Abstract
A valid cannabis withdrawal syndrome has been demonstrated in controlled studies with adult marijuana abusers, yet few published reports have examined cannabis withdrawal among adolescents. Adolescents presenting for outpatient substance abuse treatment, whose primary substance of abuse was cannabis, completed a questionnaire reporting the presence and severity of withdrawal symptoms during past periods of cannabis abstinence. Nearly two-thirds of the sample indicated that they had experienced four or more symptoms, and over one-third reported four or more symptoms that occurred at a moderate or greater severity. The magnitude of withdrawal severity was positively correlated with current emotional and behavioral symptoms and self-reported problems with cannabis use. These findings are consistent with previous studies, though the prevalence and magnitude of withdrawal symptoms were lower than that observed in a similar study with adult treatment seekers [Budney, A.J., Novy, P., Hughes, J.R., 1999. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction 94, 1311–1322]. Further research is needed to elucidate associations between cannabis withdrawal effects, the initiation of cessation attempts, and relapse.
Keywords: Cannabis, Marijuana, Withdrawal, Adolescent
1. Introduction
Epidemiological studies of drug-use patterns consistently report that cannabis is the most frequently used illicit drug in most developed countries (European Monitoring Center for Drugs and Drug Addiction, 2003; Hall et al., 1999; SAMHSA, 2003). Treatment admissions for marijuana problems in the U.S. have steadily increased since the mid-1990s and have become comparable in number to admissions for primary cocaine and heroin problems (SAMHSA, 2003). Though not recognized as clinically significant in the DSM and not well defined in the ICD, recent neurobiological, behavioral, and clinical studies have raised concern about the potential role of a cannabis withdrawal syndrome in the development, maintenance, and treatment of chronic cannabis use and dependence (Budney et al., 2004; Budney and Moore, 2002).
Cannabinoid withdrawal has been reliably precipitated using the CB1 receptor antagonist SR141716A in non-human species (Lichtman and Martin, 2002), and an association has been observed between cannabinoid withdrawal and cellular alterations in the limbic system similar to that observed during withdrawal from other drugs of abuse (deFonseca et al., 1997). Controlled laboratory studies with humans have characterized a valid and reliable cannabis withdrawal syndrome in adult heavy (daily or almost daily) cannabis users (Budney et al., 2001, 2003; Haney et al., 1999; Kouri and Pope, 2000). Commonly observed withdrawal symptoms include anger/aggression, anxiety, decreased appetite/weight loss, irritability, restlessness, and sleep difficulty. Depressed mood, stomach pain/physical discomfort, shakiness, and sweating have also been reported, but occur less frequently. Most symptoms onset within 24 h of abstinence, peak within the first week, and last approximately 1–2 weeks (Budney et al., 2003; Kouri and Pope, 2000).
The majority of adults presenting for treatment of cannabis dependence report experiencing cannabis-withdrawal symptoms during periods of abstinence (Budney et al., 1999; Copeland et al., 2001; Stephens et al., 1993, 2002). Only one report, however, provided information on the incidence and magnitude of specific withdrawal symptoms in adults seeking treatment for cannabis-use problems (Budney et al., 1999). Retrospective reports of specific symptoms were concordant with those observed in the aforementioned laboratory studies, with the majority of patients reporting four or more different symptoms of at least moderate severity.
Unfortunately, much less information on cannabis withdrawal among adolescent cannabis users is available. Clinical epidemiological data underscore the potential importance of cannabis withdrawal among youth. Recent estimates indicate that 16, 32, and 37% of 8th, 10th, and 12th graders, respectively, have used cannabis in the previous year, and among 12th graders who used, approximately 20% report using cannabis daily (Johnston et al., 2001). Most importantly, youth aged 20 and under comprise over half of all treatment admissions for cannabis abuse in the U.S., and cannabis is reported to be the primary drug of abuse in the majority of all adolescent substance abuse admissions (SAMHSA, 2001).
