExoU-dependent cytotoxicity from an extracellular location (3, 4, 8, 9). Both invasive and cytotoxic strains can target surface cells on intact corneas in vitro (7, 10), yet neither can infect healthy corneas in vivo, suggesting that protective factors are absent in in vitro assays. The most obvious of these are tear fluid and the mechanical effects of blinking. Shear stresses generated by blinking motions of the eyelids reduce, but do not eliminate, P. aeruginosa cytotoxicity (C. Lakkis, M. N. Mendoza, D. Fan, A. Chauhan, S. P. Srinivas, and S. M. J. Fleiszig, Assoc. Res. Vision Ophthalmol. Annu. Meet., 30 Apr to 4 May 2001, abstr. Investig. Ophthalmol. Vis. Sci. 42(Suppl.):S593, 2001).
The presence of antimicrobial factors in the human tear film was first reported in 1922 by Fleming and Allison, who described the bactericidal effects of lysozyme on gram-positive bacteria (12). Biochemical studies have since shown that various other factors in tears, including the iron-binding protein lactoferrin, secretory phospholipase A2, immunoglobulin A (IgA) antibodies, mucins, and β-defensins, also possess antibacterial properties. A recent study demonstrated that whole human tears have strong bactericidal activity against a wide variety of gram-positive bacteria, with secretory phospholipase A2 being the major effector (20). Gram-negative bacteria, such as P. aeruginosa, were resistant to secretory phospholipase A2 at salt concentrations found in tears (20). Defensins have bactericidal activity against a wide variety of organisms, including gram-negative bacteria, and have been found in small but detectable quantities in tears (13). Other tear components can alter behavior of P. aeruginosa; e.g., both IgA and ocular mucin(s) bind these bacteria and modify their adherence to the cornea in animal models (6, 15), while lactoferrin induces twitching motility, thereby reducing the ability of the bacteria to form surface biofilms (23).
In this study, we tested the hypothesis that whole human tear fluid protects corneal epithelial cells against P. aeruginosa invasive and cytotoxic virulence mechanisms.
MATERIALS AND METHODS
Bacterial strains and preparation of inocula.
Ten P. aeruginosa isolates were used. Five of these isolates were classified as cytotoxic because they possess the exoU gene and can induce acute cytotoxic effects on corneal epithelial cells (8, 9). Cytotoxic strains 6206, 6077, and 6073 (all serogroup O11) are corneal isolates, while strains PA103 (serogroup O11) and 19660 (serogroup O2) are laboratory strains. The other five strains were classified as invasive: they lack the exoU gene and invade corneal epithelial cells (8, 9). The invasive strains 6294 and 6487 (serogroup O6) are corneal isolates, PAK (serogroup O1) is a bacteremic isolate, and PAO1 (serogroup O2) and PA1244 (serogroup O7) are laboratory strains. All but one of the 10 strains (strain PA103) demonstrated flagellum-mediated motility.
Bacterial inocula were prepared from overnight cultures grown on Trypticase soy agar plates at 37°C before suspension in minimal essential Eagle medium with Hank's salts and l-glutamine (Sigma, St Louis, Mo.) buffered with 1 M HEPES-NaOH (pH 7.6), 0.35 g of NaHCO3, and 6 g of bovine serum albumin (Sigma) per liter (MEM). The bacteria were initially prepared to a concentration of 108 CFU/ml of MEM as determined by spectrophotometry (optical density of 0.1 at 650 nm). The bacterial suspension was then diluted to a concentration of 106 CFU/ml in either MEM or whole tear fluid for use in experiments. Bacterial numbers were confirmed by viable counts after serial dilution.
Tear collection.
Tear film was collected from the lower conjunctival sacs of human subjects by the use of capillary tubes as previously described (19) and as approved by the Committee for Protection of Human Subjects, University of California, Berkeley. A tear volume of 100 μl was collected over approximately 15 min on each occasion. Collected tears were pooled, aliquoted, and frozen (−20°C) until used in experiments. The same batch of pooled tears was used in all experiments.
Cell cultures.
Rabbit corneal epithelial cells were cultured in 96-well tissue culture plates (Becton Dickinson, Franklin Lakes, N.J.) in the presence of SHEM medium as previously described (9). Cells were fed on alternate days and were used for experiments 4 to 6 days after being passaged. Prior to each experiment, wells containing cultured cells were washed once with 100 μl of phosphate-buffered saline (PBS) to remove residual SHEM and antibiotics.
Bacterial growth assays.
