Abstract
Protective immunity against infection with Bacillus anthracis is almost entirely based on a response to the protective antigen (PA), the binding moiety for the two other toxin components. We cloned the PA gene into an auxotrophic mutant of Salmonella enterica serovar Typhimurium as a fusion with the signal sequence of the hemolysin (Hly) A gene of Escherichia coli to allow the export of PA via the Hly export system. To stabilize the export cassette, it was also integrated into the chromosome of the live Salmonella carrier. When S. enterica serovar Typhimurium with the chromosomally integrated PA gene was given intravenously to A/J mice, they developed high levels of antibody to PA. These mice were protected against intraperitoneal challenge with 100 or 1,000 50% lethal doses of B. anthracis strain STI. This work contributes to the development of a Salmonella-based orally delivered anthrax vaccine.
Bacillus anthracis is the etiological agent of anthrax, a potentially fatal disease of wildlife, livestock, and humans. The major virulence factors produced by the bacterium are a polyglutamic acid capsule and the anthrax toxin, which is composed of the lethal factor (LF), the edema factor (EF), and the so-called protective antigen (PA) (17). PA binds to a cellular receptor and permits the internalization of LF and EF into the host cell, where they exert cytotoxic effects (17). Thus, PA is important in any prophylaxis for infection with B. anthracis.
The existing subunit vaccines against anthrax contain predominantly PA, and the protection afforded after immunization with these vaccines is thought to be due mainly to an immune response to PA. In support of this suggestion, immunization with recombinant forms of PA produced in Escherichia coli (9) or in B. anthracis lacking the LF or EF genes (24) has been shown to induce protection against anthrax. The ability of PA to induce a protective response against anthrax is exploited in existing licensed vaccines in which PA is adsorbed to aluminium hydroxide or alum (16, 27). However, such vaccines require multiple parenteral doses and, as such, are not ideally suited to the immunization of large numbers of individuals, especially under field conditions in countries where anthrax is endemic. Given this background, there is a requirement for alternative vaccine delivery systems.
Attenuated Salmonella enterica serovar Typhimurium has been widely used as a vehicle for the delivery of heterologous antigens to immunize against various diseases (2, 5, 15). Attenuated Salmonella-based vaccines can solve the logistical problems associated with parenteral vaccines, since they can be administered orally, enabling them to be easily delivered for widespread use. Some attenuated Salmonella-based vaccines have now been evaluated as candidate typhoid fever vaccines in humans in clinical trials and have been shown to have acceptable safety and immunogenicity profiles (10). Previous work showed that the low-level expression of PA in S. enterica serovar Typhimurium is feasible, and immunization of mice with recombinant Salmonella provided some protection against a challenge with B. anthracis spores in the absence of detectable antibody against PA (3). However, the difficulties of expressing PA in this system meant that the dosing of mice with antibiotic was necessary for maintenance of the plasmid expressing PA.
More recently, attempts to improve the expression of various foreign antigens in S. enterica serovar Typhimurium have led to the development of the hemolysin A (HlyA) export-expression system (11, 13, 14). We considered that this system might allow the stable expression of PA, resulting in improvements in the immunogenicity of a Salmonella-based anthrax vaccine. Therefore, we set out to investigate whether PA could be expressed in S. enterica serovar Typhimurium by using the HlyA export system and whether such constructs would provide protection against anthrax. In the longer term, this work should contribute to the development of an oral vaccine against B. anthracis.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth conditions.
Zoosaloral H, an auxotrophic derivative (His− Ade−) of S. enterica serovar Typhimurium, was described previously (22). S. enterica serovar Typhimurium strain χ3760 (restriction deficient) was kindly provided by R. Curtiss III, Washington University. E. coli TOP10F′ cells were obtained from Invitrogen. Plasmids pLG612-1B and pVDL9.3 were kindly provided by C. A. Guzman, GBF, Braunschweig, Germany. The miniTn5pUTKm transposon vector and the corresponding strains for cloning and conjugation were kindly provided by K. N. Timmis, GBF. Bacteria were grown statically or with agitation (220 rpm) overnight at 37°C in Luria broth supplemented with kanamycin (50 μg/ml) or chloramphenicol (25 μg/ml) as needed. The in vitro stability of Salmonella strains was determined by culturing recombinant bacteria for 24 h in Luria broth without antibiotics and enumerating bacteria on Luria agar or Luria agar containing the appropriate antibiotics. This strategy was equivalent to culturing the bacteria for approximately 10 generations. To produce inocula, S. enterica serovar Typhimurium was cultured overnight, harvested by centrifugation (6,000 × g for 20 min at 4°C), washed in phosphate-buffered saline (PBS), and resuspended in PBS or Luria broth as indicated below. The inoculum dose was verified by plating serial dilutions of each culture on Luria agar with or without antibiotics.
Construction of recombinant Salmonella.
Recombinant Salmonella was produced according to standard molecular biology protocols (25), unless otherwise stated. All constructs were verified by sequencing analysis.