Only a few studies provide empirical data on cannabis-withdrawal symptoms among youth. Past cannabis withdrawal was endorsed by 15% of adolescents in a community-based sample that met DSM-IV criteria for either cannabis abuse or dependence (Young et al., 2002). Among adolescents enrolled in a residential treatment program for conduct disordered substance users, 79% met DSM-III-R criteria for cannabis dependence and 67% of those reported experiencing cannabis withdrawal during prior quit attempts (Crowley et al., 1998). In a similar study of conduct-disordered, substance abusing adolescents enrolled in residential or day treatment, approximately 40% met criterion for cannabis withdrawal as assessed using CIDI-SAM interviews (Mikulich et al., 2001). In the two studies that assessed the occurrence of specific withdrawal symptoms, anxiety, restlessness, irritability, trouble concentrating, appetite changes, depression, sleep difficulty, feeling tired or weak, and yawning were most commonly endorsed (Crowley et al., 1998; Mikulich et al., 2001). Last, a clinical case report on three adolescents with daily cannabis-use enrolled in outpatient treatment described similar withdrawal symptoms (Duffy and Milin, 1996).
The present study assessed the prevalence and magnitude of cannabis-withdrawal symptoms in adolescents presenting for outpatient treatment of substance abuse where cannabis was identified as the primary substance being used. As with our initial study on cannabis withdrawal in adult marijuana abusers (Budney et al., 1999), this study relies on retrospective reports of symptoms that occurred during prior periods of abstinence from cannabis. In addition to describing the withdrawal symptom profile, exploratory, correlation analyses were conducted to examine potential predictors of withdrawal such as age, cannabis problem severity, and psychiatric symptomatology. Based on our findings with adults (Budney et al., 1999), we expected positive correlations between withdrawal, cannabis problem severity, and psychiatric symptomology. Results extend previous research by systematically examining the cannabis-withdrawal syndrome in an outpatient sample with psychosocial characteristics typical of the majority of adolescents who enter outpatient treatment for cannabis abuse or dependence.
2. Methods
2.1. Participants
Participants were adolescents seeking outpatient treatment for substance abuse problems at the University of Vermont Treatment Research Center in Burlington, Vermont. Inclusion for this study required that cannabis was the primary drug of abuse, and that the self-reported usual pattern of cannabis-use was at least 15 days of use per month for at least one of the 3 months prior to intake. Patients concurrently dependent on a second drug other than tobacco, or exhibiting severe psychiatric problems (e.g. active psychosis or acute high risk of suicide) were excluded.
Of the 138 adolescents presenting for treatment, 72 (52%) met the above criteria. Sixty-two (45%) were excluded because they reported using cannabis on fewer than 15 days per month, and 4 (3%) were excluded because they met DSM-IV dependence criteria for alcohol or an illicit drug of abuse. Of the 72 participants that met criteria, 19 were enrolled in a 4-week fee-for-service, brief assessment and intervention program for adolescent substance abuse, and 53 were enrolled in a 14-week clinical trial that targeted adolescents (18 and under) with cannabis-use problems.
Participants were between 14 and 19 years old (M = 16.2, S.D. = 1.1 years), and primarily male (90%) and Caucasian (89%) (see Table 1). The homogeneity of this sample is consistent with reports of greater substance abuse and treatment admissions in males in the U.S. (SAMHSA, 2003), and reflects the ethnic composition of the community in which the study was conducted (Vermont Department of Health, 2002). Participants reported using cannabis on a mean of 18.1 (S.D. = 7.8) of the 30 days prior to the intake assessment, smoking cannabis on average 3.5 (S.D. = 2.6) times on those days. Fifty-seven and thirty-one percent met DSM-IV criteria for current cannabis dependence and abuse, respectively. Sixty-one percent reported being current tobacco smokers and approximately half (49%) reported use of alcohol at least once in the month prior to treatment intake. Participant self-report and urine drug testing suggest that use of other illicit drugs was infrequent. One participant tested positive for cocaine and a second participant tested positive for opiates at intake.
Table 1.