The effect of tear fluid on bacterial growth and viability was tested with and without the presence of corneal epithelial cells. This testing was done by adding 40 μl of bacterial suspension, in either MEM or tear fluid, to empty wells of tissue culture dishes or to wells containing corneal epithelial cell cultures. Following a 3-h incubation at 37°C, 5 μl of bacterial suspension was collected for quantification by viable cell counting after serial dilution. The number of bacteria present in each well at the end of the experiment was compared to that in the starting inoculum to study bacterial growth and killing.
Cytotoxicity assays.
Bacterium-induced cell damage was quantified by measuring lactate dehydrogenase (LDH) release from dead or damaged cells. Wells containing cultured cells were inoculated with 40 μl of MEM or tear fluid containing 106 CFU of cytotoxic P. aeruginosa/ml. After a 3-h incubation at 37°C, the supernatant from each well was collected and diluted 1:20 with fresh MEM. The quantity of LDH in the samples was detected by using a cytotoxicity detection kit (Roche Diagnostics, Indianapolis, Ind.) according to the manufacturer's instructions and expressed as absorbance at 490 nm. An additional two sets of wells were treated with MEM without bacteria. One set of cells was used to determine background LDH release, while cells in the other group were lysed with MEM containing Triton X-100 (0.25% [vol/vol]; LabChem Inc., Pittsburgh, Pa.) at the end of assay to determine the amount of LDH released when 100% of the cells were killed.
Trypan blue exclusion assays were also used to qualitatively assess the pattern of corneal cell death. Bacterial suspensions were removed after the 3-h incubation (see above), and cells were washed once with PBS (50 μl) prior to treatment with MEM (100 μl) containing gentamicin (200 μg/ml; BioWhittaker, Walkersville, Md.) for 1 h at 37°C to kill extracellular bacteria. This was done to match the methods used for invasion assays described below and to prevent the progression of cytotoxicity beyond the 3-h incubation period. Cells were washed with 100 μl of PBS before the addition of 100 μl of trypan blue solution (0.04% [wt/vol]) for 15 min to stain dead or dying cells. The trypan blue solution was then replaced with 50 μl of Ham's F-12 medium (BioWhittaker), and the center of each well was photographed by using an Olympus IX-70 inverted light microscope (10× objective, 10× ocular) attached to a video camera (Optronics, Goleta, Calif.) and a computer-based imaging system (Inovision, Raleigh, N.C.).
Invasion assays.
Bacterial invasion of corneal epithelial cells was quantified by using gentamicin survival assays as previously described (9). Briefly, cells were incubated with an invasive P. aeruginosa strain (3 h, 37°C) prior to treatment with gentamicin to kill extracellular bacteria as described above for cytotoxicity assays. After being washed to remove the antibiotic, cells were lysed by exposure to PBS containing Triton X-100 (0.25% [vol/vol]) for 15 min. Viable counts were then performed on the lysate to quantify the previously intracellular bacteria.
Microscopy.
Cells were grown on tissue culture-treated coverslips and mounted within a chamber which fit onto the stage of an Olympus IX-70 inverted light microscope. The temperature in the chamber was maintained at 37°C throughout the experiment by pumping heated water around a hollow region surrounding the metal chamber that was custom made for this purpose. Bacteria were added to the coverslips with or without tear fluid. A video camera (Optronics) and imaging system (Inovision) were used to capture video and still images of bacterial morphology, bacterial movement, and the interactions of bacteria with cells. In control experiments, bacteria were added to coverslips without corneal epithelial cells.
Statistics.
At least four wells were used for each group of samples in all experiments, which were repeated at least twice. The Student t test and analysis of variance (ANOVA) were used to analyze the data. P values of <0.05 were considered significant.
RESULTS
Human tear fluid protects corneal cells against cytotoxic P. aeruginosa strain 6206.