The coding sequence of PA was resynthesized on the basis of E. coli codon usage (GenBank accession number AX353700) (E. D. Williamson, J. Miller, N. J. Walker, L. W. J. Baillie, P. T. Holden, H. C. Flick-Smith, H. L. Bullifent, and R. W. Titball, 8 July 2001, British Patent Office) (produced by Cambridge Biosciences, Cambridge, United Kingdom, as described by Wada et al. [29]). The coding region for the mature PA83 protein (bp 1891 to 4095 [31]; hereafter referred to as PA83ec) was amplified with PCR primers 5′-ATA GGA TCC GAA GTA AAG CAA GAG AAC-3′ and 5′-ATA GTC GAC TTA ACC GAT CTC GTA AC-3′, containing BamHI and SalI restriction sites, and cloned into plasmid vector pQE30 (Qiagen) by using the BamHI and SalI restriction sites. Plasmid pQE30 contains the strong phage T5 promoter and synthetic ribosome binding site for high translation rates and is used for the high-level expression of proteins. This cloning added an additional 12 codons to the 5′ end of the inserted gene. Therefore, PA83ec consists of 747 amino acids (aa) (theoretical size, 83 kDa). The expression cassette comprising the T5 promoter region and the PA83ec coding region was amplified with primers 5′-TTT CGT CTT CAC CTC GAG AAA TC-3′ and 5′-ATA CCC GGG ACC GAT CTC GTA ACC-3′, which were designed to bind at the 5′ end of the T5 promoter region and the 3′ end of the PA83ec coding region and contained XhoI and SmaI restriction sites, respectively. The amplified fragment was subsequently cloned into plasmid pLG612-1B by using XhoI and SmaI to create a gene fusion of the PA sequence with the 3′ part of the E. coli hlyA coding region containing the signal sequence as described by Tzschaschel et al. (28). This cloning added 220 codons to the 3′ end of the inserted gene. Thus, the complete length of the expressed PA83ec-′HlyA fusion protein was 967 aa (theoretical size, 107 kDa). From this construct, the expression cassette was excised as a BglII-digested fragment and cloned into chloramphenicol-resistant plasmid vector pVDL9.3 (28) to complete the export cassette comprising the T5 promoter, the appropriate PA-′HlyA fusion, and the hlyB and hlyD genes of E. coli. Clones of E. coli TOP10F′ were tested for expression and export of the PA-′HlyA fusion protein, and a selected recombinant plasmid was designated pVDLPA83ec. This plasmid was transformed into Zoosaloral H by using S. enterica serovar Typhimurium χ3760 as a restriction-deficient intermediate host. The resulting transformant was designated ZpVDL9.3PA83ec.
To create a chromosomally integrated form of the PA expression cassette, the entire export cassette (T5 promoter, PA-′HlyA, hlyB, and hlyD) was excised from pVDL9.3 as a NotI-digested fragment and cloned into transposon vector miniTn5pUTKm. The method used for cloning into the transposon vector was described by De Lorenzo et al. (6, 7). Using E. coli S17.1λpir as the donor and Zoosaloral H as the recipient, the transposon vectors were transferred into the Salmonella vaccine strain by conjugation. Briefly, cultures of donor and recipient bacteria were mixed and plated on standard agar (Merck) without antibiotics. Following overnight incubation at 37°C, bacteria were scraped from the plates and washed and subsequently resuspended in 10 mM MgSO4. This suspension was then plated on minimal agar supplemented with 0.1 mM CaCl, 5% (wt/vol) glucose, 25 μg of niacinamide/ml, 20 μg of histidine/ml, 20 μg of adenine/ml, and 50 μg of kanamycin/ml and incubated at 37°C. Single colonies were resuspended and cultured in minimal medium overnight at 37°C and then plated on Salmonella selective agar (XLD; Difco) supplemented with kanamycin. Transconjugants carrying a chromosomally integrated copy of the recombinant transposon were selected by using the kanamycin resistance marker of the transposon and the auxotrophies of Zoosaloral H. The Tn5 transposon integrates randomly, and the site of integration of the transposon was not determined in this study. However, several transformants were tested for their generation times in vitro. A transformant with a generation time similar to that of the parent strain, Zoosaloral H, was selected. The resulting transformant was designated ZpUTKmPA83ec.
Expression of PA.
Cultures of recombinant Salmonella were grown overnight with shaking in Luria broth containing chloramphenicol or kanamycin as needed. Subsequently, 250 μl of each culture was centrifuged at 13,000 × g for 1 min to pellet the cells. The supernatant was diluted 1:1 in 2× Laemmli sample buffer (Sigma-Aldrich Co., Ltd.), and the bacterial pellet was lysed in 50 μl of 2× Laemmli sample buffer. Samples were normalized to similar CFUs per milliliter and then boiled for 10 min. The expression and secretion of PA were examined by sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) on 12.5% polyacrylamide gels (PhastSystem; Amersham Pharmacia Biotech Ltd., Bucks, United Kingdom) and Western blotting (25) on Hybond enhanced chemiluminescence (ECL) nitrocellulose membranes (Amersham). Following transfer, the membranes were blocked with PBS containing 5% bovine serum albumin. The membranes were probed by using rabbit anti-PA serum (produced at the Defence Science and Technology Laboratory [DSTL] by two immunizations with 50 μg of purified recombinant PA [21] in Alhydrogel), and a horseradish peroxidase-conjugated secondary antibody (Amersham) was added. Antibodies were added at 1:1,000 dilutions in PBS-bovine serum albumin, and the membranes were washed with PBS containing 0.05% Tween 20. Proteins were visualized with ECL Western blotting detection reagents (Amersham) and exposure of ECL hyperfilm to the gel and subsequent film development.