Participant characteristics (N = 72)
| Demographics | |
| Mean age (years) | 16.2 ± 1.1 |
| Percent male | 90 |
| Percent Caucasian | 89 |
| Substance use | |
| DSM-IV cannabis dependence (%) | 57 |
| DSM-IV cannabis abuse (%) | 31 |
| Days cannabis use (past 30) | 18.1 ± 7.8 |
| Used tobacco (past month) (%) | 61 |
| Used alcohol (past month) (%) | 49 |
| Cannabis-related problems | |
| MPI score | 8.8 ± 7.2 |
| Withdrawal discomfort score | 9.9 ± 9.6 |
| Psychiatric symptoms | |
| YSR – externalizing scale | 59.8 ± 10.4 |
| Percent in clinical range (%) | 39 |
| YSR – internalizing scale | 51.5 ± 12.4 |
| Percent in clinical range (%) | 16 |
Scores reflect sample mean and standard deviation (S.D.) for specified measures. YSR scale scores reflect t-scores and clinical range is defined as scores in the 90th percentile (t-scores ≥ 63).
2.2. Measures
Data were collected during a 2–3-h intake assessment. Written informed consent was obtained from all participants. Substance-use behavior and dependence were measured via self-report questionnaires and interviews. The Daily Marijuana Questionnaire (DMQ) was adapted from the Daily Drinking Questionnaire (Dimeff et al., 1999) and is a self-report measure of the frequency, quantity, and pattern of cannabis-use during the 3 months prior to intake. A general drug history interview was used to corroborate cannabis-use as assessed by the DMQ, and to assess recent use of alcohol, tobacco, and other illicit drugs. The Marijuana Problem Inventory (MPI), a 23-item questionnaire adapted from the Rutgers Alcohol Problem Index (RAPI) (White and Labouvie, 1989), assessed the number of problem behaviors associated with use of cannabis in the 3 months prior to intake. The MPI had high internal reliability (Cronbach’s alpha = 0.94). Substance-use disorders were assessed using the Vermont Structured Diagnostic Interview modified for the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (Hudziak et al., 1993).
A 15-item version of the Marijuana Withdrawal Checklist (MWC) (Budney et al., 1999) lists common as well as less frequently observed cannabis-withdrawal symptoms (items: craving for marijuana, depressed mood, decreased appetite, increased aggression, increased anger, headache, irritability, nausea, nervousness/anxiety, restlessness, shakiness, sleep difficulty, stomach pains, strange dreams, and sweating). Participants rated each item on a 0–3 scale (0 = not at all, 1 = mild, 2 = moderate, and 3 = severe) based on their experience the last time they stopped using cannabis. A composite withdrawal discomfort score (WDS) was created by summing the severity ratings of all 15 items. The internal reliability of this measure was high (Cronbach’s alpha = 0.92), and is comparable to that observed in our previous studies (range 0.81–0.89). The sensitivity of the MWC to cannabis abstinence effects in our prior laboratory research suggests it is a valid measure of withdrawal.
The Youth Self-Report (YSR) (Achenbach and Rescorla, 2001) assessed emotional and behavioral problems. The YSR has three broad problem scales, externalizing, internalizing, and total problems, and eight specific syndrome scales. For brevity, only the externalizing and internalizing scales are included here. The externalizing problems scale includes items concerning rule-breaking and aggressive behaviors, and the internalizing problems scale includes items concerning anxiety, depression, withdrawn behaviors, and somatic complaints. Scores above the 90th percentile denote clinical significance.
2.3. Data analyses
Data collected using the measures described above were double entered and checked for accuracy. The primary analyses comprise descriptive statistics regarding the prevalence and severity of withdrawal symptoms reported on the MWC. Secondary analyses included a one-way analysis of variance comparing those who met cannabis dependence criteria at intake (N = 41) and those who did not (N = 30) on the WDS. One participant was excluded from this analysis due to missing data on cannabis dependence. Correlation analyses were also performed to explore associations among withdrawal symptoms, and relations between WDS, internalizing and externalizing problem scores, frequency of cannabis-use, MPI score, and age. The distribution of scores was reasonably normal for variables other than the individual MWC items, and thus parametric tests were performed. Due to the limited range of values (0–3) and skewed distribution of individual MWC item scores, Spearman’s rank correlations were used to calculate the inter-item correlations of the MWC. Note that one item on the MPI asks specifically about withdrawal symptoms, and was therefore excluded from computation of the MPI score.