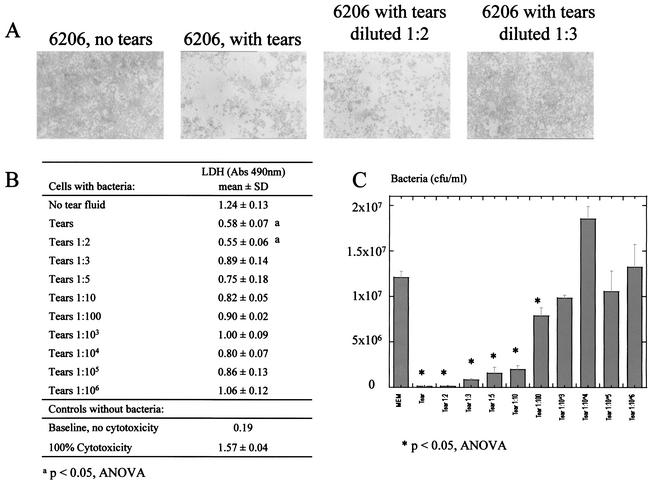
Strain 6206 was used for initial characterization of the effect of tear fluid on P. aeruginosa, since it has the strongest cytotoxic activity of all the test strains (8). As expected, 106 CFU/ml of MEM induced significant cell death after 3 h (Fig. 1A, left panel). In contrast, cells that were incubated with bacteria in whole human tear fluid instead of MEM were protected from cell damage (Fig. 1A, right panel). Quantitation by LDH release assays (Fig. 1B) confirmed the visible results obtained with trypan blue staining. In the presence of tear fluid, there was a significant reduction in 6206-induced LDH release (cytotoxicity) (P < 0.05; t test) such that LDH release was reduced to levels similar to those obtained in control samples not inoculated with bacteria. Treatment of cells with tear fluid alone did not significantly affect LDH release from cells (Fig. 1B).
FIG. 1.
Effect of human tear fluid on cytotoxicity of P. aeruginosa strain 6206 towards corneal epithelial cells. Bacterium-induced cytotoxicity was greatly reduced by the presence of human tear fluid as indicated by the significantly reduced trypan blue staining (A) and LDH release (B) in the presence of tears. Abs, absorbance; SD, standard deviation.
Retardation of bacterial growth by tear fluid.
Since human tear fluid was cytoprotective against strain 6206, its effect on bacterial viability was explored. This was done by comparing bacterial growth in tear fluid to growth in MEM in the presence of corneal epithelial cells at 37°C for 3 h. Bacteria were found to grow in tear fluid but at a significantly reduced rate compared to the growth rate in MEM. In a typical experiment, bacteria grew from a concentration of ∼1.7 × 106 CFU/ml to ∼2.5 × 106 CFU/ml in tears compared to ∼1 × 107 CFU/ml in MEM. The presence of corneal epithelial cells was not required for retardation of bacterial growth, since similar results were obtained when bacteria were inoculated into wells without cells (data not shown). This result suggested that cytoprotection might involve bacteriostatic activity.
Tear fluid effects on other cytotoxic strains of P. aeruginosa.
The effect of human tear fluid on four other cytotoxic strains was examined and compared to the effect on cytotoxic strain 6206. The results showed that tear fluid was bacteriostatic against only two of the five cytotoxic strains tested (6206 and PA103) (Fig. 2A). Surprisingly, three strains (6073, 19660, and 6077) grew at least as quickly in tear fluid as in MEM, yet the tear fluid was still cytoprotective (Fig. 2B). One of these (strain 19660) grew even faster in tear fluid than in MEM (P < 0.05; t test). The exact opposite result was obtained with strain PA103, the strain most susceptible to tear bacteriostatic activity (Fig. 2A), which demonstrated enhanced cytotoxic activity in tear fluid (Fig. 2B). This pattern of results suggested that cytoprotective activity of tear fluid might not depend upon bacteriostatic activity.
FIG. 2.
Tear fluid effects on growth and cytotoxic activity of five cytotoxic strains of P. aeruginosa. (A) After 3 h, tear fluid (gray bars) inhibited the growth of two strains (6206 and PA103), while strain 19660 grew faster in tears. (B) LDH release assays indicated significantly reduced bacterial cytotoxicity in the presence of tears for four of five P. aeruginosa strains. Abs, absorbance; SD, standard deviation.
Tear fluid cytoprotection versus bacteriostatic activity.