Measurement of expressed PA.
A comparison of PAs expressed in Luria broth by ZpVDL9.3PA83ec and ZpUTKmPA83ec was made by using a capture enzyme-linked immunosorbent assay (ELISA) for PA. Briefly, 96-well microtiter plates were coated with 10 μg of mouse anti-PA monoclonal antibody/ml overnight at 4°C. All washing steps were carried out with PBS containing 0.05% (vol/vol) Tween 20. The plates were blocked with 1% (wt/vol) skim milk in PBS for 1 h, and each culture supernatant sample was serially diluted 1:2 in the skim milk blocking solution across the plate, followed by 1 h of incubation. Expressed PA was detected by incubation with rabbit anti-PA domain 4 antibody (10 μg/ml; produced at DSTL by two immunizations with 50 μg of purified recombinant PA domain 4 [9] in Alhydrogel) for 1 h, and binding was detected by incubation with a horseradish peroxidase-conjugated polyclonal goat anti-rabbit immunoglobulin G (IgG) antibody (Bio-Rad Ltd.) diluted 1:2,000 in blocking solution for 1 h. The plates were developed with 100 μl of 2,2′-azinobis(3-ethylbenzthiazoline-6-sulfonic acid) substrate (ABTS) (Sigma-Aldrich Company Ltd.), and the A414 values of the plates were measured. All samples were assayed in duplicate. PA measurements were expressed as the maximum dilution of sample giving an absorbance reading of greater than 0.1 A414 after subtraction of the mean absorbance due to nonspecific binding detected in control wells containing the Zoosaloral H parent strain culture supernatant.
Immunization of mice.
Groups of 10 female A/J mice (supplied and used at 10 weeks of age; Charles River Laboratories, Kent, United Kingdom) were inoculated with ZpVDL9.3PA83ec, ZpUTKmPA83ec, or the parent strain, Zoosaloral H, on days 0, 14, and 28. Mice were inoculated orally (by intragastric gavage) with 109 CFU in Luria broth or intravenously (i.v.) with 105 CFU in PBS.
Measurement of serum antibody titers.
Serum samples were tested for specific antibody responses by an ELISA with standard procedures. Blood samples were collected from the tail veins of all immunized and control mice on days 56 and 72, and serum was assayed for PA-specific IgG1 and IgG2a antibody responses to give an indication of Th2- and Th1-type immune responses, respectively, in mice. Microtiter plates (96 wells) were coated with 0.5 to 1 μg of recombinant PA (produced at DSTL [21]) overnight at 4°C. All washing steps were carried out with PBS containing 0.02% (vol/vol) Tween 20. The plates were blocked with 2% (wt/vol) skim milk in PBS for 1 h, and each serum sample was serially diluted 1:2 in the skim milk blocking solution across the plate, followed by 1 h of incubation. Antibody isotypes were detected by using horseradish peroxidase-conjugated polyclonal goat anti-mouse IgG1 and IgG2a antibodies (Harlan Sera-Lab Ltd.) diluted 1:2,000 in blocking solution and incubated for 1 h. The plates were developed with 100 μl of ABTS, and the A414 values of the plates were measured. All samples were assayed in duplicate. End-point antibody titers were expressed as the maximum dilution of sample giving an absorbance of greater than 0.1 A414 unit after subtraction of the absorbance due to nonspecific binding detected in control sera from mice immunized with S. enterica serovar Typhimurium parent strain Zoosaloral H. The results are presented as the reciprocal of the dilution, and the mean represented the average of duplicate values for each sample. Groups selected for challenge were also bled on day 72 to determine prechallenge PA-specific IgG1 and IgG2a antibody titers.
Challenge with B. anthracis.
At 6 weeks after the final immunizing dose, five A/J mice from groups dosed i.v. with ZpUTKmPA83ec and from control groups (mice immunized with S. enterica serovar Typhimurium Zoosaloral H alone) were challenged intraperitoneally with B. anthracis STI (Tox+ Cap−) spores. Sufficient spores for the challenge were removed from stock cultures, washed in sterile distilled water, and resuspended in PBS to a concentration of 106 or 107 spores per ml. Mice were challenged with 100-μl volumes containing 105 or 106 spores per mouse (equivalent to 100 or 1,000 50% lethal doses [LD50s]) and were monitored for 14 days postchallenge to determine their protected status. The LD50 is based on a previous study carried out with the same strains of B. anthracis, the same mouse strain, and a similar experimental procedure (1). Humane end points were strictly observed so that any animal which displayed a collection of clinical signs that indicated a lethal infection was culled. The challenge experiment was carried out in a blinded fashion.
Statistical analysis.
Values for the mean and standard error of the mean were calculated for each data set. The Student t test was used to determine the significance of differences.
RESULTS
Construction of S. enterica serovar Typhimurium derivatives secreting PA.
