Abstract
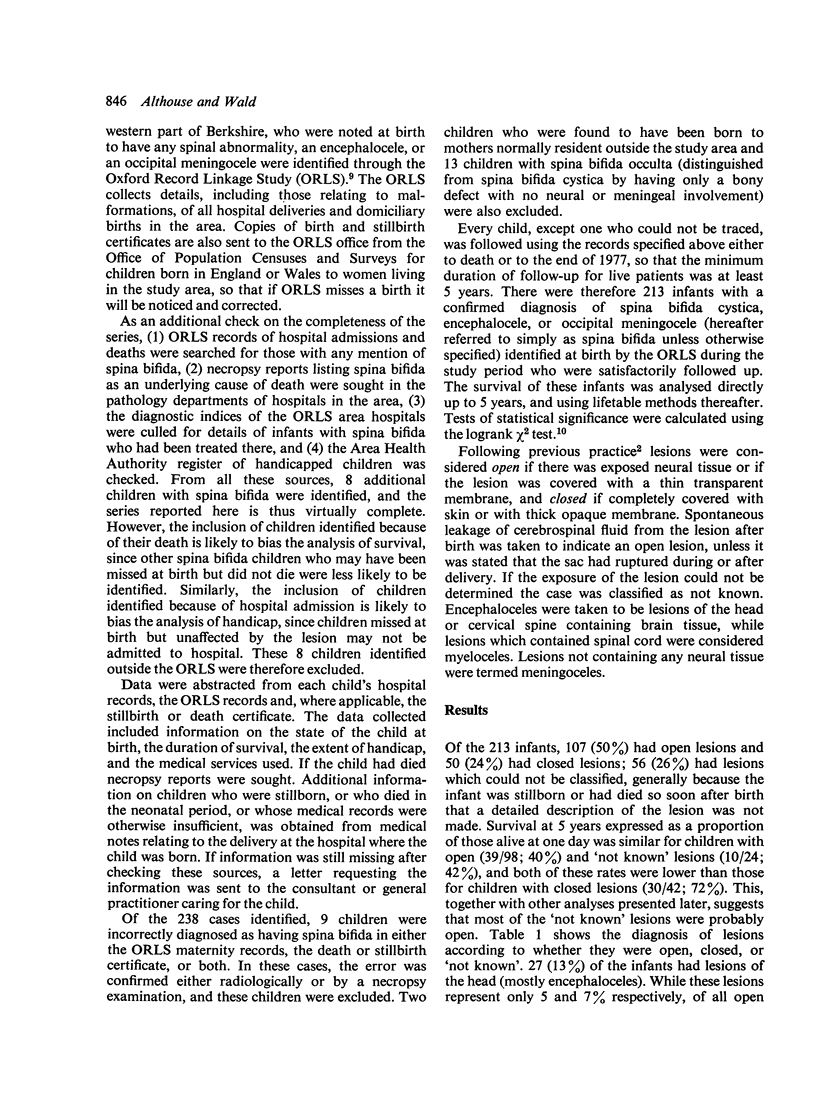
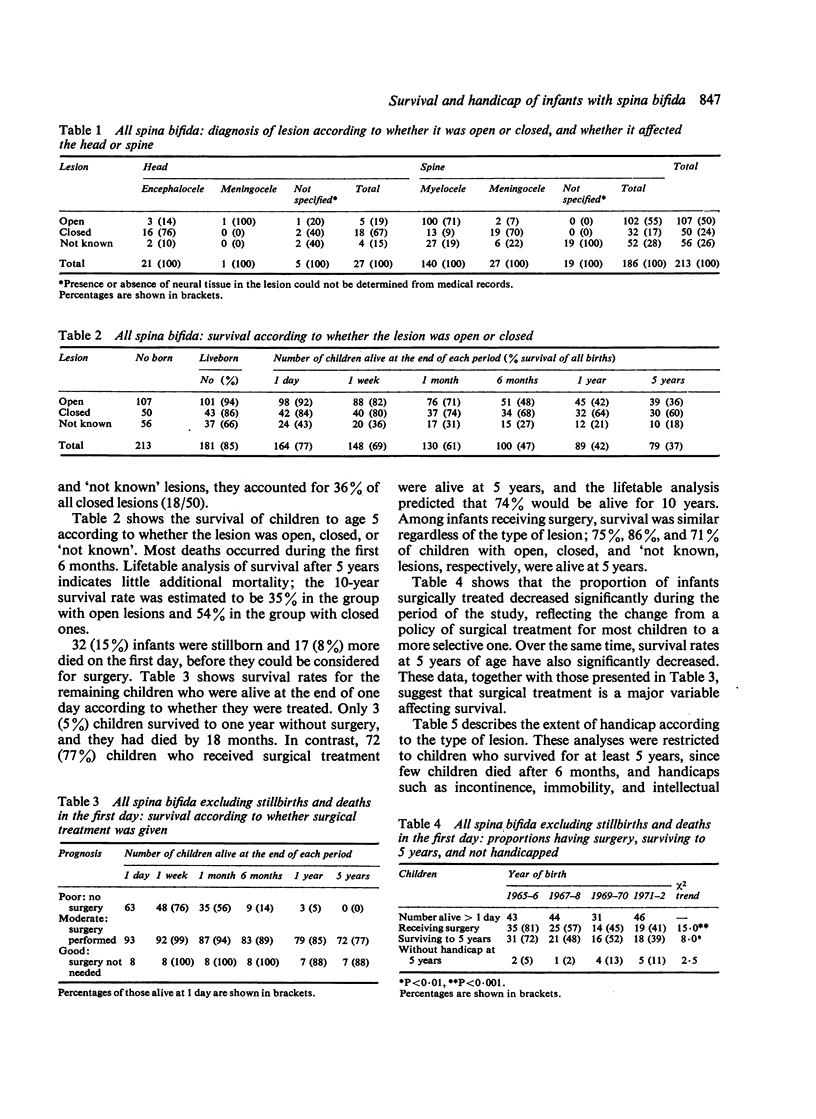
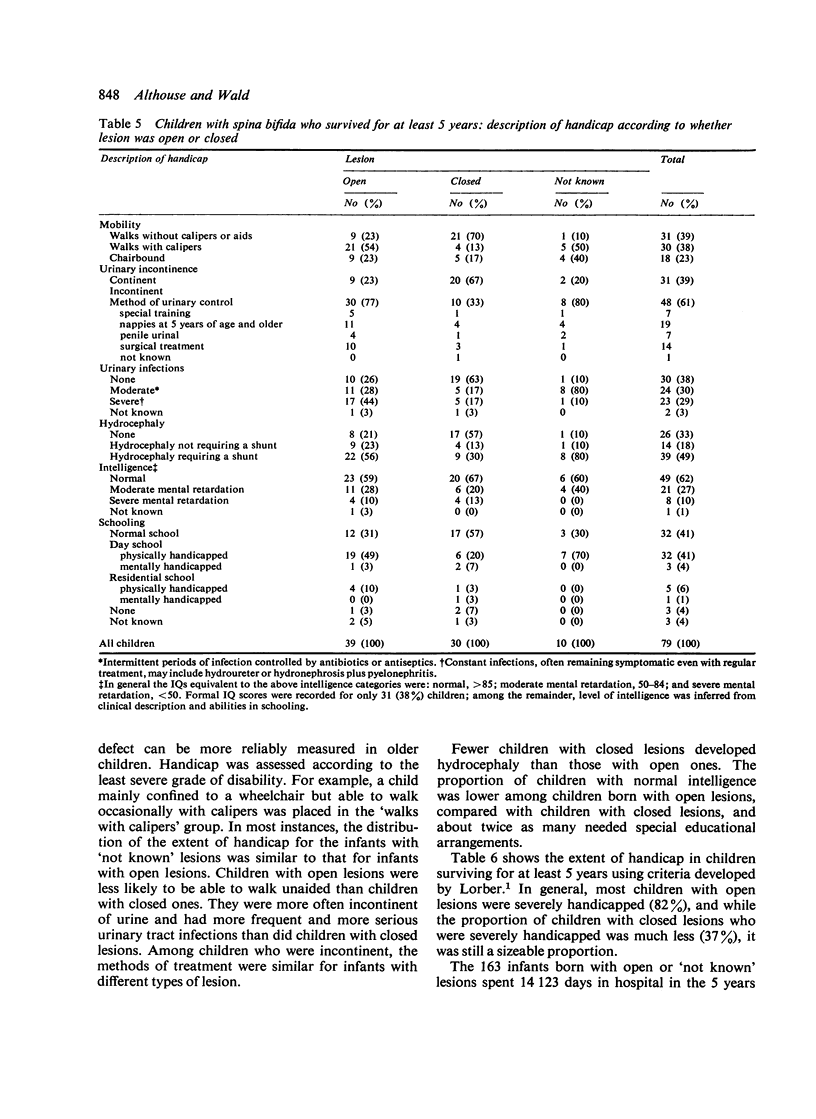
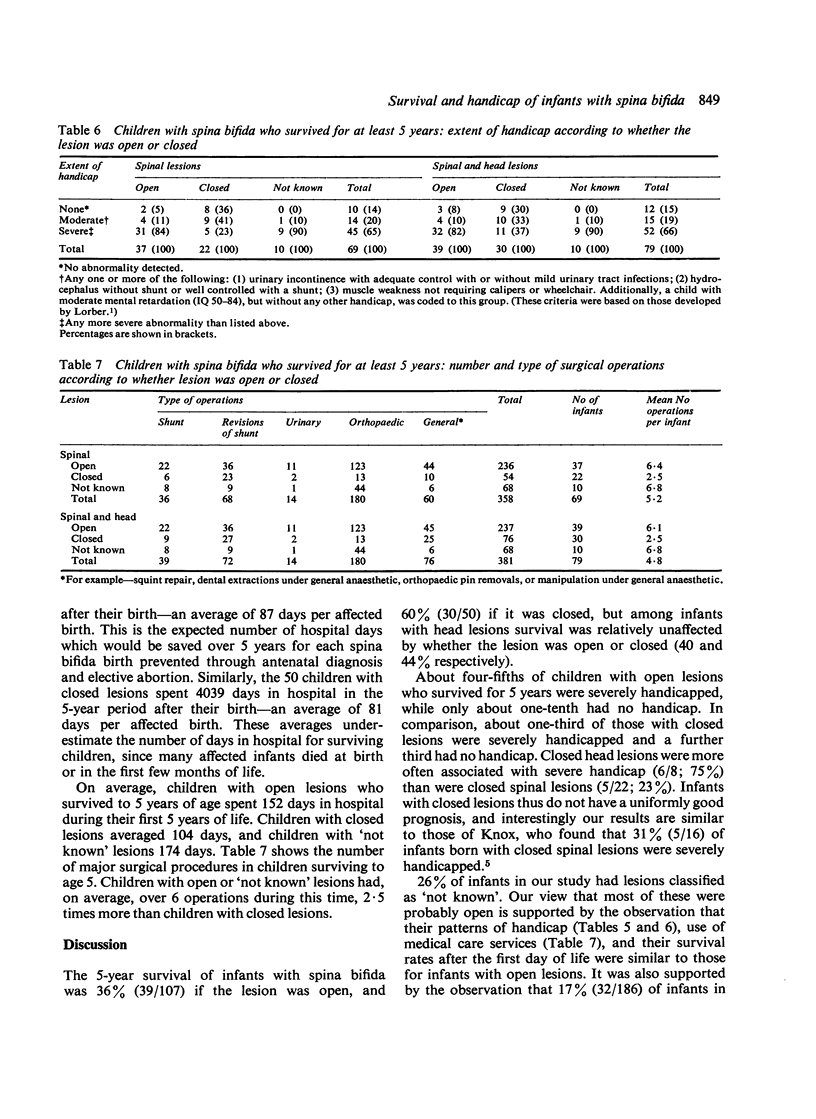
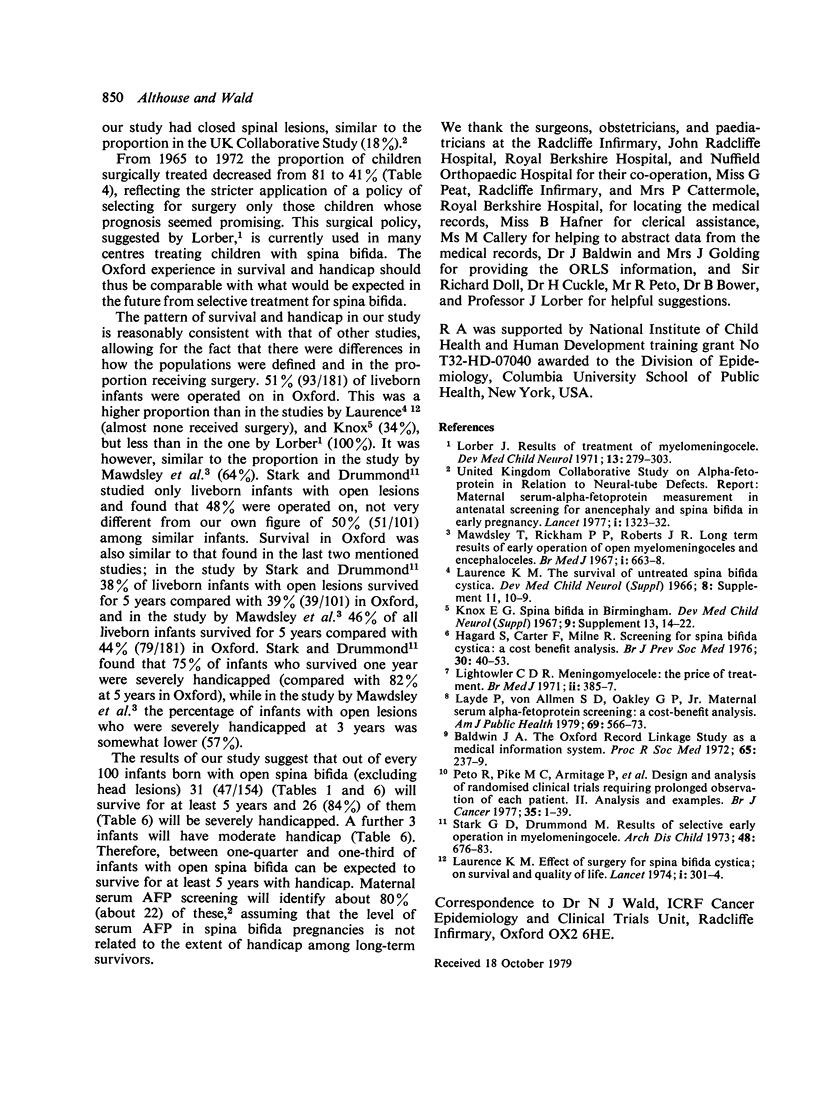
A follow-up study was carried out on 213 infants born with spina bifida cystica (including encephalocele and occipital meningocele) from 1965 to 1972 to women resident in Oxfordshire and the western part of Berkshire. The 5-year survival rate was 36% (39/107) for those with open lesions, 60% (30/50) for those with closed ones, and 18% (10/56) for those with lesions which could not be classified (not known) but which were probably nearly all open. The extent of handicap among these survivors was assessed by means of criteria described by Lorber; among those with open lesions (including 'not known') 84% (41/49) were severely handicapped, 10% (4/49) were moderately handicapped, and only 6% (3/49) had no handicap; among those with closed lesions, 37% (11/30) were severely handicapped, 33% (10/30) were moderately handicapped, and the remaining 30% (9/30) were not handicapped. Closed head lesions (encephalocele or occipital meningocele) were more often associated with severe handicap (6/8; 75%) than were closed spinal lesions (5/22; 23%). The children with open lesions who survived for at least 5 years spent, on average, at least 6 months in hospital during the first 5 years of their life and had, on average, at least 6 major surgical operations. In comparison, those with closed lesions spent one-third less time in hospital, and had fewer than half as many operations. During the period of the study a selective treatment policy was adopted typical of that commonly practised now, and all the infants were born before antenatal screening had been introduced. Our results therefore may be helpful in assessing the benefits to be expected from antenatal screening for open spina bifida.