3. Results
3.1. Prevalence and severity
Participants reported an average of 5.3 (S.D. = 4.1) discrete symptoms from the MWC of at least mild severity. Seventy-eight percent reported two or more symptoms, 58% reported four or more symptoms, and 44% reported six or more symptoms (Fig. 1). The most commonly reported symptoms were craving for marijuana, depressed mood, irritability, restlessness, sleep difficulty, increased anger, decreased appetite, increased aggression, nervousness/anxiety, and headache (Table 2). Four of these symptoms (craving for marijuana, depressed mood, irritability, and sleep difficulty) were rated as being of moderate severity or greater by at least 30% of the sample.
Fig. 1.
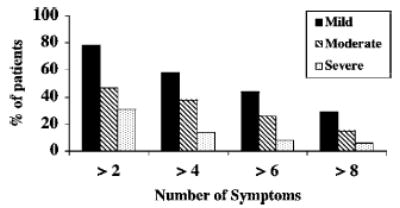
The percentage of participants reporting at least 2, 4, 6, or 8 different MWC items are shown, separated by the minimum rating of symptom severity for each symptom in the cluster.
Table 2.
Percentage of participants who reported each MWC item by severity rating
| Mild rating ≥ 1 | Moderate rating ≥ 2 | Severe rating ≥ 3 | |
|---|---|---|---|
| Mood | |||
| Depressed mood | 58 | 31 | 13 |
| Irritability | 47 | 32 | 18 |
| Increased anger | 40 | 21 | 10 |
| Nervousness/anxiety | 33 | 19 | 13 |
| Behavioral | |||
| Craving | 71 | 46 | 28 |
| Restlessness | 46 | 26 | 10 |
| Sleep difficulty | 43 | 31 | 13 |
| Decreased appetite | 39 | 21 | 6 |
| Increased aggression | 36 | 19 | 8 |
| Strange dreams | 26 | 15 | 8 |
| Physical | |||
| Headache | 32 | 18 | 7 |
| Shakiness | 29 | 14 | 6 |
| Sweating | 19 | 11 | 3 |
| Stomach pains | 18 | 7 | 4 |
| Nausea | 15 | 8 | 1 |
3.2. Secondary analyses
WDS scores for adolescents meeting criteria for cannabis dependence (M = 13.2, S.D. = 9.8) were significantly greater (F(1, 69) = 15.9, P < .01) than those not meeting dependence criteria (M = 4.9, S.D. = 6.9). The 10 most frequently reported withdrawal symptoms were moderately correlated with each other (range = 0.31–0.75; P < .01), except for the correlations between craving and nervousness/anxiety, decreased appetite and headache, and headache and nervousness/anxiety (Table 3). An insufficient sample size precluded factor analysis to further identify discrete subgroups of related symptom expression (e.g. affective, behavioral, etc.).
Table 3.
Correlations among the 10 most frequently reported withdrawal symptoms
| Craving | Appetite | Depress | Irritable | Headache | Aggress | Anger | Ner/Anx | Restless | Sleep | |
|---|---|---|---|---|---|---|---|---|---|---|
| Craving | *** | 0.34* | 0.42* | 0.53* | 0.34* | 0.37* | 0.34* | 0.17 | 0.52* | 0.62* |
| Decreased appetite | *** | 0.56* | 0.51* | 0.29* | 0.56* | 0.54* | 0.38* | 0.59* | 0.49* | |
| Depressed mood | *** | 0.63* | 0.41* | 0.42* | 0.41* | 0.40* | 0.62* | 0.47* | ||
| Irritability | *** | 0.37* | 0.60* | 0.55* | 0.41* | 0.66* | 0.58* | |||
| Headaches | *** | 0.34* | 0.50* | 0.26 | 0.55* | 0.44* | ||||
| Increased aggression | *** | 0.75* | 0.48* | 0.49* | 0.42* | |||||
| Increased anger | *** | 0.31* | 0.55* | 0.52* | ||||||
| Nervousness/anxiety | *** | 0.55* | 0.37* | |||||||
| Restlessness | *** | 0.69* | ||||||||
| Sleep difficulty | *** |
Spearman’s correlation coefficients significant at P < 0.01.