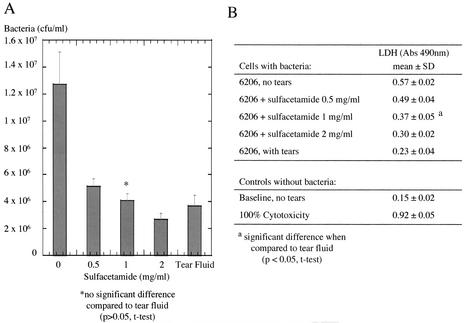
Strain 6206 was used to explore the relationship between bacteriostatic activity and cytoprotection, since it was the only cytotoxic strain susceptible to both tear fluid effects. Both trypan blue staining (Fig. 3A) and LDH release assays (Fig. 3B) showed that cytoprotective activity was rapidly lost by dilution of tear fluid with MEM and was no longer significant at a dilution of 1:3 (P > 0.05; ANOVA). In contrast, significant bacteriostatic activity prevailed at dilutions of up to 1:100 (P < 0.05; ANOVA) (Fig. 3C). In other experiments, a bacteriostatic agent was used to determine whether cytoprotection could be separated from bacteriostasis. The antimicrobial sulfacetamide was used to match the bacteriostatic effects of tears, and then the cytoprotective effects of tear fluid and sulfacetamide were compared. The bacteriostatic activity of sulfacetamide was found to be similar to that of tear fluid at a concentration of 1 mg/ml (Fig. 4A). Yet tear fluid was significantly more cytoprotective than 1 mg of sulfacetamide/ml (Fig. 4B). Although sulfacetamide could have other effects on the bacteria or epithelial cells that alter their interactions with each other, the results suggest that factors other than bacteriostatic activity contribute to cytoprotection by human tear fluid.
FIG. 3.
Effect of tear fluid dilution on cytotoxicity and viability of P. aeruginosa strain 6206. Tears were diluted with MEM, and cytotoxicity towards corneal epithelial cells was assessed by staining with trypan blue (A) and measuring LDH release (B). Significant cytoprotection by tears was lost at a dilution of 1:3. (C) Viable cell counts after 3 h of incubation in tears or MEM showed that tear fluid was significantly bacteriostatic to strain 6206 at a 1:100 dilution. Abs, absorbance; SD, standard deviation.
FIG. 4.
Comparison of the bacteriostatic agent sulfacetamide with tear fluid with respect to growth inhibition and cytoprotective activity. (A) Three hours of treatment with sulfacetamide (1 mg/ml) produced a growth inhibition of strain 6206 equivalent to that produced by tear fluid. (B) The cytoprotective activity of the same concentration of sulfacetamide did not match that of tears. Abs, absorbance; SD, standard deviation.
Cytotoxic P. aeruginosa adapts to tear fluid, but changes are lost on transfer to fresh tears.
After longer incubation times (>4 h), bacterial growth rates in tear fluid recovered to levels occurring in MEM (Fig. 5A). Cytoprotective activity was also overcome when bacteria were allowed to incubate with cells in tears for 8 h or longer (Fig. 5B). These results suggested bacterial adaptation to tears or else bacterial degradation of active tear components. Thus, experiments were performed in which bacteria were exposed to tear fluid or to MEM for 48 h and then transferred to fresh tear fluid or MEM and their growth rates were compared to those of unexposed (naïve) bacteria. The results showed that bacterial adaptation to tear fluid was lost immediately after transfer to fresh tear fluid (Fig. 5C), suggesting decay of active tear components after long-term exposure to bacteria.
FIG. 5.
Adaptation of P. aeruginosa to growth inhibitory and cytoprotective effects of tear fluid. (A) Growth of strain 6206 in tear fluid (open circles) or MEM (open squares) over a period of 8 h. After 4 h in tears, the bacterial growth rate matched that in MEM. (B) LDH release induced by strain 6206 after 8 h in tear fluid or in MEM. Cytoprotective effects of tears were no longer present at this time point. Bacterial adaptation to tears was lost on transfer to fresh tears. Abs, absorbance; SD, standard deviation. (C) Fresh tears inhibited the growth of strain 6206 for ∼4 to 6 h even when the bacteria had been previously exposed to tear fluid.
Tear fluid protects corneal epithelial cells against P. aeruginosa invasion.
Invasive P. aeruginosa strains, which invade rather than kill corneal epithelial cells (8), were also studied. Tear fluid blocked corneal epithelial cell entry by all five invasive strains tested (Fig. 6A) but was bacteriostatic against only three of the five strains (Fig. 6B). Thus, tear cytoprotection against invasive strains could also occur in the absence of bacteriostatic activity. Interestingly, the two strains that were resistant to bacteriostatic activity (6294 and 6487) were the only two human corneal isolates of the five invasive strains.
FIG. 6.
Effect of tear fluid on invasion of corneal epithelial cells by and bacterial growth of five invasive strains of P. aeruginosa. Tear fluid (gray bars) inhibited corneal cell invasion by all five invasive strains (A) but inhibited the growth of only three isolates (B).
Tear fluid effects on bacterial morphology.
