Abstract
Objectives To evaluate the guidelines on measurement of cholesterol in the national service framework for coronary heart disease and to compare alternative strategies for identifying people at high risk of coronary disease in the general population.
Design Comparison of methods (national service framework criteria, Sheffield tables, age threshold of 50 years, estimated risk assessment using fixed cholesterol values) for identifying people with a 10 year coronary event risk of 15% or greater.
Setting Health survey for England 1998.
Subjects 6307 people aged between 30 and 74 years with no history of myocardial infarction, stroke, or angina.
Main outcome measures Proportion of the total population selected for measurement of cholesterol and proportion of people at 15% or greater risk identified.
Results The national service framework guidelines selected 43.4% (95% confidence interval 42.2% to 44.6%) of the study population for cholesterol measurement and identified 81.2% (80.2% to 82.2%) of those at 15% or greater risk. The Sheffield tables selected 73.1% (72.0% to 74.2%) for cholesterol measurement and identified 99.91% (99.83% to 99.99%) of those at 15% or greater risk. An age threshold of 50 years selected 46.3% (45.1% to 47.5%) for cholesterol measurement and identified 92.8% (92.1% to 93.4%) of those at 15% or greater risk. Estimated risk assessments using fixed cholesterol values selected 17.8% (16.8% to 18.7%) for cholesterol measurement and identified 75.9% (74.8% to 76.9%) of those at 15% or greater risk.
Conclusion Measuring the cholesterol concentration of everyone aged 50 years and over is a simple and efficient method of identifying people at high risk of coronary disease in the general population.
Introduction
National guidelines for the prevention of coronary heart disease recommend the use of absolute risk profiles to guide decisions on treatment.1–3 This approach enables clinicians to target treatment to people who face the greatest risk of heart attack, stroke, or death.
One of the major barriers to routine assessment of coronary risk is that its accurate assessment requires knowledge of both total cholesterol and high density lipoprotein cholesterol.4,5 Although most people referred to outpatients for cardiovascular problems will have their serum lipids measured, extending cholesterol screening to the entire population is not generally considered to be cost effective.6 This has led to the development of different methods to select people at high risk from the general population for measurement of cholesterol and hence accurate risk assessment.
Four screening methods are commonly used in the United Kingdom. Firstly, in the section on primary prevention, the national service framework for coronary heart disease published in 2000 recommends measurement of cholesterol for people with hypertension, diabetes, or a family history of hyperlipidaemia or premature ischaemic heart disease.3 Secondly, the Sheffield tables tailor cholesterol measurement to those people who are most likely to be at 15% or greater risk on the basis of knowledge of their other cardiovascular risk factors, including age, sex, smoking status, and presence or absence of hypertension, diabetes, and left ventricular hypertrophy.7 Thirdly, people can be selected for cholesterol measurement on the basis of their age. Many screening and primary prevention programmes in the United Kingdom, including breast screening and flu vaccination, use age thresholds to identify people at high risk from the general population.8
Fourthly, risk assessments can be estimated on the basis of fixed cholesterol values.9 The Egton Medical Information Systems' clinical computer system, widely used in British general practice, integrates the Framingham equation into its patient record facility. This enables risk assessments to be made automatically by using data on risk factors already entered into the patient's record. Fixed values for the ratio of serum total cholesterol to high density lipoprotein cholesterol, based on average values in the 50-64 year age group from a national survey (5.3 for men and 4.6 for women10) have been built into the risk function. Cholesterol measurements can then be targeted to people with an estimated risk of 15% or more. Once actual cholesterol concentrations have been entered into the patient's record the fixed values can be replaced and accurate risk assessments can be made.9
Current guidelines for the prevention of coronary heart disease recommend various drug treatments for people at 15% or greater 10 year coronary risk.1,2 Selective approaches to cholesterol measurement should identify all these people if risk assessments are to be sufficiently accurate for prescribing to be targeted according to current guidelines.
We compared four approaches for selecting people at high risk from the general population against one criterion or “gold standard,” the Framingham 10 year coronary heart disease risk equation, in a sample of 6307 people from the health survey for England 1998.11,12 We evaluated the national service framework criteria, the Sheffield tables, an age threshold of 50 years, and an estimated risk assessment using fixed cholesterol values of 5.3 in men and 4.6 in women. We also evaluated the added value of incorporating the Sheffield tables, an age threshold of 50 years, or an estimated risk assessment into the current cholesterol screening guidelines of the national service framework.