To facilitate the high-level expression of PA in S. enterica serovar Typhimurium, a synthetic gene encoding PA with E. coli codon usage was used. The codon usage of the synthetic gene, the PA83ec gene, was more similar to that of Salmonella than to that of the native PA83 gene (Table 1) and thus should have improved the expression of PA. The full-length gene encoding the 83-kDa form of PA was cloned as a gene fusion with a fragment of the hlyA gene. The resultant gene encoded a fusion of the PA protein and the C-terminal region of the HlyA protein from E. coli. Plasmid pVDL9.3PA83ec expressing PA83-′HlyA was transformed into S. enterica serovar Typhimurium strain Zoosaloral H (Fig. 1). The expression cassette was also cloned into miniTn5pUTKm and transformed into Salmonella to generate a chromosomal integrant expressing the PA83-′HlyA fusion protein.
TABLE 1.
Codon usage in native PA83, E. coli codon-optimized PA83ec, and S. enterica serovar Typhimuriuma
| Amino acid | Codon | Frequency/1,000 codons in:
|
||
|---|---|---|---|---|
| PA83 | PA83ec | Salmonella | ||
| R | CGA | 2.7 | 0.0 | 3.5 |
| CGC | 0.0 | 10.8 | 22.5 | |
| CGG | 5.4 | 0.0 | 6.2 | |
| CGU | 4.1 | 27.1 | 19.9 | |
| AGA | 21.7 | 0.0 | 3.1 | |
| AGG | 4.1 | 0.0 | 2.0 | |
| L | CUA | 4.1 | 0.0 | 4.6 |
| CUC | 2.7 | 1.3 | 9.9 | |
| CUG | 1.4 | 58.4 | 49.4 | |
| CUU | 8.2 | 14.9 | 10.5 | |
| UUA | 51.6 | 10.8 | 13.4 | |
| UUG | 9.5 | 2.7 | 11.7 | |
| S | UCA | 19.0 | 0.0 | 7.4 |
| UCC | 4.1 | 25.8 | 10.9 | |
| UCG | 9.5 | 0.0 | 8.3 | |
| UCU | 28.5 | 47.5 | 8.7 | |
| AGC | 1.4 | 13.5 | 16.4 | |
| AGU | 31.2 | 6.7 | 7.6 | |
| T | ACA | 28.5 | 1.3 | 6.8 |
| ACC | 8.2 | 44.8 | 24.1 | |
| ACG | 13.6 | 8.1 | 15.5 | |
| ACU | 25.8 | 21.7 | 8.3 | |
| P | CCA | 13.6 | 8.1 | 6.5 |
| CCC | 4.1 | 1.3 | 6.0 | |
| CCG | 8.2 | 24.4 | 23.7 | |
| CCU | 12.2 | 2.7 | 7.7 | |
| A | GCA | 23.1 | 13.5 | 13.5 |
| GCC | 2.7 | 8.1 | 26.7 | |
| GCG | 9.5 | 10.8 | 37.2 | |
| GCU | 17.7 | 21.7 | 14.7 | |
| G | GGA | 25.8 | 0.0 | 7.4 |
| GGC | 2.7 | 21.7 | 34.3 | |
| GGG | 14.9 | 0.0 | 11.3 | |
| GGU | 4.1 | 24.4 | 19.6 | |
| V | GUA | 23.1 | 14.9 | 12.2 |
| GUC | 2.7 | 6.7 | 17.7 | |
| GUG | 13.6 | 10.8 | 24.8 | |
| GUU | 14.9 | 21.7 | 15.8 | |
| K | AAA | 59.8 | 47.5 | 36.7 |
| AAG | 17.1 | 29.8 | 12.0 | |
| N | AAC | 21.7 | 74.7 | 21.3 |
| AAU | 70.7 | 17.6 | 20.2 | |
| Q | CAA | 35.3 | 12.2 | 12.8 |
| CAG | 5.4 | 28.5 | 31.0 | |
| H | CAC | 1.4 | 8.1 | 9.4 |
| CAU | 12.2 | 6.7 | 11.9 | |
| E | GAA | 51.6 | 44.8 | 38.4 |
| GAC | 8.2 | 36.6 | 21.7 | |
| D | GAG | 16.3 | 23.0 | 21.5 |
| GAU | 55.7 | 27.1 | 34.1 | |
| Y | UAC | 8.2 | 27.1 | 12.6 |
| UAU | 29.9 | 10.8 | 17.6 | |
| C | UGC | 0.0 | 0.0 | 6.3 |
| UGU | 0.0 | 0.0 | 5.0 | |
| F | UUC | 6.8 | 20.3 | 15.3 |
| UUU | 25.8 | 12.2 | 22.5 | |
| I | AUA | 21.7 | 0.0 | 6.7 |
| AUC | 13.6 | 48.9 | 24.8 | |
| AUU | 38.0 | 23.0 | 28.2 | |
| M | AUG | 10.9 | 10.9 | 25.5 |
| W | UGG | 9.5 | 9.5 | 11.8 |
Data for PA83 codon usage were derived from (Williamson et al., (8 July 2001, British Patent Office). Data for S. enterica serovar Typhimurium codon usage were derived from Tzschaschel et al. (28).
FIG. 1.
Construction of ZpVDL9.3PA83ec and ZpUTKmPA83ec.