Full text
PDF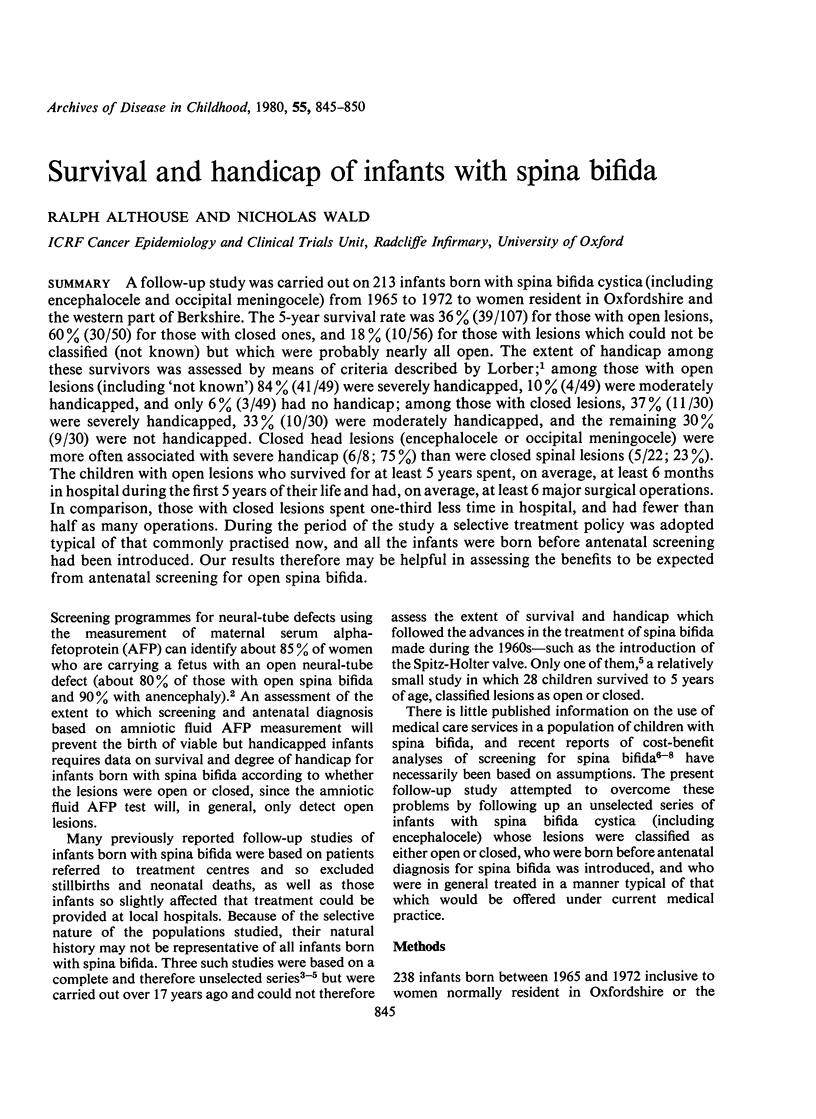
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldwin J. A. The Oxford Record Linkage Study as a medical information system. Proc R Soc Med. 1972 Mar;65(3):237–239. [PMC free article] [PubMed] [Google Scholar]
- Hagard S., Carter F., Milne R. G. Screening for spina bifida cystica. A cost-benefit analysis. Br J Prev Soc Med. 1976 Mar;30(1):40–53. doi: 10.1136/jech.30.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox E. G. Spina bifida in Birmingham. Dev Med Child Neurol. 1967;(Suppl):14–22. doi: 10.1111/j.1469-8749.1967.tb02378.x. [DOI] [PubMed] [Google Scholar]
- Laurence K. M. Effect of early surgery for spina bifida cystica on survival and quality of life. Lancet. 1974 Feb 23;1(7852):301–304. doi: 10.1016/s0140-6736(74)92606-3. [DOI] [PubMed] [Google Scholar]
- Layde P. M., von Allmen S. D., Oakley G. P., Jr Maternal serum alpha-fetoprotein screening: a cost-benefit analysis. Am J Public Health. 1979 Jun;69(6):566–573. doi: 10.2105/ajph.69.6.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightowler C. D. Meningomyelocele: the price of treatment. Br Med J. 1971 May 15;2(5758):385–387. doi: 10.1136/bmj.2.5758.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber J. Results of treatment of myelomeningocele. An analysis of 524 unselected cases, with special reference to possible selection for treatment. Dev Med Child Neurol. 1971 Jun;13(3):279–303. [PubMed] [Google Scholar]
- Mawdsley T., Rickham P. P., Roberts J. R. Long-term results of early operation of open myelomeningoceles and encephaloceles. Br Med J. 1967 Mar 18;1(5541):663–666. doi: 10.1136/bmj.1.5541.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peto R., Pike M. C., Armitage P., Breslow N. E., Cox D. R., Howard S. V., Mantel N., McPherson K., Peto J., Smith P. G. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977 Jan;35(1):1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark G. D., Drummond M. Results of selective early operation in myelomeningocele. Arch Dis Child. 1973 Sep;48(9):676–683. doi: 10.1136/adc.48.9.676. [DOI] [PMC free article] [PubMed] [Google Scholar]