Methods
Data
The health survey for England 1998 was a cross sectional survey of a stratified random sample of the English population aged between 2 and 98 years.11,12 Of the 19 654 people surveyed, 11 190 were aged between 30 and 74 years and thus suitable for risk assessment using the Framingham coronary heart disease risk equation. Complete risk factor data were available on 6748 of these people; of these, 441 people reported a previous myocardial infarction or stroke or current or previous angina, making them unsuitable for risk assessment in primary prevention. The remaining 6307 people represent a contemporary sample of the English population on which we based our analyses.11
Criterion standard
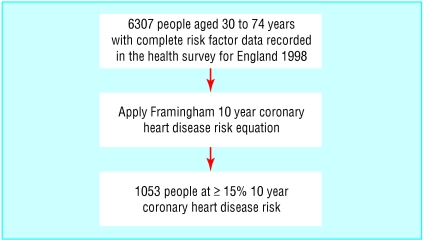
We calculated 10 year coronary heart disease risks of the sample population by using the Framingham equation (fig 1).4 We used this as the accepted criterion standard against which to compare the alternative methods to select people at high risk from the general population.
Fig 1.
Criterion standard: the Framingham coronary heart disease risk equation
Comparison of methods of selection
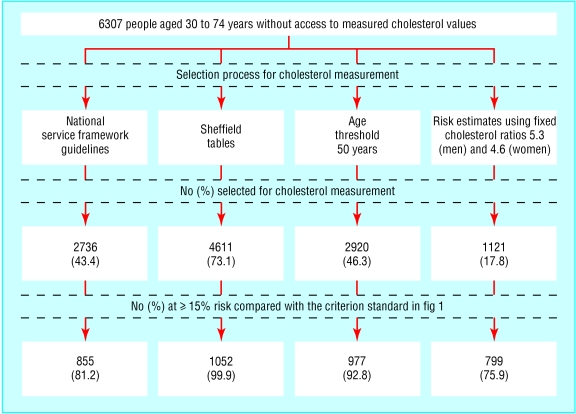
To simulate a real population we were blinded to actual cholesterol values recorded in the database. Firstly, we applied the national service framework criteria alone to the blinded data and recorded the number of people selected for cholesterol measurement. We compared the people who had been selected for cholesterol measurement with the criterion standard to determine the number of people at 15% or greater risk who had been identified (fig 2). We calculated the sensitivity and specificity of the national service framework criteria in identifying people at 15% or greater risk.13
Fig 2.
Comparison of methods to identify people at 15% or greater 10 year coronary risk without access to measured cholesterol values
We repeated the analyses for the Sheffield tables, an age threshold of 50 years, and an estimated risk assessment using a fixed total cholesterol to high density lipoprotein cholesterol ratio of 5.3 in men and 4.6 in women. We recommended actual cholesterol measurements if the estimated risk was 15% or greater. We used the same analyses to evaluate the added value of incorporating each of these selection criteria into the current national service framework guidelines.
Results
Table 1 summarises the demographics of the study population. In this population of 6307 people aged between 30 and 74 years with no previous history of myocardial infarction, angina, or stroke, the Framingham equation classified 1053 people (16.7%, 95% confidence interval 15.8% to 17.6%) at 15% or greater 10 year coronary risk.
Table 1.
Characteristics of 2901 men and 3406 women from the health survey for England 1998 who had complete risk factor data recorded. Values are means (SDs) unless stated otherwise
| Men (n=2901) | Women (n=3406) | |
|---|---|---|
| No (%) smokers | 671 (23.1) | 784 (23.0) |
| No (%) with diabetes | 73 (2.5) | 62 (1.8) |
| No (%) with Framingham 10 year coronary heart disease risk ≥ 15% | 824 (28.4) | 229 (6.7) |
| Age (years) | 49 (12.3) | 49 (12.2) |
| Systolic blood pressure (mm Hg) | 137 (16.8) | 132 (19.1) |
| Diastolic blood pressure (mm Hg) | 79 (11.4) | 73 (11.2) |
| Total cholesterol (mmol/l) | 5.7 (1.05) | 5.7 (1.14) |
| High density lipoprotein cholesterol (mmol/l) | 1.3 (0.36) | 1.6 (0.41) |
| Ratio of total cholesterol to high density lipoprotein cholesterol | 4.8 (1.71) | 3.9 (1.39) |
The current national service framework for coronary heart disease guidelines alone selected 43.4% (42.2% to 44.6%) of the population aged between 30 and 74 years for cholesterol measurement. Compared with the criterion standard this method identified 81.2% (80.2% to 82.2%) of those at 15% or greater risk (table 2).