Correlations between the WDS and internalizing and externalizing scales of the YSR, days of cannabis-use in the past 30, total problems on MPI, and age are presented in Table 4. Internalizing and externalizing scores from the YSR and total MPI score showed significant positive correlations with the WDS (r = 0.60, 0.45, and 0.59, respectively; all P < .01).
Table 4.
Correlations between withdrawal discomfort score (WDS) and baseline variables
| Age | 0.01 |
| Days cannabis use | −0.02 |
| MPI score | 0.59* |
| YSR – externalizing | 0.45* |
| YSR – internalizing | 0.60* |
Pearson’s correlation coefficients significant at P < 0.01.
4. Discussion
This study indicates that many cannabis-abusing adolescents who present for outpatient substance abuse treatment report experiencing numerous symptoms when they discontinue using cannabis. The most common symptoms reported were affective and behavioral in nature, although a subset of adolescents also experienced physical symptoms (e.g. headache, nausea, sweating). These findings are consistent with prior reports of cannabis withdrawal in clinical samples. In both the current study and earlier reports on behaviorally disordered adolescents in either residential or day treatments (Crowley et al., 1998; Mikulich et al., 2001), anxiety, appetite change, depressed mood, irritability, and restlessness were among the most commonly reported symptoms. Comparing the present findings with those in our prior study of adult treatment seekers (Budney et al., 1999), six out of the seven most frequently reported symptoms were shared across samples (craving, depressed mood, increased anger, irritability, restlessness, and sleep difficulty).
One noteworthy difference between withdrawal symptom reports in the current adolescent sample and the adult clinical sample (Budney et al., 1999) was that the incidence and magnitude of symptoms was substantially lower in the adolescent sample. For example, the prevalence of craving, depressed mood, irritability, and restlessness in the adolescent sample was 71, 58, 47, and 46%, respectively, compared with 93, 76, 87, and 76% in the adult sample. Also, in the adolescent sample, only ratings of craving were reported as severe by more than 20% of participants, compared with six symptoms (anger, craving, depression, irritability, nervousness, and restlessness) in the adult sample. These differences are likely due to the generally less frequent cannabis use in the adolescent sample compared to the adult sample. Only 32% of the adolescents used cannabis daily in the month prior to intake compared with 82% of the adults.
These findings must be interpreted with caution due to several methodological limitations. First, symptom reports were collected retrospectively, thus, responses were subject to memory and attribution biases. Second, concurrent abstinence from other substances during the referent period of abstinence from cannabis was not controlled. Note, however, that abuse of other drugs was relatively uncommon in this sample, and participants dependent on substances other than cannabis were excluded. Nonetheless, many reported past use of other illicit drugs and over half were current tobacco users, hence the influence of other drug abstinence effects on the symptom reports cannot be ruled out. That said, we believe the validity of these symptom reports is good based on the high degree of correspondence with symptom data collected in the parallel study of adults using the same methodology and laboratory studies examining cannabis withdrawal under controlled conditions (Budney et al., 2004).
Keeping these limitations in mind, nearly two-thirds of the sample reported four or more withdrawal symptoms, and over one-third reported four or more that occurred at moderate or greater severity. Note that in the most recent edition of the DSM, between two and four symptoms are needed to meet criteria for the various substance withdrawal disorders (American Psychiatric Association, 2000). Given the prevalence and magnitude of these symptoms, it is conceivable and concerning that a withdrawal syndrome could contribute to continued use of cannabis and negatively impact cessation attempts among adolescents who use cannabis regularly.
