Abstract
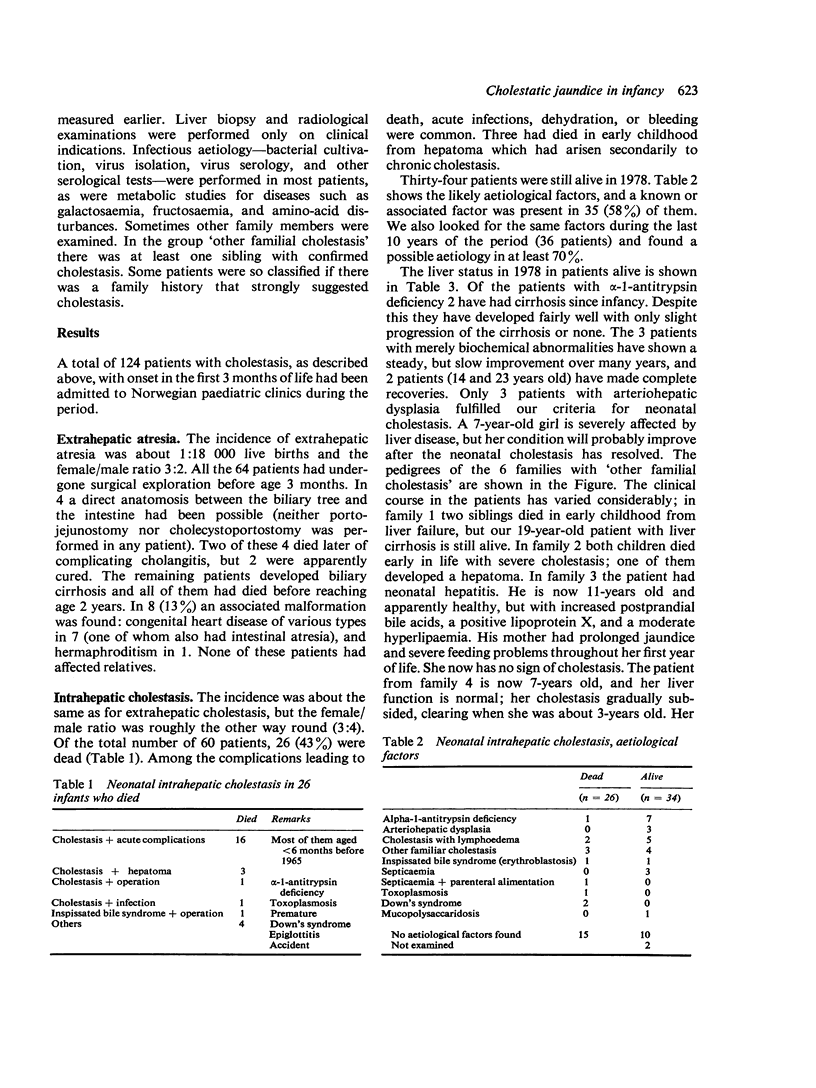
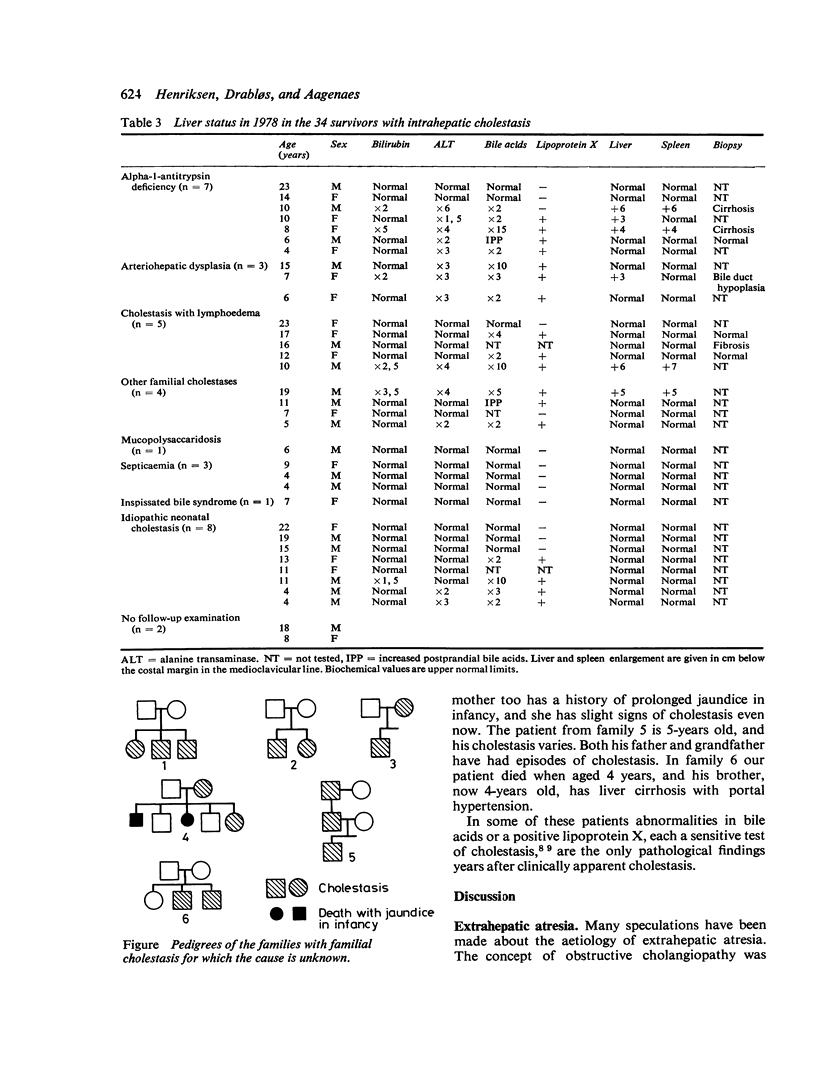
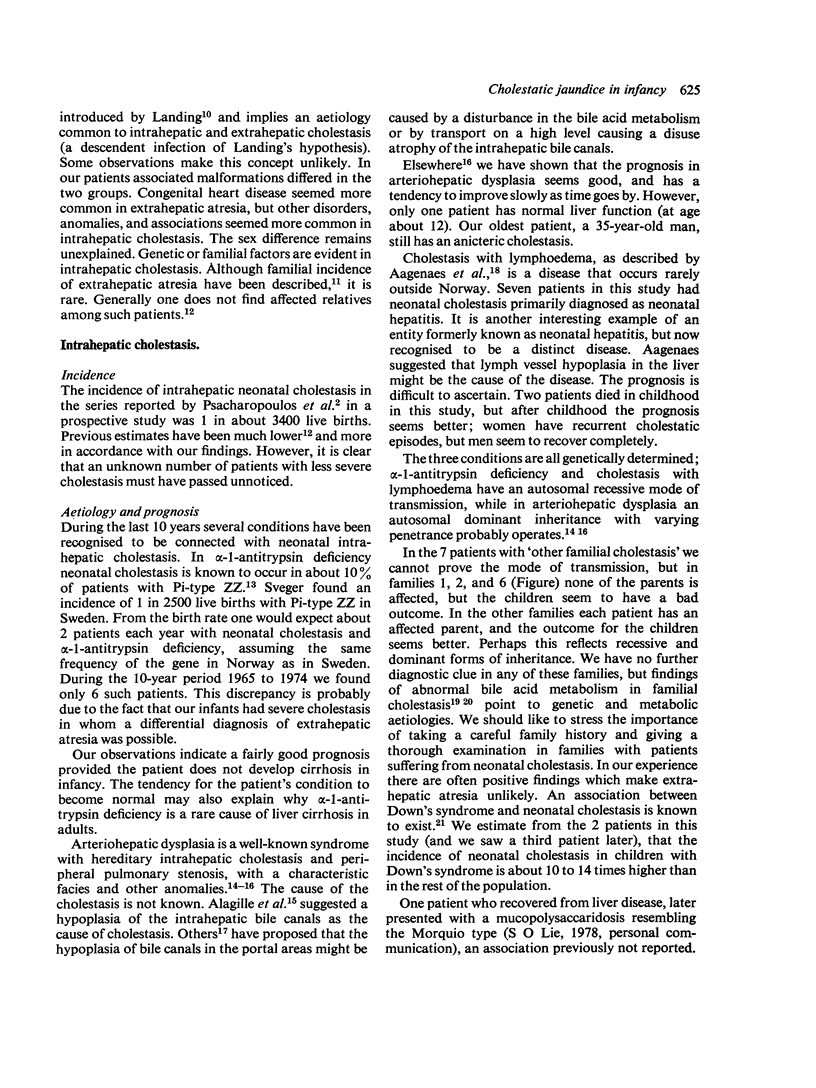
One hundred and twenty-four infants admitted to hospitals in Norway between 1955 and 1974 during the first 3 months of life with cholestatic jaundice were studied retrospectively. Sixty-four infants had had extrahepatic atresia of the biliary tree and 60 had had intrahepatic cholestasis. This gives an incidence of about 1:9000 live births for cholestasis. In 4 of the 64 infants with extra-hepatic atresia a bile duct-to-bowel anastomosis had been performed but this was successful in only 2. Sixty of these infants had died by their 2nd birthday. Twenty-six of the infants with intrahepatic cholestasis had died by 1978 and the most common causes of death were cholestasis complicated by infection, bleeding, or hepatoma. The survivors aged between 4 and 23 years were followed up in 1978. In about two-thirds of them aetiological factors--such as alpha-1-antitrypsin deficiency, arteriohepatic dysplasia, cholestasis with lymphoedema--and other familial or genetic factors, or infections were found. Four of the 34 survivors are known to have cirrhosis. Twenty patients had biochemical abnormalities, and 12 had normal liver function tests. Two patients could not be examined. Of the 19 patients with familial or genetic aetiological factors, 4 had cirrhosis, 14 had biochemical abnormalities, and only 5 had normal liver function tests. Of 11 survivors with idiopathic disease or septicaemia, none had cirrhosis and only 4 had abnormal liver function tests.