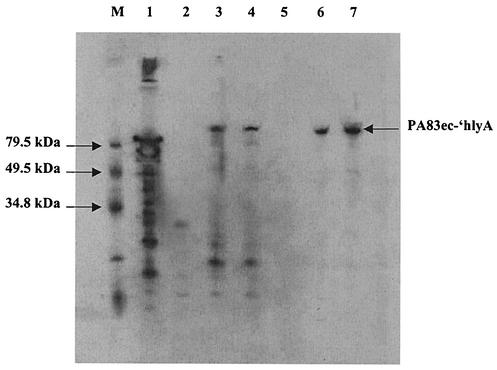
Recombinant Salmonella was orally administrated to mice, and isolates recovered from mouse livers 3 days later were generated to ensure that the modified Salmonella was invasive and capable of replication in mice. Each isolate was shown to express the PA83-′HlyA fusion protein constitutively and to export it into the culture medium (Fig. 2). The measurement of expressed PA by a capture ELISA showed that the level of PA83 secreted into the culture supernatant was higher for Salmonella containing chromosomally integrated PA83-′HlyA (end-point titer, 1:2,048) than for Salmonella carrying the PA83-′HlyA-expressing plasmid (end-point titer, 1:128). When the resulting Salmonella strains were compared in terms of their genetic stability, enumeration of bacteria on agar indicated that the recombinant plasmid expressing PA83-′HlyA was retained by 81% of the Salmonella strains that had been cultured in Luria broth without antibiotic selection for 10 generations.
FIG. 2.
Western blot of auxotrophic S. enterica serovar Typhimurium cell lysates and culture supernatants separated by SDS-PAGE and probed with anti-PA monoclonal antibody. ZpVDL9.3PA83ec (plasmid-borne PA gene), ZpUTKmPA83ec (chromosomal PA gene), and Zoosaloral H (parent) were cultured overnight in Luria broth with appropriate antibiotic selection. Harvested cells and supernatants were normalized to similar CFU per milliliter and lysed in SDS-PAGE sample buffer. Lane M, Bio-Rad biotinylated SDS-PAGE standards, low range; lane 1, 1 mg of recombinant PA/ml; lane 2, Zoosaloral H cell lysate; lane 3, ZpVDL9.3PA83ec cell lysate; lane 4, ZpUTKmPA83ec cell lysate; lane 5, Zoosaloral H supernatant; lane 6, ZpVDL9.3PA83ec supernatant; lane 7, ZpUTKmPA83ec supernatant.
Immunogenicity of Salmonella secreting PA.
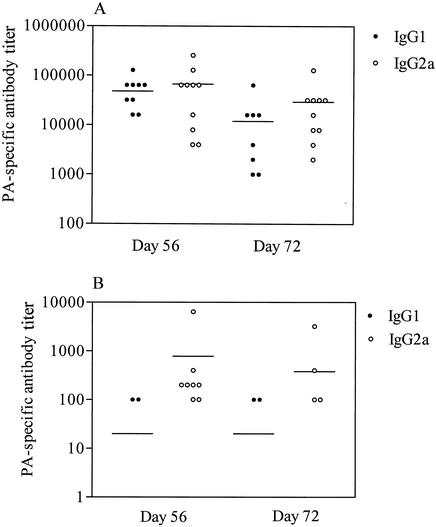
The induction of PA-specific antibodies in A/J mice inoculated three times at 14-day intervals with PA83-′HlyA-expressing Salmonella was evaluated. When a Salmonella strain with the chromosomally encoded PA83-′HlyA fusion protein was administered to A/J mice by the i.v. route, all 10 mice developed IgG1 (titer, 48,000 ± 11,700) and IgG2a (titer, 67,200 ± 24,400) antibodies to PA (Fig. 3A). Thus, administration by the i.v. route resulted in the development of high titers of antibodies to PA (Fig. 3A). In comparison, oral dosing induced significantly lower levels (P < 0.005) of IgG1 (titer, 12,000 ± 6,200) and IgG2a (29,400 ± 11,600) antibodies to PA (Fig. 3B). In addition, similar antibody titers were induced when this Salmonella strain was administered to BALB/c mice (data not shown). Control mice inoculated with S. enterica serovar Typhimurium Zoosaloral H alone did not develop detectable anti-PA antibodies.
FIG. 3.
IgG1 and IgG2a responses to PA determined by ELISA of serum samples following oral or i.v. immunization of mice. Groups of A/J mice (n = 10) were inoculated i.v. (105 CFU) (A) or orally (109 CFU, with a gavage needle) (B) with S. enterica serovar Typhimurium expressing chromosomally encoded PA83ec-′hlyA. Circles show individual values; mean values are indicated by horizontal lines. Results for mice with responses to PA below the limit of detection are not shown.
Protection against challenge with B. anthracis.