To begin to understand the mechanism for tear effects on P. aeruginosa, bacteria exposed to tear fluid or MEM were studied by video and still phase-contrast microscopy. After 3 h in tear fluid, but not in MEM, all 10 strains were found to exist predominantly in clumps and/or chains (Fig. 7). In the case of strain 6206, chains were long, appearing to consist of eight or more individual bacteria linked end-to-end. For other strains, e.g., 6294, chains were shorter (two or three bacteria in length) (Fig. 7). Each of the nine motile P. aeruginosa strains, including those that were not susceptible to tear bacteriostatic activity, became nonmotile within minutes of exposure to tear fluid. Loss of motility was observed even with single bacterial cells. Sulfacetamide (1 mg/ml) matched tear bacteriostatic activity and caused chain formation but did not cause motility loss. The nine motile strains were the nine strains susceptible to tear cytoprotective effects. These data suggested a possible link between loss of motility and the mechanism of tear cytoprotection.
FIG. 7.
Phase-contrast microscopy showing tear fluid effects on P. aeruginosa morphology. Cytotoxic and invasive P. aeruginosa isolates were examined in MEM (upper panels) and compared with those exposed to tear fluid for 3 h (lower panels). Typical results for three P. aeruginosa isolates are shown. Tear fluid induced short (e.g., strain 6294) and long (e.g., strain 6206) chain formation or aggregated bacteria into clumps (e.g., strain 6073). All previously motile strains became nonmotile in tear fluid.
Tear bacteriostatic activity and inhibition of bacterial motility are heat labile; tear cytoprotective activity is heat stable.
To denature certain proteins known to have antibacterial properties, e.g., lactoferrin, lysozyme, and IgA, whole tear samples were boiled for 5 min. Heat-treated tear fluid was then tested for bacteriostatic activity, effects on bacterial morphology and motility, and cytoprotection by using the cytotoxic strain 6206 and the invasive strain PAK. These strains were selected since they were each susceptible to all three tear fluid effects.
Boiled tear fluid was no longer bacteriostatic against strain 6206 (Fig. 8A) and no longer visibly affected bacterial morphology, yet it retained full cytoprotective capacity as shown by both trypan blue staining (Fig. 8B) and LDH release (Fig. 8C). Similarly, boiled tear fluid was no longer bacteriostatic against strain PAK (Fig. 9A), but it retained the ability to block invasion by this strain (Fig. 9B). Boiled tears could no longer inhibit motility of any of the motile strains. These results showed that neither bacteriostatic activity nor motility loss was required for cytoprotection. They also suggested that separate tear film components might be involved.
FIG. 8.
Effect of boiled tear fluid on growth and cytotoxicity of P. aeruginosa strain 6206. (A) Bacteriostatic effects of tear fluid were lost after the fluid was boiled. Trypan blue staining (B) and LDH release assay (C) showed that boiled tears retained cytoprotective effects on cultured corneal epithelial cells. Abs, absorbance; SD, standard deviation.
FIG. 9.
Effect of boiled tear fluid on growth of and invasion by P. aeruginosa strain PAK. (A) Bacteriostatic effects of tear fluid were lost after the fluid was boiled. (B) Boiled tears retained their ability to inhibit bacterial invasion of cultured corneal epithelial cells.
Tear cytoprotective activity is not inhibited by elevated salt concentration.
The activity of several tear film components, e.g., lactoferrin, lysozyme, and defensins, has been shown to be sensitive to the elevation of sodium chloride concentration (20, 23). In the present study, the addition of sodium chloride to tear samples did not affect the ability of tear fluid to prevent the cytotoxicity of strain 6206 towards corneal epithelial cells. In a typical experiment with strain 6206, LDH release (absorbance at 490 nm) in the absence of tear fluid was 0.870 ± 0.151, which decreased to 0.416 ± 0.01 in the presence of tear fluid. Addition of sodium chloride (50 mM) to tear fluid did not significantly change the fluid's ability to protect corneal cells from strain 6206 (absorbance at 490 nm, 0.410 ± 0.033). Similarly, sodium chloride did not affect bacteriostatic activity or effects on bacterial motility even when added at a concentration of 100 mM. Bacterial growth in tear fluid with added sodium chloride (100 mM) was minimal and similar to the growth rate in tear fluid without added salt. In a typical experiment, bacterial numbers increased from 1.38 × 106 to 2.02 × 106 CFU/ml in tear fluid with added salt and from 1.28 × 106 to 2.02 × 106 CFU/ml in tear fluid without added salt (P > 0.05; t test). Results from control samples with MEM showed that the addition of 100 mM sodium chloride had no significant effect on bacterial growth (1.84 × 106 to 1.85 × 107 CFU/ml with added salt compared to 1.72 × 106 to 2.08 × 107 CFU/ml without added salt; P > 0.05; t test).