Full text
PDF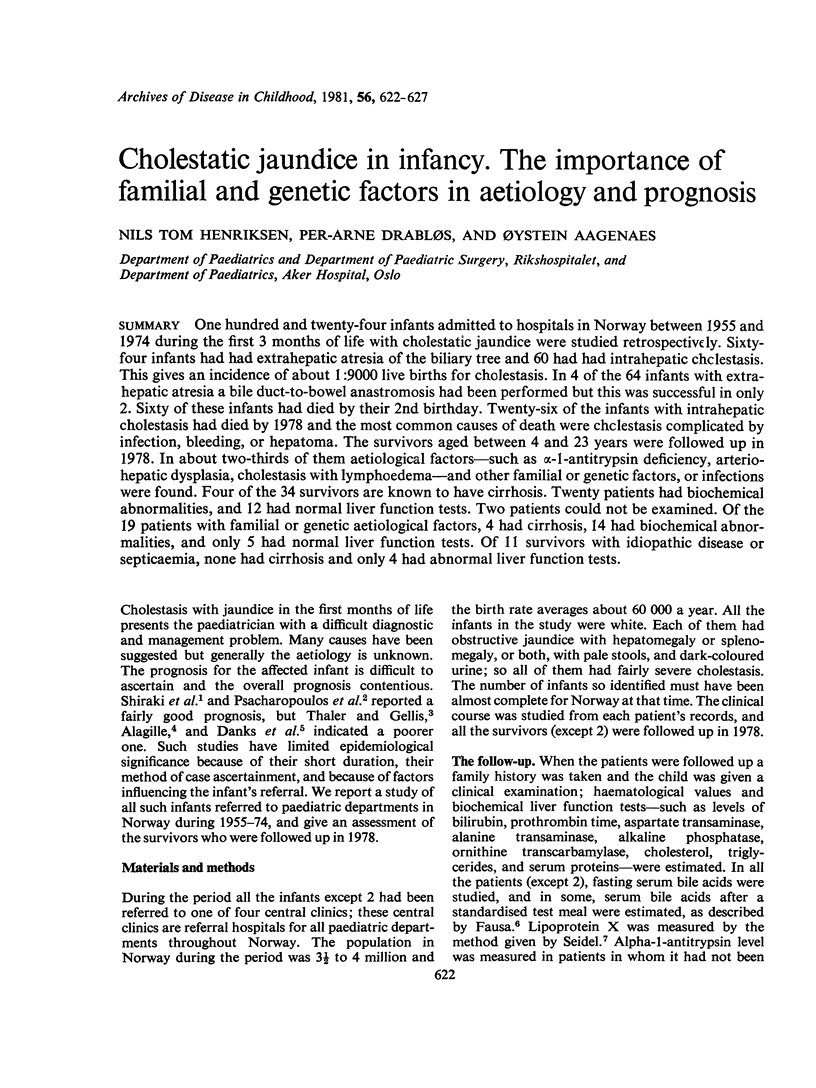
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aagenaes O., van der Hagen C. B., Refsum S. Hereditary recurrent intrahepatic cholestasis from birth. Arch Dis Child. 1968 Dec;43(232):646–657. doi: 10.1136/adc.43.232.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alagille D. Clinical aspects of neonatal hepatitis. Am J Dis Child. 1972 Apr;123(4):287–291. doi: 10.1001/archpedi.1972.02110100019007. [DOI] [PubMed] [Google Scholar]
- Alagille D., Odièvre M., Gautier M., Dommergues J. P. Hepatic ductular hypoplasia associated with characteristic facies, vertebral malformations, retarded physical, mental, and sexual development, and cardiac murmur. J Pediatr. 1975 Jan;86(1):63–71. doi: 10.1016/s0022-3476(75)80706-2. [DOI] [PubMed] [Google Scholar]
- Boon J., Bakkeren J., Miseré J., Schretlen E., Parmentier G., Eyssen H. Increased trihydroxycoprostanic acid in bile in familial intrahepatic biliary atresia. Padiatr Padol. 1973;8(2):181–186. [PubMed] [Google Scholar]
- DANKS D., BODIAN M. A GENETIC STUDY OF NEONATAL OBSTRUCTIVE JAUNDICE. Arch Dis Child. 1963 Aug;38:378–390. doi: 10.1136/adc.38.200.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danks D. M., Campbell P. E., Smith A. L., Rogers J. Prognosis of babies with neonatal hepatitis. Arch Dis Child. 1977 May;52(5):368–372. doi: 10.1136/adc.52.5.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fausa O., Gjone E. Serum bile acid concentrations in patients with liver disease. Scand J Gastroenterol. 1976;11(5):537–543. [PubMed] [Google Scholar]
- Fausa O. Serum bile acid concentration after a test meal. Scand J Gastroenterol. 1976;11(3):229–232. [PubMed] [Google Scholar]