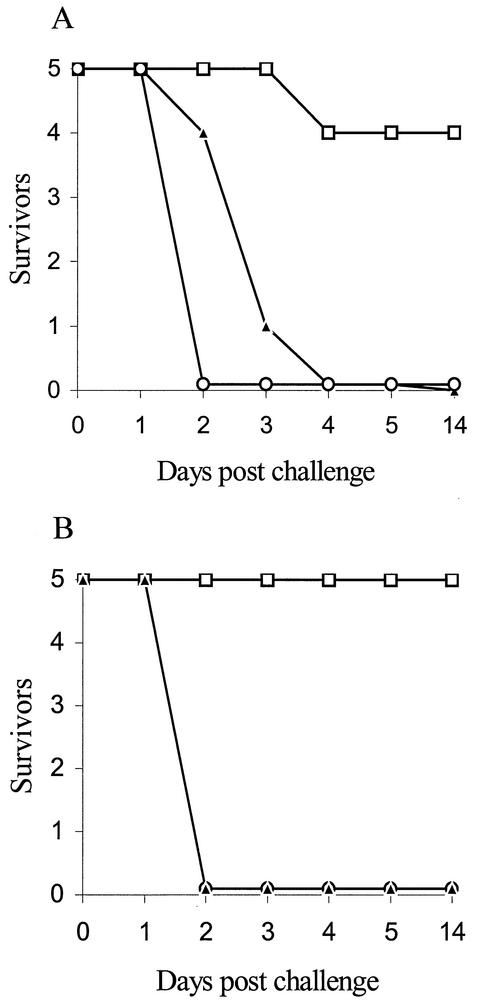
A/J mice which had been inoculated i.v. with S. enterica serovar Typhimurium expressing chromosomally encoded PA83ec-′HlyA were challenged by the intraperitoneal route with 100 or 1,000 LD50s of B. anthracis strain STI spores. Control mice inoculated with S. enterica serovar Typhimurium Zoosaloral H died between 2 and 4 days postchallenge (Fig. 4). In contrast, 9 of 10 immunized mice were protected against the challenge with B. anthracis. The antibody titers of the nonsurvivor had fallen from 1:32,000 for IgG1 and 1:16,000 for IgG2a on day 56 to an undetectable IgG1 titer (at a dilution of 1:1,000) and an IgG2a titer of 1:2,000 on day 72. In comparison, survivors maintained high titers of PA-specific antibodies to day 72 (Fig. 3).
FIG. 4.
Numbers of mice surviving challenge with 100 (A) or 1,000 (B) LD50s of B. anthracis STI spores over 14 days after oral (open circles) or i.v. (open squares) inoculation with S. enterica serovar Typhimurium expressing chromosomally encoded PA83ec-′hlyA. The survival of control mice inoculated with S. enterica serovar Typhimurium Zoosaloral H alone is also shown (closed triangles).
DISCUSSION
Protective immunity against infection with B. anthracis is almost entirely based on a response to PA, the binding moiety for the other toxin components (24). The effectiveness of both animal and human vaccines depends on the induction of anti-PA antibodies. One key function of these antibodies may be to block the effects of the edema and lethal toxins (19, 20). Antibodies to PA can also reduce the ability of B. anthracis spores to germinate and to survive phagocytosis by macrophages (30). Thus, the induction of PA-specific antibodies is believed to be a key requirement for an improved anthrax vaccine.
Previous work by Coulson et al. (3) reported the expression in S. enterica serovar Typhimurium of PA on a multicopy plasmid derived from the pUC series. This construct suffered from at least two shortcomings. First, the expression of PA was driven by the lac promoter, which may be at least partially inhibited by the plasmid-borne lacIq inhibitor. Second, plasmid derivatives of the pUC series are known to be unstable in Salmonella in the absence of the selective pressure of antibiotics (4). Moreover, the PA signal sequence may be detrimental for the Salmonella host. In the study by Coulson et al. (3), the level of expression of PA in vivo was found to be low, and no antibodies were detectable even after i.v. administration of recombinant Salmonella.
With our cloning system, we attempted to overcome these shortcomings. The PA gene was cloned as the PA83 gene without its own signal sequence and under the control of the T5 promoter. Resynthesized sequences were used with a codon usage optimized for translation in E. coli, thereby enhancing the expression by at least 10-fold compared to that of the original sequence for PA (data not shown). To allow the export of PA, the gene encoding PA was fused to the signal sequence coding region of the E. coli hlyA gene and also linked to the hlyB and hlyD genes. The HlyA export system has been used by others to direct the expression of antigens such as Shiga toxin B subunit (26), interleukin 6 (18), Theileria parva p67 antigen (12), and diphtheria toxoid (23).
Since the PA83-′HlyA-expressing plasmid was not fully stable in Salmonella, a chromosomal integrant was selected for use in animal immunization studies. This Salmonella strain was shown to secrete more PA into the culture supernatant than the plasmid-harboring Salmonella strain, perhaps as a consequence of plasmid instability. Previous workers used BALB/c mice to test the efficacy of Salmonella-based vaccines against anthrax (3). More recently, A/J mice were shown to be susceptible to spores of toxigenic, nonencapsulated strain STI of B. anthracis in a dose-dependent manner (1). Thus, we used the A/J mouse model of B. anthracis infection to test the ability of recombinant Salmonella to induce a protective response against anthrax. Although A/J mice (Ityr) might be more resistant to infection with S. enterica serovar Typhimurium, we found that the serum antibody levels were similar in A/J and BALB/c mice (Itys) which had been immunized with recombinant Salmonella expressing PA (data not shown).