Table 2.
Comparison of the current national service framework for coronary heart disease cholesterol screening criteria, the Sheffield tables, age thresholds, and estimated risk assessments. Values are percentages (95% confidence intervals) unless stated otherwise
| Strategy to identify people for cholesterol measurement | Adults (aged 30-74 years with no previous history of MI, stroke, angina) identified for cholesterol measurement | People at ≥ 15% risk identified | No of cholesterol measurements needed to identify one person at ≥ 15% risk (yield) |
|---|---|---|---|
| National service framework criteria | 43.4 (42.2 to 44.6) | 81.2 (80.2 to 82.2) | 3.2 |
| Sheffield tables | 73.1 (72.0 to 74.2) | 99.91 (99.83 to 99.99) | 4.4 |
| All people aged ≥50 years | 46.3 (45.1 to 47.5) | 92.8 (92.1 to 93.4) | 2.9 |
| All people whose estimated risk calculated by using fixed TC:HDL (5.3 in men and 4.6 in women) is ≥15% | 17.8 (16.8 to 18.7) | 75.9 (74.8 to 76.9) | 1.4 |
| National service framework criteria plus Sheffield tables | 78.4 (77.4 to 79.4) | 99.91 (99.83 to 99.99) | 4.7 |
| National service framework criteria plus all those ≥50 years | 60.9 (59.8 to 62.2) | 97.5 (97.2 to 97.9) | 3.7 |
| National service framework criteria plus all those whose estimated risk calculated by using fixed TC:HDL is ≥15% | 46.8 (45.5 to 48.0) | 93.4 (92.7 to 93.9) | 3.0 |
MI=myocardial infarction; TC:HDL=ratio of total cholesterol to high density lipoprotein cholesterol.
The Sheffield tables selected 73.1% (72.0% to 74.2%) of the population aged between 30 and 74 years for cholesterol measurement. Compared with the criterion standard this method identified 99.91% (99.83% to 99.99%) of those at 15% or greater risk (table 2). An age threshold of 50 years selected 46.3% (45.1% to 47.5%) of the population aged between 30 and 74 years for cholesterol measurement. Compared with the criterion standard this method identified 92.8% (92.1% to 93.4%) of those at 15% or greater risk (table 2).
An estimated risk assessment using fixed total cholesterol to high density lipoprotein cholesterol ratios of 5.3 in men and 4.6 in women selected 17.8% (16.8% to 18.7%) of the population aged between 30 and 74 years for cholesterol measurement. Compared with the criterion standard this method identified 75.9% (74.8% to 76.9%) of those at 15% or greater risk (table 2). Table 2 also summarises the impact of adding the Sheffield tables, an age threshold of 50 years, or an estimated risk assessment to the current national service framework criteria on cholesterol measurement.
Discussion
In a contemporary sample of the English population the current national service framework guidelines recommend cholesterol measurement in 43.4% of people aged between 30 and 74 years and identify 81.2% of those with a 10 year coronary risk of 15% or greater. Of the alternative screening tests evaluated, an age threshold of 50 years selected a similar proportion of the study population for cholesterol measurement (46.3%) and identified an additional 11.6% of those at 15% or greater 10 year coronary risk.
The effectiveness of a screening programme can be improved in two ways. The intervention can be made more effective or the population can be targeted more efficiently.9 In this study we compared alternative methods for selecting people at high risk from a sample of the English population aged between 30 and 74 years against one criterion standard, the Framingham coronary risk equation with data on all covariates. We have presented the results to enable comparisons to be made between the proportion of the population who were selected for cholesterol measurement and the proportion of people at 15% or greater risk who were identified. This is important because general practitioners need to know whose cholesterol to measure based on a rational justification of any approach suggested. This study contributes to the debate on how limited resources are targeted to those people who, according to current guidelines, are most likely to benefit from treatment to reduce their risk of heart disease.