DISCUSSION
The data presented in this study demonstrate two protective functions of human tear fluid that affect the opportunistic bacterial pathogen P. aeruginosa: protection of corneal epithelial cells against bacterium-induced cytotoxicity and inhibition of cellular invasion by these bacteria. Tear film cytoprotection did not rely upon tear fluid bactericidal activity or even upon inhibition of bacterial growth. This was shown in four different ways. (i) Not all strains that were susceptible to cytoprotection by tear fluid were susceptible to tear fluid bacteriostatic activity. One strain that was susceptible to bacteriostatic activity became even more cytotoxic in tear fluid, while another became less cytotoxic while growing faster in tear fluid. (ii) Dilution of tear fluid removed cytoprotection without affecting tear fluid bacteriostatic activity. (iii) Inducing bacteriostasis by using a different agent, sulfacetamide, was significantly less cytoprotective than using tear fluid. (iv) Bacteriostatic activity was heat labile, while cytoprotection was heat stable.
All nine normally motile strains became nonmotile after incubation in tear fluid, and these strains were all susceptible to tear fluid cytoprotection. This suggested a possible link between loss of motility and cell protection. Yet tear cytoprotection occurred without motility loss after heat treatment of tear fluid. Since motility is not required for cytotoxic activity, as demonstrated by the nonmotile cytotoxic strain PA103, this was not a surprising result. It is, however, intriguing that PA103 was the only strain tested that resisted cytoprotection, becoming even more cytotoxic in tears, despite its susceptibility to bacteriostatic activity.
Tear fluid had various morphological effects on bacteria that varied among the 10 strains. In addition to motility loss, there was bacterial chain formation and clumping, which were not seen when bacteria were exposed to MEM. Clumping and chain formation were not universal responses and did not necessarily occur with the same strains, and clumps and chains were variable in size and shape depending upon the strain. None of the three observable morphological effects of tear fluid on bacteria were consistently correlated with either bacteriostatic or cytoprotective activity.
With the functional separation of tear bacteriostatic activity and cytoprotection demonstrated, the activity of boiled tear fluid suggested that there might also be biochemical differences. Heat treatment led to complete loss of both bacteriostatic activity and visible effects on bacterial morphology, while cytoprotective activity against both cytotoxic and invasive P. aeruginosa strains prevailed. The neat functional separation of these effects by heat treatment hints at differences in the responsible tear components. Candidate tear proteins for bacteriostatic activity and visible effects on bacterial morphology include lysozyme, lactoferrin, and IgA but not defensins or secretory phospholipase A, which are both heat stable. Chain formation suggested disruption of bacterial cell wall synthesis, a known target of both lysozyme and lactoferrin in gram-positive bacteria (1, 14). Although lysozyme and lactoferrin do not kill gram-negative bacteria by themselves, they can be bactericidal against some gram-negative bacteria in combination (2) and may have other effects on P. aeruginosa, particularly when combined with other antimicrobial factors present in tear fluid. IgA and tear film mucus may be involved in visible bacterial clumping; both have bacterial binding properties (6, 15, 17). In contrast to bacteriostatic factors, tear cytoprotective factors were heat stable, suggesting that lysozyme, lactoferrin, and IgA may not be required.
The mechanism of tear cytoprotective activity might also involve effects on the corneal epithelial cells. P. aeruginosa cytotoxicity and invasion of corneal epithelial cells require active participation of host epithelial cells, and inhibitors of host cell signaling can prevent these bacterium-induced effects (3). Furthermore, recent evidence suggests that corneal epithelia, like other epithelial surfaces, are capable of innate immune responses that include the secretion of antibacterial defensins (13, 18) and mucin(s) that may protect against bacterial adherence (17). These innate responses also involve host cell signaling (16). Various tear factors have the potential to affect bacterial interactions with cells through effects on corneal epithelia. These include growth factors and cytokines that modulate cell signaling; e.g., hepatocyte growth factor modulates corneal epithelial cell susceptibility to both invasive and cytotoxic P. aeruginosa strains via effects on epithelial cell polarity (11).