Following i.v. inoculation of A/J mice with recombinant Salmonella, high titers of PA-specific antibodies were detected, including high titers of both IgG1 and IgG2a subclasses (Fig. 3A). In comparison, oral inoculation induced low levels of antibodies to PA (Fig. 3B). Following inoculation by the oral route, recombinant Salmonella was required to penetrate the gut mucosa and invade enterocytes, including the M cells of Peyer's patches, before dissemination to the mesenteric lymph nodes and through the reticuloendothelial system into deep tissues, such as the liver and spleen (8). In comparison, the i.v. route of administration bypasses some of these barriers and may confer less stress upon recombinant Salmonella. Groups of five mice inoculated i.v. were challenged with either 100 or 1,000 LD50s of B. anthracis spores. Nine out of 10 immunized mice were protected against challenge (Fig. 4), and the high PA-specific antibody titer of the nonsurvivor at day 56 had fallen to a low level by day 72 (prechallenge). These findings indicate the importance of PA-specific antibodies in protection against B. anthracis.
This study confirms that Salmonella may be used to deliver PA as a vaccine against B. anthracis. A rational approach of using the HlyA export system has been taken toward the production of secreted PA and to stabilize the expression of PA through chromosomal integration of the export apparatus and PA83 coding sequence. A high level of protection against up to 1,000 LD50s of B. anthracis was afforded by i.v. inoculation with recombinant Salmonella. Future studies will continue to work toward the development of an orally delivered Salmonella-based anthrax vaccine.
Acknowledgments
This work was supported in part by grant InSan I 1200-V-4802 from the Ministry of Defense of Germany.
We thank C. Redmond, H. Flick-Smith, N. Walker, D. Rogers, A. Westwood, H. Jones, S. Hoche, and J. Scott for excellent technical assistance.
Editor: A. D. O'Brien
REFERENCES
- 1.Beedham, R. J., P. C. Turnbull, and E. D. Williamson. 2001. Passive transfer of protection against Bacillus anthracis infection in a murine model. Vaccine 19:4409-4416. [DOI] [PubMed]
- 2.Chatfield, S. N., G. Dougan, and M. Roberts. 1994. Progress in the development of multivalent oral vaccines based on live attenuated Salmonella, p. 55-86. In E. Kurstak (ed.), Modern vaccinology. Plenum Press, New York, N.Y.
- 3.Coulson, N. M., M. Fulop, and R. W. Titball. 1994. Bacillus anthracis protective antigen, expressed in Salmonella typhimurium SL3261, affords protection against anthrax spore challenge. Vaccine 12:1395-1401. [DOI] [PubMed] [Google Scholar]
- 4.Coulson, N. M., M. Fulop, and R. W. Titball. 1995. Effect of different plasmids on colonization of mouse tissues by aromatic amino acid dependant Salmonella typhimurium SL3261. Microb. Pathog. 16:305-311. [DOI] [PubMed] [Google Scholar]
- 5.Curtiss, R., III. 1990. Attenuated salmonella strains as live vectors for the expression of foreign antigens, p. 161-188. In G. C. Woodrow and M. M. Levine (ed.), New generation vaccines. Marcel Dekker, Inc., New York, N.Y.
- 6.De Lorenzo, V., M. Herrero, V. Jakubzik, and K. N. Timmis. 1990. Mini-Tn5 transposon derivatives for insertion, mutagenesis, promoter probing, and chromosomal insertion of cloned DNA in gram-negative eubacteria. J. Bacteriol. 172:6568-6572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Lorenzo, V., and K. N. Timmis. 1994. Analysis and construction of stable phenotypes in Gram-negative bacteria with Tn5- and Tn10-derived mini-transposons. Methods Enzymol. 235:386-405. [DOI] [PubMed] [Google Scholar]
- 8.Finlay, B. B., and S. Falkow. 1989. Common themes in microbial pathogenicity. Microbiol. Rev. 53:210-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flick-Smith, H. C., N. J. Walker, P. Gibson, H. L. Bullifent, S. Hayward, J. Miller, R. W. Titball, and E. D. Williamson. 2002. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 70:1653-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garmory, H. S., K. A. Brown, and R. W. Titball. 2002. Salmonella vaccines for use in humans: present and future perspectives. FEMS Microbiol. Rev. 26:339-353. [DOI] [PubMed] [Google Scholar]
- 11.Gentschev, I., H. J. Mollenkopf, Z. Sokolovic, A. Ludwig, C. Tengel, R. Gross, J. Hess, A. Demut, and A. Goebel. 1994. Synthesis and secretion of bacterial antigens by attenuated Salmonella via the Escherichia coli hemolysin secretion system. Behring Inst. Mitt. 95:57-66. [PubMed] [Google Scholar]
- 12.Gentschev, I., I. Glaser, W. Goebel, D. J. McKeever, A. Musoke, and V. T. Heussler. 1998. Delivery of the p67 sporozoite antigen of Theileria parva by using recombinant Salmonella dublin: secretion of the product enhances specific antibody responses in cattle. Infect. Immun. 66:2060-2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hahn, H. P., C. Hess, J. Gabelsberger, H. Domdey, and B. U. Von Specht. 1998. A Salmonella typhimurium strain genetically engineered to secrete effectively a bioactive human interleukin (hIL)-6 via the Escherichia coli hemolysin secretion apparatus. FEMS Immunol. Med. Microbiol. 20:111-119. [DOI] [PubMed] [Google Scholar]
- 14.Hess, J., L. Grode, I. Gentschev, J. Fensterla, G. Dietrich, W. Goebel, and S. H. E. Kaufmann. 2000. Secretion of different listeriolysin cognates by recombinant attenuated Salmonella typhimurium: superior efficacy of haemolytic over non-haemolytic constructs after oral vaccination. Microbes Infect. 2:1799-1806. [DOI] [PubMed] [Google Scholar]
- 15.Hormaeche, C. E., C. M. A. Khan, P. Mastroeni, B. Villarreal, G. Dougan, M. Roberts, and S. N. Chatfield. 1995. Salmonella vaccines: mechanisms of immunity and their use as carriers of recombinant antigens, p. 119-153. In D. A. A. Ala'Aldeen and C. E. Hormaeche (ed.) Molecular and clinical aspects of bacterial vaccine development. John Wiley & Sons, London, England.