Comparison of screening methods
The Sheffield tables identified almost all people at 15% or greater risk. However, the “cost” of such a high sensitivity is a false positive rate of 67.7% and a requirement to measure the cholesterol in 73.1% of people aged between 30 and 74 years.
The transparency of a screening method based on age may have advantages over other more complex strategies. In this study we used an age threshold of 50 years to select people for cholesterol measurement and hence accurate risk assessment. This strategy required measurement of cholesterol in 46.3% of the population and led to 92.8% of those at 15% or greater risk being identified. Adding this age threshold to the current national service framework criteria resulted in 60.9% of the study population being selected for cholesterol measurement and identified 97.5% of those at 15% or greater risk. Compared with the results from the Sheffield tables this is a big reduction in the number of cholesterol measurements needed. Age is a strong predictor of cardiovascular risk and has the advantage of being readily identifiable by both doctor and patient. The simplicity of this criterion may help to increase the uptake in screening and outweigh the extra cholesterol measurements needed. In addition, this approach may help to identify people with other modifiable risk factors (such as hypertension, diabetes, and smoking) and thus lead to an integrated screening programme for coronary heart disease.
We made estimated risk assessments by using average ratios of total cholesterol to high density lipoprotein cholesterol from a population survey of adults aged between 50 and 64 years.10 We chose these values as they have been built into the Framingham risk function in clinical information systems that are widely used in British general practice. This method required the fewest cholesterol measurements (17.8% of the population aged between 30 and 74 years) and identified 75.9% of people at 15% or greater risk. Adding this method to the current national service framework criteria resulted in 46.8% of the study population being selected for cholesterol measurement (a small increase of 3.4% on the national service framework criteria alone) and identified 93.4% of those at 15% or greater risk. We believe that given the small increase in workload and large increase in the number of people at high risk identified it may be of value to investigate further the fixed cholesterol values used in the equation to improve the proportion of people at 15% or greater risk identified. An additional advantage of this method is that estimating the coronary risk by using fixed total cholesterol to high density lipoprotein cholesterol ratios puts actual cholesterol measurement firmly in the context of risk assessment and thus focuses clinicians' attention on the purpose of the cholesterol measurement.
Health survey for England
We based this study on a sample of adults from the health survey for England 1998,11,12 which comprised 11 190 adults aged between 30 and 74 years. Blood pressure measurements were recorded for 77% of these people. From this sample, 79% had a complete record of other coronary risk factors, including age; sex; total cholesterol and high density lipoprotein cholesterol; reported history of diabetes, myocardial infarction, angina, or stroke; detailed smoking history; and family history including, where appropriate, the age and cause of death of both parents.11 These data provided a contemporary and representative source of risk factor profiles from the adult English population on which to base our analyses.
Risk assessment
We considered cholesterol measurements to be necessary in those people whose Framingham 10 year coronary risk was 15% or greater, as current UK guidelines recommend various drug treatments above this threshold.1,2 Although we acknowledge that the Framingham equation is an imperfect way of predicting coronary events, it represents an accepted criterion standard and has been validated in various populations from the United States, Northern Europe, and Western Australia.14–16 Guidelines emphasise that these boundaries are likely to be temporary, as evidence from clinical trials already shows the benefits of treatment with statins well below 15% 10 year coronary heart disease risk.17 Thus with increasing evidence of therapeutic benefits, improved affordability of drug treatments, and perhaps new funding options emerging, these thresholds may be revisited. However, in this study we chose to reflect current practice and have thus used a 15% risk threshold as the minimum standard above which we believe people should have a cholesterol measurement to enable risk assessments to be sufficiently accurate for treatments to be targeted according to current UK guidelines.