Although it would be feasible to study known tear components in isolation, studies of antimicrobial components of tissue secretions have shown that the components can be dependent upon one another for their activities. For example, enteric bacteria are not susceptible to killing by either lactoferrin or secretory IgA alone but are susceptible to the combination of these proteins (21). Similar additive or synergistic effects were shown for lactoferrin and lysozyme (2, 14, 22). Furthermore, the activities of antimicrobial factors can depend heavily upon the concentration of other bystander factors, such as salt and calcium (2). Interestingly, the addition of salt to human tear fluid did not affect its bacteriostatic activity, motility inhibition, or cytoprotective effects, even when added at concentrations that were shown previously to inhibit the synergistic activity of antimicrobials that are known to be in tears (22). Thus, subtractive methods are likely to be the most useful for understanding the relative roles of different tear components in the effects of tear fluid on bacteria. These studies are currently under way.
The relationship between the findings of this study and ocular surface defenses in vivo is yet to be determined. It is interesting, however, that four of the five corneal isolates among the group were resistant to tear bacteriostatic activity and four of five laboratory isolates were susceptible. During contact lens wear, the leading predisposing factor for P. aeruginosa corneal infection, bacteria can adhere to contact lens surfaces, and bacteria that gain access to the tear film may become trapped under the lens. In the present study, tear fluid was found to lose all observed activities against P. aeruginosa after prolonged contact, suggesting bacterial degradation of active tear film components. Cytoprotective activity of tear fluid also declined rapidly with dilution, suggesting another mechanism by which contact lens wear could interfere with tear protective functions. When a lens is inserted into the eye (when it is most likely to be inoculated with gram-negative bacteria), it is accompanied by a volume of lens care solution several times the volume of the tear film on the ocular surface. Whether or not changes to tear protective effects contribute to the increased risk of infection associated with the use of contact lenses is to be determined.
These results also raise questions about the significance of in vitro assays performed in the presence of tissue culture media to study bacterial interactions with host cells. Like the ocular surface, other mucosal sites are also coated with fluid secretions. Whether or not in vitro cell culture phenomena mirror bacteria-cell interactions that actually occur in vivo in the presence of these fluids may need to be examined separately for each mucosal site.
The data collected in this study suggest that tear effects on P. aeruginosa and the interactions of this bacterium with corneal epithelial cells may be complex. Although cytoprotection does not depend upon tear bacteriostatic activity or effects on bacterial motility, it remains possible that these activities involve the same, or overlapping, tear film components. Studies aimed at deciphering the molecular mechanisms of tear effects on P. aeruginosa are likely to improve our understanding of how the ocular surface resists infection and what circumstances predispose to infectious disease. Furthermore, the identification of contributing tear factors could eventually lead to new approaches to the prevention and treatment of infections.
Acknowledgments
This work was supported by research grant R01-EY11221 from the National Institutes of Health, Bethesda, Md., and a Faculty Research Grant from the University of California, Berkeley, to Suzanne M. J. Fleiszig.
We also thank Minjian Ni for technical assistance and Robert Sack for helpful discussions.
Editor: V. J. DiRita
REFERENCES
- 1.Coonrod, J. D., R. Varble, and K. Yoneda. 1991. Mechanism of killing of pneumococci by lysozyme. J. Infect. Dis. 164:527-532. [DOI] [PubMed] [Google Scholar]
- 2.Ellison, R. T., and T. J. Giehl. 1991. Killing of gram-negative bacteria by lactoferrin and lysozyme. J. Clin. Investig. 88:1080-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans, D. J., D. W. Frank, V. Finck-Barbançon, C. Wu, and S. M. J. Fleiszig. 1998. Pseudomonas aeruginosa invasion and cytotoxicity are independent events, both of which involve protein tyrosine kinase activity. Infect. Immun. 66:1453-1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finck-Barbançon, V., J. Goranson, L. Zhu, T. Sawa, J. P. Wiener-Kronish, S. M. J. Fleiszig, C. Wu, L. Mende-Mueller, and D. W. Frank. 1997. ExoU expression by Pseudomonas aeruginosa correlates with acute cytotoxicity and epithelial injury. Mol. Microbiol. 25:547-557. [DOI] [PubMed] [Google Scholar]