- 16.Ivins, B. E., S. L. Welkos, S. F. Liffle, M. H. Crumrine, and G. O. Nelson. Immunization against anthrax with Bacillus anthracis protective antigen combined with adjuvants. Infect. Immun. 60:662-668. [DOI] [PMC free article] [PubMed]
- 17.Leppla, S. H. 1995. Anthrax toxins, p. 543-572. In J. Moss, B. Iglewski, M. Vaughan, and A. Tu (ed.), Bacterial toxins and virulence factors in disease. Marcel Dekker, Inc., New York, N.Y.
- 18.Li, Y., C. Hess, B. U. Von Specht, and H. P. Hahn. 2000. Molecular analysis of hemolysin-mediated secretion of a human interleukin-6 fusion protein in Salmonella typhimurium. FEMS Immunol. Med. Microbiol. 27:333-340. [DOI] [PubMed] [Google Scholar]
- 19.Little, S. F., B. E. Ivins, P. F. Fellows, and A. M. Friedlander. 1997. Passive protection by polyclonal antibodies against Bacillus anthracis infection in guinea pigs. Infect. Immun. 65:6171-6175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McBride, B. W., A. Mogg, J. L. Telfer, M. S. Lever, J. Miller, P. C. B. Turnbull, and L. Baillie. 1998. Protective efficacy of a recombinant protective antigen against Bacillus anthracis challenge and assessment of immunological markers. Vaccine 16:810-817. [DOI] [PubMed] [Google Scholar]
- 21.Miller, J., B. W. McBride, R. J. Manchee, P. Moore, and L. W. J. Baillie. 1998. Production and purification of recombinant protective antigen and protective efficacy against Bacillus anthracis. Lett. Appl. Microbiol. 26:56-60. [DOI] [PubMed] [Google Scholar]
- 22.Mitov, I., V. Denchev, and K. Linde. 1992. Humoral and cell-mediated immunity in mice after immunization with live oral vaccines of Salmonella typhimurium: auxotrophic mutants with two attenuating markers. Vaccine 10:61-66. [DOI] [PubMed] [Google Scholar]
- 23.Orr, N., J. E. Galen, and M. M. Levine. 1999. Expression and immunogenicity of a mutant diphtheria toxin molecule, CRM(197), and its fragments in Salmonella typhi vaccine strain CVD 908-htrA. Infect. Immun. 67:4290-4294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pezard, C., M. Weber, J. C. Sirard, P. Berche, and M. Mock. 1995. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect. Immun. 63:1369-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 26.Su, G. F., H. N. Brahmbhatt, V. de Lorenzo, J. Wehland, and K. N. Timmis. 1992. Extracellular export of Shiga toxin B-subunit/haemolysin A (C-terminus) fusion protein expressed in Salmonella typhimurium aroA-mutant and stimulation of B-subunit specific antibody responses in mice. Microb. Pathog. 13:465-476. [DOI] [PubMed] [Google Scholar]
- 27.Turnbull, P. C. B. 1991. Anthrax vaccines: past, present and future. Vaccine 9:533-539. [DOI] [PubMed] [Google Scholar]
- 28.Tzschaschel, B. D., C. A. Guzmán, K. N. Timmis, and V. De Lorenzo. 1996. An Escherichia coli hemolysin transport system-based vector for the export of polypeptides: export of Shiga-like toxin of IIeB subunit by Salmonella typhimurium aroA. Nat. Biotechnol. 14:765-770. [DOI] [PubMed] [Google Scholar]
- 29.Wada, K.-N., Y. Wada, F. Ishibashi, T. Gojobori, and T. Ikemura. 1992. Codon usage tabulated from the GenBank genetic sequence data. Nucleic Acids Res. 20:2111-2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Welkos, S., S. Little, A. Friedlander, D. Fritz, and P. Fellows. 2001. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiology 147:1677-1685. [DOI] [PubMed] [Google Scholar]
- 31.Welkos, S. L., J. R. Lowe, F. E. McCutchan, M. Vodkin, S. H. Leppla, and J. J. Schmidt. 1988. Sequence and analysis of the DNA encoding protective antigen of Bacillus anthracis. Gene 69:287-300. [DOI] [PubMed] [Google Scholar]