The present study replicated the positive correlation between emotional and behavioral symptoms and withdrawal severity observed in our initial study with adult treatment seekers (Budney et al., 1999). Whether this association reflects an overlap of common symptom reporting in persons with existing psychiatric symptomatology, or indicates that existing psychiatric symptoms exacerbate withdrawal severity is not clear. Similar associations have been observed in tobacco users showing that anxiety, depression, and disordered eating are associated with increased severity of nicotine-withdrawal symptoms (Pomerleau et al., 2000). Prior controlled laboratory studies with adult cannabis users show that such behavioral and emotional symptoms increase in severity during cannabis abstinence compared with measures of these symptoms under conditions of continued cannabis use (Budney et al., 2001, 2003). Hence, the symptoms attributed to cannabis withdrawal in the present sample of adolescents likely reflect valid indicators of a withdrawal syndrome, and suggest that cannabis abusing adolescents with more emotional and behavioral symptoms, like adults with such problems, are apt to experience more severe discomfort when abstaining from cannabis.
In contrast to expectations, significant correlations were not observed between withdrawal severity and age or cannabis use frequency. The failure to observe such associations may have resulted from the narrow range of both variables in the present sample. Moreover, we were unable to control for the time between the interview and the referent abstinence period or the frequency of cannabis use prior to that period, which also may have confounded the relation between these variables. Prospective studies with a larger sample size and broader range of cannabis use are needed to better understand these relations. The strong associations between problem severity (MPI), cannabis dependence, and withdrawal severity may reflect a tendency to attribute problems to cannabis use, or it may indicate that those who have more severe problems or are more severely dependent on cannabis are likely to experience greater withdrawal. These measures may be useful indices for predicting cannabis withdrawal symptoms among those entering treatment.
Significant strides have been made in characterizing and understanding cannabis withdrawal, however, many questions remain, especially concerning adolescents. A prospective examination of withdrawal in adolescent cannabis users would further establish the reliability and validity of the extant findings. Moreover, studies examining the impact of cannabis withdrawal on cessation attempts are clearly needed, as well as those that evaluate whether treatments targeting cannabis withdrawal enhance treatment outcome.
Acknowledgments
This research was supported by grants DA15186, DA12471, and T32-DA07242 from the National Institute on Drug Abuse. Preliminary findings from this article were presented at the Annual Convention of the American Psychological Association, August 2003, Toronto, Ont., Canada.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-age Forms and Profiles. University of Vermont Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; Washington, DC: 2000. (IV-TR ed.). [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Novy PL. Marijuana abstinence effects in marijuana smokers maintained in their home environment. Arch Gen Psychiatry. 2001;58:917–924. doi: 10.1001/archpsyc.58.10.917. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Vandrey RG. A review of the validity and significance of the cannabis withdrawal syndrome. Am J Psychiatry. 2004;161:1967–1977. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA. Development and consequences of cannabis dependence. J Clin Pharmacol. 2002;42:28S–33S. doi: 10.1002/j.1552-4604.2002.tb06000.x. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003;112:393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Novy P, Hughes JR. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–1322. doi: 10.1046/j.1360-0443.1999.94913114.x. [DOI] [PubMed] [Google Scholar]