- 5.Fleiszig, S. M. J., T. S. Zaidi, E. L. Fletcher, M. J. Preston, and G. B. Pier. 1994. Pseudomonas aeruginosa invades corneal epithelial cells during experimental infection. Infect. Immun. 62:3485-3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fleiszig, S. M. J., T. S. Zaidi, R. Ramphal, and G. B. Pier. 1994. Modulation of P. aeruginosa adherence to the corneal surface by mucus. Infect. Immun. 62:1799-1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleiszig, S. M. J., T. S. Zaidi, and G. B. Pier. 1995. Pseudomonas aeruginosa invasion of and multiplication within corneal epithelial cells in vitro. Infect. Immun. 63:4072-4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleiszig, S. M. J., T. S. Zaidi, M. J. Preston, M. Grout, D. J. Evans, and G. B. Pier. 1996. Relationship between cytotoxicity and corneal epithelial cell invasion by clinical isolates of Pseudomonas aeruginosa. Infect. Immun. 64:2288-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleiszig, S. M. J., J. P. Wiener-Kronish, H. Miyazaki, V. Vallas, K. E. Mostov, D. Kanda, T. Sawa, T. S. B. Yen, and D. W. Frank. 1997. Pseudomonas aeruginosa-mediated cytotoxicity and invasion correlate with distinct genotypes at the loci encoding exoenzyme S. Infect. Immun. 65:579-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fleiszig, S. M. J., E. J. Lee, C. Wu, R. C. Andika, V. Vallas, M. Portoles, and D. W. Frank. 1998. Cytotoxic strains of Pseudomonas aeruginosa can damage the intact corneal surface in vitro. CLAO J. 24:41-47. [PubMed] [Google Scholar]
- 11.Fleiszig, S. M. J., V. Vallas, C. H. Jun, L. Mok, D. F. Balkovetz, M. G. Roth, and K. E. Mostov. 1998. Susceptibility of epithelial cells to Pseudomonas aeruginosa invasion and cytotoxicity is upregulated by hepatocyte growth factor. Infect. Immun. 66:3443-3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleming, A., and V. D. Allison. 1922. Observations on a bacteriolytic ferment found in secretions and tissues. Br. J. Exp. Pathol. 3:252-260. [Google Scholar]
- 13.Haynes, R. J., P. J. Tighe, and H. S. Dua. 1999. Antimicrobial defensin peptides of the human ocular surface. Br. J. Ophthalmol. 83:737-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leitch, E. C., and M. D. P. Willcox. 1999. Elucidation of the antistaphylococcal action of lactoferrin and lysozyme. J. Med. Microbiol. 48:867-871. [DOI] [PubMed] [Google Scholar]
- 15.Masinick, S. A., C. P. Montgomery, P. C. Montgomery, and L. D. Hazlett. 1997. Secretory IgA inhibits Pseudomonas aeruginosa binding to cornea and protects against keratitis. Investig. Ophthalmol. Vis. Sci. 38:910-918. [PubMed] [Google Scholar]
- 16.McNamara, N. A., A. Khong, D. McKemy, M. Caterina, J. Boyer, D. Julius, and C. Basbaum. 2001. ATP transduces signals from ASGM1, a glycolipid that functions as a bacterial receptor. Proc. Natl. Acad. Sci. USA 98:9086-9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McNamara, N. A., and S. M. J. Fleiszig. 1998. Human tear film components bind Pseudomonas aeruginosa. Adv. Exp. Med. Biol. 438:653-658. [DOI] [PubMed] [Google Scholar]
- 18.McNamara, N. A., R. Van, O. S. Tuchin, and S. M. J. Fleiszig. 1999. Ocular surface epithelia express mRNA for human beta defensin-2. Exp. Eye Res. 69:483-490. [DOI] [PubMed] [Google Scholar]
- 19.Nagyova, B., and J. M. Tiffany. 1999. Components responsible for the surface tension of human tear fluid. Curr. Eye Res. 19:4-11. [DOI] [PubMed] [Google Scholar]
- 20.Qu, X.-D., and R. I. Lehrer. 1998. Secretory phospholipase A2 is the principal bactericide for staphylococci and other gram-positive bacteria in human tear fluid. Infect. Immun. 66:2791-2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ragers, H. J., and C. Synge. 1978. Bacteriostatic effect of human milk on E. coli: the role of IgA. Immunology 34:19-28. [PMC free article] [PubMed] [Google Scholar]
- 22.Singh, P. K., B. F. Tack, P. B. McCray, and M. J. Welsh. 2000. Synergistic and additive killing by antimicrobial factors found in human airway surface liquid. Am. J. Physiol. Lung Cell. Mol. Physiol. 279:L799-L805. [DOI] [PubMed] [Google Scholar]
- 23.Singh, P. K., M. R. Parsek, E. P. Greenberg, and M. J. Welsh. 2002. A component of innate immunity prevents bacterial biofilm development. Nature 417:552-555. [DOI] [PubMed] [Google Scholar]