- Hanson R. F., Isenberg J. N., Williams G. C., Hachey D., Szczepanik P., Klein P. D., Sharp H. L. The metabolism of 3alpha, 7alpha, 12alpha-trihydorxy-5beta-cholestan-26-oic acid in two siblings with cholestasis due to intrahepatic bile duct anomalies. An apparent inborn error of cholic acid synthesis. J Clin Invest. 1975 Sep;56(3):577–587. doi: 10.1172/JCI108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksen N. T., Langmark F., Sorland S. J., Fausa O., Landaas S., Aagenaes O. Hereditary cholestasis combined with peripheral pulmonary stenosis and other anomalies. Acta Paediatr Scand. 1977 Jan;66(1):7–15. doi: 10.1111/j.1651-2227.1977.tb07801.x. [DOI] [PubMed] [Google Scholar]
- Landing B. H. Considerations of the pathogenesis of neonatal hepatitis, biliary atresia and choledochal cyst--the concept of infantile obstructive cholangiopathy. Prog Pediatr Surg. 1974;6:113–139. [PubMed] [Google Scholar]
- Riely C. A., LaBrecque D. R., Ghent C., Horwich A., Klatskin G. A father and son with cholestasis and peripheral pulmonic stenosis: a distinct form of intrahepatic cholestasis. J Pediatr. 1978 Mar;92(3):406–411. doi: 10.1016/s0022-3476(78)80428-4. [DOI] [PubMed] [Google Scholar]
- Ritland S., Blomhoff J. P., Elgjo K., Gjone E. Lipoprotein-X (LP-X) in liver disease. Scand J Gastroenterol. 1973;8(2):155–160. [PubMed] [Google Scholar]
- Seidel D. A new immunochemical technique for a rapid, semi-quantitative determination of the abnormal lipoprotein (LP-X) characterizing cholestasis. Clin Chim Acta. 1971 Jan;31(1):225–229. doi: 10.1016/0009-8981(71)90381-0. [DOI] [PubMed] [Google Scholar]
- Sommer A., Moody P. E., Jr, Reiner C. B. Familial extrahepatic biliary atresia. Report of a case situation. Clin Pediatr (Phila) 1976 Jul;15(7):627–629. doi: 10.1177/000992287601500710. [DOI] [PubMed] [Google Scholar]
- Thaler M. M., Gellis S. S. Studies in neonatal hepatitis and biliary atresia. I. Long-term prognosis of neonatal hepatitis. Am J Dis Child. 1968 Sep;116(3):257–261. doi: 10.1001/archpedi.1968.02100020259005. [DOI] [PubMed] [Google Scholar]
- Watson G. H., Miller V. Arteriohepatic dysplasia: familial pulmonary arterial stenosis with neonatal liver disease. Arch Dis Child. 1973 Jun;48(6):459–466. doi: 10.1136/adc.48.6.459. [DOI] [PMC free article] [PubMed] [Google Scholar]