- Copeland J, Swift W, Rees V. Clinical profile of participants in a brief intervention program for cannabis use disorder. J Subst Abuse Treat. 2001;20:45–52. doi: 10.1016/s0740-5472(00)00148-3. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, MacDonald MJ, Whitmore EA, Mikulich SK. Cannabis dependence, withdrawal, and reinforcing effects among adolescents with conduct disorder symptoms and substance use disorders. Drug Alcohol Depend. 1998;50:27–37. doi: 10.1016/s0376-8716(98)00003-9. [DOI] [PubMed] [Google Scholar]
- deFonseca FR, Carrera MRA, Navarro M, Koob GF, Weiss F. Activation of corticotropin-releasing factor in the limbic system during cannabinoid withdrawal. Science. 1997;276:2050–2054. doi: 10.1126/science.276.5321.2050. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS): A Harm Reduction Approach. The Guilford Press; New York, NY: 1999. [Google Scholar]
- Duffy A, Milin R. Case study: withdrawal syndrome in adolescent chronic cannabis users. J Am Acad Child Adolesc Psychiatry. 1996;35:1618–1621. doi: 10.1097/00004583-199612000-00013. [DOI] [PubMed] [Google Scholar]
- European Monitoring Center for Drugs and Drug Addiction. Annual Report 2003. Office of the Official Publications of the European Communities, Luxembourg. 2003. The state of the drugs problem in the acceding and candidate countries to the European Union. [Google Scholar]
- Hall W, Johnston L, Donnelly N. Epidemiology of cannabis use and its consequences. In: Kalant H, Corrigall WA, Hall W, Smart R, editors. The Health Effects of Cannabis. Centre for Addiction and Mental Health; Toronto: 1999. pp. 69–126. [Google Scholar]
- Haney M, Ward AS, Comer SD, Foltin RW, Fischman MW. Abstinence symptoms following smoked marijuana in humans. Psychopharmacology. 1999;14:395–404. doi: 10.1007/s002130050849. [DOI] [PubMed] [Google Scholar]
- Hudziak J, Helzer JE, Wetzel MW, Kessel KB, McBee B, Janca A, Przybeck P. The use of the DSM-III-R checklist for initial diagnostic assessments. Compr Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings. National Institute Drug Abuse; Bethesda, MD: 2000. (NIH Publication # 01-4923). [Google Scholar]
- Kouri EM, Pope HG. Abstinence symptoms during withdrawal from chronic marijuana use. Exp Clin Psychopharmacol. 2000;8:483–492. doi: 10.1037//1064-1297.8.4.483. [DOI] [PubMed] [Google Scholar]
- Lichtman AH, Martin BR. Marijuana withdrawal syndrome in the animal model. J Clin Pharmacol. 2002;42:20S–27S. doi: 10.1002/j.1552-4604.2002.tb05999.x. [DOI] [PubMed] [Google Scholar]
- Mikulich SK, Hall SK, Whitmore TJ, Crowley TJ. Concordance between DSM-III-R and DSM-IV diagnoses of substance use disorders in adolescents. Drug Alcohol Depend. 2001;61:237–248. doi: 10.1016/s0376-8716(00)00143-5. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Marks JL, Pomerleau OF. Who gets what syndrome? Effects of psychiatric cofactors and nicotine dependence on patterns of smoking withdrawal symptomatology. Nicotine Tob Res. 2000;2:275–280. doi: 10.1080/14622200050147547. [DOI] [PubMed] [Google Scholar]
- SAMHSA. Treatment Episode Data Set (TEDS) 1996–1999: National Admissions to Substance Abuse Treatment Services. DHHS; Rockville, MD: 2001. [Google Scholar]
- SAMHSA. Summary of Findings from the 2002 National Household Survey on Drug Abuse. USDHHS; Rockville, MD: 2003. [Google Scholar]
- Stephens RS, Babor TF, Kadden R, Miller M The Marijuana Treatment Project Research Group. The marijuana treatment project: rationale, design, and participant characteristics. Addiction. 2002;97:109S–124S. doi: 10.1046/j.1360-0443.97.s01.6.x. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Simpson EE. Adult marijuana users seeking treatment. J Consult Clin Psychol. 1993;61:1100–1104. doi: 10.1037//0022-006x.61.6.1100. [DOI] [PubMed] [Google Scholar]
- Vermont Department of Health. Summary of Ethnicity in Vermont based on 2000 U.S. Census. Vermont Department of Health; Burlington, VT: 2002. [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Young SE, Corley RP, Stallings MC, Rhee SH, Crowley TJ, Hewitt JK. Substance use, abuse and dependence in adolescence: prevalence, symptom profiles and correlates. Drug Alcohol Depend. 2002;68:309–322. doi: 10.1016/s0376-8716(02)00225-9. [DOI] [PubMed] [Google Scholar]