What is already known on this topic
National guidelines for the prevention of coronary heart disease recommend the use of absolute risk profiles to guide decisions on treatment
Various methods are used to select people for measurement of cholesterol and hence accurate risk assessment
What this study adds
The current national service framework criteria identified 81% of people at 15% or greater 10 year coronary risk
Targeting people aged 50 years and over is a simple and efficient method of identifying people for accurate risk assessment
Conclusion
The current national service framework criteria on cholesterol measurement when strictly applied to a sample of the general population aged between 30 and 74 years identified 81.2% of those at 15% or greater 10 year coronary risk. Thus additional methods are needed to identify people at risk of coronary heart disease from the general population. Of the alternative screening tests evaluated in this study, targeting people aged 50 years and over for cholesterol measurement, and hence accurate risk assessment, is a simple and efficient method of identifying those at 15% or greater 10 year coronary risk from the general population.
We thank the Data Archive for access to the 1998 health survey for England.
Contributors: SW initiated the project and was the principal writer of the paper. AJ advised on the statistical analysis. All authors participated in the design of the study and interpretation of the data and contributed to writing the paper. MJC will act as guarantor.
Funding: Barts and The London NHS Trust.
Competing interests: None declared.
References
- 1.Wood D, Durrington P, Poulter N, McInnes G, Rees A, Wray R. Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart 1998;80(suppl 2): 1-29.9764046 [Google Scholar]
- 2.Ramsay LE, Williams B, Johnston GD, MacGregor GA, Poston L, Potter JF, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens 1999;13: 569-92. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. National service framework for coronary heart disease. London, Department of Health, 2000.
- 4.Anderson KM, Wilson PWF, Odell PM, Kannel WB. An updated coronary risk profile: a statement for health professionals. Circulation 1991;83: 356-62. [DOI] [PubMed] [Google Scholar]
- 5.Wilson S, Johnston A, Robson J, Poulter N, Collier D, Feder G, et al. Predicting coronary risk in the general population: is it necessary to measure high density lipoprotein cholesterol? J Cardiovasc Risk 2003;10: 137-41. [DOI] [PubMed] [Google Scholar]
- 6.NHS Centre for Reviews and Dissemination. Cholesterol and coronary heart disease: screening and treatment. Eff Health Care 1998;14(1): 1-16. [Google Scholar]
- 7.Wallis EJ, Ramsay LE, Haq UI, Ghahramani P, Jackson PR, Rowland-Yeo K, et al. Coronary and cardiovascular risk estimation for primary prevention: validation of new Sheffield table in the 1995 Scottish health survey population. BMJ 2000;320: 671-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health. www.doh.gov.uk/publich.htm (accessed 10 Oct 2002).
- 9.Robson J, Boomla K, Hart B, Feder G. Estimating cardiovascular risk for primary prevention: outstanding questions for primary care. BMJ 2000;320: 702-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gregory JR, Foster K, Tyler H, Wiseman M. Dietary and nutritional survey of British adults. London: HMSO, 1990.
- 11.Erens B, Primatesta P. Health survey for England, 1998 [computer file]. 2nd ed. Colchester, Essex: The Data Archive [distributor], 2000. [SN 4150]
- 12.Erens B, Primatesta P, eds. Health survey for England 1998: cardiovascular disease. Vol 1: Findings, Vol 2: Methodology and documentation. London: Stationery Office, 1999.
- 13.Altman DG. Practical statistics for medical research. London: Chapman and Hall, 1991.
- 14.Karter AJ, Gazzaniga JM, Cohen RD, Casper ML, Davis BD, Kaplan GA. Ischemic heart disease and stroke mortality in African-American, Hispanic and non-Hispanic white men and women, 1985-1991. West J Med 1998;169: 139-45. [PMC free article] [PubMed] [Google Scholar]
- 15.Haq IU, Ramsay LE, Yeo WW, Jackson PR, Wallis EJ. Is the Framingham risk function valid for northern European populations? A comparison of methods for estimating absolute coronary risk in high risk men. Heart 1999;81: 40-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knuiman MW, Vu HTV. Prediction of coronary heart disease mortality in Busselton, Western Australia: an evaluation of the Framingham, national health epidemiologic follow up study, and WHO ERICA risk scores. J Epidemiol Commun Health 1997;51: 515-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian cardiac outcomes trial—lipid lowering arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2003;361: 1149-58. [DOI] [PubMed] [Google Scholar]